Back to Journals » Vascular Health and Risk Management » Volume 20
Intraluminal Thrombus of the Extracranial Cerebral Arteries in Acute Ischemic Stroke: Manifestations, Treatment Strategies, and Outcome
Authors Alhowaish TS , Alhamadh MS , Alsulayhim A , Alotaibi N , Alrashid AA , Alhabeeb AY , Alqirnas MQ , Alrushid E , Alnafisah MS , Anversha AA
Received 24 October 2023
Accepted for publication 21 December 2023
Published 3 January 2024 Volume 2024:20 Pages 1—12
DOI https://doi.org/10.2147/VHRM.S435227
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Thamer S Alhowaish,1,2 Moustafa S Alhamadh,2,3 Abdullah Alsulayhim,2,4 Najla Alotaibi,5 Azzam Abdulaziz Alrashid,2,3 Abdulrahman Yousef Alhabeeb,2,3 Muhannad Q Alqirnas,2,3 Eythar Alrushid,1,2 Mohammed S Alnafisah,1,2 Ajmal Ali Anversha1,2
1Division of Neurology, Department of Medicine, King Abdulaziz Medical City, Ministry of the National Guard Health Affairs (MNGHA), Riyadh, Kingdom of Saudi Arabia; 2King Abdullah International Medical Research Center, Ministry of the National Guard-Health Affairs, Riyadh, 11481, Kingdom of Saudi Arabia; 3College of Medicine, King Saud Bin Abdulaziz University for Health Sciences (KSAU-HS), Ministry of the National Guard-Health Affairs, Riyadh, 14611, Kingdom of Saudi Arabia; 4Radiology Department, King Abdul Aziz Medical City, Riyadh, Kingdom of Saudi Arabia; 5College of Public Health, Oregon State University, Corvallis, OR, USA
Correspondence: Ajmal Ali Anversha, Division of Neurology, King Abdulaziz Medical City, King Abdullah International Medical Research Center, Ministry of the National Guard Health Affairs, Riyadh, Kingdom of Saudi Arabia, Tel +966-11-8011111 Ext: 13460, Email [email protected]
Background: Intraluminal thrombus (ILT) of the cervical arteries is an uncommon finding that can lead to acute or recurrent ischemic stroke. Currently, antithrombotic therapy in the form of antiplatelet and/or anticoagulation is considered the mainstay of treatment, but evidence of which one has a better outcome is lacking.
Methods: A retrospective cohort study included 28 patients diagnosed with acute stroke or transient ischemic attack with ILT of the extracranial arteries from 2013 to 2022. The primary efficacy outcome was assessed as recurrent stroke, and the primary safety outcome was assessed as hemorrhagic complications. Secondary outcomes were assessed as the resolution of thrombi by CT angiography (CTA) and clinical improvement by the Modified Rankin Scale (mRS) and NIH Stroke Scale (NIHSS).
Results: Out of 28 patients, more than half (57.1%; n = 16) were males with a mean age of 57.8 ± 9.5 years and an average BMI of 26.9 ± 4.5 kg/m2. As initial treatment, twenty-four patients received anticoagulation and four received antiplatelet agents. Recurrent strokes were found in four patients (14.29%), and all were initially treated with anticoagulation. One patient in the anticoagulation group had a significant retroperitoneal hemorrhage. None of the patients in the antiplatelets group had a recurrent stroke or bleeding event. Initial treatment with antiplatelet agents significantly improved the NIHSS on day 7 (P = 0.017). A significant improvement in NIHSS on day 90 was observed in the anticoagulant group (P = 0.011). In the follow-up CTA performed on 24 patients, 18 (75%) showed complete resolution (3 out of 3 (100%) in the antiplatelet group and 15 out of 21 (71.43%) in the anticoagulant group).
Conclusion: Initial treatment with anticoagulants improves neurologic outcomes in patients with ILT-induced acute ischemic stroke but carries the risk of recurrent stroke and bleeding. However, initial treatment with dual antiplatelet agents appears to have comparable efficacy without sequelae, particularly in atherosclerosis-induced ILT.
Keywords: stroke, free-floating thrombus, intraluminal thrombus, Intraluminal clot, doughnut sign, antithrombotic, anticoagulation, antiplatelet agents, stroke in Saudi Arabia
Introduction
Intraluminal thrombus (ILT) is an infrequent finding that can lead to an acute or recurrent ischemic stroke. It is defined as an elongated thrombus attached to the arterial wall with circumferential blood flow at its most distal aspect and cyclical motion relating to cardiac cycles.1 Hence, it is sometimes referred to as a free-floating thrombus (FFT).2 ILT is also known as intraluminal clot,3,4 intraluminal non-occlusive thrombus,5 and the doughnut sign.6 ILT is commonly seen in the cervical arteries, such as the common carotid artery, internal carotid artery (ICA), and vertebral artery, but can also occur in the intracranial segments and other extra cervical arteries, such as the arch of the aorta, the brachiocephalic artery, and the subclavian artery.2,7 The prevalence of ILT among patients with acute stroke or transient ischemic attack (TIA) is around 3.2%, according to recent studies using computed tomography angiography (CTA).2 ILT is more common in men than women, with a ratio of 2:1.1,8 It has different overlapping pathologies with differing clinical implications.1 The most common etiology is a complication of an atherosclerotic or ulcerated plaque. Other medical and multifactorial conditions include hypercoagulability, autoimmune diseases, carotid artery aneurysm, dissection, cardiogenic embolism, cancer, and trauma.8,9 ILT can be readily detected with color Doppler studies and confirmed, if necessary, with a contrast-enhanced examination (computed tomography or magnetic resonance imaging).8,10,11 Due to the high risk of recurrent stroke and lack of evidence to direct appropriate treatment for ILT, its management is considered a therapeutic challenge and remains poorly defined.3,4
Several case series have reported different treatment modalities, including medical, surgical, and endovascular treatments. However, there have been no randomized controlled trials comparing medical (antiplatelet and/or anticoagulant) and interventional treatments (Carotid endarterectomy (CEA), endovascular treatment).12,13 Bhatti et al, in their review article, included 145 cases and concluded that there was no clear superiority between medical and surgical management for ILT of the carotid artery.1 Furthermore, Ferrero et al reviewed 16 cases of ILT of the ICA. They could not conclude that early surgery is superior to temporary anticoagulation and/or delayed intervention because of the absence of a comparison group.9 Although the best treatment strategy has yet to be determined, medical management with antithrombotic is currently the standard of care.8 Medical management may include a single antiplatelet (SAPT), dual antiplatelet (DAPT), anticoagulation, or a combination of antiplatelet and anticoagulation. Despite the agreement on antithrombotic as the medical treatment strategy in some studies, diverse antithrombotic approaches were used, yet which approach is the best is still unknown.3,4,14,15
Therefore, we aimed to evaluate the efficacy and safety outcomes of various antithrombotic strategies for ischemic stroke or TIA secondary to ILT of the extracranial cerebral arteries in our center. We retrospectively analyzed our data and compared our results with the published literature.
Method
Study Design and Setting
This was a single-center retrospective cohort study conducted at King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia.
Inclusion and Exclusion Criteria
All patients who presented with acute ischemic stroke or TIA secondary to ILT of the extracranial cerebral arteries and confirmed by brain CTA from 2013 to 2022 were screened. An ILT was diagnosed if there was a filling defect in the arterial lumen surrounded by the contrast. ILT had to be in one of the following arteries to be eligible for inclusion: Common carotid, ICA, vertebral, subclavian, brachiocephalic arteries, or aortic arch. Patients with ILT who received tissue plasminogen activators (tPA) were also included. In addition, the included patients had to have a follow-up visit within three months of the initial insult. We excluded patients who had no follow-up, had essential data missing, had not received any treatment, or had a complete occlusion.
Data Collection
A diagnostic neuro-radiologist retrospectively screened all CT brain angiograms taken from January 2013 until April 2022 in KAMC for luminal thrombus using the Change Healthcare Radiology Solutions Picture Archiving and Communication System (PACS) and the Radiology Information System (RIS). A consultant Stroke physician reviewed all the selected patients to meet our inclusion criteria. The following data were collected for the included patients from the patient’s electronic records using the KAMC electronic system Best-Care; Seoul, South Korea: ezCaretech Co. Demographic data and comorbid conditions, Presenting symptoms, NIHSS and mRS at admission, discharge, and follow-up, Location of the thrombus, The cause of the stroke, Treatment given (SAPT, DAPT, anticoagulants, both antiplatelet and anticoagulants, tPA, acute intervention with either mechanical or surgical means), Duration of treatment, Laboratory values (hemoglobin, hematocrit, platelet, and hemoglobin A1C), Outcomes (resolution of the thrombus in the follow-up brain CTA), stroke recurrence and hemorrhagic complications such as Intra or extracranial bleeding.
Statistical Analysis
Descriptive statistics are presented as the mean ± standard deviation (SD) for continuous parameters and as numbers (percentages) for categorical parameters. The analysis was performed by comparing patients on antiplatelet agents versus those on anticoagulants at different treatment time intervals using the Chi-square test. Time intervals were initial treatment (less than seven days since presentation), short-term treatment (7 days to 3 months), and long-term treatment (more than three months). In addition, the relationship between admission and discharge was evaluated based on the mRS scores, which ranged from 0 (no symptoms) to 6 (death), and the NIHSS. The mRS score was assessed using Fisher’s Exact test, and the NIHSS score was assessed using Welch’s two-sample t-test. Results were considered significant at an alpha level of 0.05. All statistical analyses were completed using R Statistical Software (Foundation for Statistical Computing, Vienna, Austria).
Ethical Considerations
The study was approved by the Institutional Review Board of King Abdullah International Medical Research Center, MNG-HA, Riyadh, Kingdom of Saudi Arabia (RC20/665/R). Informed consent was waived because of the retrospective nature of this study. Access to the data was restricted to the researchers. The confidentiality of all patients was protected, and no names or medical record numbers were used. Privacy and confidentiality were assured, and all the hard and soft copies of data were kept in a secure place within the MNG-HA premises.
Results
The demographics of the patients are shown in (Table 1). There were a total of 45 patients with an ILT of the extracranial cerebral arteries, only 28 of whom were eligible for inclusion. More than half (57.1%; n = 16) of the patients were males. The patients’ mean age was 57.8 ± 9.5 years, with an average BMI of 26.9 ± 4.5 kg/m2. Only a small proportion (14.3%; n = 4) of the patients were documented as smokers. Hypertension (HTN) was the most notable comorbidity (60.7%; n = 17), followed by Diabetes mellitus (DM) (57.1%; n = 16), previous TIA or stroke (39.3%; n = 11), and PFO (17.9%; n = 5). The ICA was the most commonly involved artery, followed by the aortic arch, accounting for 87.6% and 7.1%, respectively (Figure 1). Those with ICA thrombus had significantly better discharge mRS and NIHSS scores than non-carotid arteries (P=0.02 and P<0.0001, respectively). Unilateral limb weakness, dysarthria, and facial weakness were the most frequent presenting symptoms (Table 2). The majority (60.7%; n = 17) of the patients presented to the hospital in less than 12 hours since symptoms onset, with almost a third (28.6%; n = 8) presented between 12 and 48 hours after symptoms onset and the remaining patients (10.7%; n=3) presented after 48 hours. Patients who were obese or overweight had a significantly more extended hospital stay (P=0.032).
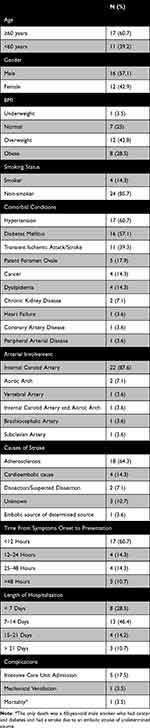 |
Table 1 Patients’ Baseline Characteristics and Associated Comorbid Conditions |
 |
Table 2 The Presenting Signs and Symptoms of the Studied Sample |
The majority (85.7%; n = 24) of the patients were initially (<7 days since presentation) anti-coagulated, and all received heparin. As short-term treatment (7 days to 90 days), 20 patients received anticoagulants, and eight received antiplatelet agents. As long-term treatment (>3 months since presentation), 12 received anticoagulants, and 14 received antiplatelet agents (Table 3). Admission NIHSS score was higher in the antiplatelet group compared to the anticoagulant group (11.3±7.8 Vs 7.2±5.4). Three patients were treated with tPA on admission, two of whom were subsequently treated with heparin and one with a single antiplatelet agent 24 hours after thrombolysis.
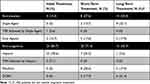 |
Table 3 Treatment Offered to the Patients at Different Time Intervals |
Four (14.29%) out of 28 patients had recurrent strokes (Table 4). Three of these patients had recurrence within three months, and one after three months. Two of the three patients had recurrent strokes within one week due to ILT in ICA. One patient had it after two months due to ILT in the aortic arch. All three subjects were initially treated with anticoagulation and switched to warfarin as short-term therapy. The fourth patient, who had a stroke after three months, was initially treated with heparin, followed by warfarin, and then was switched to aspirin after two months as follow-up CTA showed resolution of ILT in the ICA. However, after six months, she developed another stroke in the same ICA territory with a new ILT which was again treated with anticoagulation. This patient was later found to have Atrial fibrillation (AF) on prolonged cardiac monitoring with REVEAL device. Also, among the anticoagulation group, one patient had a significant retroperitoneal hemorrhage three days after starting heparin as an initial treatment, which led to hemodynamic instability, acute renal failure, low hemoglobin, and ICU admission. On the other hand, four patients were initially treated with antiplatelet agents, and none had a recurrent stroke or bleeding complication.
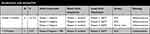 |
Table 4 Safety Outcomes Based on Treatment Group |
Initial treatment with antiplatelet agents led to a significant improvement in NIHSS on day seven, but not on day 90 (P = 0.011). However, when comparing the difference between the NIHSS at admission and at day 90, anticoagulants significantly improved the NIHSS (P = 0.017). (Table 5)
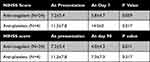 |
Table 5 Efficacy Outcomes Based on NIHSS at Different Time Intervals |
Follow-up repeat scans that were done in 24 patients showed complete resolution in 18 patients (75%) (Figure 2). Three of the four patients initially treated with antiplatelet agents had a follow-up CT, and all (100%) had complete thrombus resolution. On the other hand, 21 patients initially treated with anticoagulants had a follow-up CT, and a complete resolution of the thrombus was found in 15 (71.43%). In the anticoagulants group, one patient had a worsening thrombus, three patients had a partial resolution, and the remaining two had no change (Table 6). The patient with worsening thrombus was associated with severe ICA stenosis.
 |
Table 6 Efficacy Outcomes Based on Follow-Up Repeat Scans |
Five patients (17.5%) were admitted to the ICU, and admission was required in 50% (N=2) of patients who started with antiplatelet agents and 12.5% (N=3) who started with an anticoagulant required ICU admission.
Discussion
In cases of complete ICA occlusion, intervention is rarely needed except in cases of tandem occlusion in a hyper-acute stroke where recanalization of the ICA is necessary before the middle cerebral artery.16–18 Contrary to the complete occlusion of ICA, ILT, which is almost always symptomatic, can be associated with an increased risk of stroke recurrence if not treated acutely, mainly due to the dislodging of the clot that causes embolism to the brain.1,2,19 Although the detection and reporting of ILT of the extracranial cerebral arteries is still rare due to its low incidence rate,14,20 once detected, it is associated with poor outcomes if not treated promptly and appropriately.1 For this reason, treatment should be considered immediately after diagnosis. In addition, there is no clear definition of ILT and it is difficult to find comparable case studies. Therefore, it is a challenge to develop a clinical management strategy for ILT based on scientific resources.1
Similar to Bhatti et al, Ferrero, Emanuele et al, and the majority of previous studies, our patients were all symptomatic, and seventeen (60%) of them presented within 12 hours of symptoms onset, which emphasizes the fact that ILT is considered an emergency that needs immediate action.
Males were more commonly affected in our study population, with a mean age of patients 57.8 ± 9.5 years, which is much younger than the typical age reported having an atherosclerotic carotid disease according to Bhatti et al.1 The younger age in our study is likely due to the increasing prevalence of atherosclerosis risk factors in the Saudi population. According to WHO, Saudi Arabia ranks second in the prevalence of DM in the Middle East. A more recent study reported that the prevalence of DM had risen to 34.1% in males and 27.6% in females.21,22 The same is true for HTN in our population.23 In addition, 39.3% of our patients had a previous stroke or TIA. In comparison to Singh et al study which showed 18% had a previous stroke or TIA.2 The most reported cause of stroke in our study was vascular atherosclerosis (64.28%), which was also the most commonly reported cause of ICA stroke in Singh et al (82%) and Ferrero et al (81.3%).2,9
In our study, recurrent strokes were found in four patients, and almost the same percentage was reported by Fridman et al.24 All four patients who had a recurrent stroke were initially treated with heparin and then switched to warfarin as short-term therapy. A stroke recurrence within three months may indicate treatment failure and incomplete resolution of existing thrombi. However, stroke recurrence after three months is mainly due to an etiology other than the pre-existing thrombus. In the antiplatelet group, no recurrent stroke was seen. Even though there were no recurrent strokes or bleeding events in the antiplatelet group, we could not conclude superiority due to the small number of patients. Singh et al included 61 patients with ILT in their study and found stroke recurrence in four patients; heparin was the initial therapy for two patients, and the other two patients received antiplatelet agents (one patient received aspirin monotherapy, and the other received dual therapy with aspirin and clopidogrel).2 Other studies showed conflicting results about which antithrombotic is associated with the risk of future stroke recurrence. Another study by Vellimana et al included twenty-four patients and showed that using antiplatelet agents plus anticoagulation in patients with ILT was associated with a low rate of recurrent ischemic events.7 In Karan et al study of 18 patients with a DAPT plus parenteral anticoagulation regimen, there were neither recurrent ischemic events nor bleeding episodes.13 Although most physicians prefer to use anticoagulation as initial treatment, no clear superiority was found in these retrospective cohorts, just like in our study. Hence, it may be reasonable to use DAPT, which can be equally and more effective with less bleeding risk, especially if the underlying etiology is atherosclerosis.
In our study, follow-up repeat scans showed complete resolution in eighteen patients (75%), and repeat scans showed 100% and 71.43% resolution of the thrombus in the antiplatelet and anticoagulant groups, respectively. The literature review by Bhatti et al showed that complete resolution of the ILT, without any further neurologic progression, occurred in 86% of patients treated medically. Also, our findings are almost consistent with the Vellimana et al findings.7 Similarly, in the study by Buchan et al, fourteen patients were treated medically with an anticoagulant, and eight of those did not need a delayed surgical intervention and had a resolution of the clot by angiography as well as good clinical outcomes.25 In an Indian study that included eighteen patients diagnosed with acute ischemic stroke and extracranial carotid artery thrombus, patients were managed medically with DAPT and low‑molecular‑weight heparin, followed by an angiogram after 14 days of allocation. The results suggested that 50% had a resolution of the thrombus. Those with persistent thrombus were significantly older and had associated comorbidities. The authors concluded that their regimen of DAPT plus short‑term anticoagulation was safe and effective in managing ILT.13 Compared to this study, our study showed that either anticoagulation alone or DAPT alone resulted in similar or better thrombus resolution rates.
Our study’s most popular medical management strategy was initial heparin treatment, followed by conversion to warfarin for several weeks to months, the same strategy reported by Bhatti et al and a previous study.1,26 There was an improvement in the day 7 and day 90 NIHSS scores in the antiplatelet and anticoagulant groups, respectively. Patients with severe stroke likely tend to get antiplatelet agents rather than anticoagulants because of the perceived risk of hemorrhagic transformation in this group. This was obvious in our study group as higher admission NIHSS in the antiplatelet group compared to the anticoagulant group. Of six patients who were switched to DOAC, only one patient was diagnosed with atrial fibrillation; we assume that the other patients were treated “off-label” at the physician’s discretion.
Although our treatment was based mainly on a medical approach rather than surgical intervention for most cases, three of our patients underwent interventions for the ICA following the initial medical management. Two patients had delayed stenting. One patient underwent CEA, and this patient had an ICA ILT, which was treated with heparin and then warfarin before being discharged home. However, after a few days, she was readmitted for stroke symptoms and worsening stenosis and thrombus; hence proceeded to CEA. This patient had further ICA thrombosis post-CEA and developed a massive stroke. According to one of the largest series that compared different interventional approaches for ILT, no definitive statement about the relative risk and benefit of surgical or endovascular intervention can be made due to the small number of these subtypes of management.1,27,28 Medical treatment can be used alone or in combination with delayed revascularization.13 A study of six patients treated with anticoagulation alone showed no recurrent ischemic events. The same study included three additional patients treated with anticoagulation and delayed revascularization, with no recurrence between starting anticoagulation and surgery. One patient in that study died as a result of a fatal post-carotid endarterectomy stroke.4 An early emergent surgical intervention is an option for carotid ILT. However, results from multiple studies have demonstrated a high risk of perioperative stroke (12–29%). Moreover, it was reported in another study that there was a 17% risk of perioperative stroke or death after early carotid stenting. Also, Karan et al study of 18 patients reported that out of the three patients who underwent CEA directly, one developed a postoperative ischemic stroke.13 On the other hand, Caplan et al reported in their small case series that there was no stroke recurrence after early CEA.4
Study Limitations and Future Directions
This study had several limitations. First, it was a retrospective study, and some defects in the study design cannot be ignored (eg, small sample size, single-center design). Second, we excluded some patients due to a lack of follow-up. Third, most of our patients were treated with anticoagulants and only four with antiplatelet agents; this makes direct comparison difficult. However, our study results could contribute to a wider meta-analysis. Due to the practical difficulties of doing a randomized controlled trial in this patient group, a meta-analysis study could guide us to a better conclusion.
Conclusion
ILT was found to be more frequently reported in men than women and at a younger age in the Saudi population. The ICA was the most commonly affected vessel and was associated with better neurological outcomes than the non-carotid ILT. The most commonly associated etiology of ILT was atherosclerosis. Initial anticoagulation treatment was our cohort’s most commonly used strategy, but there were stroke recurrences and significant bleeding in that group. On the other hand, antiplatelet treatment was used in a smaller number of patients, none of whom had a recurrent stroke or bleeding, and all had complete resolution of thrombi.
Recommendations
Based on our study and previously published studies, ILT has a good prognosis overall, irrespective of the initial treatment with anticoagulation or DAPT. We suggest treating these patients based on the underlying etiology. We prefer DAPTs as initial treatment if ILT is associated with atherosclerotic plaque and anticoagulants for non-atherosclerotic ILT. A meta-analysis of all the published studies may shed more light on this. With our population’s low mean age of stroke, which is related to the increasing prevalence of risk factors, we recommend an effective public health awareness and screening program.
Abbreviations
ILT, Intraluminal thrombus; CTA, Computed Tomography Angiography; NIHSS, National Institute of Health Stroke Score; mRS, Modified Rankin Score; FFT, Free-Floating Thrombus; ICA, Internal Carotid Artery; TIA, Transient Ischemic Attack; CEA, Carotid Endarterectomy; SAPT, Single Antiplatelet; DAPT, Dual Antiplatelet; tPA, Tissue Plasminogen Activator; HTN, Hypertension; DM, Diabetes Mellitus; AF, Atrial fibrillation.
Data and Materials Availability
The dataset used and/or analyzed to write the current study is available upon request.
Acknowledgments
Dr Yazan Alghammas for his valuable contribution to drawing Figure 1.
The abstract of this paper was presented at the 7th Health Specialties Conference (HPC) as a conference talk with interim findings. The abstract was published in HPC Abstract Booklet.
Contribution to the Field
Given the high risk of recurrence and the limited data to direct the appropriate treatment, ILT is considered a therapeutic challenge. This paper evaluated the efficacy and safety outcomes of medical treatment for the ILT of the extracranial cerebral arteries. This manuscript is important in stroke because ILT is considered rare, most published studies are based on case reports and case series, and no clinical trial compares different antithrombotic agents (antiplatelet and/or anticoagulant). Most physicians prefer to treat ILT with anticoagulation despite no clear evidence. We raise an important question of whether dual antiplatelet treatment could be equally or more effective in preventing recurrent stroke due to ILT. So far, no studies have addressed this particular question. Our data suggest that we could use dual antiplatelet treatment for ILT with equal efficacy and less bleeding risk. Though the numbers are small in our study, our cohort may enrich the literature and contribute to a systemic meta-analysis. With more published studies, researchers and strokologist can have better medical treatment strategies for managing this rare type of stroke.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work”.
Funding
There is no funding to report.
Disclosure
All authors declare no conflict of interest.
References
1. Bhatti AF, Leon LR, Labropoulos N, et al. Free-floating thrombus of the carotid artery: literature review and case reports. J Vasc Surg. 2007;45(1):199–205. doi:10.1016/j.jvs.2006.09.057
2. Singh RJ, Chakraborty D, Dey S, et al. Intraluminal thrombi in the cervico-cephalic arteries. Stroke. 2019;50(2):357–364. doi:10.1161/STROKEAHA.118.023015
3. Biller J, Adams HP, Boarini D, Godersky JC, Smoker WRK, Kongable G. Intraluminal clot of the carotid artery. A clinical-angiographic correlation of nine patients and literature review. Surg Neurol. 1986;25(5):467–477. doi:10.1016/0090-3019(86)90086-8
4. Caplan L, Stein R, Patel D, Amico L, Cashman N, Gewertz B. Intraluminal clot of the carotid artery detected radiographically. Neurology. 1984;34(9):1175–1181. doi:10.1212/WNL.34.9.1175
5. Demchuk AM, Puetz V, Dzialowski I, et al. Frequency and clinical course of stroke and transient ischemic attack patients with intracranial nonocclusive thrombus on computed tomographic angiography. Stroke. 2009;40(1):193–199. doi:10.1161/STROKEAHA.108.526277
6. Menon BK, Singh J, Al-Khataami A, Demchuk AM, Goyal M. The donut sign on CT angiography: an indicator of reversible intraluminal carotid thrombus? Neuroradiology. 2010;52(11):1055–1056. doi:10.1007/s00234-010-0738-x
7. Vellimana AK, Kadkhodayan Y, Rich KM, et al. Symptomatic patients with intraluminal carotid artery thrombus: outcome with a strategy of initial anticoagulation. J Neurosurg. 2013;118(1):34–41. doi:10.3171/2012.9.JNS12406
8. Akpınar ÇK, Özdemir AÖ. Free-floating thrombus in the carotid artery: two different etiologies and treatment approaches. Turkish J Cerebrovasc Dis. 2019;25(2):129–133. doi:10.5505/tbdhd.2018.73636
9. Ferrero E, Ferri M, Viazzo A, et al. Free-floating thrombus in the internal carotid artery: diagnosis and treatment of 16 cases in a single center. Ann Vasc Surg. 2011;25(6):805–812. doi:10.1016/j.avsg.2011.02.030
10. Rossetti AO, Urbano LA, Lobrinus JA, Devuyst G; Stroke vignette. Ultrasonographical, radiological and pathological correlation of a floating thrombus in the common carotid artery. Cerebrovasc Dis. 2002;14(1):64. doi:10.1159/000063727
11. Pagliariccio G, Catalini R, Zingaretti O, Mancinelli L. Idiopathic floating thrombus of the common carotid artery: diagnosis and treatment options. J Ultrasound. 2010;13(2):57. doi:10.1016/j.jus.2010.07.001
12. Giragani S, Balani A, Agrawal V. Stentriever thrombectomy with distal protection device for carotid free floating thrombus: a technical case report. J Neurointerv Surg. 2017;9(8):e33. doi:10.1136/neurintsurg-2016-012904.rep
13. Karan V, Vyas D, Bohra V, Huded V. Symptomatic extracranial carotid artery thrombus: an Indian experience. J Neurosci Rural Pract. 2019;10(2):312. doi:10.4103/jnrp.jnrp_225_18
14. Roberson GH, Scott WR, Rosenbaum AE. Thrombi at the site of carotid stenosis. Radiology. 1973;109(2):353–356. doi:10.1148/109.2.353
15. Combe J, Poinsard P, Besancenot J, et al. Free-floating thrombus of the extracranial internal carotid artery. Ann Vasc Surg. 1990;4(6):558–562. doi:10.1016/S0890-5096(06)60839-X
16. Hackam DG. Prognosis of asymptomatic carotid artery occlusion: systematic review and meta-analysis. Stroke. 2016;47(5):1253–1257. doi:10.1161/STROKEAHA.116.012760
17. Thanvi B, Robinson T. Complete occlusion of extracranial internal carotid artery: clinical features, pathophysiology, diagnosis and management. Postgrad Med J. 2007;83(976):95. doi:10.1136/pgmj.2006.048041
18. Constantinou J, Jayia P, Hamilton G. Best evidence for medical therapy for carotid artery stenosis. J Vasc Surg. 2013;58(4):1129–1139. doi:10.1016/j.jvs.2013.06.085
19. Inoue M, Olivot JM, Labreuche J, et al. Impact of diffusion-weighted imaging Alberta stroke program early computed tomography score on the success of endovascular reperfusion therapy. Stroke. 2014;45(7):1992–1998. doi:10.1161/STROKEAHA.114.005084
20. Choi HY, Ye BS, Ahn SH, et al. Characteristics and the fate of intraluminal thrombus of the intracranial and extracranial cerebral arteries in acute ischemic stroke patients. Eur Neurol. 2009;62(2):72–78. doi:10.1159/000222776
21. Al Dawish M A, Alwin Robert A, Braham R, et al. Diabetes mellitus in Saudi Arabia: a review of the recent literature. Curr Diabetes Rev. 2016;12(4):359–368. doi:10.2174/1573399811666150724095130
22. Alqahtani B, Elnaggar RK, Alshehri MM, Khunti K, Alenazi A. National and regional prevalence rates of diabetes in Saudi Arabia: analysis of national survey data. Int J Diabetes Dev Ctries. 2022;43:1–6.
23. Aldiab A, Shubair MM, Al-Zahrani JM, et al. Prevalence of hypertension and prehypertension and its associated cardioembolic risk factors; a population based cross-sectional study in Alkharj, Saudi Arabia. BMC Public Health. 2018;18(1): doi:10.1186/s12889-018-6216-9
24. Fridman S, Lownie SP, Mandzia J. Diagnosis and management of carotid free-floating thrombus: a systematic literature review. J Vasc Surg. 2019;70(1):329–330. doi:10.1016/j.jvs.2019.04.447
25. Buchan A, Gates P, Pelz D, Barnett HJM. Intraluminal thrombus in the cerebral circulation Implications for surgical management. Stroke. 1988;19(6):681–687.
26. Caplan LR. Resolved: heparin may be useful in selected patients with brain ischemia. Stroke. 2003;34(1):230–231. doi:10.1161/01.STR.0000047036.77466.E8
27. Chakhtoura EY, Goldstein JE, Hobson RW. Management of mobile floating carotid plaque using carotid artery stenting. J Endovasc Ther. 2003;10(3):653–656. doi:10.1177/152660280301000336
28. González A, Mayol A, Gil-Peralta A, González-Marcos JR, Boza F, Ruano J. Angioplasty of symptomatic high-grade internal carotid artery stenosis with intraluminal thrombus: therapeutic approach. Neuroradiology. 2004;46(4):313–317. doi:10.1007/s00234-004-1168-4
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


