Back to Journals » Infection and Drug Resistance » Volume 16
Intervention Effect of New Tuberculosis Control Model on Tuberculosis Incidence in Xinjiang
Authors Zhang Y , Wang X, Liu N, Wang S, Wang X, Cao M
Received 25 September 2023
Accepted for publication 29 November 2023
Published 6 December 2023 Volume 2023:16 Pages 7485—7496
DOI https://doi.org/10.2147/IDR.S441899
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Yan Zhang,1 Xinqi Wang,2 Nianqiang Liu,2 Senlu Wang,2 Xiaomin Wang,1 Mingqin Cao1
1Department of Epidemiology and Health Statistics, College of Public Health, Xinjiang Medical University, Urumqi, Xinjiang, 830011, People’s Republic of China; 2The Center for Disease Control and Prevention of Xinjiang Uygur Autonomous Region, Urumqi, Xinjiang, 830002, People’s Republic of China
Correspondence: Mingqin Cao, Department of Epidemiology and Health Statistics, College of Public Health, Xinjiang Medical University, No. 393 Xinyi Road, Urumqi, 830011, People’s Republic of China, Tel +86-13319912419, Email [email protected]
Objective: To quantitatively evaluate the intervention effect of the “Xinjiang model” policy on pulmonary tuberculosis (PTB) incidence in Xinjiang, and to compare the difference of policy effect between areas with different tuberculosis burdens.
Methods: We retrospectively collected data on the registered incidence of PTB patients in 14 prefectures of Xinjiang from January 2012 to December 2021 and used Joinpoint model to describe the time trend of registered incidence, single-group interrupted time series (ITS) model to analyze the dynamics of registered incidence before and after the policy intervention, and controlled interrupted time series (CITS) model to compare the differences in the effects of the policy in different tuberculosis burdened areas.
Results: The areas with high registered incidence of PTB in Xinjiang were mainly located in the four prefectures of southern Xinjiang. The time trend of registered incidence of PTB in Xinjiang from 2012 to 2021 showed a general downward trend (AAPC=− 3.4%), an upward trend from 2012 to 2018 (APC=12.1%), and a rapid downward trend from 2018 to 2021 (APC=− 28.3%). Single-group ITS results showed that registered incidence in Xinjiang increased by 13.806/100,000 one month after policy was implemented (P< 0.001); the long-term effect of policy was a downward trend in registered incidence (β3< 0, P< 0.001), decreasing by 0.690/100,000 per month. In high-, medium-, and low-burden areas of PTB, the long-term effect of policy was a monthly decrease in registered incidence of 1.460/100,000, 0.227/100,000, and 0.064/100,000, respectively. The long-term effects of policy interventions in high- and medium-burden areas showed a faster decline in registered incidence than in low-burden areas (β7 was − 1.548 and − 0.194, respectively, P< 0.001).
Conclusion: A dynamic causal relationship exists between “Xinjiang model” policy and registered incidence, and its continued implementation is effective in controlling the spread of tuberculosis.
Keywords: pulmonary tuberculosis, interrupted time series, policy evaluation, active case finding, treatment
Introduction
Tuberculosis is a chronic infectious disease that seriously endangers human health. China is one of the 30 countries with high tuberculosis burden in the world, with an estimated new tuberculosis case of 780,000 (incidence rate of 55/100,000) in 2021, second only to Indonesia (969,000) and India (2.95 million).1 Xinjiang is a high incidence area of tuberculosis in China, and the reported incidence has been in the forefront of the whole country, especially in the four prefectures of southern Xinjiang (Hotan, Aksu, Kashgar and Kizilsu Kirgiz Autonomous Prefecture).2,3 In view of the serious situation of tuberculosis epidemic in Xinjiang, a series of innovations such as incorporating tuberculosis chest X-ray screening into national health examination, hospitalization of tuberculosis patients during infectious period, and home treatment mode of “centralized medication + nutritious breakfast” were implemented in July 2018, forming a new tuberculosis prevention and control model in line with the actual situation in Xinjiang, namely “Xinjiang Model”.4 Because the “Xinjiang model” policy is leading in the field of tuberculosis control in China, quantitative evaluation of the effect of the policy in Xinjiang tuberculosis control is of great value to the promotion of the “Xinjiang model” policy.
The primary problem of policy evaluation is whether there is a causal relationship between the implementation of the policy and the output of the target variable. Randomized controlled trials (RCTs) are the gold standard for assessing causality, but they are often difficult to conduct because of ethical and feasibility constraints, especially for population-level health policies and programs.5 In the real world, policy evaluation usually relies on evidence from natural experiments or observational studies, and quasi-experimental design can be used to identify the real causal relationship between policy variables and target variables. Interrupted time series (ITS) design is one of the robust and powerful quasi-experimental designs that can be used to assess the effectiveness of population-level health interventions implemented at well-defined time points, visually demonstrates the short-and long-term effects of policy interventions, and reduces the possibility that intervention effects are confounded by long-term trends and time-varying confounders.6–8
In order to comprehensively and objectively evaluate the implementation effect of the “Xinjiang Model” policy at the population level, the study was conducted from two perspectives: the whole (Xinjiang region) and the local (areas with a high-, medium- and low-burden of tuberculosis). Based on registered incidence of PTB from 2012 to 2021, the causal effect between the “Xinjiang model” policy and registered incidence was analyzed using the ITS method, and the differences of the policy implementation among areas with different tuberculosis burdens were compared, to provide quantitative data support for the development and promotion of the new model of tuberculosis prevention and treatment in Xinjiang.
Materials and Methods
Study Setting
In July 2018, on the basis of fully implementing the “trinity” tuberculosis prevention and control mode characterized by integration of medical prevention and control (ie, the three-level tuberculosis prevention and control network with the Center for Disease Control and Prevention, designated tuberculosis hospitals and community health service centers as the core),9 Xinjiang strengthened its efforts to continuously strengthen tuberculosis prevention and control and began to implement the “Xinjiang Model” policy. The policy of “Xinjiang Model” prevents and controls tuberculosis from three aspects: (i) actively finding tuberculosis patients, that is, carrying out tuberculosis screening in key population and incorporating tuberculosis chest X-ray screening into national health examination; (ii) expanding the coverage of treatment, that is, on the one hand, to improve the medical service ability of designated medical institutions for tuberculosis, on the other hand, to implement 100% reimbursement of outpatient medical examination expenses and 90% reimbursement of hospitalization expenses for PTB patients to improve the medical security level of patients; (iii) improving the quality of tuberculosis treatment, that is to say, hospitalization for tuberculosis patients in infectious period and “centralized medication + nutritious breakfast” in consolidation period. Centralized medication means that patients go to designated village/community health service room for medication every day, and eat nutritious breakfast half an hour after taking the medicine, which includes eggs, milk and bread.
Study Design and Data Sources
This study was a retrospective study, using 14 prefectures in Xinjiang as the basic data collection unit, and retrospectively collected the registered incidence data of PTB patients from January 2012 to December 2021. Data were collected from the China Tuberculosis Management Information System, both longitudinally and routinely. The registered incidence reflects the epidemic intensity of tuberculosis, which can be used to evaluate the intervention effect of “Xinjiang model” policy in the whole population. Registered incidence = number of PTB patients registered in medical institutions/population × 100,000/100,000. Population data for each year are taken from the Xinjiang Statistical Yearbook.
Research Methods
In this study, registered incidence was used as outcome variable. First, Joinpoint model was constructed to describe and analyze the time trend of registered incidence, and then ITS model was used to analyze the intervention effect of “Xinjiang model” policy.
Joinpoint Regression Model
Joinpoint regression analysis is a time trend analysis method, superior to other time trend analysis methods that only analyze overall trends,10 which can divide a time period into multiple parts and find statistically significant connection points of time trends to reveal specific trends of local data. The model uses the least square method to estimate the variation of rate, avoiding the non-objectivity of typical trend analysis based on linear trend.11 The main outcome measures of the model include annual percent change (APC) and average annual percent change (AAPC). APC is used to evaluate the internal trend of each independent time interval of the piecewise function, or the global trend with 0 connection points; AAPC is used to evaluate the global average change trend including multiple time intervals. APC and AAPC are dimensionless relative numbers that reflect only the direction and speed of time trend change. APC and AAPC less than 0 indicate that the outcome variable has a downward trend over time; APC and AAPC greater than 0 indicate that the outcome variable has an upward trend over time.
Log-linear model  indicating the result variable and x indicating the time, then the APC calculation formula of the fitted model is:
indicating the result variable and x indicating the time, then the APC calculation formula of the fitted model is:
where wi is the interval span width of each segmentation function, and βi is the regression coefficient corresponding to each interval.
Interrupted Time Series
Model Introduction
ITS uses a time series of specific results to establish potential trends that are pre-“broken” at known time points. The hypothetical scenario in which the intervention does not occur and the trend remains unchanged is called a “counterfactual”. This counterfactual scenario provides a comparison for assessing the impact of the intervention by examining any changes that occur in the post-intervention period.12 ITS uses piecewise regression analysis to model the trend before and after intervention, and uses statistical models to evaluate the effect of intervention measures, including the level change and slope change before and after intervention points.13
Single-group ITS model in which there is only one group of time series data and an intervening event occurs at a particular point in time, the model equation is:
Where Y is the outcome variable; β0 is the constant term; Time is the time series, which corresponds to the observation point; Int represents the intervention stage where the observation point is located; Post represents the time series after the intervention; ε represents the random error; β1 is the change trend before the intervention; β2 is the level change; β3 is the difference of slope change before and after the intervention; β1+β3 is the slope after the intervention, indicating the change trend after the intervention.
History limits the ability to draw causal inferences from a single-group interrupted time series model, a control group can be introduced for comparative analysis14 called controlled interrupted time series (CITS) model. It can help to study multiple groups of time series data and compare the effect of intervention between different groups, the CITS model equation is:
where Group is a dummy variable representing the group (experimental or control); β0 to β3 represent the parameter estimates for the control group; β4 to β7 represent the parameter estimates for the experimental group; β4 is the difference between the intercept terms of the control and experimental groups before the intervention; β5 is the difference between the slopes of the control and experimental groups before the intervention; β6 is the difference between the amount of the change in immediate level at the time of the intervention occurrence in the control and experimental groups; β7 is the difference between the amount of slope change in the control and experimental groups after the intervention.
Model Construction
The study used registered incidence of PTB as the outcome variables, the implementation of the “Xinjiang Model” policy in July 2018 as the intervention cut-off point, and the independent variables included time variables, representing each month from January 2013 to December 2023. For the two stages before the implementation of the policy (January 2012 ~ June 2018) and after the implementation (July 2018 ~ December 2021), the implementation effect of the “Xinjiang Model” policy is analyzed by single-group ITS.
In order to evaluate the implementation effect of the “Xinjiang model” policy in areas with different PTB burdens, the study constructed a CITS model to compare the implementation effect of the policy, using low-burdened areas as control areas, and medium- and high-burdened areas as experimental areas, respectively.
Statistical Processing
The study used Excel 2019 software for data collection and collation. Arcgis10.8 software was used to make maps to describe the spatial distribution of registered incidence in Xinjiang. Log-linear regression models were constructed using Joinpoint Regression Program 4.9.0 to calculate APC and AAPC to describe the temporal trend of registered incidence. ITS model was constructed by itsa function in Stata 16 software. The Durbin Watson method was used to test whether there was first-order autocorrelation in time series,15 and Prais-Winsten method was used to deal with the first-order autocorrelation problem. α=0.05 is used as the test level.
Result
Prevalence of Registered Incidence of PTB
Spatial Distribution of Registered Incidence in Xinjiang
From 2012 to 2021, the areas with high registered incidence of PTB in Xinjiang were mainly located in Aksu, Hotan, Kashgar, and Kizilsu Kyrgyz Autonomous Prefecture, which were called high-burden areas of PTB, with an average registered incidence of 279.20/100,000; the areas with low registered incidence were mainly located in Urumqi, Karamay, Changji Hui Autonomous Prefecture, and Hami, which were called low-burden areas of PTB, with an average registered incidence of 46.81/100,000; and the other regions (Tacheng, Altay, Bortala Mongol Autonomous Prefecture, Bayinguoleng Mongol Autonomous Prefecture, Ili Kazakh Autonomous Prefecture, Turpan) were called medium-burden areas of PTB, and the average registered incidence was 86.25/100,000, as shown in Figure 1.
 |
Figure 1 Spatial prevalence of registered incidence of PTB in Xinjiang from 2012 to 2021. |
Temporal Distribution of Registered Incidence in Xinjiang
From 2012 to 2021, registered incidence in Xinjiang showed a general downward trend (AAPC=−3.4%, P<0.05), and the turning point of time trend change was 2018, showing an upward trend (APC=12.1%) from 2012 to 2018, and a rapid downward trend (APC=−28.3%) from 2018 to 2021; registered incidence of PTB in high-, medium- and low-burden areas showed a downward trend (AAPC was −1.3%, −8.0% and −6.1% respectively), in which the turning point of time trend change in high- and medium-burden areas was 2018, showing an upward trend from 2012 to 2018 and a rapid downward trend from 2018 to 2021, see Table 1 and Figure 2.
 |
Table 1 Temporal Epidemic Trend of PTB Registered Incidence from 2012 to 2021 |
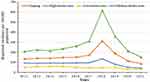 |
Figure 2 Temporal trend of PTB registered incidence in Xinjiang from 2012 to 2021. |
Analysis of Policy Intervention Effect Based on ITS
The registered incidence of PTB in Xinjiang did not increase significantly before the implementation of the “Xinjiang Model” policy (β1=0.056, P>0.05); one month after the implementation of the policy, registered incidence increased by 13.806/100,000 (P<0.001), indicating that the policy intervention had an immediate effect on increasing registered incidence; the long-term effect after the implementation of the policy was that registered incidence shows a downward trend (β3<0, P<0.001), with a monthly decrease of 0.690/100,000 (β1+β3=−0.690), indicating that the policy intervention has a long-term effect of reducing registered incidence.
In high-, medium- and low-burden areas of PTB, there was no significant upward trend before the implementation of the “Xinjiang model” policy, and the long-term effect of the policy was that registered incidence decreased (β3<0, P<0.001), with monthly decreases of 1.460/100,000, 0.227/100,000, and 0.064/100,000 per month, respectively, 0.064/100,000 per month, respectively. One month after the implementation of the policy, registered incidence in high-burden areas increased significantly by 31.578/100,000 (P<0.001), while there was no significant increase in medium- and low-burden areas (P>0.05), as shown in Table 2 and Figure 3.
 |
Table 2 Intervention Effect of “Xinjiang Model” Policy Based on Single-Group ITS |
 |
Figure 3 Fitting trend of PTB registered incidence in Xinjiang based on ITS. (A) Xinjiang. (B) High-burden areas. (C) Medium-burden areas. (D) Low-burden areas. |
Comparison of Policy Intervention Effects Among Different Areas
The difference in the upward trend before policy implementation was not statistically significant in high-burden compared with low-burden areas; one month after policy implementation, the increase in registered incidence was significantly higher in high-burden than in low-burden areas (β6= 30.919, P<0.001); and the long-term effect of the policy was a greater decline in registered incidence in high-burden than in low-burden areas (β7= −1.548, P<0.001). The difference in the upward trend before policy implementation was not statistically significant, as well as the difference in the amount of increase in registered incidence one month after policy implementation (P=0.358) in medium-burden compared with low-burden areas; the long-term effect of the policy was a greater decrease in registered incidence in medium-burden than in low-burden areas (β7=−0.194, P<0.001), as shown in Table 3 and Figure 4.
 |
Table 3 Comparison of Policy Intervention Effects Among Different Areas Based on CITS |
 |
Figure 4 Fitting trend of PTB registered incidence in Xinjiang based on CITS. (A) High-burden areas. (B) Medium-burden areas. |
Discussion
Xinjiang is located in northwestern China and is relatively lagging in socioeconomic development, especially in the four prefectures of southern Xinjiang. The socio-economic level has a strong influence on the prevalence of tuberculosis,16 and regions with slow economic development often suffer from a lack of financial resources for health, relatively few qualified medical personnel, weak public health infrastructure, and relatively poor health and nutritional status of the population, all of which are associated with a high-burden of tuberculosis. In this study, according to the spatial distribution of PTB epidemic in Xinjiang, the areas with high registered incidence are mainly distributed in the four prefectures of southern Xinjiang, which is related to the low level of economic development and low accessibility of medical services in the four prefectures of southern Xinjiang.
The study has shown that from 2012 to 2021, the turning point of the registered incidence in Xinjiang and four prefectures of southern Xinjiang occurred in 2018, with an upward trend before 2018 and a downward trend after 2018. It can be assumed that the implementation of the “Xinjiang model” policy can change the trend of registered incidence in Xinjiang and four prefectures of southern Xinjiang, and that there is a correlation between policy interventions and registered incidence. The comparison of PTB change trend between the four prefectures in southern Xinjiang and the level of the whole Xinjiang shows that the rising speed of registered incidence before the implementation of the policy and the decreasing speed after the implementation of the policy are greater than the level of the whole Xinjiang. Therefore, the “Xinjiang Model” policy shows more significant effect in the areas with high tuberculosis burden.
Further ITS analysis showed that there was a dynamic causal relationship between the policy intervention and registered incidence, that is, the policy intervention caused a temporary increase in the registered incidence, but its long-term effect was a downward trend. The brief increase in registered incidence could be explained by the “Xinjiang model” policy involving active case finding (ACF), which led to more PTB patients being detected through screening of key populations and chest X-ray examination in national health examination. Especially in some areas with high tuberculosis burden, the per capita disposable income of residents is low, and some tuberculosis patients have symptoms but do not seek medical treatment due to economic reasons. Therefore, implementing ACF can increase the number of tuberculosis patients. A systematic review of community-based tuberculosis active case finding showed that ACF was effective in initially increasing tuberculosis detection and that, if provided with adequate intensity and coverage, ACF could reduce tuberculosis prevalence in the community.17
The long-term trend of decreasing registered incidence may be related to many factors. Due to the infectious characteristics of PTB, the implementation of ACF strategy enables more tuberculosis patients to be detected or detected early, reducing the delay of patient diagnosis and reducing the possibility of community transmission,18 that is, under the continuous development of the policy, the registered incidence shows a downward trend. In addition, in the “Xinjiang model” policy development, the four prefectures of southern Xinjiang implemented full-course hospitalization isolation treatment or infectious period hospitalization isolation treatment for PTB patients, on the one hand, the patients received standardized and effective treatment, improved the success rate of treatment for tuberculosis patients; on the other hand, PTB patients hospitalized isolation treatment, to a certain extent blocked the transmission route of tuberculosis. During the treatment period, each patient is provided with a nutritious breakfast to help improve the patient’s immunity and body resistance. Studies have shown that undernutrition is associated with increased incidence and severity of tuberculosis, worse treatment outcomes, and increased mortality.19,20 Therefore, giving patients nutritional support during treatment reduces the likelihood of developing unfavorable treatment outcomes. It should also be noted that the government has implemented a medical security policy of 90% reimbursement of hospitalization expenses and 100% reimbursement of outpatient examination expenses, effectively alleviating the economic burden of tuberculosis patients and improving patients’ medical compliance and medication compliance.
Currently, strategies to identify PTB patients and ensure timely and correct treatment have been shown to be effective in settings with high tuberculosis burden,21 reducing transmission by eliminating infected cases from the population before more transmission occurs. Considering that the effectiveness of ACF depends on the prevalence of infection in the population,22 and that ACF strategies are most cost-effective in populations at high risk of PTB,18,23,24 it is recommended that, once the incidence of tuberculosis in Xinjiang has fallen to a certain level, mass screening for tuberculosis should no longer be conducted, but rather focus on ACF strategies in populations at high risk of tuberculosis infection.
In the ITS analysis, data were collected at multiple time points before and after the intervention to understand changes and trends in outcome variables before and after the intervention and to analyze whether the intervention was associated with outcomes outside of any previous long-term trends. ITS is suitable for assessing the effectiveness of population-level public health interventions,25 including studies assessing the relationship between the implementation of alcohol control policies in Lithuania and all-cause mortality in adults,26 the effectiveness of community-based Directly Observed Treatment Short-course strategies on tuberculosis treatment success rates,27 and the effectiveness and safety of telemedicine in prenatal care during the COVID-19 pandemic.28 The “Xinjiang Model” policy is a population-oriented public health policy, and the study uses ITS to analyze the changes and trends of registered incidence before and after intervention, which can quantitatively evaluate the dynamic effect of the “Xinjiang Model” policy on the registered incidence of tuberculosis in Xinjiang, and vividly demonstrate the immediate and long-term effects of policy intervention.
However, there are some limitations to this study. Xinjiang and the four prefectures of southern Xinjiang were taken as the policy intervention areas, respectively, and no control area was set. The ITS analysis could not exclude the influence of time-dependent factors on the analysis results.29 In addition, the outcome variable concerned in the study was the registered incidence from 2012 to 2021, during which the diagnostic criteria for tuberculosis would have changed to some extent, would lead to a decrease in comparability of the registered incidence at different time points. There is also a non-negligible impact of the COVID-19 global pandemic on the implementation of the “Xinjiang model” policy, which involves active screening and treatment of tuberculosis. In 2020, Xinjiang implemented social isolation measures for about two months. During this period, active screening could not be carried out normally and tuberculosis patients in infectious period could not be hospitalized for isolation treatment. However, tuberculosis workers took a series of remedial measures, such as calling to inform tuberculosis patients to avoid close contact with family members, ventilation and disinfection measures in the room, and treatment drugs were delivered to patients’ homes by staff. The rapid resumption of hospitalization of patients after the end of social isolation and the orderly active screening of tuberculosis by medical institutions have weakened the impact of COVID-19 on the implementation of the “Xinjiang Model” policy to a certain extent.
Conclusions
The “Xinjiang Model” policy has achieved remarkable results in tuberculosis prevention and treatment in Xinjiang. The long-term effect of decreasing registered incidence of tuberculosis shows that the implementation of the policy can effectively control the spread of tuberculosis and has significant public health value. The effectiveness of the “Xinjiang Model” policy suggests that active mass tuberculosis screening and timely treatment of patients in areas with high tuberculosis burden are critical to curbing the tuberculosis epidemic. The “Xinjiang Model” policy has certain reference value for other countries with high tuberculosis burden. Combating tuberculosis is a long-term and arduous task, and given the long-term benefits of the “Xinjiang Model” policy in tuberculosis control, it requires sustained and high-quality implementation. In this process, further improvement and enhancement are needed, with emphasis on improving the quality of tuberculosis treatment, tuberculosis case management, and monitoring and supervision of tuberculosis services.
Abbreviations
PTB, Pulmonary tuberculosis; ITS, Interrupted time series; ACF, Active case finding.
Data Sharing Statement
The datasets used and analyzed during the current study are not publicly available, but they are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Xinjiang Medical University (XJYKDXR20230303016) and was conducted in accordance with the guiding principles of the Declaration of Helsinki. The ethics committee waived the need for written informed consent provided by participants due to the retrospective nature of this study and the fact that the data did not contain personal information about the patients. Patient data was used only for this study and was kept strictly confidential.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the Xinjiang Uygur Autonomous Region Postgraduate Scientific Research Innovation Project (grant number XJ2023G188), and the National Natural Science Foundation of China (grant number 82060622).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. World Health Organization. Global tuberculosis report 2022; 2022: 68. Available from: https://www.who.int/teams/global-tuberculosis-programme/TB-reports/global-tuberculosis-report-2022.
2. Ming-zhe W, Le W, Aierken Z, Fei H, Xin-qi W. Epidemiological characteristics of common patients with pulmonary tuberculosis in Xinjiang from 2011 to 2020. J Prevent Med Inform. 2022;38(10):1334–1339+1345.
3. Abudula Z, Xinqi W, Zhen Z, et al. Epidemiological characteristics of pulmonary tuberculosis in Xinjiang, 2015–2019. Dis Surveillance. 2021;36(11):1138–1141. doi:10.3784/jbjc.202107010375
4. Xin-qi W, Yipaer A, Sen-lu W, Nian-qiang L, Zhen Z, Xi-hong Y. Preliminary discussion and prospect of mode of tuberculosis prevention and control in Xinjiang. Bull Dis Contr Prevent. 2022;37(02):11–16. doi:10.13215/j.cnki.jbyfkztb.2112021
5. Miller CJ, Smith SN, Pugatch M. Experimental and quasi-experimental designs in implementation research. Psychiatry Res. 2020;283:112452. doi:10.1016/j.psychres.2019.06.027
6. Ewusie JE, Soobiah C, Blondal E, Beyene J, Thabane L, Hamid JS. Methods, applications and challenges in the analysis of interrupted time series data: a scoping review. J Multidiscip Healthc. 2020;13:411–423. doi:10.2147/jmdh.S241085
7. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions. a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi:10.1093/ije/dyw098
8. Degli Esposti M, Spreckelsen T, Gasparrini A, et al. Can synthetic controls improve causal inference in interrupted time series evaluations of public health interventions? Int J Epidemiol. 2020;49(6):2010–2020. doi:10.1093/ije/dyaa152
9. Long Q, Guo L, Jiang W, Huan S, Tang S. Ending tuberculosis in China: health system challenges. Lancet Public Health. 2021;6(12):e948–e953. doi:10.1016/s2468-2667(21)00203-6
10. Si-qing Z. Joinpoint regression model and its application in epidemic trend analysis of infectious diseases Chinese. J Health Statist. 2019;36(5):787–791.
11. Zhang Y, Liu J, Han X, et al. Long-term trends in the burden of inflammatory bowel disease in China over three decades: a joinpoint regression and age-period-cohort analysis based on GBD 2019. Front Public Health. 2022;10:994619. doi:10.3389/fpubh.2022.994619
12. Xiao H, Augusto O, Wagenaar BH. Reflection on modern methods: a common error in the segmented regression parameterization of interrupted time-series analyses. Int J Epidemiol. 2021;50(3):1011–1015. doi:10.1093/ije/dyaa148
13. Jiang H, Feng X, Lange S, Tran A, Manthey J, Rehm J. Estimating effects of health policy interventions using interrupted time-series analyses: a simulation study. BMC Med Res Methodol. 2022;22(1):235. doi:10.1186/s12874-022-01716-4
14. Linden A. Challenges to validity in single-group interrupted time series analysis. J Eval Clin Pract. 2017;23(2):413–418. doi:10.1111/jep.12638
15. Turner SL, Forbes AB, Karahalios A, Taljaard M, McKenzie JE. Evaluation of statistical methods used in the analysis of interrupted time series studies: a simulation study. BMC Med Res Methodol. 2021;21(1):181. doi:10.1186/s12874-021-01364-0
16. He X, Cao M, Mahapatra T, et al. Burden of tuberculosis in Xinjiang between 2011 and 2015: a surveillance data-based study. PLoS One. 2017;12(11):e0187592. doi:10.1371/journal.pone.0187592
17. Burke RM, Nliwasa M, Feasey HRA, et al. Community-based active case-finding interventions for tuberculosis: a systematic review. Lancet Public Health. 2021;6(5):e283–e299. doi:10.1016/s2468-2667(21)00033-5
18. Bohlbro AS, Hvingelby VS, Rudolf F, Wejse C, Patsche CB. Active case-finding of tuberculosis in general populations and at-risk groups: a systematic review and meta-analysis. Eur Respir J. 2021;58(4):2100090. doi:10.1183/13993003.00090-2021
19. Sinha P, Lönnroth K, Bhargava A, et al. Food for thought: addressing undernutrition to end tuberculosis. Lancet Infect Dis. 2021;21(10):e318–e325. doi:10.1016/s1473-3099(20)30792-1
20. Ockenga J, Fuhse K, Chatterjee S, et al. Tuberculosis and malnutrition: the European perspective. Clin Nutr. 2023;42(4):486–492. doi:10.1016/j.clnu.2023.01.016
21. Yuen CM, Amanullah F, Dharmadhikari A, et al. Turning off the tap: stopping tuberculosis transmission through active case-finding and prompt effective treatment. Lancet. 2015;386(10010):2334–2343. doi:10.1016/s0140-6736(15)00322-0
22. Mugwagwa T, Stagg HR, Abubakar I, White PJ. Comparing different technologies for active TB case-finding among the homeless: a transmission-dynamic modelling study. Sci Rep. 2018;8(1):1433. doi:10.1038/s41598-018-19757-5
23. Chen JO, Qiu YB, Rueda ZV, et al. Role of community-based active case finding in screening tuberculosis in Yunnan province of China. Infect Dis Poverty. 2019;8(1):92. doi:10.1186/s40249-019-0602-0
24. André E, Rusumba O, Evans CA, et al. Patient-led active tuberculosis case-finding in the Democratic Republic of the Congo. Bull World Health Organ. 2018;96(8):522–530. doi:10.2471/blt.17.203968
25. Xiaohan X, Chunquan O. An introduction to interrupted time series design in evaluating the effect of public health interventions and its application. Chin J Health Statist. 2023;40(1):41–44. doi:10.11783/j.issn.1002-3674.2023.01.009
26. Štelemėkas M, Manthey J, Badaras R, et al. Alcohol control policy measures and all-cause mortality in Lithuania: an interrupted time-series analysis. Addiction. 2021;116(10):2673–2684. doi:10.1111/add.15470
27. Kibuule D, Rennie TW, Ruswa N, Mavhunga F, Verbeeck RK. Effectiveness of community-based DOTS strategy on tuberculosis treatment success rates in Namibia. Int J Tuberculosis Lung Dis. 2019;23(4):441–449. doi:10.5588/ijtld.17.0785
28. Palmer KR, Tanner M, Davies-Tuck M, et al. Widespread implementation of a low-cost telehealth service in the delivery of antenatal care during the COVID-19 pandemic: an interrupted time-series analysis. Lancet. 2021;398(10294):41–52. doi:10.1016/s0140-6736(21)00668-1
29. Sørup S, Englund H, Laake I, et al. Revaccination with measles-mumps-rubella vaccine and hospitalization for infection in Denmark and Sweden – an interrupted time-series analysis. Vaccine. 2022;40(11):1583–1593. doi:10.1016/j.vaccine.2021.01.028
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




