Back to Journals » Journal of Pain Research » Volume 15
Interspinous Process Devices Do Not Reduce Intervertebral Foramina and Discs Heights on Adjacent Segments
Authors Krakowiak M, Rulewska N, Rudaś M, Broda M, Sabramowicz M, Jaremko A , Leki K , Sokal P
Received 15 January 2022
Accepted for publication 13 June 2022
Published 14 July 2022 Volume 2022:15 Pages 1971—1982
DOI https://doi.org/10.2147/JPR.S356898
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Krishnan Chakravarthy
Mateusz Krakowiak,1 Natalia Rulewska,2 Marcin Rudaś,1 Maciej Broda,1 Michał Sabramowicz,1 Andrzej Jaremko,1 Krzysztof Leki,3 Paweł Sokal1
1Department of Neurosurgery and Neurology, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland; 2Students’ Scientific Circle at the Department of Neurosurgery, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland; 3Centre for Statistical Analysis, Nicolaus Copernicus University, Toruń, Poland
Correspondence: Paweł Sokal, Department of Neurosurgery and Neurology, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland, Tel/Fax +48 523655505, Email [email protected]
Aim: Interspinous process device (IPD) placement is an attractive treatment option for lumbar spinal and foraminal stenosis. The goal of the treatment is to release the stress on facets joints as well as decompress the nerve roots by enlarging the intervertebral foramina and narrowed canal recesses.
Purpose: To evaluate possible structural changes in the lumbar spine after implantation of an IPD on operated and adjacent segments.
Patients and Methods: Twenty-two patients were enrolled in the study. Preoperative MRI scans of the lumbar spine evaluated recess and foraminal stenosis prior to the application of an IPD. CT exams were performed and morphometric measurements were made to assess the size of intervertebral foramina after implantation on the operated and adjacent segments.
Results: Statistically significant enlargements in diameter and surface area of the intervertebral foramen were seen at the operating level. On the right and left sides, foraminal enlargement after the procedure was 1 mm in diameter. The average enlargement of the foramina surface area at the level of implantation was 10 mm2. The median interspinous distance was significantly enlarged by 3.5 mm. No significant changes in adjacent segments were observed. Clinical improvement was confirmed by the Oswestry Disability Index (ODI) and visual analog scale (VAS). Preoperative disability was reduced (mean ODI from 70.5 (12.25) to 49.5 (23.75)), as well as back pain (mean VAS from 8.0 (1.7) to 4.4 (2.6)) and pain in lower limbs (mean VAS from 7.4 (1.9) to 3.8 (2.9)).
Conclusion: Decompression surgery using an IPD is effective in the treatment of lumbar foraminal and canal stenosis. It provides relief of symptoms in short-term observation through enlargement of intervertebral foramina and decompression of neural roots. It reduces overload of facet joints of the operated segment and does not decrease the size of the intervertebral foramina and disc heights of adjacent segments.
Keywords: interspinous device, low lumbar back pain, lumbar decompression, spinal canal stenosis, foraminal stenosis
Introduction
Spinal degenerative disease constantly progresses throughout life and is accelerated by a sedentary lifestyle and bad nutritional habits.1 Overload of lumbar spine segments leads to hypertrophy of vertebral facets and thickening of the yellow ligament, causing narrowing of the spinal canal and subsequently intermittent neurogenic claudication. Degeneration of the spine during the restabilization phase produces both foraminal and spinal canal stenoses. The narrowed spinal canal and general spondylosis are the source of neurogenic claudication, radicular and low back pain.2 Surgical techniques for spinal canal decompression are aimed to decompress subsequent nerve roots within the vertebral recesses and foramina. These procedures have demonstrated effectiveness in reducing chronic pain and claudication.2
One possible alternative to mild-to-moderate lumbar stenosis is the use of an interspinous process device (IPD), known as a “Knowles plug” which was first introduced by Knowles in 1950.3 Existing evidence supports the application of IPDs as an acceptable strategy in the management of patients with lumbar spondylosis and stenosis.4 Compared to decompression and fusion, IPD surgery has better pain relief and higher improvements in disability with a lower incidence of complications.5
Biomechanically, IPDs ensure dynamic stabilization and prevent the protrusion of the yellow ligament into the spinal canal during extension.2 Various manufactured IPDs have different degrees of range of motion restriction and stress over the disc at the instrumented level.6
Even though IPDs have been used in many centers around the world, there is still no clear consensus or protocol to use them as a first-choice treatment for foraminal stenosis. However, several reports have demonstrated an improvement in pain symptoms after IPD application.4 Comparison of IPD and decompressive surgery based on five randomized clinical trials revealed similar clinical outcomes in both groups with slightly higher reoperation rate in IPDs7.
When analyzing the available literature on IPD application, there are a very few articles addressing the morphometric changes in the lumbar spine after implantation of the IPD.2,8,9 The main aim of this study was to evaluate the changes in spinal morphometric parameters after the surgery. The subtle changes in the foramina surface area and height of intervertebral discs might directly contribute to the decompression of nerve roots at the operated level and progression of adjacent segment degeneration.
Materials and Methods
The presented study was carried out with the approval of the bioethics committee and the informed consent of patients. Twenty-two patients who underwent lumbar spinal decompression and IPD implantation for foraminal, central or lateral recess stenosis were enrolled in the study. Qualification for the procedure was based on preoperative MRI findings and correlating clinical symptoms. Spinal decompression consisted of central flavectomy or fenestration with medial facetectomy and foraminotomy. Stand-alone IPD technique was performed in 7 cases.
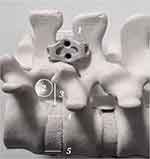
With regard to IPDs, two PEEK dynamic spacers (Pioneer Surgical Technology Inc., Marquette, USA): Back Jack (16 patients) and Back Fuse (6 patients) were used. The majority of patients: 18 received implants at the L4/L5 level, 2 patients at the L3/L4 level, and 2 patients at both the L4/L5 and L5/S1 segments (Table 1). The day after the surgical procedure, a CT scan of the lumbar spine was performed. Measurements of the diameter and surface area of bilateral intervertebral foramina, as well as the anterior and posterior disc space heights, the spinal canal diameter, and the interspinous distance, were taken on sagittal projections of preoperative MRI and postoperative CT using standard tools in Radiant DICOM software (Medixant, Poznań, Poland) (as length of a certain line segment) before and after the procedure (Figures 1 and 2).
 |
Table 1 Characteristics of Operated Patients and Performed Implantations |
 |
Figure 1 Morphometric data: 54 measurements taken for 22 patients, in total 1188 measured parameters. |
The results of these measurements were compared and the changes were analyzed statistically.
All general parameters were measured for the adjacent segments with the exclusion of two cases in which the implants were placed at the L5-S1 level making it impossible to take these measurements from the level below.
Patients after surgery required only standard doses of non-steroidal anti-inflammatory drugs (NSAIDs) and were successfully upright on the day after surgery.
Four weeks after the patient’s discharge, the outcome of the surgical treatment was assessed using the visual analog scale (VAS) and Oswestry Disability Index (ODI).
Statistical analysis was carried out with the use of PS IMAGO PRO v. 7 software based on the IBM SPSS Statistics v. 27 analytical engine. Data visualizations were made with Python v. 3.8.10, using the modules Seaborn v. 0.11.1 and Matplotlib v. 3.4.2. The normality of the distribution of differences was tested with the Shapiro–Wilk test. In the case of the non-normality of the distribution, the significance of the differences was verified using the non-parametric exact Wilcoxon signed-rank test. Otherwise, the paired Student’s t-test was used. As the collective null hypothesis about the effect of IPD on the spinal morphometric parameters was tested, the Bonferroni correction for multiple testing was applied.10
Results
Statistical analysis showed that the distribution of differences after and before surgery was not normal for all features except the interspinous distance at the IPD level. Additionally, the sample size was not large (22 observations). Therefore, for the consistency of the results, in all cases the non-parametric exact Wilcoxon signed rank test was performed with Bonferroni correction (Table 2).
 |
Table 2 Before and After Surgery Comparisons |
Wilcoxon signed-rank test was used to analyze the rest of the data with a Bonferroni correction due to multiple comparison factors. This statistical tool showed a statistically significant difference (p-value less than 0.05) in:
- Surface area of the spinal canal before and after surgery at the level of the IPD implantation. The median of the differences in spinal canal surface area at the level of IPD implantation was 10 mm2.
- Foraminal surface area before and after surgery bilaterally at the level of implantation. On the right and left sides, the median enlargement in foramina surface area at the level of implantation was 10 mm2 (Figure 3A and B).
- The right side of foramina diameter before and after surgery at the level of implantation. The median diameter of the right-side foramina at the level of implantation increased by 1 mm (Figure 4).
- Interspinous distance at the level of implantation. The interspinous distance was significantly increased with a median increase of 3.5 mm (Figure 5).
 |
Figure 4 Median diameter of the right intervertebral foramen on the operated and adjacent segments. |
 |
Figure 5 Median interspinous distance on the operated and adjacent levels before and after surgery. |
Values that showed statistically significant differences before and after surgery were as follows:
No significant differences before and after surgery were observed in:
- Foraminal height and surface area at the levels above and below.
- Surface area and width of the spinal canal at the levels above and below.
- Anterior and posterior intervertebral disc height above and below the implant level. At the operating level, the anterior disc height decreased, while the posterior disc height increased but not significantly (Figure 6A and B).
Analysis of clinical outcomes demonstrated statistical differences for Visual Analogue Scale (VAS) in low back pain and lower limb pain as well as in ODI scores. Two patients from 22 were lost in follow-up (Table 3) (Figure 7).
 |
Table 3 Intensity of Pain in VAS and Degree of Disability in ODI in Patients Before and 4 Weeks After Surgery |
 |
Figure 7 Low back pain (LBP) and lower limbs pain before and after surgical procedure in visual analogue scale (VAS). |
Discussion
In the presented study, the analysis of morphometric measurements before and after the surgical placement of an IPD was conducted. In all 22 patients who participated in the study, MRI before and CT after the procedure were performed. Analysis of the results demonstrated a repeated pattern of enlargement of the nerve root foramen bilaterally at the level of implantation that was found to be statistically significant. Our results are in concordance with those of a study conducted on frozen cadaveric lumbar spines, which demonstrated opening of the intervertebral foramen on the operating level and non-significant modification of the foraminal surface areas of adjacent levels.9
On follow-up observations, a significant reduction in pain radiating to the lower limbs was observed in the majority of participants, confirming previous findings. It was reported in a meta-analysis of four randomized controlled trials comparing decompression surgery to IPD surgery that the use of an implant was an attractive option for the treatment of lumbar stenosis resulting in alleviation of annoying symptoms; however, the IPD group had a higher reoperation rate.4 In another meta-analysis, patients undergoing IPD surgery required reoperation more frequently, but the postoperative complication rates and perioperative blood loss were lower in comparison to decompression surgery.11 Overall, the interspinous spacer devices effect in pain and disability reduction without advantage over decompression alone, but the quality of scientific evidence varies from low to high.12
According to the presented data, IPDs might directly contribute to a decrease in low back pain by decreasing excessive loads on the facet joints. Improvements in lower back pain, as seen by decreases in the VAS scale as reported by patients after surgery, may be due to reduced loads on the facet joints. The interspinous distance was significantly increased by the IPD which resulted in reduced facet joint loads. The mean enlargement of this distance was 3.5 mm. The reduction in radicular symptoms was mainly due to the enlargement of foraminal size and decompression of recesses.
Although the median enlargement of 1 mm in diameter and 10 mm2 in surface area might not seem like a significant improvement, this additional space was sufficient to improve the clinical state of patients. In most patients, decompression with medial facetectomy was performed resulting in an enlargement of the spinal canal. There might be concerns about the adjacent levels since the enlargement of foramina at one level might cause compression of the nerve roots at the level above and/or below. Observed enlargement of the intervertebral foramen at the operated level was caused by distraction of the facets due to implantation of an IPD. No reduction in diameter size nor surface area of adjacent intervertebral foramina was noted. This observation leads to the conclusion that an IPD does not compress the upper and lower roots within the foramina. These findings are comparable with previously published results of the study by Richards et al.2 Another study found that radiological symptoms from adjacent segment disease were attributed to lower disc height, but in our study, we did not observe a reduction in these parameters at levels above and below the surgery.13 Significant reduction of the anterior height of the disc at the operated level is observed. Considering the true representation of the above-mentioned model, extensive pressure on the disc space is caused by the anterior column.
In the in vitro study by Hirsch et al, none of the four IPDs placed at the L4-L5 level changed the upper foramen surface area, while the lower foramen surface area in the two types of IPD examined decreased in extension.9
In several reports, an iatrogenic atraumatic fracture of the spinous process is described as the “sandwich phenomenon” was associated with double-level IPD surgeries.14 In our group, no cases of this phenomenon were encountered, although in 1 case a double-level IPD implantation was performed.
Minimal invasion is the main target for both surgeons and patients. Avoidance of tissue traumatization is desirable since it should always be the main goal of surgery to preserve as many healthy tissues as possible. The approach using IPD provides lower pain, lower hospitalization costs, and moderate cost-effectiveness. Minimally invasive procedures should be effective and have satisfactory results for patients as well as improvements in measurable data.
There are multiple alternative approaches to treat foraminal stenosis, such as a technically simple decompression with the removal of the facet joints. While there are more complicated approaches in cases of foraminal stenosis, where lateral access has to be performed through the facet joint requiring an additional fusion of the segment (intervertebral implant, transpedicular screws, or both). The placement of the implant into the intervertebral space might be a standalone technique sufficient to enlarge vertebral foramina.15 This approach implicates the necessity to stabilize the motor segment with transpedicular screws but expands the range of surgical procedures as well as enhances the traumatization of surrounding tissues. Apart from open lumbar surgeries, microscopic decompression surgery utilizing endoscopic techniques has been used with satisfactory clinical outcomes.16 The endoscopic approach is a minimally invasive procedure with minimal scar tissue formation and a lower risk of postoperative instability but has a significant learning curve and requires special tools.
Both factors improve the cost-effectiveness of these procedures by shortening the length of hospital stay and lowering the doses of analgesic medication required. Overall, the clinical outcome in both methods is similar.17
In our center, microscopic methods of lumbar decompression along with implantation of an IPD are the most frequent procedures for lumbar decompression surgery, although endoscopic and microscopic decompressive techniques are not seldom used.
Limitations
One of the objections that might be raised is the fact that an MRI scan was performed before the procedure and compared to a CT scan after IPD placement. The accuracy of MRI and CT scan measurements is comparable according to multiple studies not only for neuronal foramina and spinal canal diameter but also for more CT occult soft tissue structures like ligaments and nerve roots.18
Patients enrolled in our study observed reductions in pain 4 weeks after IPD implantation. Nevertheless, over a longer time frame, some may develop degenerative changes, which could translate into increased pain as observed by Spallone et al.19 Therefore, it seems reasonable to explore this topic furthermore on a larger group of patients in order to establish reliable protocols for lumbar foraminal stenosis management with the use of IPD as proposed by Anderson et al.20
Conclusions
Application of an IPD standalone or augmented by decompressive surgery is effective in the treatment of lumbar foraminal and canal stenosis. It provides relief of symptoms in short-term observation through enlargement of intervertebral foramina and decompression of neural roots in recesses and foramina. It reduces the overload of facet joints of the operated segment and does not decrease the size of the intervertebral foramina and disc heights of adjacent segments.
Compliance with Ethics Guideline
Bioethical committee at Nicolaus Copernicus University reviewed and approved the study protocol (No. 156/2020). The present work was implemented under the guidance of the principles of the Declaration of Helsinki.
Acknowledgments
We thank Dr Joanna Karłowska-Pik for advice on statistical analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest.
References
1. Maurer E, Klinger C, Lorbeer R, et al. Long-term effect of physical inactivity on thoracic and lumbar disc degeneration—an MRI-based analysis of 385 individuals from the general population. Spine J. 2020;20(9):1386–1396. doi:10.1016/j.spinee.2020.04.016
2. Richards JC, Majumdar S, Lindsey DP, Beaupré GS, Yerby SA. The treatment mechanism of an interspinous process implant for lumbar neurogenic intermittent claudication. Spine. 2005;30(7):744–749. doi:10.1097/01.brs.0000157483.28505.e3
3. Lau AC, Wang MY. Interspinous devices: an overview and review of the evidence. Contemp Spine Surg. 2018;19(7):1–8. doi:10.1097/01.css.0000540057.58094.49
4. Zhao X-W, Ma J-X, Ma X-L. Interspinous process devices (IPD) alone versus decompression surgery for lumbar spinal stenosis (LSS): a systematic review and meta-analysis of randomized controlled trials. Int J Surg. 2017;39:57–64. doi:10.1016/j.ijsu.2017.01.074
5. Zhang Y, Lu D, Ji W, et al. Which is the most effective treatment for lumbar spinal stenosis: decompression, fusion, or interspinous process device? A Bayesian network meta-analysis. J Orthop Transl. 2021;26(2020):45–53. doi:10.1016/j.jot.2020.07.003
6. Lo HJ, Chen HM, Kuo YJ, Yang SW, Farouk O. Effect of different designs of interspinous process devices on the instrumented and adjacent levels after double-level lumbar decompression surgery: a finite element analysis. PLoS One. 2020;15(12):1–13. doi:10.1371/journal.pone.0244571
7. Poetscher AW, Gentil AF, Ferretti M, Lenza M, Bekelis K. Interspinous process devices for treatment of degenerative lumbar spine stenosis: a systematic review and meta-analysis. PLoS One. 2018;13(7):1–19. doi:10.1371/journal.pone.0199623
8. Nachanakian A, El Helou A, Alaywan M. The interspinous spacer: a new posterior dynamic stabilization concept for prevention of adjacent segment disease. Adv Orthop. 2013;2013:1–7. doi:10.1155/2013/637362
9. Hirsch C, Breque C, Ragot S, et al. Biomechanical study of dynamic changes in L4-L5 foramen surface area in flexion and extension after implantation of four interspinous process devices. Orthop Traumatol Surg Res. 2015;101(2):215–219. doi:10.1016/j.otsr.2014.11.016
10. Armstrong RA. When to use the Bonferroni correction. Ophthalmic Physiol Opt. 2014;34(5):502–508. doi:10.1111/opo.12131
11. Hong P, Liu Y, Li H. Comparison of the efficacy and safety between interspinous process distraction device and open decompression surgery in treating lumbar spinal stenosis: a meta analysis. J Investig Surg. 2015;28(1):40–49. doi:10.3109/08941939.2014.932474
12. Machado GC, Ferreira PH, Yoo RI, et al. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;2016:11. doi:10.1002/14651858.CD012421
13. Kim KR, Lee CK, Kim IS. Efficacy of interspinous device on adjacent segment degeneration after single level posterior lumbar interbody fusion: a minimum 2-year follow-up. Br J Neurosurg. 2020:1–9. doi:10.1080/02688697.2020.1812516
14. Barbagallo GMV, Corbino LA, Olindo G, Foti P, Albanese V, Signorelli F. The “sandwich phenomenon”: a rare complication in adjacent, double-level X-stop surgery: report of three cases and review of the literature. Spine. 2010;35(3):96–100. doi:10.1097/BRS.0b013e3181c83820
15. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ ATP, LLIF and ALIF. J Spine Surg. 2015;1(1):2–18. doi:10.3978/j.issn.2414-469X.2015.10.05
16. Ruetten S, Komp M. Endoscopic lumbar decompression. Neurosurg Clin N Am. 2020;31(1):25–32. doi:10.1016/j.nec.2019.08.003
17. Chen T, Zhou G, Chen Z, Yao X, Liu D. Biportal endoscopic decompression vs. microscopic decompression for lumbar canal stenosis: a systematic review and meta‑analysis. Exp Ther Med. 2020;20(3):2743–2751. doi:10.3892/etm.2020.9001
18. Kostelic J, Haughton M, Sether L. Proximal imaging, lumbar CT, and spinal anatomic nerves in axial sections’. Radiology. 1992;183:239–241. doi:10.1148/radiology.183.1.1549679
19. Spallone A, Lavorato L, Belvisi D. Long-term results for the bacjac interspinous device in lumbar spine degenerative disease. J Neurol Surg. 2018;80(1):3–7. doi:10.1055/s-0038-1641180
20. Anderson DB, Ferreira ML, Harris IA, et al. SUcceSS, SUrgery for spinal stenosis: protocol of a randomised, placebo-controlled trial. BMJ Open. 2019;9(2):1–9. doi:10.1136/bmjopen-2018-024944
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.