Back to Journals » International Journal of General Medicine » Volume 14
Intention to Use and Its Predictors Towards Preconception Care Use Among Reproductive Age Women in Southwest Ethiopia, 2020: Application of Theory of Planned Behavior (TPB)
Authors Setegn M
Received 14 June 2021
Accepted for publication 2 August 2021
Published 16 August 2021 Volume 2021:14 Pages 4567—4577
DOI https://doi.org/10.2147/IJGM.S324242
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Melsew Setegn
Department of Reproductive Health and Human Nutrition, School of Public Health, College of Medicine and Health Science, Mizan-Tepi University, Mizan-Aman, Ethiopia
Correspondence: Melsew Setegn Email [email protected]
Background: Preconception care should be given in universal manner worldwide by manifesto of WHO. The government of Ethiopia gives the emphasis to maternal and child health but the progress of its improvement is too slow. Maternal health services especially before pregnancy is the unreached agenda in Ethiopia. Therefore, there is limited evidence on the intention to preconception care and its determinants in southwest Ethiopia. So, the aim of this study to determine the intention to use and its predictors of preconception care use among reproductive age women.
Methods: A community-based cross-sectional study was conducted in southwest Ethiopia. Systematically selected 427 reproductive age women were involved in this study. Face-to-face interview was used to collect the data by trained data collectors. The collected data was entered into EpiData version 3.1 and then exported to SPSS version 25 for further analysis. Multiple linear regression analysis was conducted to identify predictors to intention to use preconception care. P-value less than 5% was considered to indicate significant association. The standardized β-coefficient was presented as measure of association following a multivariable linear regression analysis.
Results: The response rate of the study was 98.13%. The mean age of respondents in the study was 34.21[± 6.21] years. Nearly twenty (19.8%) respondents had used preconception care previously. The attitude (β =0.320, p=0.0418), subjective norm (β =0.344, p< 0.001), perceived behavioral control (β=0.512, p< 0.001), indirect subjective norm (β =− 0.108, p=0.002) and age of respondents (β =0.046, p=0.020) were predictors of intention to use preconception care.
Conclusion: Intention to use preconception care is a multiplicative effect of attitude, subjective norm, perceived behavioral control and indirect subjective norm. Age is the only socio-demographic variables associated to intention.
Keywords: prenatal care, preconception care, maternal health, theory of planned behavior
Introduction
Preconception care is the establishment of preventive, promotive or curative health before conception occurs. The period before conception and interconception is included under preconception care which is categorized as distal and proximal preconception care.1 Currently preconception care should be delivered by every health care providers at every time.2 There are three components of preconception care; wellness check, counseling, and intervention. Preconception care risk assessment includes reproductive history, environmental hazard and toxin, a medication that are known teratogen, nutrition, folic acid intake, weight management, family history, chronic disease and mental illness. Growing with good health is the right of all babies and children. Being physically, psychologically and socially healthy is the right of all individuals.1
One of the essential elements of preconception care is reproductive life plan.3 Preconception care gives a chance for both clinicians and respective women to improve birth outcome and it motivates the women to see other life planning opportunity.3 Preconception care also reduces too early pregnancy, unplanned pregnancy and pregnancy that are too close. It could contribute to each dimension of health and risk factors, to reducing maternal and childhood mortality. WHO recommended everywhere like folic acid supplementation, tobacco cessation advice, family planning services and interventions for limited resource countries.1
The government of Ethiopia gives emphasis for the continuum of care through expanding health extension program, health developmental army, expanding health post, giving iron and folate supplementation, making the maternity service free of charge and construction of health institution are some of the interventions of the government together with non-government organizations.4–6 Despite all the above efforts, the proportion of PCC use is almost nil.7–9 Even though WHO and CDC highly recommended preconception care to improve maternal and child health,1,2,10 no study was done on intention to use preconception care in southwest Ethiopia. During reviewing literatures, different factors were identified like having formal education, being multiparous, having planning pregnancy, being elder, prior adverse birth outcomes, and pre-existing chronic health conditions.7,8,11
Theory planned behavior (TPB) is used in different aspects of health activities to intervene, assess, evaluate programs, and projects. It predicts the individual involvement in specific time and place for specific behaviour, that is all behaviors are self-control.12 The TPB has been found to be the most tightfisted model in predicting intentions and various behavioral outcomes.13 TPB has 39% variance in intention and 27% variance in behavior but in other study 32% variance in behavioral intention.14,15 The intention of maternal health services use were highly and effectively predicted by theory of planned behavior (TPB).16–18 So far, TPB has been used in predicting the changes in intention in relation to behaviors such as pre-pregnancy care, prenatal care, and receiving pre-pregnancy counseling.19,20 In the previous literature, the predictors of intention were perceived behavioral control,21–27 subjective norm,16,22,23,25,26,28 attitude16,22,24,25,27,29,30 and sociodemographic factors. Despite the above studies, intention to use preconception care and its predictors in southwest Ethiopia is not studied yet. Thus, this study applied TPB because of: the first reason is women’s decision-making is the result of the process of decision making reflects people’s values and attitudes. The second reason is to act in a specific direction requires that people behave in line with their motivation and attitudes. In addition, participating in PCC services is a result of external factors that control or enhance the behavior. The decision of the individuals is affected by their own motivation and attitude. In addition to those performing a behavior is influenced by factors from external environment which influence the individual’s confidence. The confidence that overcome external factors is also covered by theory of planned behavior. Therefore, the aim of this study was to determine intention to use and its predictors towards preconception care among reproductive age women in southwest Ethiopia.
Methods
Study Design, Period and Area
A community based cross-sectional study design was conducted in Mizan-Aman town, Bench-Sheko Zone, and Southwest Ethiopia from April 16 to May 26, 2020. The town is located 561 KM Southwest of Addis Ababa. The town divided into 5 kebeles that has a total area of 142.71 km with an average elevation of 2840m above sea level. There is one teaching hospital, one health center and five health posts, one University and one college under the government.
Study Participants
All reproductive age women who lived in Mizan-Aman town were the source and study population. All reproductive age group women who lived in Mizan-Aman town for 6 months and above were included under the study.
Sampling Technique and Procedure
The sample size was determined by using single population proportion formula with the assumption of 95% confidence level, 5% margin of error and the proportion of behavioral intention towards preconception care use was taken 50% since there is no previous study conducted in the area.
Where; n=sample size
Zα/2=95% confidence interval (1.96)
P=50% proportion of behavioral intention towards preconception care use
d=5% margin of error
Based on the above assumption
n= (1.96)2*0.5(1–0.5) (⁄0.04)2≈384, 10% was added as non-response rate as a contingency rate for the non-response rate. So, the final sample size was 427. A multistage sampling technique was used, in the first stage proportional allocation to the five kebele was done. In the second stage systematic random sampling was applied to select the actual study participant of the study. To reach the study unit systematic random sampling technique was used in the Kebeles. The first house was selected randomly from 1–24 household and then every 24th house for all kebele was asked (Figure 1). In case of more than one eligible woman being encountered in the selected household, a lottery method was used.
 |
Figure 1 Schematic presentation of sampling procedure for a study conducted in Mizan-A man town, Bench-Sheko Zone, Southwest Ethiopia, 2020. Abbreviation: HHs, Households. |
Study Variables
Dependent variable: intention to use preconception care
Independent variables:
- Socio-demographic characteristics: age, religion, ethnicity, marital status, residency, education status, occupation
- Reproductive health related factors: ANC, PNC, FP, planning to pregnancy
- Knowledge towards preconception care
- TPB constructs direct attitude, subjective norm, perceived behavioral control, indirect subjective norm and indirect attitude.
Data Collection Process
Pretested interviewer-administered structured questionnaire was adapted from TPB constructs and different literature.12,16,31,32 Before the data collection tool was prepared an elicitation study was done by conducting 18 in-depth interviews in the target population on locally available salient behavioral, normative belief and control belief on preconception care. In addition, a face-to-face interview on 20 persons was conducted to elicit the salient beliefs using open-ended questions. The questionnaire was developed based on TPB questionnaire development guidelines, different literature and modified based on the result of elicitation study. In addition to constructs of TPB, the questionnaire covered sociodemographic information, knowledge about preconception care and reproductive history. Finally, the overall developed questionnaire was pretested on 5% of sample size before actual data collection on Tsebejaji town. Four Bachelor of science degree holder health professionals collected data and two health officers supervised the data collection process. Two days training was given to the data collectors and supervisors on the data collection tools and procedures by principal investigators.
Data Management and Analysis
Each questionnaires were checked for completeness and consistency of data at the end of each data collection day. Data were coded, edited and checked for clarity, consistency, and completeness up to the end of the data collection period. The data were coded and entered into EpiData version 3.1 then exported to SPSS version 25.0 for further analysis. Descriptive statistics were presented in mean and standard deviation for numerical variables and frequency and percentage for the categorical variables. The normality of the data was checked before calculating the mean with its standard deviation. The normality of the data was checked before the analysis of mean with standard deviation. The normality was checked by SPSS main bar (analysis-descriptive statistics-explore-normality plot) with drawing histogram with normality curve, P-P plot and stem and leaf. All normality tests indicated that the data is normally distributed. Correlation analysis was used to examine the association between intention and constructs of theory of planned behavior as bivariate analysis. The variables with the p<0.25 in bivariate analysis were qualified for multiple linear regression analysis. Multiple linear regression analysis was conducted to identify independent predictors of intention to use preconception care. P-value < 0.05 was considered to indicate significant association. The standardized β-coefficient were presented as a measure of association following a multivariable linear regression analysis.
Data Quality Control
The questionnaire was prepared first in English and then translated to Amharic and was re-translated back to English by another person to ensure its consistency and accuracy. The questionnaire was pre-tested by data collectors on people who did not participate in the actual data collection. Training was given for the data collectors and supervisors on data collection process, approach and with additional training for the supervisors for data quality management. The supervisors for the clarity, completeness, and proper procedure of data collection closely supervised data collection. The questionnaire after data collection was also checked by the principal investigator for its clarity and completeness. Double data entry was done in separated data sheet to improve data quality. Health education, gynecologist, epidemiology, health promotion and reproductive experts evaluate the content validity of the tool by compressive review. The quantitative content validity of the questionnaire were done by content validity index (CVI). Five experts determined the content validity index by asking the necessity and relevance of each item using 4 point Likert scale. The CVI of each item and each construct were calculated (CVI≥0.81) which indicated that acceptable range. Reliability test was done to ensure construct validity. The test of reliability was at acceptable range. The Cronbach’s alpha was at acceptable range (0.665–0.875).
Measurements and Scoring
Intention to use preconception care: was measured by using four items. Responses ranged from “strongly disagree” (1) to “strongly agree” (5). Composite score was done by summing up all the items then new composite scores of the intention were created.
Direct attitude: was measured by 5 items semantic differential scales (SDS) measuring about the benefit/outcome of using PCC services in the next 3 months on bipolar adjectives.
Four Likert scale items measured direct subjective norm.
Direct measure of PBC was measured by using four items on bipolar differential scales. High composite score shows strong perceived ability or less difficulty to have preconception care services. The higher scores indicate a greater value for all measured TPB constructs towards the use of preconception care services (Table 1).
 |
Table 1 Summary of Measurements and Scoring of Direct and Belief Based Measures of Constructs of TPB of the Study Conducted in Mizan Aman Town Southwest Ethiopia, 2020 |
Knowledge about preconception care use were assessed using 17 items with ”Yes” or “No” response format.33 All items were scored as continuous variables and pulled together where the mean score was computed for further analysis.
Past experience of PCC: seventeen item was used to ask respondents whether they have ever practiced preconception care by using yes/no approach. Greater than one component use before pregnancy is considered as good practiced.11
Operational Definition
Intention to preconception care: assessed by asking the participants the statement with responses strongly disagree, disagree, neutral, agree and strongly agree. High scores in this study shows a high intention to perform preconception care.34
Preconception Care: It provides preventive, promotive or curative health and related interventions before the women become pregnant. During preconception care, interventions such as nutritional deficiencies and disorders, vaccine-preventable infections, tobacco use, environmental risks, early pregnancies, unwanted pregnancies and rapid succession pregnancies, sexually transmitted infections.35 A modification of any situation before pregnancy on the aspect of preconception care components. Preconception care components in this study is assessed such as whether or not they have intention screened for HIV/AIDS, screened for STI, screened for hypertension, screened for DM, screened for blood group, screened for hepatitis b, screened for anemia, screened for obesity, took folic acid, took tetanus vaccine, took iron/ferrous, prepare diet from different cereals, took extra meal, consulting health workers for advice, reduced/stopped of drinking alcohol, reduced/stopped of smoking, reduced/ stopped of chat chewing, stopped using family planning and husband screening for any infection/diseases.
Results
Socio-Demographic Characteristics
From the total of 427 participants, 419 respondents completed the interview producing 98.13% response rate. The age of the respondents ranged between 17 to 48 years with mean age of 34.21 ± 6.21 years and nearly half, 205 (48.9%) of the respondents were in age category 35–49 years. More than half, 222 (53.0%), were orthodox religion followers, followed by protestant accounting for 147 (35.1%). About 161 (38.4%) of the respondents were Bench ethnic groups. Majority of the respondents, 321 (76.6%), were married. Most, 302 (72.1%), of respondents were housewife. Most, 284 (67.8%), of the respondents did not attend formal education (Table 2).
 |
Table 2 Socio-Demographic Characteristics of Respondents in Mizan-Aman Town, Southwest Ethiopia 2017 (N= 419) |
Health Facility Related Factors
Majority, 333 (79.5%), of the study participants were multiparous. Most, 275 (65.1%), of the respondents had experienced 2–4 pregnancies. About 174 (41.5%) of the study participants planned their pregnancy. About 63.0% of the respondents used family planning. More than half (57.5%) of the respondents attended at least one ANC visit in their nearest pregnancy (Table 3).
 |
Table 3 Reproductive Health Characteristics of Reproductive Age Women in Mizan-Aman Town, Bench-Sheko Zone, Southwest Ethiopia, 2020 (n=419) |
Source of Information, Knowledge and Practice of PCC
Out of 331 (79.0%) respondents who have heard about preconception care, 147 (44.4%) heard during other service use in health facility and 139 (42.0%) heard from health workers and others heard from mass media, 12 (3.6%), family/friend, 24 (7.3%), school, 7(2.1%) and neighbor, 2 (0.6%). Regarding knowledge about preconception care, 121 (36.6%), 124 (37.2%), 111 (33.5%), 99 (29.9%),110 (33.3%) and 116 (35.0%) knew about screening to STI, screening to hypertension, screening of diabetes mellitus, taking folic acid before pregnancy, taking Iron/ferrous and taking good nutrition, respectively. For each knowledge item, scores were summed and mean score was computed. Accordingly, only 157 (47.4%) of the respondents were answered above the mean and considered as knowledgeable. Preconception care practice was low in the area, as only 83 (19.8%) had good practice for it.
Direct and Indirect Measure of TPB Constructs
The mean score of direct attitude, subjective norm and PBC were [11.51 (SD=3.7)], [11.54 (SD=4.04)] and [11.51 (SD=3.98)] respectively and intention with mean score of [11.59 (SD=3.97)] (Table 4).
 |
Table 4 Descriptive Statistics for Components of Theory of Planned Behavior and Intention for Reproductive Age Women in Mizan-Aman Town Southwest Ethiopia (N= 419) |
Relationship Between Intention, Socio-Demographic and Reproductive Factors and Measures of TPB Constructs
To identify the associated factors all necessary analysis was done. While age is the only sociodemographic factor identified as predictor of intention to use preconception care. All the direct measures of TPB were significantly and positively correlated with each other and with their respective indirect measures. In the current study all direct and indirect TPB components were significantly and positively correlated, which is important for further analysis (Table 5).
 |
Table 5 Pearson’s Correlation Between Intention, Direct and Indirect Measure of TPB of the Current Study (N= 419) |
Independent Predictors of Intention to Use Preconception Care
Prediction of behavioral intention to preconception care use was conducted with all direct constructs of TPB and variables that were significant in bivariate analysis. These are: attitude, subjective norms, perceived behavioral control, knowledge towards preconception care, age, past behavioral experience and time to reach health facility were entered to multivariate linear regression analysis. In multivariable linear regression analysis five predictor variables were identified. The standardized regression coefficients, PBC was found to be the best factor (β= 0.512, p<0.001) followed by subjective norm (β= 0.344, p<0.001). This indicates a unit positive change in women’s perception of ability to control over circumstances that inhibit them from using preconception care services will increase intention to use preconception care by 51.2% keeping other conditions constant. Women who perceive significant others will approve of their using preconception care services will have 34.4% higher intention to use preconception care than their counterparts. A unit-positive change in women’s attitude toward the advantage associated with the use of preconception care services will increase the individual’s intention to use it by 32.0% provided that all the other factors kept unvaried. Similarly, a unit-positive change in women’s age associated with the use of preconception care services will increase the individual’s intention to use preconception care services by 4.6% provided that all the other factors kept constant. In this study, indirect subjective norm is negatively predicted with the intention to use preconception care (β= −0.108, p=0.002). In this study, age the women was found to be the least factor associated to intention to preconception care utilization (β= 0.046, p=0.020) (Table 6).
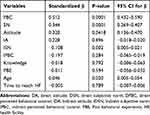 |
Table 6 Independent Predictors to Behavioral Intention to Preconception Care Service Utilization, Mizan-Aman Town, Southern Ethiopia, 2020 (N= 419) |
Discussion
The aim of this study was to determine intention to use preconception care services and its predictors among reproductive age women. In the present study perceived behavioral control is the strongest predictor of the intention to use preconception care. A unite in change to control the circumstance that hindered from using preconception care which increase the intention to use by 51.2% by holding other covariates constant. This is consistent with a study conducted in southern Ethiopia on intention to cervical cancer screening,22 in Jimma zone which conducted on intention to use maternity waiting home,23 the study conducted in Harari region, Ethiopia,24 north showa zone, Ethiopia,25 the study conducted in Nairobi,26 and other study conducted in Bench Maji zone.27 This implies that those women who had resources and opportunities to the behaviour (preconception care use) expressed greater intention towards it. In addition, this indicates that authorizing the women against challenges like access of health care provider, transportation, waiting time to take services, and supply of Iron, folic acid may improve the utilization of preconception care. As such interventions involved on challenges towards behavior is an effect on the increment of preconception care utilization. This implies that removing the barriers and increase the facilitators of performing the preconception care could improve the intention of the women to use preconception care. The implication of this finding is that responsible body should work on the barriers that hinder on maternal health services.
However, perceived behavioral control is not the predictor of intention to use pre-pregnancy care in a study conducted in Iran16 and intention to voluntary HIV counseling and testing (VCT) among health professionals in Jimma zone.29 Since the concept, perceived behavioral control is very similar to Bandura’s self-efficacy and similar results were obtained in studies examining self-efficacy.20,36 This could be due to other factors which also affect the intention of the women to perform the behavior. This could be due to the theory of planned behavior prediction being not fully hundred percent. In addition, this could be due to the importance of determining the intention of behavior vary from population to population and behavior to behavior. Specifically the study conducted in Jimma zone done on health professionals who were more likely to have awareness on the behavior since intention is self-instruction to perform behavior. This implies that interventions designed based on the population of the study participants and the behavior that intervene on it.
The second strongest predictor of intention to use preconception care in this study is subjective norm of the individual study participants. A unite change of approving the behavior by other (family, husband, health care provider, friends, neighbor) will increase the intention to use by 34.4% by keeping other variables constant. This implies that those women who more strongly recognized that their important others expected them to have preconception care services expressed stronger intention. As such, considering interventions addressing normative dimension of the women could have an effect on preconception care utilization. This is consistent with the previous study conducted in Ethiopia,22,23 north showa zone, Amhara region, Ethiopia,25 the study conducted in Norwegian adult,28 the study conducted in Nairobi,26 and Iran16 which showed that subjective norm is a predictor of intention to perform the behaviour and in the study conducted in Harari region, Ethiopia24 subjective norm is the strongest predictor of intention to use. The intention to perform a behavior is the function of attitude, subjective norm and perceived behavioral control according to Ajzen theory of planned behavior.32 This could be due to the study being conducted on the same target population since intention to perform a behavior is population specific. This implies that knowing the importance of others could improve the intention to perform preconception care. Therefore, the interventions on clarifying the importance of a behavior on parents, husbands and friends is important to improve the women’s intention to perform preconception care.
In the present study, attitude was predictor of women’s intention to perform preconception care in the near/far future. This implies that those women who know the importance and usefulness of preconception care expressed more intention towards preconception care utilization than others. So, intervention on preconception care usefulness and awareness creation on it improves women’s intention towards the behavior. This finding is consistent with study conducted in Ethiopia,22,27,29 Harari region, western Ethiopia,24 North showa Amhara region Ethiopia,25 other study conducted somewhere30 and Iran16 which indicated that attitude is the predictor of intention to perform the behavior. This could be due to intention is the cumulative effect of those constructs on the intention towards the behavior. While, in the other study conducted attitude cannot predict mammography behavior.37 This could be accredited to the difference in the context/circumstances under which the behavior is to take place and the place where the study was conducted. This could be due to variance in theory of planned behavior interpersonal intention. The other predictor of intention to the behavior is indirect subjective norm. This implies that the women that had no comply of others and give recognition by someone increase the intention to the behavior. The other and the only socio demographic predictor of intention to preconception care utilization is age of individual women. While in the previous literature socio-demographic factors were not associated with intention to act the behavior. This could be due to the difference in the population. Since intention change as time goes by which the mean that it is simply as a function of time.12 This indicated that intention to perform a behavior has an effect of other factors in addition of the constructs of theory of planned behavior.
In this study, only 19.8% of the women reported they had practiced good preconception care in previous time. However, it’s higher than the study conducted in Debre Birhan, Adet, West Shoa and northern Ethiopia.7–9,11 This might be due to difference in socio economic status of study participants and difference in sample size of the study. Although this study has addressed pressing public health issues by applying effective health behavioral theory, it has a few limitations. The cross sectional nature of the study does not show cause effect relations among these psychographic variables. In addition, the social desirability bias may affect the precision of the data through its influence on individuals’ attitude and intention.
Conclusions
Overall, the study revealed that the behavioral intention to use preconception care services was a function of attitude, subjective norm and PBC. The perceived behavioral control was found to be the strongest predictor of the intention to behavior. Age is the only socio-demographic variable, which was significantly associated to intention to perform a preconception care. Health behavior change interventions should focus women’s autonomy and empowering them to develop ability against social norms that could compete with the use of preconception care services and build an attitude that support the behavior. Study employing interventional design should be conducted to see the translation of behavioral intention to the actual behavior to see causal effect relation. The author recommended that intervening hindering factors and importance of others could improve the intention to use preconception care.
Abbreviations
HDA, Health development army; HEW, Health extension workers; PBC, Perceived behavioral control; PBE, Past behavior experience; PCC, Preconception care; SPSS, Statistical package for social sciences; TPB, Theory of planned behavior; WHO, World Health Organization.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from Institutional Review Board (IRB) of Jimma University, Institute of health, Faculty of public health. The study was conducted in accordance with the Declaration of Helsinki. Support letter was obtained from department of population and family health. The necessary permission was obtained from Mizan-Aman town health office. Anonymity of the participants was kept by not writing their name and individuals information will not be disclosed to other third party. Informed verbal consent was obtained from each study participant for the women above 18 years old and informed consent was obtained from parents and/or husband for the women under 18 years old and the Jimma University ethical committee approved this consent.
Acknowledgments
I would like to express our deepest heartfelt thanks to Jimma University for allowing conducting of this study. I would like to thank Mizan-Aman town Health Bureau and health extension workers on which the study conduct for their positive responses to facilitate this study. My special thanks also go to study participants, data collectors and supervisors.
Disclosure
The author declares that they have no competing interests in this work.
References
1. Organization WH. Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity. In: Christiansen C, Mason VC-M, editors. Geneva, Swizerland: WHO; 2012.
2. Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and Health Care—United States: report of the CDC/ATSDR preconception care work group and the select panel on preconception care. Morbidity Mortality Weekly Rep. 2006;55(6):
3. Files JA, Frey KA, David PS, et al. Developing a reproductive life plan. J Midwifery Women’s Health. 2011;56(5):468–474. doi:10.1111/j.1542-2011.2011.00048.x
4. Health FMo. National Newborn and Child Survival Strategy Document Brief Summary 2015/16-2019/20. Addis Ababa: FMOH; 2015.
5. Emiru AA, Alene GD, Debelew GT. Women’s retention on the continuum of maternal care pathway in west Gojjam zone, Ethiopia: multilevel analysis. BMC Pregnancy Childbirth. 2020;20:1–14. doi:10.1186/s12884-020-02953-5
6. Sarwar MF, Sarwar MH, Sarwar M. Understanding some of the best practices for discipline of health education to the public on the sphere. Int J Innovation Res Educ Sci. 2015;2(1):1–4.
7. Asresu TT, Hailu D, Girmay B, et al. Mothers’ utilization and associated factors in preconception care in northern Ethiopia: a community based cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):347. doi:10.1186/s12884-019-2478-1
8. Goshu Y, Liyeh T, Simegn Ayele A. Preconception care utilization and its associated factors among pregnant women in Adet, North-Western Ethiopia (Implication of reproductive health). J Women’s Health Care. 2018;7(445):2167. doi:10.4172/2167-0420.1000445
9. Fekene D, Woldeyes BS, Erena MM. Knowledge, uptake of preconception care and associated factors among reproductive age group women in west shoa zone, Ethiopia, 2018. BMC Women’s Health. 2019;20(1):1–8.
10. Mason E, Chandra-Mouli V, Baltag V, et al. Preconception care: advancing from ‘important to do and can be done’to ‘is being done and is making a difference’. Reprod Health. 2014;11(S3):S8. doi:10.1186/1742-4755-11-S3-S8
11. Demisse TL, Aliyu SA, Kitila SB, et al. Utilization of preconception care and associated factors among reproductive age group women in Debre Birhan town, North Shewa, Ethiopia. Reprod Health. 2019;16(1):96. doi:10.1186/s12978-019-0758-x
12. Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. Action Control. Springer; 1985:11–39.
13. Sparks P. Theory of planned behaviour and health behaviour. Predicting Health Behav. 2005;2:170.
14. Armitage CJ, Conner M. Efficacy of the theory of planned behaviour: a meta‐analytic review. Br J Soc Psychol. 2001;40(4):471–499. doi:10.1348/014466601164939
15. Øygard L, Rise J. Predicting the intention to eat healthier food among young adults. Health Educ Res. 1996;11(4):453–461. doi:10.1093/her/11.4.453
16. Zamani O, Tabatabaei SVA, Mohseni M, et al. Factors affecting pre-pregnancy care among women based on the theory of planned behavior in Larestan, Iran, in 2016. J Public Health (Bangkok). 2019;25:1–9.
17. Austvoll‐Dahlgren A, Falk RS, Helseth S. Cognitive factors predicting intentions to search for health information: an application of the theory of planned behaviour. Health Info Libr J. 2012;29(4):296–308. doi:10.1111/hir.12006
18. Grønhøj A, Bech‐Larsen T, Chan K, et al. Using theory of planned behavior to predict healthy eating among Danish adolescents. Health Educ. 2013.
19. Natan MB, Ashkenazi M, Masarwe S. Intentions of muslim Arab women in Israel to attend prenatal classes. Women and Birth. 2016;29(1):e8–e12. doi:10.1016/j.wombi.2015.07.009
20. Komiti A, Jackson HJ, Nankervis A, et al. An investigation of psycho-social factors associated with the uptake of pre-pregnancy care in Australian women with type 1 and type 2 diabetes. J Psycho Obstetrics Gynecol. 2013;34(2):75–81. doi:10.3109/0167482X.2013.793664
21. Åstrøm AN, Nasir EF. Predicting intention to treat HIV-infected patients among Tanzanian and Sudanese medical and dental students using the theory of planned behaviour-a cross sectional study. BMC Health Serv Res. 2009;9(1):213. doi:10.1186/1472-6963-9-213
22. Abamecha F, Tena A, Kiros G. Psychographic predictors of intention to use cervical cancer screening services among women attending maternal and child health services in Southern Ethiopia: the theory of planned behavior (TPB) perspective. BMC Public Health. 2019;19(1):434. doi:10.1186/s12889-019-6745-x
23. Endalew GB, Gebretsadik LA, Gizaw AT. Intention to use maternity waiting home among pregnant women in Jimma District, Southwest Ethiopia. Glob J Med Res. 2017;16(6):1–9.
24. Omer S, Haidar J. Applicability of the theory of planned behavior in predicting intended use of voluntary HIV counseling and testing services among teachers of Harari Region, Ethiopia. Ethiop J Health Develop. 2010;24:2. doi:10.4314/ejhd.v24i2.62957
25. Assefa N, Haidar J. The utility of theory of planned behavior in predicting consistent condom use intention of HIV patients on ART in North Shoa Zone health facilities, Ethiopia, 2011. Ethiop J Health Develop. 2013;27(1):40–47.
26. Koyio LN, Kikwilu E, Mulder J, et al. Attitudes, subjective norms, and intention to perform routine oral examination for oropharyngeal candidiasis as perceived by primary health‐care providers in Nairobi Province. J Public Health Dent. 2013;73(2):127–134. doi:10.1111/j.1752-7325.2012.00353.x
27. Nigussie T, Yaekob R, Geremew M, et al. Predictors of intention to use maternity waiting home among pregnant women in Bench Maji Zone, Southwest Ethiopia using the theory of planned behavior. Int J Women’s Health. 2020;12:901. doi:10.2147/IJWH.S267730
28. Åstrøm AN, Lie SA, Gülcan F. Applying the theory of planned behavior to self-report dental attendance in Norwegian adults through structural equation modelling approach. BMC Oral Health. 2018;18(1):1–10. doi:10.1186/s12903-018-0558-7
29. Abamecha F, Godesso A, Girma E. Intention to voluntary HIV counseling and testing (VCT) among health professionals in Jimma zone, Ethiopia: the theory of planned behavior (TPB) perspective. BMC Public Health. 2013;13(1):140. doi:10.1186/1471-2458-13-140
30. Quick BL, Stephenson MT, Witte K, et al. An examination of antecedents to coal miners’ hearing protection behaviors: a test of the theory of planned behavior. J Safety Res. 2008;39(3):329–338. doi:10.1016/j.jsr.2008.02.032
31. Creanga AA, Odhiambo GA, Odera B, et al. Pregnant women’s intentions and subsequent behaviors regarding maternal and neonatal service utilization: results from a cohort study in Nyanza Province, Kenya. PLoS One. 2016;11(9):e0162017. doi:10.1371/journal.pone.0162017
32. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
33. Ayalew Y, Mulat A, Dile M, et al. Women’s knowledge and associated factors in preconception care in adet, west gojjam, northwest Ethiopia: a community based cross sectional study. Reprod Health. 2017;14(1):15. doi:10.1186/s12978-017-0279-4
34. Temel S, Birnie E, Sonneveld H, et al. Determinants of the intention of preconception care use: lessons from a multi-ethnic urban population in the Netherlands. Int J Public Health. 2013;58(2):295–304. doi:10.1007/s00038-012-0396-3
35. Dean SV, Mason EM, Howson CP, et al. Born too soon: care before and between pregnancy to prevent preterm births: from evidence to action. Reprod Health. 2013;10(S1):S3. doi:10.1186/1742-4755-10-S1-S3
36. Janz NK, Herman WH, Becker MP, et al. Diabetes and pregnancy: factors associated with seeking pre-conception care. Diabetes Care. 1995;18(2):157–165. doi:10.2337/diacare.18.2.157
37. Dezham S, Roozbahani N, Khorsandi M. Application of Theory of Planned Behavior in Predicting Screening Mammography in Housewives Over 40 Years. 2015.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

