Back to Journals » Advances in Medical Education and Practice » Volume 14
Integrating Virtual Teaching in a New Era of Medical Education: Lessons from a Neurology Course
Authors Kaplan T, Tarolli C, Doughty CT
Received 8 April 2023
Accepted for publication 23 August 2023
Published 11 October 2023 Volume 2023:14 Pages 1147—1156
DOI https://doi.org/10.2147/AMEP.S413816
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Md Anwarul Azim Majumder
Tamara Kaplan,1,2 Christopher Tarolli,3 Christopher T Doughty1,2
1Department of Neurology, Brigham and Women’s Hospital, Boston, MA, USA; 2Harvard Medical School, Boston, MA, USA; 3Department of Neurology and Center for Health + Technology, University of Rochester Medical Center, Rochester, NY, USA
Correspondence: Tamara Kaplan, Department of Neurology, Brigham and Women’s Hospital, Harvard Medical School Brigham Multiple Sclerosis Center, 60 Fenwood Road, Boston, MA, 02115, USA, Email [email protected]
Abstract: The COVID-19 pandemic has led to a sudden shift toward virtual learning in neurology education, which presents challenges for educators. However, virtual learning is here to stay for three key reasons: demand among students, ease of dissemination, and potential to improve educational quality. Despite challenges, educators can teach effectively using appropriate virtual tools and methods, with innovative approaches that will ultimately lead to sustained improvements in neurology education. Here, we aim to help educators effectively incorporate virtual instruction into their “new normal” by offering practical, evidence-based tips for balancing in-person and virtual learning, selecting the appropriate tools and methods for virtual teaching, and creating a supportive virtual learning environment. Using a systematic approach, educators can identify specific, achievable goals, determine the content’s scope, appropriate assessments, select appropriate teaching methods, and create the session schedule and materials. Here we described evidence-based strategies for best practices, developing virtual material, and creating the appropriate virtual learning environment.
Plain Language Summary: This paper reviews how the COVID-19 pandemic has made it necessary for medical educators to switch to virtual learning for neurology courses. Even though it presents challenges, virtual learning is important because students want it, it’s easy to disseminate, and it can improve the quality of education. Educators can learn how to use virtual tools and methods effectively by being innovative and making sustained improvements in neurology education. This paper offers practical tips based on evidence to help educators balance in-person and virtual learning, select appropriate tools and methods, and create a supportive virtual learning environment. By taking a systematic approach, educators can set achievable goals, decide what to teach, pick the best ways to teach it, and create a schedule and materials for the course.
Keywords: virtual learning, Learning Enviornment, Synchronous Learning, Asynchronous Learning, Curriculum
Introduction
Virtual learning platforms and technology have been widely adopted in higher education in recent decades with the dissemination of new teaching modalities such as the flipped classroom, massive open online courses, interactive virtual modules, and remote lectures. These methods can be used in addition to or instead of traditional in-person learning and have improved access for learners globally.1 Before the COVID-19 pandemic, adoption depended on the learning setting and acceptance from educators and students locally; implementation in neurologic education had been particularly slow.2
The COVID-19 pandemic caused a rapid shift toward virtual learning, with medical educators required to transform learning activities to virtual formats nearly overnight. This presented challenges in neurologic education at all levels (Table 1).3–5 Medical school neuroanatomy traditionally relies on cadaveric specimens, while clinical neurology training involves hands-on practice examining real patients. Virtual learning also carries the risk of feeling impersonal, as learners may feel isolated or unable to connect with faculty.6 This can exacerbate neurophobia among medical students and trainees. Despite these challenges, neurology can be taught effectively using appropriate virtual tools and methods,7 with novel and innovative approaches leading to sustained improvements in neurology education. In medical school courses, for example, remote instruction is similarly effective to in-person sessions and leads to equivalent knowledge acquisition and higher student satisfaction.8–10
 |
Table 1 Risks and Benefits of Virtual Learning |
Although we have shifted some activities back to the classroom, virtual learning is here to stay. There are three key reasons for this: 1) demand – research shows that students still prefer some virtual component;11 2) dissemination – virtual teaching expands the reach of educational activities with opportunities for interinstitutional collaboration and global education;1 and 3) quality – virtual formats and platforms can improve the educational quality of sessions.10 With careful consideration, virtual teaching can augment in-person instruction, enhance courses, and increase student engagement.12
Here, we aim to help educators effectively incorporate virtual instruction into their “new normal” by offering practical, evidence-based tips for balancing in-person and virtual learning, selecting the appropriate tools and methods for virtual teaching, and creating a supportive virtual learning environment.
Best Practices for Teaching Virtually
Virtual instruction can be asynchronous (eg pre-recorded lectures or online modules) or synchronous (eg teleconferencing or a virtual classroom). Asynchronous formats allow students to learn at their own pace, while synchronous formats occur in real-time and mimic traditional in-person sessions. Asynchronous formats can be used to introduce new material, typically as pre-work,13 while synchronous sessions are best suited to focus on interactive application of the material. Mixing asynchronous and synchronous formats can thus create more engaging and effective learner-centered experiences.14–16 Recent studies have highlighted the importance of utilizing multimodal, engaging, team-based learning to create successful neuroscience and neuroanatomy curriculum. For example, most students now prefer watching pre-recorded material over live, in-person lecture and generally prefer a “flipped-classroom” model.8,9
There are several pitfalls to avoid when utilizing virtual teaching (Table 2), and it is essential to understand the learner group to both select the appropriate amount and depth of asynchronous pre-work and to ensure a proper focus of synchronous activities. Medical students in a neuroscience course expect work outside classroom time and may be asked to watch concept videos to prepare for active learning during synchronous sessions. In contrast, residents must balance formal education with busy clinical responsibilities and may be more likely to complete shorter and more portable pre-work.
 |
Table 2 Key Strategies to Avoid Pitfalls in Virtual Teaching |
With creativity, most teaching formats can be carried out online. Chalk talks can be recreated using virtual whiteboards and annotation; tracing neuroanatomical pathways can use engaging online modules that allow learners to more easily visualize anatomic structures; and didactic patient interviews can be conducted virtually, offering benefits for both patient convenience and offering insights into their home living environment. When employed effectively, virtual tools such as polling and annotation encourage active learning,18 which promotes deeper understanding and retention.19–21 These can also encourage more universal participation by allowing students to respond anonymously and by whichever means they feel most comfortable.
Maximizing the Impact of Asynchronous Content
Many tools exist for curating and creating asynchronous (eg pre-recorded lectures or online modules) virtual content. Developing new asynchronous materials requires considerable time and energy to master new technology and adapt new teaching styles.22 The use of externally-created materials can reduce the effort in transitioning to virtual teaching, though it is essential to select materials that match the needs of learners. For those creating content themselves, simply recording a pre-existing 60-minute lecture is not recommended. It is better to divide the content into shorter 6–15 minute sessions, each focusing on 1–2 learning points, as viewing retention tends to decline over time.23 Recorded video tutorials using personal, engaging formats are most highly rated by preclinical learners.11,24 Students especially value multi-modal asynchronous options for neuroanatomy instruction, as properly designed materials can ease cognitive load when learning complex, 3D neuroanatomical structures.25–27
The success of the flipped classroom model critically depends on learners completing asynchronous pre-work. Assessing knowledge with tools like readiness assessment questions and community message boards can improve accountability and performance.13 In class, an instructor can additionally prompt learners to discuss the most challenging concepts (“muddiest point” exercise)13 and provide feedback. Flipped classroom models that utilize these strategies are associated with better learner performance.9
Have a Plan for Facilitating Student Participation During Synchronous Sessions
To minimize teleconferencing fatigue during virtual synchronous sessions, it is crucial to shorten session duration, actively engage learners, and establish ground rules for participation.28 For example, should learners raise their virtual “hand” or unmute to ask questions? During the initial transition to online learning during the pandemic, student participation decreased by 50%.21 To encourage participation, instructors can ask direct questions more often and allow more silence. These strategies are crucial for hybrid sessions with in-person and virtual attendees, as virtual participants may otherwise become silent observers or risk disrupting session flow.
Encouraging the use of the chat function is an effective way to increase participation in large groups, but there are limits.15,29 Given the challenges of monitoring the chat while teaching, it may be best to designate a teaching assistant to moderate and answer questions. Learners can also become distracted by the chat, contributing to teleconferencing fatigue. These strategies take time—course content may need to be curtailed accordingly compared to prior in-person sessions.
Use Specific Tools to Foster Student Engagement
Polling software can stimulate low-risk, anonymous, universal participation from learners.20 In hybrid sessions, the use of polling can also level the playing field between in-person and online participants, maximizing participation from both. Most polling programs allow participants to join from a smartphone, so in-person participants are not excluded.
In a virtual setting, teleconferencing software’s “annotation” function allows students to type text or draw directly on the shared screen or whiteboard as an alternative to chat. This encourages more advanced discussion than chat can offer, as students can anonymously affirm or disagree with each other’s annotations and answer questions directly.30 This also allows educators to focus on teaching material without dividing their attention between the chat and student comments (Figure 1).
Finally, breakout rooms can facilitate small-group discussions among students and facilitate case-based learning formats.31–34 Fixed small groups throughout a longitudinal course can build trust and comfort between learners, encouraging participation. “Warm-calling” breakout groups—pre-designating one or more group to report back to the class at large after discussion in breakout rooms—can also encourage participation from students who may be hesitant to speak up.
Creating Virtual Teaching Material
Once informed about the tools at their disposal, educators can begin to create virtual teaching material. Creating effective virtual teaching material should rely on a systematic approach, and educators should first identify concrete goals for their course or module.35 The optimal educational tools, assessments, and learning activities should flow naturally from there. Below, we highlight a five-step process based on the Understanding by Design framework.36 Table 3 demonstrates the application of this framework in developing a virtual learning activity.
 |
Table 3 Example of the Development of a Virtual Learning Program Focused on the Teleneurology for Neurology Residents, Using the 5-Step Framework |
Identify specific, achievable goals: Focusing on session goals first ensures alignment between learning activities and learner outcomes. This allows the educator to develop assessments and session content that are appropriately matched.
- Determine the scope of the content: This step matches the identified learning goals to the methods for content delivery and considers whether the content should be delivered virtually. This helps the educator adjust the scope to ensure the content is covered appropriately in the virtual learning environment, and initiates the process of selecting the learning methods.
- Determine which type(s) of assessment are most appropriate: Assessments can range from simple observation of participation to formal evaluation of knowledge or skills and should be matched to the session goals. Diagnostic assessments can be conducted as a part of pre-work and may allow educators to modify focus based on identified needs. In contrast, formative (for the benefit of the learner) or summative (for formal assessment of learning achievement) assessments can be conducted during or following a synchronous session to monitor learner progress and ensure goal achievement.
- Select Appropriate Teaching Methods: This step focuses on selecting asynchronous and synchronous methods to ensure alignment with session goals and assessments. Asynchronous formats allow students to learn at their own pace outside formal classroom time and are well suited to introduce new material, typically as pre-work. Synchronous formats occur in real-time and mimic traditional in-person sessions. Delivering a traditional lecture over synchronous, live teleconferencing makes it difficult for learners to sustain attention. Focusing instead on activities that promote synthesis of concepts and interactive application of the material is recommended. Table 4 outlines a framework for matching goals to teaching methods.
- Create the session schedule and teaching materials: The creation of the schedule starts with consideration of the timing and logical order of activities. In general, sessions should progress from passive to active methods, and from knowledge attainment and understanding to skill development and application. Once the schedule is developed, content can be selected and created, always focusing on how content achieves the identified goals.
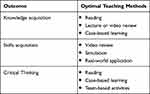 |
Table 4 Matching Teaching Methods to Desired Outcomes in the Creation of Virtual Teaching Activities |
Creating the Learning Environment
While we develop, create and deliver virtual teaching material, we must always consider the learning environment. Robust research across disciplines demonstrates that the learning environment significantly impacts student learning.15 A supportive environment promotes student well-being, empathy, professionalism, and academic success. In virtual learning, where face-to-face interactions are limited, educators must consider how to facilitate interactions between learners and between learners and educators.
Establish and Maintain a Personal Presence as an Instructor
Faculty presence is essential for developing a social connection and creating a sense of community in online learning environments.15,37 While this may be less important for CME courses for practicing physicians, social connections are crucial for students, especially those considering a career in neurology, as socialization of students into neurology may combat neurophobia.2 Similarly, post-graduate trainees need to feel confident in their sense of belonging and build professional relationships to advance their careers.
One way for faculty to build relationships with students and establish a positive classroom environment is through “non-instructor” talk, such as short, personal video introductions. Faculty introductory videos can be a valuable tool to help students connect with their instructors on a personal level. These videos can provide information about the faculty members’ clinical and research interests, as well as personal details. A high degree of faculty engagement positively influences student satisfaction and retention in online learning.15,37,38
Encourage Learner Feedback and Collaboration
Students should be able to give frequent, anonymous feedback and receive communication from faculty when changes are made or when changes are not possible. This helps learners feel heard and fosters collaboration between learners and teachers. The engagement of learners in creating course content can be particularly fruitful, as many may be eager to help with curriculum design and material development.
Facilitate 1:1 Time Between Faculty and Learners
In-person interactions between learners and teachers can be challenging to replicate in a virtual setting. However, there are methods to optimize student access to their virtual instructors (Table 4). Virtual formats can additionally increase inclusion and access to faculty for all learners.39 In a traditional in-person format, much of the exchange of questions and ideas occurs after class, for a select few, often one-on-one between an instructor and student. In a virtual format, a concurrent chat allows all students to ask questions and voice comments, and communication with the instructor may be more accessible, personal, and immediate.39
Respect Diversity – Foster an Inclusive and Equitable Learning Environment
Creating an inclusive learning environment involves acknowledging students’ personal circumstances. For example, a student may not be able to turn on their video due to technical issues or personal circumstances rather than a lack of engagement. However, virtual professional conference and course formats can potentially improve diversity and inclusion. Recent research found that with the transition to a virtual format, female attendance at virtual science and engineering meetings increased by 253%, and genderqueer scientist attendance jumped by 700%.40
Conclusion
The COVID-19 pandemic accelerated the adoption of virtual elements in medical education, presenting educators with both challenges and opportunities. Virtual learning is here to stay, driven by student demand, ease of dissemination, and the potential to enhance educational quality. With creativity, many curricular components can be adapted to a virtual format. When done well, such a transition can allow learners to approach material at their own pace and can promote more inclusive access to content and time with instructors. The careful use of tools like annotation, polling, and learner reactions can promote active learning and increase participation. These techniques can also enhance understanding and retention.18,30 By leveraging appropriate virtual tools and methods, educators can create a supportive and engaging virtual learning environment that complements in-person instruction, enhances learning experiences, and improves educational outcomes. A hybrid experience with an effective online learning community supplemented by live sessions may become the next gold standard in teaching trainees and students.
Suggestions for Further Reading
- Schaefer SM, Dominguez M, Moeller JJ. The Future of the Lecture in Neurology Education. Semin Neurol. Aug 2018;38(4):418–427. doi:10.1055/s-0038-1667042
- Reinholz DL, Stone-Johnstone A, White I, Sianez LM, Jr., Shah N. A Pandemic Crash Course: Learning to Teach Equitably in Synchronous Online Classes. CBE Life Sci Educ. Dec 2020;19(4):ar60. doi:10.1187/cbe.20–06-0126
- Anderson T. Teaching in an online learning context. Theory and practice of online learning. 2004;273
Key Points
- Virtual learning is here to stay for three key reasons: demand among students, ease of dissemination, and potential to improve educational quality.
- Mixing asynchronous and synchronous formats can create more engaging and effective learner-centered experiences. The success of using mixed modalities depends on learners completing pre-work and educators incorporating strategies like readiness assessment questions and community message boards.
- Virtual learning activities should be individualized to the needs of the learners, and many tools exist for curating and creating asynchronous virtual content.
- High-quality virtual curricula can be developed using a 5-step process that asks educators first to identify concrete goals, then develop assessments and learning activities.
- A supportive virtual learning environment plays a critical role in student learning.
Disclosure
Dr Christopher Doughty reports grants from Brigham Education Institute, clinical trial funding from Astra Zeneca, Scientific Advisory Board for UCB, royalties for CME courses from Oakstone and Haymarket, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Goodman J, Melkers J, Pallais A. Can online delivery increase access to education? Natl Bureau Econ Res Work Paper Ser. 2016;22754. doi:10.3386/w22754
2. Tarolli CG, Józefowicz RF. Managing Neurophobia: How Can We Meet the Current and Future Needs of Our Students? Thieme Medical Publishers; 2018:407–412.
3. Shell K, Holt E, Kington A, et al. Motivation to learn neuroanatomy by cadaveric dissection is correlated with academic performance. Clin Anatomy. 2020;33(1):128–135. doi:10.1002/ca.23500
4. Richards S. Faculty perception of student engagement in online anatomy laboratory courses during the COVID-19 pandemic. In: Medical Science Educator. Springer; 2023:1–16.
5. Yadala S, Nalleballe K, Sharma R, et al. Resident education during COVID-19 pandemic: effectiveness of virtual electroencephalogram learning. Cureus. 2020;12(10):e11094.
6. Jiang Z, Wu H, Cheng H, Wang W, Xie A, Fitzgerald SR. Twelve tips for teaching medical students online under COVID-19. Med Educ Online. 2021;26(1):1854066. doi:10.1080/10872981.2020.1854066
7. Stojan J, Haas M, Thammasitboon S, et al. Online learning developments in undergraduate medical education in response to the COVID-19 pandemic: a BEME systematic review: BEME Guide No. 69. Med Teach. 2022;44(2):109–129. doi:10.1080/0142159X.2021.1992373
8. Chen KS, Monrouxe L, Lu YH, et al. Academic outcomes of flipped classroom learning: a meta-analysis. Med Educ. 2018;52(9):910–924. doi:10.1111/medu.13616
9. Sandrone S, Berthaud JV, Carlson C, et al. Education research: flipped classroom in neurology: principles, practices, and perspectives. Neurology. 2019;93(1):e106–e111. doi:10.1212/wnl.0000000000007730
10. Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–212. doi:10.1097/00001888-200603000-00002
11. Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ open. 2020;10(11):e042378. doi:10.1136/bmjopen-2020-042378
12. Akcaoglu M, Lee E. Increasing social presence in online learning through small group discussions. Int Rev Res Open Distribut Learn. 2016;17(3). doi:10.19173/irrodl.v17i3.2293
13. Moffett J. Twelve tips for “flipping” the classroom. Med Teach. 2015;37(4):331–336. doi:10.3109/0142159X.2014.943710
14. Garrison DR, Anderson T, Archer W. Critical inquiry in a text-based environment: computer conferencing in higher education. Internet Higher Educ. 1999;2(2):87–105. doi:10.1016/S1096-7516(00)00016-6
15. Shochet RB, Colbert-Getz JM, Levine RB, Wright SM. Gauging events that influence students’ perceptions of the medical school learning environment: findings from one institution. Acad Med. 2013;88(2):246–252. doi:10.1097/ACM.0b013e31827bfa14
16. Schaefer SM, Dominguez M, Moeller JJ. The future of the lecture in neurology education. Semin Neurol. 2018;38(4):418–427. doi:10.1055/s-0038-1667042
17. Fuchs K. The difference between emergency remote teaching and e-learning. Frontiers. 2022;7:921332.
18. Stephenson CR, Yudkowsky R, Wittich CM, Cook DA. Learner engagement and teaching effectiveness in livestreamed versus in‐person CME. Med Edu. 2023;57(4):349–358. doi:10.1111/medu.14996
19. Stephenson CR, Bonnes SL, Sawatsky AP, et al. The relationship between learner engagement and teaching effectiveness: a novel assessment of student engagement in continuing medical education. BMC Med Educ. 2020;20(1):1–8. doi:10.1186/s12909-020-02331-x
20. Morawo A, Sun C, Lowden M. Enhancing engagement during live virtual learning using interactive quizzes. Med Educ. 2020;54(12):1188. doi:10.1111/medu.14253
21. Reinholz DL, Stone-Johnstone A, White I, Sianez LM, Shah N, Schussler E. A pandemic crash course: learning to teach equitably in synchronous online classes. CBE Life Sci Educ. 2020;19(4):ar60. doi:10.1187/cbe.20-06-0126
22. Regmi K, Jones L. A systematic review of the factors–enablers and barriers–affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):1–18. doi:10.1186/s12909-020-02007-6
23. Lau KV, Farooque P, Leydon G, Schwartz ML, Sadler RM, Moeller JJ. Using learning analytics to evaluate a video-based lecture series. Med Teach. 2018;40(1):91–98. doi:10.1080/0142159X.2017.1395001
24. Choe RC, Scuric Z, Eshkol E, et al. Student satisfaction and learning outcomes in asynchronous online lecture videos. CBE Life Sci Educ. 2019;18(4):ar55. doi:10.1187/cbe.18-08-0171
25. Javaid MA, Chakraborty S, Cryan JF, Schellekens H, Toulouse A. Understanding neurophobia: reasons behind impaired understanding and learning of neuroanatomy in cross-disciplinary healthcare students. Anat Sci Educ. 2018;11(1):81–93. doi:10.1002/ase.1711
26. Longhurst GJ, Stone DM, Dulohery K, Scully D, Campbell T, Smith CF. Strength, Weakness, Opportunity, Threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the Covid-19 pandemic. Anat Sci Educ. 2020;13(3):301–311. doi:10.1002/ase.1967
27. Newman HJ, Meyer AJ, Wilkinson TJ, Pather N, Carr SE. Technology enhanced neuroanatomy teaching techniques: a focused BEME systematic review of current evidence: BEME Guide No. 75. Med Teach. 2022;44(10):1069–1080. doi:10.1080/0142159x.2022.2039382
28. Bailenson JN. Nonverbal Overload: A Theoretical Argument for the Causes of Zoom Fatigue. American Psychological Association; 2021. doi:10.1037/tmb0000030
29. Murdock HM, Penner JC, Le S, Nematollahi S. Virtual morning report during COVID‐19: a novel model for case‐based teaching conferences. Med Edu. 2020;54(9):851–852. doi:10.1111/medu.14226
30. Adams B, Wilson NS. Building community in asynchronous online higher education courses through collaborative annotation. J Educ Technol Syst. 2020;49(2):250–261. doi:10.1177/0047239520946422
31. Rucker J, Steele S, Zumwalt J, Bray N. Utilizing zoom breakout rooms to expose preclerkship medical students to TeleMedicine encounters. Med Sci Educ. 2020;30(4):1359–1360. doi:10.1007/s40670-020-01113-w
32. Spicer JO, Nguyen TT, Arnold MW, Anderson T, Khalife R. A faculty development workshop for planning and implementing interactive virtual case-based teaching. MedEdPORTAL. 2021;17:11126. doi:10.15766/mep_2374-8265.11126
33. Vollbrecht PJ, Porter-Stransky KA, Lackey-Cornelison WL. Lessons learned while creating an effective emergency remote learning environment for students during the COVID-19 pandemic. Adv Physiol Educ. 2020;44(4):722–725. doi:10.1152/advan.00140.2020
34. Gaber DA, Shehata MH, Amin HAA. Online team‐based learning sessions as interactive methodologies during the pandemic. Med Edu. 2020;54(7):666. doi:10.1111/medu.14198
35. Nunneley CE, Fishman M, Sundheim KM, et al. Leading synchronous virtual teaching sessions. Clin Teach. 2021;18(3):231–235. doi:10.1111/tct.13282
36. Dávila A, Wiggins G, McTighe J. 2005 Understanding by Design. Alexandria, VA: Association for Supervision and Curriculum Development ASCD. Bogotá Colombia: Facultad de Ciencias y Educación de la Universidad Distrital; 2017.
37. Anderson T. Teaching in an online learning context. In: Theory and practice of online learning. 2004;273.
38. Suchman AL, Williamson PR, Litzelman DK, et al. Toward an informal curriculum that teaches professionalism: transforming the social environment of a medical school. J Gen Intern Med. 2004;19(5):501–504. doi:10.1111/j.1525-1497.2004.30157.x
39. Kisilevsky E, Margolin E, Kohly RP. Access, an unintended consequence of virtual continuing medical education during COVID-19: a department’s experience at the University of Toronto. Can J Ophthalmol. 2021;56(1):e18–e19. doi:10.1016/j.jcjo.2020.10.002
40. Skiles M, Yang E, Reshef O, et al. Conference demographics and footprint changed by virtual platforms. Nat Sustain. 2022;5(2):149–156. doi:10.1038/s41893-021-00823-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

