Back to Journals » Advances in Medical Education and Practice » Volume 14
Integrated Educational Technology in Teaching Anatomy Using the ASIC Framework: A Case Study from VinUniversity
Authors Ha TM, Hoang D , Huynh CD , Le L
Received 18 January 2023
Accepted for publication 19 May 2023
Published 29 June 2023 Volume 2023:14 Pages 669—681
DOI https://doi.org/10.2147/AMEP.S405340
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Thuy Minh Ha,* Duy Hoang,* Chien Dinh Huynh, Linh Le
College of Health Sciences, VinUniversity, Hanoi, Vietnam
*These authors contributed equally to this work
Correspondence: Duy Hoang, College of Health Sciences, VinUniversity, Vinhomes Ocean Park, Gia Lam District, Hanoi, Vietnam, Tel +84 961 727 259, Email [email protected]
Abstract: The curriculum in teaching anatomy is under increasing pressure to transform from traditional to interdisciplinary integration, from cadaver-based to multimodal instruction with a system-based approach. Educational technologies are becoming critical and urged to be integrated into teaching medicine. At the College of Health Sciences, VinUniversity, the block of Human Body Structure and Function (HBSF) within the undergraduate medical training program was designed to teach anatomy with relevant basic medical sciences based on the principles of the system-based integrated structure. To support students in achieving the intended learning outcomes, multiple innovative technological platforms have been introduced into the curriculum using the moderation of the Adaptation – Standardization – Integration – Compliance (ASIC) framework over four key terms: adaptation, standardization, integration, and compliance. In this paper, the process for curriculum development is presented with an illustration of the selected technological platforms and the lessons learned using the ASIC model.
Keywords: anatomy, education, innovation, integration, technology
Introduction
In medical curricula, Anatomy is considered one of the keystone courses. The prerequisite of a deep understanding of human anatomy is essential for safe clinical practice.1 Without it, regardless of the area of healthcare, practitioners can experience difficulties in performing investigations effectively as they require knowledge of the precise locations of organs and tissues.2 For many years, teaching anatomy was delivered through lectures with a slideshow presentation and audible annotations of the teaching concepts, prosections and dissections, clinical cases, and autodidactic activities using two-dimensional images and multimedia resources.3 Nevertheless, this conventional model does not adequately prepare students for the exponential increase in medical knowledge expected in the 21st century. Traditional cadaver-based training does not tackle the critical need for growing healthcare advancements.4 Careful dissection is time-consuming, and access to dissection laboratories is generally limited.5 There is also a high cost associated with maintaining a dissection laboratory. The use of two-dimensional images limits the ability to be creative and visual, thus limiting the correlation with clinical sciences. A study by Garg et. al. suggests that the capability to imagine is crucial to learn anatomy.6 Textual explanation of three-dimensional structures is often inefficient for students to comprehend them.7 In the era of digitalization, a new generation of learners expects their education to be a technology-rich learning environment with varying levels of technology integration.8
Mohamed Estai and Stuart Bunt published a critical review in 2015 that examined the best practices for teaching anatomy, demonstrating the shift from traditional to interdisciplinary structure, from cadaver-based instruction to multimodal instruction through a system-based integrated approach.1 In recent years, many medical schools have transformed the way of teaching anatomy by incorporating educational technologies, such as virtual and augmented reality, 3D digital anatomy models, virtual dissection, and other computer-based educational programs, into the course.3,9,10 There was, however, no “one-size-fits-all” concept for teaching anatomy. A pedagogical model must be adapted to the institutional context regarding curriculum philosophy, pedagogy methods, financial investment, and educational resources available. As a continuous quality improvement process, the use of technology in anatomy teaching is a continuous process' into 'The use of technology in anatomy teaching is a continuous process of quality improvement. It is critical to evaluate whether these technologies help students meet their learning outcomes; reflection on the curriculum development process is also essential for optimizing their use.
The Current Context of Teaching Anatomy in Vietnam
Anatomy is one of the core components required in the medical curriculum framework endorsed by the Vietnam Ministry of Education and Training.11 Typically, the course is taught in the first or second year as a separate subject, delivered with lectures and practicum using plastic models and cadaveric dissections and prosections. However, the number of bodies donated for teaching purposes is limited due to restrictions mainly from religious belief. There are only two to four cadavers available each year at Hanoi Medical University (HMU), one of the largest medical schools in Vietnam, for the approximately 800 students enrolled in anatomy courses.12 Despite receiving more than 1000 applications for body donation over the past five years, only ten bodies have been donated. This may be attributed to the fact that the relatives of the body donors did not donate them following their deaths, since most Vietnamese do not wish to see their relatives pass away without a complete body.
Vietnamese medical institutions should therefore consider alternative approaches to designing and delivering the curriculum, as well as learning from best practices in similar settings.
Background of VinUniversity and Undergraduate Medical Curriculum
Founded in 2020, VinUniversity is located in Hanoi, the capital city of Vietnam. The College of Health Sciences of VinUniversity offers a six-year medical doctor training program at the undergraduate level, with approximately 50–60 new students enrolling annually. The curriculum for the MD program applied the “backward” design concept so that the program’s outcomes were identified first. The competencies required for graduates have been developed in accordance with the university’s attributes, vision, and mission. During the pre-clinical phase, learning objectives are developed for the Human Body Structure and Function block (HBSF). Consequently, curricular content and teaching activities are constructed in accordance with constructive alignment principles.13 The anatomy curriculum incorporates other disciplines, including Histology, Embryology, Radiology, and Physiology, into the integrative block grid of HBSF. A variety of models and technological platforms aligned with educational strategies have been explored and considered in order to determine whether adopting them will enhance the teaching and learning experience as well as enable students to achieve the desired outcomes. During this period, the Adaptation – Standardization – Integration – Compliance (ASIC) framework has been adopted as the guideline to facilitate the process over four key domains as its name mentions. As part of this paper, the process for curriculum development is described, along with an illustration of the selected technological platforms and lessons learned when using the ASIC model.
The ASIC Framework
Owolabi proposed the ASIC framework as the guide to consider learning theories and pedagogical principles integrating educational technology and innovations.14 This model describes four key terms: Adaptation, Standardization, Integration, and Compliance.
A - Adaptation: identifying innovations and technologies that can be adopted to enhance the learning experience, curriculum delivery, and program outcomes in accordance with curriculum design and institutional resources. In order to make a final decision, a number of factors need to be considered.
S- Standardization: identify the purposes and objectives for which innovations and technologies are used. It is imperative that this technology be applied in a manner that is compatible with the program objectives and expectations by learning from the current practices and standards.
I–Integration: Establish a multi-level plan for using the technology and aligning it with other resources for optimal performance.
C - Compliance: Prior to implementation, usage documentation and other evidence should be established in order to ensure compliance with institutional standards and regulations, as well as meeting program requirements.
An important feature of the framework is that it requires the program to consider multiple aspects of the educational technology in alignment with three domains of the learning objectives, namely cognitive [knowledge], psychomotor [skills], and affective [attitudes]. In order to achieve the milestones and program outcomes, the space required to utilize these technologies must be reserved and matched with the purposes of each practice session; therefore, these technologies will be used within the curriculum.14 The framework also emphasizes evidence-based practice by requesting the program to extensively examine empirical evidence to prove the benefits of educational technology. It has been a challenging task to develop an integrated model to teach anatomy using an interdisciplinary approach; however, with the guidance of the ASIC framework, comprehensive integration of educational technology has been provided on a step-by-step basis.
Curriculum Development and Delivery Using the ASIC Framework
Philosophy of Curricular Design
Curriculum development uses the concept of backward design, where program outcomes are predetermined after needs assessments. In the national context, since 2015, the Ministry of Health of Vietnam has endorsed the list of competencies that general doctors should possess upon graduation, which consists of four domains (i) professional practice, (ii) medical knowledge, (iii) medical care, and (iv) communication and cooperation.15 MD program’s expectation is not only fulfilling the Ministry requirement but also adopting competencies from the domains of (i) practice-based learning and improvement and (ii) system-based practice as per the guidelines of the Accreditation Council for Graduate Medical Education (ACGME) (Table 1).16
 |
Table 1 Comparison of the Core Domains from the List of Expected Competencies for Medical Doctor Graduation |
Curriculum outcome mapping has been developed in accordance with the distribution of expected competencies across the entire program, which is used to determine the learning objectives of each course. Anatomy is taught within an integrative block-grid HBSF structure in the second year. Several disciplines have been integrated into the block, including Histology, Embryology, Radiology, and Physiology. As part of the learning objectives of the block, efforts have been made to achieve the expected competencies while also laying a solid foundation for the clinical years to follow. Blocks are structured according to the organ body systems, which range in length from one to three weeks. Educational strategies were developed constructively in alignment with the learning objectives.13 In addition to lectures and case-based small group discussions, there are practical sessions in the lab where technology plays a crucial role in moderating the learning process (Table 2).
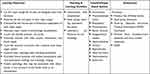 |
Table 2 Learning Objectives, Teaching & Learning Activities, and Assessment of the HBSF Block |
Adaptation
A key component of the success of a course is the development of educational strategies. In addition to planning learning objectives and pedagogy, many other factors must be considered during the adaptation process. Integration with educational platforms serves the following purposes:
- Filling the gaps/shortage of lacking cadaveric dissection.
- Enhancing teaching and learning experiences by using the advantage of innovations and technological platforms in an updated manner.
- Assisting students in moving from surface learning to deep learning and achieving their learning outcomes.
Multiple working sessions have been organized to collect stakeholders’ comments and feedback to evaluate the feasibility. To shorten the process of seeking suitable platforms, a list of considerations has been developed, and a comparison was conducted to make the decision (Table 3). The list of the technological platforms for each of the disciplines that have been selected is described in Table 4.
 |
Table 3 Considerations When Seeking the Suitable Educational Platforms |
 |
Table 4 The List of the Platforms for Consideration |
The methods used to teach anatomy and other principles in the HBSF block have also substantially changed in recent years. As new technologies are introduced, there is a greater opportunity to explore and understand the anatomy of the human body and its functions.
In order to facilitate block-wide anatomy, physiology, and radiology teaching, the Pirogov Anatomy Table (Pirogov table), Complete 3D Anatomy software, and plastinated cadavers have been identified. In pathology, slides are analyzed using a digital pathology platform called Pathcore Flow, which is a connected workspace for research and clinical practices. All these mentioned technologies can be used remotely and allow concurrent access from multiple devices.
Standardization
Standardization has been implemented, but the literature evidence could be more comprehensive. A simple explanation could be the variety of medical educational contexts, the complex character of medical education, and the wide range of educational technological systems.17 In 2017, Vaitsis et al published a review of standards that allow the technical needs and educational needs to work in concert in the contemporary context of Outcome-Based Medical and Healthcare Education;18 giving an insight into the most current relevant standards that could effectively evaluate and measure teaching against the determined outcomes or competencies, compare curriculum based on structured analyses, and help students better understand their learning intentions.
The standardization process has also been enhanced by field trips to other medical schools in order to learn about their practices. Several field trips were conducted by the university’s leadership from 2018 to 2021 to National University Singapore, the University of Pennsylvania, and Yale University. Aside from exploring the learning resources, the main purpose of the trip was to visit the laboratories and interact with the person in charge of the learning resources. A valuable resource for obtaining information would be the vendors themselves. Despite not being entirely objective, essential data can be provided on request and can contribute to the decision-making process. Several types of information are immediately available, including current users, customer feedback, analysis of the situation, and comparisons with competitors.
Integration
Integration is a time-consuming process. Initially, faculty and support staff participated in training workshops offered by vendors. The team works internally to match the platforms to the objectives of the curriculum. For the HBSF block, these platforms are prioritized for practice sessions, while lectures and small group discussions can be conducted using presentation slides. In advance of the implementation, handouts containing details about the relevant platform, expected learning outcomes, and associated activities are prepared and distributed to all students in advance. The instruction manuals for each platform were provided to students at the beginning of the academic year. Presentations and guidelines in the form of recorded videos are also prepared and presented to students during orientation. This document contains essential information regarding the purpose of the platforms, how they will be integrated within the block, how to install the app, and the confidentiality of the account.
As a result of the multiple platforms that are used during anatomy laboratory practice, the situation is complicated at times. For clarification, a detailed handout containing the guidelines for teaching and learning activities has been prepared and is used to moderate the classes (Figure 1).
 |
Figure 1 A sample of the laboratory handout plan which integrated multiple educational platforms. |
At the course level, these educational platforms have been integrated into the schedule, as in the example of Figure 2. Mondays, Wednesdays, and Fridays were designated as the days for the block, and the associated platforms with teaching content needed to be ready by the start of the session. These platforms, however, require further customization to fit in with the learning objectives; and they significantly increase the workload of the teaching staff with regard to mastering the teaching content as well as facilitating learning activities through these platforms.
 |
Figure 2 An example of teaching sessions using educational technological platforms in a week of Pulmonary block-system (HBSF, VinUniversity). Note: Reproduced with permission from Canvas.28 |
A key factor in driving the implementation of innovative technology across the HBSF is the robust use of Canvas, a reliable Learning Management System (LMS) that has become widely used at other organizations. By integrating all learning materials and resources into the LMS, Canvas plays a critical role in block delivery and management by integrating all learning materials and resources into the LMS. In the module section of the course, a list of the teaching sessions has been arranged sequentially according to the flow of teaching activities. All lectures, case studies, and lab handouts are organized according to the relevant topics. In some cases, pre-reading requirements may be designed as self-quizzes or items that must be acquired prior to the class. Links to external platforms can be inserted into Canvas without significant difficulties. A basic Canvas training program is a requirement for both onboarding faculty and students.
Compliance
Using educational technology to teach anatomy and relevant medical sciences has demonstrated numerous benefits so far. To implement the course smoothly, many aspects needed to be considered by the stakeholders’ compliance. Firstly, students should be familiar with the platform and follow all the instructions prepared by the teaching team. Course instructors should follow the plan and continuously seek quality improvement and feedback to improve the experiences. Visible, continuous development of the software or the capability to allow users to self-integrate their teaching materials into the platform of choice are among the most important decision-making factors. It is therefore imperative that the technology team provides prompt support for optimal use of educational technologies.
Results
It is impossible to ignore the advantages of the educational technology platform integrated into the curriculum. In spite of this, the process of developing a curriculum is highly resource- and time-consuming, and it requires detailed guidelines to ensure that all aspects have been considered adequately. The primary purposes of the integration process are to help students achieve the program’s outcomes and improve learning experiences. The ASIC framework can be used to help the program construct the plan for integrating the technological platforms into the curriculum. The following is a brief description of these selected platforms and their highlights.
Complete 3D Anatomy Software
The Complete 3D Anatomy (CA) software by Elsevier has been modernizing how anatomy and physiology are taught in higher education.19 Students can examine human body structures in three dimensions by zooming into every miniature detail at every angle, dissecting through anatomical layers, and revealing structures and functions from underneath. Interactive three-dimensional (3D) models illustrate complex anatomical relations and visualize the fundamental link between anatomy and physiology (Figure 3). Other anatomical information, such as muscles’ origin, insertion, innervation, vascular supply, or clinical correlations if a structure is damaged, is provided in great detail to users. The application comes with the “Lecturer Builder” feature, in which course instructors can assemble a lecture by combining recordings, screens, and quizzes that fit their teaching goals and directly share them with students within the program’s platform or via LMS. The use of CA software also supports the VARK (Visual, Aural, Reading, and Kinesthetic) theory of learning by offering kinesthetic advantages.20,21 The libraries of images, videos, animations, 3D lectures, and continually updated courses are accessible for learners to self-study and deepen their knowledge. To monitor the progress of students, the statistic reports after quizzes/assignments demonstrate how students engage in their lessons, retain information, and perform compared to their classmates.
 |
Figure 3 An example of an interactive model of the human liver in CA software. Users can zoom in and rotate at every angle, making the subject more appealing to learners. (Image courtesy of Complete Anatomy.).29 |
A key feature of CA is augmented reality (AR). Instructors and students can use this function on their mobile phones to project a model onto a flat and textured surface (eg, tabletop). Multiple users can also share a model view in real time, meaning that one user can host a model or a cadaveric dissection, and other users in the same class can join. An instructor may use this feature to emphasize a specific structure or demonstrate a virtual dissection to the entire class. This feature is available on most smart handheld devices with a user-friendly interface (Figure 4).
 |
Figure 4 An example of how the AR feature of CA software works on a mobile phone. Users can project any model onto a flat surface. Through their phones’ cameras, they can walk around and investigate the projected model at any angle. The projection is also interactive, meaning users can tap on any region of the model to obtain related anatomical information. (Image courtesy of Complete Anatomy).29 |
Another advantage of CA software is its accessibility regardless of learning activities occurring inside or outside of class. This software is both compatible with PC (Windows and Mac), tablets, and smartphones (iOS and Android).
Pirogov Table
The Pirogov table (Figure 5) is named after a Russian pioneering surgeon and medical scientist – Nikolay Ivanovich Pirogov.22 It is a product of the Pirogov company located in Russia and is commercially available via local distributors. Different from other popular products based on a similar concept (eg, Anatomage table), the Pirogov table solely focuses on anatomy with aspects of histology and radiology rather than demonstrating the functionality of anatomical structures. The slice tool of the Pirogov table is surprisingly powerful, allowing users to slice through structures and radiographic images at different dissection planes. The visible human project, a detailed dataset of cross-sectional, 3D representations of a human male body and a human female body,23 is also integrated into the Pirogov table Other benefits of the Pirogov Anatomy Table may include but are not limited to the virtual 3D atlas, virtual dissection, and comparative 3D images between normal and pathological anatomy. The table also comes with a “quiz” function, but it is not as comprehensive as the “lecture builder” and “curriculum management” functions on CA software according to the faculty’s evaluation.
Recently, the Pirogov company has launched a mobile version of the Pirogov table for convenient accessibility. Even without the mobile version, students could still access the Pirogov table from a distance by joining the same local network that the Pirogov table is connected to or gaining access via the virtual portal network (VPN) granted by the university’s IT department.
Pathcore Flow Platform
Instead of using conventional light microscopy, digital microscopy has been proven to be an adequate learning tool for students.24 For histological/pathological teaching, Pathcore Flow – one of the digital microscopic platforms is selected to replace conventional light microscopy (Figure 6). It is a collection of high-quality normal and pathological slide images where the annotations can be created for teaching and assessment activities. The data stored within Pathcore Flow can serve not only for teaching activities but also for research purposes.
 |
Figure 6 An image of skeletal muscle at 40x magnification on Pathcore Flow. (Image courtesy of Pathcore). |
Plastinated Cadavers
The plastinated cadavers (Figure 7) are a valuable learning resource, and their contributions to the learning experience of the students cannot be unstated. They are particularly durable, and their required storage conditions are minimal with room temperature below 35 degrees Celsius and humidity under 50%. The most appropriate setting for learning anatomy is where learners can examine desired structures from all angles using cadavers or synthetic recreations. This innovation of Dr. Gunther von Hagens shows explicit flexibility, in which instructors and students can treat dissected cadaver or cadaver parts as plastic models but are provided with profound details of real human body structures.25 They address various shortcomings of using formaldehyde-treated cadavers, including unpleasant smells, tiredness/dizziness, lacrimation, and excessive cost of keeping the facility up to the standard for safety regulations.26 While virtual models in CA software and Pirogov table are graphical representations of the human body, plastination gives learners a real perspective of anatomy. Whenever students need to identify and examine anatomical structures on plastinated cadavers, they could project a model next to the plastinated specimens using the AR function of CA software or look them up in the virtual 3D atlas on CA software or Pirogov table for further investigation.
 |
Figure 7 Plastinated cadavers are a valuable learning resource for students. |
Discussion
Effectiveness and Challenges of the Integration
HBSF is an integral part of the medical curriculum, and the use of technology within this block limits the disadvantages of traditional learning. While cadavers provide spatial information in anatomy education, anatomical and physiological information is generally obtained from textbooks in conjunction with the specimen. Generally, written resources contain excessive amounts of information and may not be necessary for the level of undergraduate students. Several anatomical areas cannot be taught using dissections, including the nervous system, skeletal system, or muscular anatomy in the contracted state. By utilizing 3D anatomical models, these shortcomings can be addressed by enhancing the spatial understanding of relationships between the various structures of the human body. Spatial knowledge development can be facilitated with the exploration of a virtual environment, and it is proven comparable to when students study an object in real life.27 It is not only possible to narrow the gap between students who find it challenging to visualize structures spatially and those who are confident in their spatial abilities by using the CA application and Pirogov table, but it also reduces the cognitive effort required to comprehend new anatomical contexts. Students can access every detail and provide a description of the chosen structure by using 3D models, which may also aid in their long-term retention of gross anatomy. As a result, we were able to observe an increase in student engagement and an improvement in productivity in class since students are no longer solely dependent on their spatial abilities to study and retain new anatomical knowledge. The block is designed to allow students to utilize both the CA application and Pathcore platform frequently in both lectures and lab sessions, while the Pirogov table and plastinated cadavers are primarily used in lab sessions. In a typical lab session of the Anatomy course at VinUniversity, students are divided into small groups with different assignments using different learning resources, including CA software, Pirogov table, plastic models, and plastinated models, and a facilitator is present at every assignment. Each assignment usually lasts 30 minutes, and then students rotate to the next assignment until all tasks are completed. Plastinated cadavers are the ultimate learning resource while all other resources are graphical representations of the human body; they usually are the first source of information students look for when they start studying or revising any anatomical concept. Students are able to become highly familiar with each technology and maximize the use of all learning resources through this teaching flow.
The use of Pathcore also significantly reduces the workload of instructors and laboratory technicians when teaching histology both in theory and in practice. The web-based platform allows Pathcore Flow to be accessed from both mobile and desktop devices. Courses are designed and integrated with LMSs or shared directly on Pathcore Flow, and instructors have access to a large library of high-definition slide images of cells and tissues. The platform also allows instructors to import new slide images so they can share any images of interest.
This deployment of technology involves a substantial investment, both financially and human resource-wise. As part of the curriculum development process, a significant amount of time and effort is devoted to embedding the application in alignment with the teaching contents and learning objectives. Additionally, instructors from previous generations have a more difficult time adapting to new, fast-paced technological changes. Accordingly, intensive training in educational technology and support from teaching assistants are provided to both faculty and students. The university is also required to pay a subscription and maintenance fee in order to maintain the technology application.
Limitations of the Study
“At the time of submission of this paper, the process has been running for less than two years, and further evaluation and feedback are required from the stakeholders . As the paper focuses on the design and implementation, it does not address the assessment aspects associated with their use. It also does not examine the financial aspect but focuses primarily on curriculum development and reflection.
Recommendations
Considering the emergence of educational technologies, without guidance from the framework for curriculum development, it is predictable that curriculum team will become lost in the integrating process and depart from the learning objectives.
Collaboration with vendors is highly recommended to ensure prompt resolution of issues as well as to reap the benefits of faculty capacity building.
Establishing a shared library and resources is recommended to be included in planning the curriculum.
Evaluating the effectiveness of these platforms should be conducted, and continuously seeking improvement is highly important.
Conclusion
Continuous integration of technology into medical education is essential to improving learning outcomes and addressing the cognitive load associated with Anatomy. The lessons learned from VinUniversity can benefit other institutions in considering the integration of education technology focusing on teaching anatomy and related basic medical sciences using the ASIC framework.
Acknowledgments
Sincere thanks to VinUniversity’s strategic partner – the University of Pennsylvania for their collaborative contributions to develop the MD curriculum.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Estai M, Bunt S. Best teaching practices in anatomy education: a critical review. Ann Anat. 2016;208:151–157. doi:10.1016/j.aanat.2016.02.010
2. Singh R, Shane Tubbs R, Gupta K, Singh M, Jones DG, Kumar R. Is the decline of human anatomy hazardous to medical education/profession?--A review. Surg Radiol Anat. 2015;37(10):1257–1265. doi:10.1007/s00276-015-1507-7
3. Murgitroyd E, Madurska M, Gonzalez J, Watson A. 3D digital anatomy modelling - Practical or pretty? Surgeon. 2015;13(3):177–180. doi:10.1016/j.surge.2014.10.007
4. Wickramasinghe N, Thompson BR, Xiao J. The opportunities and challenges of digital anatomy for medical sciences: narrative review. JMIR Med Educ. 2022;8(2):e34687. doi:10.2196/34687
5. Papa V, Vaccarezza M. Teaching anatomy in the XXI century: new aspects and pitfalls. Sci World J. 2013;2013:310348. doi:10.1155/2013/310348
6. Garg AX, Norman GR, Eva KW, Spero L, Sharan S. Is there any real virtue of virtual reality?: the minor role of multiple orientations in learning anatomy from computers. Acad Med. 2002;77(10 Suppl):S97–9. doi:10.1097/00001888-200210001-00030
7. Fairén González M, Farrés M, Moyes Ardiaca J, Insa E. Virtual Reality to teach anatomy. In: Eurographics 2017: Education Papers. European Association for Computer Graphics; 2017. doi10.2312/eged.20171026
8. Guze PA. Using technology to meet the challenges of medical education. Trans Am Clin Climatol Assoc. 2015;126:260–270.
9. Mansing R, Taru M, S S. Innovative teaching verses traditional teaching in anatomy. Indian J Bas AppMed Res. 2014;4(1):503–505.
10. Patra A, Asghar A, Chaudhary P, Ravi KS. Integration of innovative educational technologies in anatomy teaching: new normal in anatomy education. Surg Radiol Anat. 2022;44(1):25–32. doi:10.1007/s00276-021-02868-6
11. Ministry of Education and Training. Circular 01/2012/TT-BGDDT “Promulgating the set of higher education framework programs for the health sciences sector, undergraduate level”; 2012. Available from: https://vanban.chinhphu.vn/default.aspx?pageid=27160&docid=157514.
12. VietNamNet Global. Barriers exist for people to donate their bodies to science. VietNamNet Global. Available from: https://vietnamnet.vn/en/barriers-exist-for-people-to-donate-their-bodies-to-science-727058.html.
13. Biggs J, Tang C. Teaching for Quality Learning at University.
14. Owolabi J. Proposing a framework guide for the integration of educational technologies and innovations into the teaching of anatomy and medical sciences: the ASIC framework. Advan Med Educat Pract. 2021;12:1277–1282. doi:10.2147/amep.s338262
15. Ministry of Health. Decision 1854/QD-BYT on the approval of the document “Basic Standards of Competency of General Practitioners”; 2015. Available from: https://thuvienphapluat.vn/van-ban/EN/The-thao-Y-te/Decision-No-1854-QD-BYT-2015-document-about-competence-standards-for-general-practitioners/286613/tieng-anh.aspx.
16. ACGME. Accreditation Council for Graduate Medical Education. Available from: https://www.acgme.org/. Accessed
17. Mennin S. Self-organisation, integration and curriculum in the complex world of medical education. Med Educ. 2010;44(1):20–30. doi:10.1111/j.1365-2923.2009.03548.x
18. Vaitsis C, Spachos D, Karolyi M, et al. Standardization in medical education: review, collection and selection of standards to address technical and educational aspects in outcome-based medical education. MEFANET J. 2017;2017:28–39.
19. Danish J, Sadat A. Innovations in teaching methods of anatomy. Ann Med Health Sci. 2016;3(2):56–58. doi:10.5958/2322-0422.2016.00013.8
20. Othman N, Amiruddin MH. Different perspectives of learning styles from VARK model. Proc Soc Behav Sci. 2010;7:652–660. doi:10.1016/j.sbspro.2010.10.088
21. Meyer AJ, Stomski NJ, Innes SI, Armson AJ. VARK learning preferences and mobile anatomy software application use in pre-clinical chiropractic students. Anat Sci Educ. 2016;9(3):247–254. doi:10.1002/ase.1555
22. Hendriks IF, Bovill JG, van Luijt PA, Hogendoorn PC. Nikolay Ivanovich Pirogov (1810–1881): a pioneering Russian surgeon and medical scientist. J Med Biogr. 2018;26(1):10–22. doi:10.1177/0967772016633399
23. Ackerman M. The visible human project. Access Visib Human Proj. 1995;1:4.
24. Rodrigues-Fernandes CI, Speight PM, Khurram SA, et al. The use of digital microscopy as a teaching method for human pathology: a systematic review. Virchows Arch. 2020;477(4):475–486. doi:10.1007/s00428-020-02908-3
25. von Hagens G, Tiedemann K, Kriz W. The current potential of plastination. Anat Embryol. 1987;175(4):411–421. doi:10.1007/bf00309677
26. Tiruneh C. Acute adverse effects of formaldehyde treated cadaver on new innovative medical students and anatomy staff members in the dissection Hall at Wollo University, Northeast Ethiopia. Adv Med Educ Pract. 2021;12:41–47. doi:10.2147/amep.S291755
27. Dalgarno B, Hedberg J, Harper B The contribution of 3-D environments to conceptual understanding; 2002:149–158.
28. Instructure. Canvas by Instructure. Available from: https://www.instructure.com/k12/products/canvas. Accessed January 03, 2023.
29. 3D4Medical. 3D4Medical from Elsevier. Available from: https://3d4medical.com/. Accessed January 15, 2023.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

