Back to Journals » Journal of Pain Research » Volume 16
Insight into Dysmenorrhea Research from 1992 to 2022: A Bibliometric Analysis
Authors Dong Y , Li MJ , Hong YZ, Li WJ
Received 4 August 2023
Accepted for publication 29 September 2023
Published 27 October 2023 Volume 2023:16 Pages 3591—3611
DOI https://doi.org/10.2147/JPR.S430233
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Robert B. Raffa
Yin Dong,1,* Ming-Jing Li,2,* Yan-Zhu Hong,3 Wen-Jie Li4
1Putuo Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 2Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 3School of Medicine, Xiamen University, Xiamen, People’s Republic of China; 4Shanghai Innovation Center of TCM Health Service, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yan-Zhu Hong, Xiamen University, No. 422, Siming South Road, Siming District, Xiamen, Fujian, 361005, People’s Republic of China, Tel +86 13671617025, Email [email protected] Wen-Jie Li, Shanghai University of Traditional Chinese Medicine, No. 1200 Cai-lun Road, Pudong District, Shanghai, 201203, People’s Republic of China, Tel +86 15397687742, Email [email protected]
Abstract: Dysmenorrhea, classified as primary dysmenorrhea and secondary dysmenorrhea, is a common gynecological symptom that seriously affects female daily life. At present, studies on dysmenorrhea are numerous and complex. To better reflect the trend and innovative progress of dysmenorrhea-related research, this study screened papers on the Web of Science from January 1, 1992, to December 31, 2022. A total of 1012 papers were selected and analyzed for their affiliated countries, institutions, authors, keywords, etc. China is the country with the most academic output, Beijing University of Traditional Chinese Medicine is the most influential institution, and Yang Jie, from Chengdu University of Traditional Chinese Medicine, China, is the scholar with the most papers. We consider that the current research focus is on pathogenesis, treatment, epidemiology, and self-management. With increasing research on functional connectivity between dysmenorrhea and various brain regions, functional connectivity has gradually become the forefront of research. We hope our study can promote the further study of dysmenorrhea.
Keywords: pathogenesis, treatment, management, traditional Chinese medicine
Introduction
Dysmenorrhea, defined as painful cramps that occur with menstruation, is the most common gynecologic problem for women of all ages and races and one of the most common causes of pelvic pain. The history of dysmenorrhea dates back to the Greeks who defined the word as “painful menstrual flow”.1 In the modern medical system, dysmenorrhea can be classified into primary dysmenorrhea (PD) and secondary dysmenorrhea (SD).2 PD refers to pain with no definite cause in the menstrual cycle, which usually starts within 1 year after menarche. The main pathogenesis is related to the secretion of prostaglandin F2α (PGF2α) (Figure 1). SD is associated with an underlying pelvic disease and manifests later than PD, usually more than 2 years after menarche. For reasons including endometriosis, pelvic inflammatory disease, chronic salpingitis, ovarian cysts, use of intrauterine devices, cervical stenosis, submucosal fibroma, uterine fibroids, uterine polyps, adenomyosis, and early pregnancy, most commonly endometriosis.3–5 Regarding the external factors of dysmenorrhea, there is no systematic study to date.
 |
Figure 1 The main mechanism of PD. Arachidonic acid is metabolized through the cyclooxygenase (COX) and 5-lipoxygenase (5-LO) pathway to produce prostaglandins and Leukotriene (LT) A4 respectively, and is transported out of cells through corresponding transporters (prostaglandin transporters (PGT), multidrug resistance related proteins (MRP1)). After extracellular metabolism, PGF2α, PGE2 and LTE4 act on the corresponding cell receptors (the G prote– coupled receptor (EP, FP), cysteinyl leukotriene receptors (Cys-LTs)), causing potent vasoconstriction and myometrial contractions, and leading to ischemia and pain.6–8 |
According to studies, the prevalence of dysmenorrhea varies greatly in different regions, age groups. The overall prevalence is 15% to 94%.9 The prevalence in married women is generally lower than that in unmarried women.10–13 The prevalence in young women aged 17–24 years has been investigated and ranges from 67% to 90% and begins to decline after the age of 25 years.5,9 Dysmenorrhea has been shown to affect women’s quality of life, reflected mainly in school and work performance, including lack of energy for daily activities, higher level of stress, absenteeism and decreased efficiency, sports participation, and socialization, which causes a great deal of lost productivity.14–18 As menstrual health problems cause consequences for women’s lives, the World Health Organization stated that menstrual health to be recognized, framed, and addressed as a health and human rights issue.19
There are many treatments for PD, but pharmacological treatment may be the most effective (Figure 2), including nonsteroidal anti-inflammatory drugs (NSAIDs), hormonal contraceptives, tocolytics, vitamins, and omega-3, among which NSAIDs are the prime choice. Nonpharmacological treatments include lifestyle changes, transcutaneous electrical nerve stimulation (TENS), local heating, acupuncture, and acupressure. Surgical treatment, which includes laparoscopic uterosacral nerve association (LUNA), presacral neurectomy (PSN), and hysterectomy, is only applicable to a few women with severe or refractory dysmenorrhea, but there are few relevant studies.4
 |
Figure 2 The treatment of dysmenorrhea and their advantages and disadvantages.4,20,21 |
Although pharmacological treatment is the most effective, a considerable number of women tend to perform self-management and nonpharmacological treatment strategies during the menstrual period, such as hot compress, rest, hot shower/bath and exercise.22,23 At present, many researchers have made great progress in interventions for dysmenorrhea. However, some of these interventions still lack experimental evidence. Among them, the levonorgestrel releasing intrauterine system (LNG-IUS) has a good therapeutic effect in dysmenorrhea in women of all ages and has great advantages in the treatment of adolescent endometriosis.24 Bibliometrics, known as an effective method for exploiting statistical approaches for quantitatively analyzing scientific documents, provides a solution to systematically review relatively large-scale documents and explore objective results while minimizing subjective bias.25 This study uses bibliometric methods to collect data (including countries, institutions, journals, authors, keywords and citations). The bibliometric method simplifies the process of extracting key information from massive literature information so that we can search for features with visual significance in the visual network and extract clear directional information. The analysis of these visual networks makes it possible to study the research hotspots, research trends, cooperative networks, and the development direction of the whole discipline in each period.26,27 This study aims to explore some questions for discussion, such as pathogenic factors other than prostaglandins and relatively effective therapies, and to examine future research trends.
In the current article, compared to Fu et al,28 the treatment methods for dysmenorrhea are supplemented and analyzed, and the etiology, pathogenesis, epidemiology, and self-management of dysmenorrhea are discussed. Compared to Liu et al,29 this article selects a larger time range and provides explanations on treatment methods and pathogenesis.
To further understand the development of dysmenorrhea, we seek answers to the following research questions:
RQ1: What effective methods are available for treating or alleviating dysmenorrhea?
RQ2: What are the hotspots in research on dysmenorrhea-related fields in the past thirty years?
RQ3: What is the current pioneering research in the field of dysmenorrhea?
RQ4: What are the possible future research directions in the field of dysmenorrhea?
Materials and Methodology
Data Retrieval and Data Collection
This cross-sectional study retrieved literature information from the Web of Science core collection (WOSCC) (https://www.webofscience.com). All searches were completed within one day to avoid deviations from daily database updates. The edition we selected was Science Citation Index Expanded (SCI-EXPANDED). The search formula was “TS=(dysmenorrhea) OR TS=(dysmenorrheal) OR TS=(dysmenorrhoea)”, including different expressions of “dysmenorrhea”. The index date range was from January 1, 1992, to December 31, 2022. After selecting the type “article and review” in the search results, we obtained 4220 paper results. By investigating the title, abstract and content, we excluded repetitive literature or literature unrelated to “dysmenorrhea” and ultimately included 1012 articles in the research scope. The filtered data with “Full record and Cited references” were exported from WOSCC as a plain text file, Excel file and tab-delimited file.
Data Analysis and Network Mapping
The bibliometrics and visual analysis of this study were mainly based on CiteSpace (Version 6.1.R2/5.7. R2, USA), VOSviewer (version 1.6.18, USA), Scimago Graphics (USA) and https://bibliometric.com/app. We uploaded the tab-delimited file data to the website to analyze the annual overall publication trends and publication trends for countries around the world. The data, processed by VOSviewer, were used in Scimago graphics to generate a national cooperative network. The rest of the analysis, including institutions, author collaboration network, subject co-occurrence analysis, keywords co-occurrence analysis, and literature co-citation analysis, were completed through CiteSpace using the data of the plain text file.
Except where noted, the parameters for CiteSpace settings were as follows: Time slices from January 1992 to December 2022, with 1 year per slice. The Links Strength was “Cosine”; the Links Scope was “Within Slices”. The selection used a modified g index in each slice where the scale factor k = 25.30 The “Pathfinder”, “Pruning sliced networks”, and “Pruning the merged network” options were selected in the “Pruning window” to obtain a concise and clear visual network without changing any other details. The choice of node type depends on the project being analyzed.
Results
Annual Publication Trend
There were 882 articles and 130 review articles. First, we counted the number of annual publications related to dysmenorrhea from January 1, 1992, to December 31, 2022. As shown in Figure 3A, the overall publications show a steady upward trend. This is due to the growing concern about women’s health. In addition, we examined the statistics of the number of dysmenorrhea-related papers published in various countries every year. As shown in Figure 3B. The top 10 most productive countries or regions are presented in Table 1. The main evaluation indicators include the number of documents, the first publicized year, and citations. The top 3 countries are China, the United States and Iran. Relevant papers have been published annually in the United States since 1992, but the trend has fluctuated. Regardless, the United States ranked first in the total number of citations, far surpassing other countries, indicating the leading position of the United States in the research of dysmenorrhea-related fields; China has been cited less frequently than the United States, but in terms of annual publications, China has ranked first in annual publication volume since 2010, showing an increasing yearly trend. The trend of literature publication shows that research related to dysmenorrhea is increasing, and researchers around the world are paying increasing attention to it every year.
 |
Figure 3 (A) The number of annual publications on dysmenorrhea from 1992 to 2022. (B) The number of publications per year on dysmenorrhea in the United States and China from 1992 to 2022. |
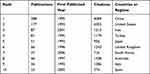 |
Table 1 The Top 10 Countries or Regions on Publications on Dysmenorrhea from 1992 to 2022 |
Analysis of Published Journals
By analyzing publications related to dysmenorrhea in 331 journals, 228 publications belonging to the top 10 journals accounted for 21.46% of the overall number. Table 2 lists their publications, citations, average citations, impact factors (IF) in 2022, journal citation reports (JCR) (https//:www.webofscience.com), and publishers. Of the publications, Medicine ranked first, with 28 publications. Journal of Pediatric and Adolescent Gynecology ranked second, with 27 publications. The average citation reflects, to a certain extent, the authority and recognition of these publications in journals in the area of dysmenorrhea. The average citations in Medicine were only 4.36. In contrast, the total number of publications in Obstetrics and Gynecology was 17, but the average citations reached 79.24, ranking first, which indicates that Obstetrics and Gynecology has high authority in the research of the dysmenorrhea-related area. The impact factor (IF) is an internationally accepted journal evaluation index. Table 2 shows the IF of each journal in 2022, ranging from 1.6 to 7.4, with an average value of 3.89. Among them, the IF of Pain is 7.4, ranking first, demonstrating that it has a great influence in dysmenorrhea-related fields. The journals with larger articles are located in Q3 or Q4, which have potential for growth.
 |
Table 2 The Top 10 Journals of Publications Volume on Dysmenorrhea from 1992 to 2022 |
Analysis of Cooperation Network
Countries
The cooperation between different countries or institutions is of far-reaching significance. The cooperation network between countries can show us the influence and cooperation attitude of countries or regions. To this end, we used VOSviewer and Scimago Graphic together to visualize cooperation in countries or regions. A total of 69 countries or regions were included. The results are shown in Figure 4. Forty-nine of the 69 countries had international cooperation, the United States had cooperated with 25 countries (Figure 4A), and the total number of cooperation occurrences was 56 (Figure 4B), ranking first. The United Kingdom conducted international cooperation with 16 countries, ranking second. Australia ranked third and cooperated with 15 countries. However, China has shown a higher trend of cooperation. It has conducted 42 international cooperations, ranking second in the world, surpassing 35 in the United Kingdom and 23 in Australia. It is worth noting that among the countries that have participated in international cooperation, nearly one-third of the countries have only cooperated with one country, and nearly half of the countries have cooperated with less than two countries, which indicates that research in dysmenorrhea-related fields is more conducted through domestic cooperation. More extensive international cooperation can be expected in the future.
Institutions
A total of 1273 institutions participated in research related to dysmenorrhea. Table 3 lists the total number of publications of the top 10 institutions and their related content, the number of citations and their countries. Table 4 lists the total number of papers, the number of citations and the average number of citations published by these institutions as the first finishers. Half of the top 10 institutions in total publications are from China. Beijing University of Chinese Medicine has the largest number of publications, with 25 publications, and Chengdu University of Traditional Chinese Medicine has 22 publications in total, ranking second. In addition, more than half of the publications in dysmenorrhea-related fields of these 2 institutions are published by the first author, indicating that the relevant literature of the 2 institutions occupies a dominant position in this field. The average number of citations of National Yang-Ming University ranked first, with 30.68. The number of papers issued by the first author of the organization varied. Half of the institutions were from China, and the other institutions were from South Korea, South Africa and Australia. It is worth noting that the average number of citations of the first author of Witwatersrand University was 32.2, ranking first, and far exceeding the 19.36 of National Yang-Ming University, which ranked second, indicating that the first author of this organization has a high worth and great influence in the field of dysmenorrhea. Whether it is the total number of publications or the number of first author publications, institutions from China account for a large proportion, while research institutions from the United States and Iran are relatively rare on the list. We checked the number of relevant institutions, and a total of 335 US institutions and 83 Iranian institutions have published literature in the field of dysmenorrhea, indicating that they have a large number of institutions and relatively scattered research.
 |
Table 3 The Top 10 Institutions of Publications Volume on Dysmenorrhea from 1992 to 2022 |
 |
Table 4 Number of Publications in First-Author Units at the Top 10 Institutions in the Northeast in Terms of Number of Publications from 1992 to 2022 |
The results from the CiteSpace institutional cooperation network analysis are shown in Figure 5. Among the institutions with a large number of publications, Taipei Veterans General Hospital, China Medical University and National Yang-Ming University constituted the cooperation triangle. The China Academy of Chinese Medical Sciences and Capital Medical University, Beijing University of Chinese Medicine showed more cooperation. These universities seem to constitute two relatively independent cooperation systems, and there is no correlation between the two cooperation systems. Closer cooperation efforts are mostly from within the same country, and there is less cooperation between institutions from different countries.
Authors
Through the analysis of the number of articles published by the authors, the citation of the articles and the cooperative network, we found that 3859 authors have studied dysmenorrhea. Combining the analysis of the top 10 authors in Table 5, we found that most of the authors are from China. Among them, Jie Yang, from Chengdu University of Traditional Chinese Medicine, has published the largest number of articles, with 28 articles published and 207 citations. His research directions include Neurosciences Neurology, Integrated Comprehensive Medicine, Anesthesiology, and General Internal Medicine. The second is Professor Hsieh, Jen-Chuen from National Yang-Ming Chiao Tung University, who published 14 articles and was cited 462 times. His research directions include Neurosciences, Medicine Research Experimental, Integrative Complementary Medicine, and Neuroimaging.
 |
Table 5 The Top 10 Authors of Publications Volume on Dysmenorrhea from 1992 to 2022 |
Through the analysis of the cooperative relationship network, it can be found that most scholars have relatively fixed partners, and their cooperative relationships are intertwined to form several cooperative networks (Figure 6). Cooperation between Yu Chen and Ling Chen and between Hsieh Jen-Chuen, three scholars, is more frequent; Hellman Kevin and Tu Frank, Liang Fanrong and Jie Yang have also established close collaborations and published a large number of articles; and authors such as Yong-xiang Wang, Chen, Chen X. and Ji-xin Liu are more inclined to collaborate with different authors.
Analysis of Co-Occurrence Network
Interdisciplinary
To study the combination and development of various disciplines in the field of dysmenorrhea, we conducted a co-occurrence analysis of disciplines, as shown in Figure 7. Dysmenorrhea, as a gynecological symptom, easily affects women’s lives. It has many inducements and various treatment methods, of which research involves multiple disciplines. Dysmenorrhea is a pain caused by uterine muscle spasms or organic lesions. Therefore, obstetrics and gynecology is the most important subject category of dysmenorrhea, which can directly indicate the pathological characteristics of dysmenorrhea.
Integrative and complementary medicine, general and internal medicine, pharmacology and pharmacy, neurosciences and neurology, and reproductive biology are also important disciplines for dysmenorrhea. The subject areas include mechanism exploration, incentive analysis, treatment and efficacy, clinical trials, and other aspects. In addition, public, environmental and occupational health is also a subject that cannot be ignored, including epidemiological investigation of dysmenorrhea, and health management.
Keywords
Figures 8–10 are the charts related to the keywords we exported. Keywords are used to express the theme and research direction of articles. Figure 8 shows the main keywords of the literature we collected and the complex relationship network between them. We used CiteSpace to filter articles related to keywords. We used dysmenorrhea as the key word to filter different expressions of dysmenorrheal, dysmenorrhoea, dysmenorrhea, menalgia, and dysmenorrheic. Table 6 shows the 20 most popular keywords. Among them, “women”, “adolescent”, “pain”, “menstrual pain” and “pelvic pain” were found to be the basic features of dysmenorrhea; “primary dysmenorrhea” and “endometriosis” represent different pathogenic mechanisms of dysmenorrhea; “efficacy” and “double blind” relate to studies on the efficacy of dysmenorrhea drugs; and “prevalence”, “management”, “quality of life”, “impact”, etc., are related to epidemiology, self-health management and other aspects. These are the most important keywords.
 |
Figure 9 Clustered networks of keywords. Each color represents a cluster. The smaller the clustering label, the more articles in the cluster. |
 |
Table 6 The Top 20 Keywords Related to Dysmenorrhea from 1992 to 2022 |
Clustering tags are important noun phrases extracted from article titles. We used CiteSpace to construct a visual network map and analyze co-occurrence keyword clustering to obtain the status of each research topic of dysmenorrhea from 1992 to 2022. As shown in Figure 9, the co-occurrence keywords were divided into 15 groups, including # 0 minor analgesics, # 1 dysfunctional uterine bleeding, # 2 prospective study, # 3 childhood adversity, # 4 possible role, # 5 preterm labor, # 6 auricular acupressure, # 7 si-wu decoction, # 8 somatothermal far-infrared ray, # 9 laparoscopic presacral neurectomy, # 10 functional connectivity, # 11 healthy condition, # 12 systematic review, # 13 oral contraceptive, and # 14 skin temperature response.
We also conducted keywords burst detection; that is, keywords that have been cited many times in a certain period are usually considered indicators of cutting-edge topics. According to Figure 10, young women have a high outbreak intensity. Younger women, intrauterine pressure, cigarette smoking and naproxen sodium last the longest. The earliest keywords were in 1994: young women, prostaglandin, and intrauterine pressure. Moreover, basically every one or two years, new salient keywords emerged. After 2015, mefenamic acid, population, herbal medicine and functional connectivity gradually came into use. The results indicate that researchers are further exploring other mechanisms and treatment methods of dysmenorrhea while paying more attention to group research.
Analysis of Reference Co-Citation Network
The co-citation of literature as a research method to measure the relationship between documents was first proposed by American intelligence scientist Henry Small in 1973.31 We used CiteSpace to analyze the co-cited articles and obtained the network of co-cited references, the timeline map and the charts of the top ten most frequently cited articles. We found that the top 8 most cited documents can be classified into two categories: the first is a consensus guide for dysmenorrhea, and the second is a common treatment plan. These articles provide sufficient and reliable theoretical support for us to understand the mechanism, impact and clinical treatment of dysmenorrhea, which is convenient for us to study dysmenorrhea. We hope to identify influential and landmark research on dysmenorrhea through co-citation literature analysis.
We selected the top ten most frequently cited articles and tabulated their first authors, titles and publication years, citations, DOI and publishers (Table 7). These ten articles represent different types, including six papers and four review articles. Among them, the most frequently cited is the literature published by Riley, JL: A meta-analytic review of pain perception across the menstrual cycle. This article reviews and summarizes the correlation between women’s menstrual cycle stages and experimentally induced pain perception in previous studies and confirms the conclusion that the menstrual cycle has a significant impact on human pain perception. It also systematically analyzes the article and raises issues that have not been addressed or noted in the article, such as whether subjects have clinical pain syndrome.32 The second most cited article is Primary dysmenorrhea - Advances in pathogenesis and management by Dawood, MY in obstetrics and gynecology. This article introduces the prevalence, pathogenesis, treatment, and detection methods of dysmenorrhea, providing convenience for the understanding and management of primary dysmenorrhea.33 Next is What we know about primary dysmenorrhea today: a critical review by Iacovides, S at Human Reproduction Update. Compared to the previous article, the author added a study on the effects and consequences of recurrent menstrual pain on pain sensitivity, mood, quality of life, and sleep in women with primary dysmenorrhea and concluded that the quality of life in women with primary dysmenorrhea significantly decreased during menstruation, with poor mood.34 In addition, Chapron, C’s article published in Human Reproduction on Deep infiltrating endometriosis: relation between severity of dysmenorrhoea and extent of disease examined other variables associated with more severe PD and confirmed that the extent of subperitoneal infiltration and extensive attachment were the only factors associated with the severity of PD.35
 |
Table 7 The Top 10 Most Highly Cited Documents in the Field of Dysmenorrhea |
The timeline view reflects the time span over which the literature was cited. Each line is a collection of similar articles, so the novelty and continuity of the research topic can be determined. Figure 11 shows the 10 components of 985 cited papers clustered by keywords, including # 0 moxibustion, # 1 randomized controlled trial, # 2 functional connectivity, # 3 Ghana, # 4 nonsteroidal anti-inflammatory drugs, # 5 dienogest, # 6 migraine, # 7 school absences, # 8 naproxen sodium, # 9 fennel extract. The higher the cluster tag is, the more documents are referenced. According to Figure 11, we find that the earliest research hotspot is naproxen sodium, a nonsteroidal anti-inflammatory drug. NSAIDs can relieve dysmenorrhea in most women, one of which is naproxen sodium.40 With the gradual increase in the number of published papers on dysmenorrhea, coupled with the emphasis on the study of the causes and clinical mechanisms of dysmenorrhea, dienogest, functional connectivity, randomized controlled trials, the relationship between migraine and dysmenorrhea, etc., gradually became research hotspots between 2010 and 2015. At the same time, with the continuous development and promotion of traditional Chinese medicine, Chinese herbal medicine and some traditional Chinese medicine treatment methods gradually entered people’s vision and have been applied to the relief treatment of dysmenorrhea. Since 2015, moxibustion has gradually become a research hotspot, and the number of studies has gradually increased in the past two year.
Discussion
General Information
In this study, we screened the literature in the field of dysmenorrhea in WOSCC and ultimately selected 1012 studies. Through the combination of bibliometrics and visual analysis, we studied the overall research content, research hotspots and development trends of dysmenorrhea in the past 30 years.
Dysmenorrhea has always been the most common gynecological disease, and it is also a disease with a high incidence. However, few women with dysmenorrhea have sought medical treatment in the past, and so people have not paid much attention to it. However, with the development of society, people’s awareness has begun to change, and increasing attention has been given to gynecological diseases. During the 30 years from 1992 to 2022, the total number of published studies increased, and the growth rate increased year by year. There were great differences in the number of literature publications in various countries, and their development trends were also different. Judging from the publishing trend in the current year, China and the United States are globally leading dysmenorrhea research, with China achieving a higher influence in the research due to its larger annual increase of academic publications.
It has become increasingly common for different countries, institutions and authors participate in joint research. To date, the United States is the most active country in cooperation and has cooperated with 25 countries 56 times. The top 3 cooperating institutions are Beijing University of Chinese Medicine, Chengdu University of Traditional Chinese Medicine, and National Yang-Ming Chiao Tung University. Six of the top 10 institutions are from China, indicating that China occupies an important position in international cooperation. The perspective of institutional cooperation networks indicates that most institutions are still more inclined to cooperate with domestic institutions, and international cooperation still needs to be strengthened. In any case, such cooperation will further promote academic progress and exchanges and contribute to further research on dysmenorrhea.
Research Hotspots
Keywords co-occurrence analysis and clustering can reflect the research hotspots in related fields. Through the visualized map, four related research hotspots can be found: pathogenesis, epidemiology, self-management and treatment.
Pathogenesis
The first theme is pathogenesis. Dysmenorrhea is classified into PD and SD, and there are essential differences between them. At present, modern medicine has recognized that increased prostaglandin is the main pathogenesis of PD and has been widely accepted. A large number of research papers on the mechanism of dysmenorrhea have been published.3,34 Oxytocin,41,42 Leukotriene,43,44 β-endorphin,45 and psychological factors46 have also been shown to be associated with dysmenorrhea, but there seems to be little research on them. It is noteworthy that the mechanism of the effect of serum vasopressin on dysmenorrhea is still controversial. Ekstrom believes that elevated serum vasopressin can lead to vasoconstriction and pathological uterine contraction.47,48 However, Valentin believes that vasopressin has nothing to do with the pathogenesis of dysmenorrhea.49 Ekstrom’s study contained ten healthy nulliparous women, and Valentin’s study contained eight nulligravida with primary dysmenorrhea and eight nulligravida controls. The number of subjects in both groups was small, which may lead to the differentiation of conclusions. Further studies need to expand the sample size to prove that there is a correlation between serum vasopressin and dysmenorrhea. The pathogenesis of SD is different due to the different diseases that cause pain. A study proved that the most common cause of SD is endometriosis.4 Keyword analysis showed that the frequency of endometrium was high, which confirmed its popularity in recent years. In existing studies, it is hypothesized that the postulated origins of endometriotic tissue are retrograde menstruation, coelomic metaplasia, and lymphatic and vascular metastasis. Retrograde transplants of endometrial tissue and cells attach to the surface of the peritoneum, invading nearby structures and causing an inflammatory response that can lead to dysmenorrhea.50,51 Research related to pain and risk factors for dysmenorrhea52 has been used to study the effects and management strategies of PD in college students.23
Epidemiology and Self-Management
The epidemiology of dysmenorrhea and self-management research is also a hot spot. Many countries have studied the incidence of dysmenorrhea in people of different occupations and ages.53–55 These studies aim to support epidemiologists in understanding disease-related patterns of occurrence, thereby helping to inform research on the etiology, risk factors and treatment of dysmenorrhea. It also helps to develop targeted and effective prevention programs, design more reliable diagnostic models and interventions, and guide protocols appropriate for dysmenorrhea research and treatment. According to the study, different ages and different regions of women have different prevalence. Among them, the prevalence in young women is generally higher.55,56 No more than 30% of women seek help from a doctor when they have dysmenorrhea.57 Approximately 70% of women practice self-management.58,59 In women’s self-management of dysmenorrhea, they use bed rest, herbal preparations, heating pads, and dietary supplements, which can relieve the symptoms of most people.60 Among them, the use of heat is a popular measure. Heating pads have a significant effect on the lower abdomen.61,62 Drinking tea is also one of the self-management methods used by many women experiencing dysmenorrhea,63 but there is still controversy about whether it alleviates or aggravates dysmenorrhea.64,65 After studying different types of tea drinking, some scholars found that moderate drinking of green tea and oolong tea could alleviate dysmenorrhea, while black tea aggravates it.66 In addition, smartphone apps are also used to help women relieve dysmenorrhea.67,68 During our analysis, we found that a large part of the epidemiological research subjects were young women, which may be because dysmenorrhea symptoms will slow down or disappear with age.9 There are few epidemiological studies on SD and no comprehensive description, so it is difficult to evaluate and judge.
Treatment
At present, the most commonly used treatment for dysmenorrhea is nonsteroidal anti-inflammatory drugs (NSAIDs).50 NSAIDs exert their effect by blocking the production of prostaglandins, which play a role by inhibiting cyclooxygenase (COX). NSAIDs include the common painkillers aspirin, naproxen, ibuprofen, and mefenamic acid.69 Researchers such as Jane Marjoribanks have systematically studied the efficacy and safety of NSAIDs, which provides strong evidence for NSAIDs as the first-line treatment for PD.70,71 For women whose nonsteroidal anti-inflammatory drugs do not reduce dysmenorrhea, hormone therapy is optional, including a combination of oral contraceptives, injectable contraceptive depot medroxyprogesterone acetate (DMPA), and other long-acting progestin-only hormonal contraceptives (such as Mirena LNG-IUS). The most widely used are combined oral contraceptives (OCPs).72 Aslam N’s study has shown that there is a 92% improvement in dysmenorrhea with the LNG-IUS.73 In addition, research on traditional Chinese medicine and herbal medicine for dysmenorrhea treatment has also been a hotspot in recent years.74 Among them, Shaofu-Zhuyu decoction can effectively relieve menstrual pain.75,76 Transcutaneous electrical nerve stimulation, acupuncture, and surgical interventions have also been shown to relieve menstrual pain.77,78 The effect of acupuncture proved to be significant and rapid.79 Moxibustion is also used to treat dysmenorrhea, but Yang Mingxiao and other researchers believe that the effectiveness of moxibustion in treating menstrual pain cannot exclude the influence of psychological factors.80 Note that as traditional Chinese medical treatments, acupuncture and moxibustion need dialectical typing as the basis.
Research Frontiers
In recent years, the increased prevalence of “herbal medicine” and “functional connectivity” has emphasized the importance of both. Herbal medicine, as an ancient method of health care, has been widely used throughout human history. Currently, there is still a certain failure rate in the conventional treatment of dysmenorrhea, which is contraindicated or intolerant for some women. Herbal therapy, as a complementary and alternative medicine, has received increasing scholarly attention in recent years and has been shown to have a better effect.81,82 Among them, Chinese herbal medicine is one of the most widely used herbal treatments, and the herbal prescription contains a unique herbal formula that can effectively treat dysmenorrhea by eliminating qi stagnation, dissolving blood stasis, and decomposing masses in blood vessels, thus promoting the flow of Qi and blood.83 Categories of herbs such as herbs “regulating the Qi and Blood”, “warming the Interior”, “tonifying the Kidney and Liver” and “reinforcing Qi and Blood” are most commonly used, and clinical practice proves that TCM has an effective duration of up to three months.84,85 Dang-Gui-Shao-Yao-San, Si-Wu-Tang and their appendages are commonly used formulas after preliminary clinical experiments demonstrating their efficacy.86,87 Some commonly used Chinese herbal medicines, such as Corydalis Rhizoma (Yanhusuo) and Cyperi Rhizoma (Xiangfu), have multitarget effects on primary dysmenorrhea, such as analgesia, emotion regulation, and hormone regulation.85,88 Currently, some promising evidence has been found to support the use of herbal medicine for the treatment of primary dysmenorrhea. RCTs have shown beneficial effects of Chinese herbal medicine on pain compared with placebo control, such as Ge-Gen decoction, Si-Wu-Tang and Dang-Gui-Shao-Yao-San.84,86,89,90 However, there is still a lack of consistent and systematic evidence-based data to support efficacy and safety.
The study of the relationship between dysmenorrhea and functional connectivity between brain regions is receiving increasing attention. Primary dysmenorrhea is characterized by menstrual spasms without organic lesions, and there have been several findings suggesting that periodic menstrual pain is associated with structural and functional changes in relevant areas of the brain.91–93 Current studies of functional connectivity have focused on the interactive interactions between primary dysmenorrhea and the neural central mechanisms associated with it. For example, the results from Cheng-Hao Tu and his team demonstrate that abnormal gray matter volume changes are present in PD patients. These changes may underpin a combination of impaired pain inhibition, increased pain facilitation and increased affect.94 There are also research teams that explore the mechanism and effectiveness of treatments through related central mechanisms.95,96 The increase in functional connections has continued since 2017 and is a leading edge in the field of dysmenorrhea in recent years. At present, the mechanisms linking primary dysmenorrhea to altered neural centers are in their infancy, and future research will continue.
Limitations
First, we only searched the relevant literature in WOSCC, which may lead to the omission of articles from other sources. Because the WOS is an English language database, it may omit other literature related to dysmenorrhea. Second, the screening process of articles was manual, and there may be deviations in understanding, leading to the omission of some documents. In addition, dysmenorrhea is classified as PD and SD. SD is caused by pelvic organic diseases, and most of its research focuses on diseases. We screen dysmenorrhea as a disease rather than a symptom, so we may have omitted some important literature.
Conclusions
This study systematically summarizes and analyzes the research progress of dysmenorrhea in various countries, institutions, disciplines and researchers from 1992 to 2022 by means of bibliometrics. The literature on dysmenorrhea is increasing yearly. Prostaglandins are the main pathogenesis of dysmenorrhea, which has been widely recognized by the academic community. However, the mechanism of other substances affecting dysmenorrhea is not completely clear, such as serum vasopressin, which needs further research.
At present, the effect of NSAIDs on dysmenorrhea has been widely recognized. However, there is no clear treatment plan for patients who experience no effect on NSAIDs. Traditional Chinese medicine (such as acupuncture or moxibustion, prescriptions of traditional Chinese medicine) is used as a complementary and alternative medicine and has been proven to have a good therapeutic effect on dysmenorrhea. However, due to the difference in thinking and theoretical basis between Chinese traditional medicine and Western medicine, there is less combination between the two and a lack of strong evidence. In general, the research in this paper is based on the existing dysmenorrhea literature database. The treatment plan for dysmenorrhea in patients with ineffective nonsteroidal anti-inflammatory drugs and the treatment of traditional Chinese medicine need further research, hoping to aid the future research of dysmenorrhea.
Abbreviations
PD, primary dysmenorrhea; SD, secondary dysmenorrhea; PGF2α, prostaglandin F2α; NSAIDs, nonsteroidal anti-inflammatory drugs; TENS, transcutaneous electrical nerve stimulation; LUNA, laparoscopic uterosacral nerve association; PSN, presacral neurectomy; LNG-IUS, levonorgestrel releasing intrauterine system; WOSCC, Web of Science core collection; SCI-EXPANDED, Science Citation Index Expanded; IF, impact factors; JCR, journal citation reports; NSAIDs, nonsteroidal anti-inflammatory drugs; COX, cyclooxygenase; DMPA, depot medroxyprogesterone acetate; OCPs, oral contraceptives.
Acknowledgments
This work was supported by the Three-year Action Plan for Shanghai [project number: ZY (2021-2023)-0211]; National Natural Science Foundation of China (81973730); Local Colleges Faculty Constitution of Shanghai MSTC 2022 (22010504300); and Shanghai Collaborative Innovation Center for Chronic Disease Prevention and Health Services (2021 Science and Technology 02-37).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
None of the authors have conflicts of interest with respect to this work.
References
1. Voto SJ, Essig GF. Primary dysmenorrhea: current concepts. Ohio State Med J. 1984;80(8):606–609.
2. Osayande AS, Mehulic S. Diagnosis and initial management of dysmenorrhea. Am Fam Physician. 2014;89(5):341–346.
3. Ferries-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: diagnosis and therapy. Obstet Gynecol. 2020;136(5):1047–1058. doi:10.1097/AOG.0000000000004096
4. Guimaraes I, Povoa AM. Dismenorreia primaria: avaliacao e tratamento. Primary dysmenorrhea: assessment and treatment. Rev Bras Ginecol Obstet. 2020;42(8):501–507. doi:10.1055/s-0040-1712131
5. Wolf LL, Schumann L. Dysmenorrhea. J Am Acad Nurse Pract. 1999;11(3):125–30; quiz 131–3. doi:10.1111/j.1745-7599.1999.tb00549.x
6. Dawood MY. Nonsteroidal anti-inflammatory drugs and changing attitudes toward dysmenorrhea. Am J Med. 1988;84(5A):23–29. doi:10.1016/0002-9343(88)90473-1
7. Funk CD. Prostaglandins and leukotrienes: advances in eicosanoid biology. Science. 2001;294(5548):1871–1875. doi:10.1126/science.294.5548.1871
8. Harel Z. Dysmenorrhea in adolescents and young adults: from pathophysiology to pharmacological treatments and management strategies. Expert Opin Pharmacother. 2008;9(15):2661–2672. doi:10.1517/14656566.9.15.2661
9. Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Article. Epidemiol Rev. 2014;36(1):104–113. doi:10.1093/epirev/mxt009
10. Hu Z, Tang L, Chen L, Kaminga AC, Xu HL. Prevalence and risk factors associated with primary dysmenorrhea among Chinese Female University Students: a cross-sectional study. Article. J Pediatr Adolesc Gynecol. 2020;33(1):15–22. doi:10.1016/j.jpag.2019.09.004
11. Jang IA, Kim MY, Lee SR, Jeong KA, Chung HW. Factors related to dysmenorrhea among Vietnamese and Vietnamese marriage immigrant women in South Korea. Obstetr Gynecol Sci. 2013;56(4):242–248. doi:10.5468/ogs.2013.56.4.242
12. Soderman L, Edlund M, Marions L. Prevalence and impact of dysmenorrhea in Swedish adolescents. Article. Acta Obstet Gynecol Scand. 2019;98(2):215–221. doi:10.1111/aogs.13480
13. Jiang W, Hua XG, Hu CY, Li FL, Huang K, Zhang XJ. The prevalence and risk factors of menstrual pain of married women in Anhui Province, China. Article. Eur J Obstet Gynecol Reprod Biol. 2018;229:190–194. doi:10.1016/j.ejogrb.2018.09.002
14. Schoep ME, Adang EMM, Maas JWM, De Bie B, Aarts JWM, Nieboer TE. Productivity loss due to menstruation-related symptoms: a nationwide cross-sectional survey among 32 748 women. Article. BMJ Open. 2019;9(6):
15. Iacovides S, Avidon I, Bentley A, Baker FC. Reduced quality of life when experiencing menstrual pain in women with primary dysmenorrhea. Acta Obstet Gynecol Scand. 2014;93(2):213–217. doi:10.1111/aogs.12287
16. Al-Jefout M, Seham A, Jameel H, et al. Dysmenorrhea: prevalence and impact on quality of life among young adult Jordanian females. J Pediatr Adolesc Gynecol. 2015;28(3):173–185. doi:10.1016/j.jpag.2014.07.005
17. Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adol Med. 2000;154(12):1226–1229. doi:10.1001/archpedi.154.12.1226
18. Sima RM, Sulea M, Radosa JC, et al. The prevalence, management and impact of dysmenorrhea on medical students’ lives-a multicenter study. Healthcare. 2022;10(1):157. doi:10.3390/healthcare10010157
19. World Health Organization. WHO statement on menstrual health and rights. World Health Organization. Available from: https://www.who.int/news/item/22-06-2022-who-statement-on-menstrual-health-and-rights.
20. Vercellini P, Vigano P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261–275. doi:10.1038/nrendo.2013.255
21. Sachedina A, Todd N. Dysmenorrhea, endometriosis and chronic pelvic pain in adolescents. J Clin Res Pediatr Endocrinol. 2020;12(Suppl 1):7–17. doi:10.4274/jcrpe.galenos.2019.2019.S0217
22. De Sanctis V, Soliman A, Bernasconi S, et al. Primary dysmenorrhea in adolescents: prevalence, impact and recent knowledge. Pediatr Endocrinol Rev. 2015;13(2):512–520.
23. Durand H, Monahan K, McGuire BE. Prevalence and impact of dysmenorrhea among university students in Ireland. Article. Pain Med. 2021;22(12):2835–2845. doi:10.1093/pm/pnab122
24. Bianchi P, Guo SW, Habiba M, Benagiano G. Utility of the levonorgestrel-releasing intrauterine system in the treatment of abnormal uterine bleeding and dysmenorrhea: a narrative review. J Clin Med. 2022;11(19):5836. doi:10.3390/jcm11195836
25. Zhang Y, Porter AL, Cunningham S, Chiavetta D, Newman N. Parallel or intersecting lines? Intelligent bibliometrics for investigating the involvement of data science in policy analysis. IEEE Trans Eng Manage. 2021;68(5):1259–1271. doi:10.1109/tem.2020.2974761
26. van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Article. Scientometrics. 2010;84(2):523–538. doi:10.1007/s11192-009-0146-3
27. Chen CM. Searching for intellectual turning points: progressive knowledge domain visualization. Article; Proceedings Paper. Proc Natl Acad Sci U S A. 2004;101:5303–5310. doi:10.1073/pnas.0307513100
28. Fu L, Lv H, Li Z. Research trends of acupuncture therapy on dysmenorrhea from 2002 to 2022: a bibliometric analysis. Biotechnol Genet Eng Rev. 2023;1–20. doi:10.1080/02648725.2023.2202539
29. Liu Z, Li Z, Meng Q, Gu Z, Cui J. Bibliometric analysis of global research landscape and hotspots on dysmenorrhea: where are we now? J Pain Res. 2023;16:269–285. doi:10.2147/JPR.S396083
30. Li W, Yang G, Tian W, et al. Bibliometric and visual analysis of nocturnal enuresis from 1982 to 2022. Front Pediatr. 2022;10:972751. doi:10.3389/fped.2022.972751
31. Henry S. Co-citation in the scientific literature: a new measure of the relationship between two documents. J Am Soc Inf Sci. 1973;24(4):265–269. doi:10.1002/asi.4630240406
32. Riley JL, Robinson ME, Wise EA, Price D. A meta-analytic review of pain perception across the menstrual cycle. Pain. 1999;81(3):225–235. doi:10.1016/S0304-3959(98)00258-9
33. Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428–441. doi:10.1097/01.AOG.0000230214.26638.0c
34. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762–778. doi:10.1093/humupd/dmv039
35. Chapron C, Fauconnier A, Dubuisson JB, Barakat H, Vieira M, Breart G. Deep infiltrating endometriosis: relation between severity of dysmenorrhoea and extent of disease. Hum Reprod. 2003;18(4):760–766. doi:10.1093/humrep/deg152
36. Jamieson DJ, Steege JF. The prevalence of dysmenorrhea, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol. 1996;87(1):55–58. doi:10.1016/0029-7844(95)00360-6
37. Proctor M, Farquhar C. Diagnosis and management of dysmenorrhoea. BMJ. 2006;332(7550):1134–1138. doi:10.1136/bmj.332.7550.1134
38. French L. Dysmenorrhea. Am Fam Physician. 2005;71(2):285–291.
39. Vercellini P, Frontino G, De Giorgi O, Pietropaolo G, Pasin R, Crosignani PG. Continuous use of an oral contraceptive for endometriosis-associated recurrent dysmenorrhea that does not respond to a cyclic pill regimen. Fertil Steril. 2003;80(3):560–563. doi:10.1016/s0015-0282(03)00794-5
40. Oladosu FA, Tu FF, Hellman KM. Nonsteroidal antiinflammatory drug resistance in dysmenorrhea: epidemiology, causes, and treatment. Am J Obstet Gynecol. 2018;218(4):390–400. doi:10.1016/j.ajog.2017.08.108
41. Guo SW, Mao XY, Ma QL, Liu XS. Dysmenorrhea and its severity are associated with increased uterine contractility and overexpression of oxytocin receptor (OTR) in women with symptomatic adenomyosis. Fertil Steril. 2013;99(1):231–240. doi:10.1016/j.fertnstert.2012.08.038
42. Liedman R, Hansson SR, Howe D, et al. Reproductive hormones in plasma over the menstrual cycle in primary dysmenorrhea compared with healthy subjects. Gynecol Endocrinol. 2008;24(9):508–513. doi:10.1080/09513590802306218
43. Harel Z, Lilly C, Riggs S, Vaz R, Drazen J. Urinary leukotriene (LT) E(4) in adolescents with dysmenorrhea: a pilot study. J Adolesc Health. 2000;27(3):151–154. doi:10.1016/s1054-139x(00)00123-3
44. Abu JI, Konje JC. Leukotrienes in gynaecology: the hypothetical value of anti-leukotriene therapy in dysmenorrhoea and endometriosis. Hum Reprod Update. 2000;6(2):200–205. doi:10.1093/humupd/6.2.200
45. Marchini M, Manfredi B, Tozzi L, Sacerdote P, Panerai A, Fedele L. Mitogen-induced lymphocyte proliferation and peripheral blood mononuclear cell beta-endorphin concentrations in primary dysmenorrhoea. Hum Reprod. 1995;10(4):815–817. doi:10.1093/oxfordjournals.humrep.a136045
46. Li YZ, Kang BX, Zhao XY, Cui XN, Chen J, Wang LJ. Association between depression and dysmenorrhea among adolescent girls: multiple mediating effects of binge eating and sleep quality. BMC Womens Health. 2023;23(1). doi:10.1186/s12905-023-02283-6
47. Akerlund M. Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog Brain Res. 2002;139:359–365.
48. Ekstrom P, Akerlund M, Forsling M, Kindahl H, Laudanski T, Mrugacz G. Stimulation of vasopressin release in women with primary dysmenorrhea and after oral-contraceptive treatment - effect on uterine contractility. Brit J Obstet Gynaec. 1992;99(8):680–684. doi:10.1111/j.1471-0528.1992.tb13855.x
49. Valentin L, Sladkevicius P, Kindahl H, Broeders A, Marsal K, Melin P. Effects of a vasopressin antagonist in women with dysmenorrhea. Gynecol Obstet Invest. 2000;50(3):170–177. doi:10.1159/000010319
50. French L. Dysmenorrhea in adolescents: diagnosis and treatment. Paediatr Drugs. 2008;10(1):1–7. doi:10.2165/00148581-200810010-00001
51. Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382(13):1244–1256. doi:10.1056/NEJMra1810764
52. Nohara M, Momoeda M, Kubota T, Nakabayashi M. Menstrual cycle and menstrual pain problems and related risk factors among Japanese Female Workers. Ind Health. 2011;49(2):228–234. doi:10.2486/indhealth.MS1047
53. Ohde S, Tokuda Y, Takahashi O, Yanai H, Hinohara S, Fukui T. Dysmenorrhea among Japanese women. Int J Gynecol Obstet. 2008;100(1):13–17. doi:10.1016/j.ijgo.2007.06.039
54. Bakhsh H, Algenaimi E, Aldhuwayhi R, AboWadaan M. Prevalence of dysmenorrhea among reproductive age group in Saudi Women. BMC Womens Health. 2022;22(1). doi:10.1186/s12905-022-01654-9
55. Hadjou OK, Jouannin A, Lavoue V, Leveque J, Esvan M, Bidet M. Prevalence of dysmenorrhea in adolescents in France: results of a large cross-sectional study. J Gynecol Obstet Hum. 2022;51(3). doi:10.1016/j.jogoh.2021.102302
56. Dos Santos LB, Barbosa IR, Dantas THD, et al. Prevalence of primary dysmenorrhea and associated factors in adult women. Rev Assoc Med Bras. 2022;68(1):31–36. doi:10.1590/1806-9282.20210341
57. Chen L, Tang L, Guo SY, Kaminga AC, Xu HL. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019;9(9):e026813. doi:10.1136/bmjopen-2018-026813
58. Chia CF, Lai JHY, Cheung PK, et al. Dysmenorrhoea among Hong Kong university students: prevalence, impact, and management. Hong Kong Med J. 2013;19(3):222–228. doi:10.12809/hkmj133807
59. Chen CX, Kwekkeboom KL, Ward SE. Beliefs about dysmenorrhea and their relationship to self-management. Res Nurs Health. 2016;39(4):263–276. doi:10.1002/nur.21726
60. Ameade EPK, Amalba A, Mohammed BS. Prevalence of dysmenorrhea among University students in Northern Ghana; its impact and management strategies. BMC Womens Health. 2018;18(1):39. doi:10.1186/s12905-018-0532-1
61. Hong YR. Effects of heat therapy using a far infrared rays heating element for dysmenorrhea in high school girls. J Korean Acad Nurs. 2011;41(1):141–148. doi:10.4040/jkan.2011.41.1.141
62. Abubakar U, Zulkarnain AI, Samri F, et al. Use of complementary and alternative therapies for the treatment of dysmenorrhea among undergraduate pharmacy students in Malaysia: a cross sectional study. BMC Complement Med. 2020;20(1). doi:10.1186/s12906-020-03082-4
63. Pattanittum P, Kunyanone N, Brown J, et al. Dietary supplements for dysmenorrhoea. Cochrane Database Syst Rev. 2016;3(3):CD002124. doi:10.1002/14651858.CD002124.pub2
64. Al-Husban N, Odeh O, Dabit T, Masadeh A. The influence of lifestyle variables on primary dysmenorrhea: a cross-sectional study. Int J Womens Health. 2022;14:545–553. doi:10.2147/Ijwh.S338651
65. Mesele TT, Dheresa M, Oljira L, Wakwoya EB, Gemeda GM. Prevalence of dysmenorrhea and associated factors among Haramaya University Students, Eastern Ethiopia. Int J Womens Health. 2022;14:517–527. doi:10.2147/Ijwh.S333447
66. Zhang X, Zhang R, Chen D, et al. Association of tea drinking and dysmenorrhoea among reproductive-age women in Shanghai, China (2013–2015): a cross-sectional study. BMJ Open. 2019;9(4):e026643. doi:10.1136/bmjopen-2018-026643
67. Blodt S, Pach D, von Eisenhart-Rothe S, et al. Effectiveness of app-based self-acupressure for women with menstrual pain compared to usual care: a randomized pragmatic trial. Obstet Gynecol Surv. 2018;73(6):348–350. doi:10.1097/OGX.0000000000000558
68. Blodt S, Witt CM, Holmberg C. Women’s reasons for participation in a clinical trial for menstrual pain: a qualitative study. BMJ Open. 2016;6(12):e012592. doi:10.1136/bmjopen-2016-012592
69. Barcikowska Z, Rajkowska-Labon E, Grzybowska ME, Hansdorfer-Korzon R, Zorena K. Inflammatory markers in dysmenorrhea and therapeutic options. Int J Environ Res Public Health. 2020;17(4):1191. doi:10.3390/ijerph17041191
70. Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Db Syst Rev. 2015;7. doi:10.1002/14651858.CD001751.pub3
71. Karout S, Soubra L, Rahme D, Karout L, Khojah HMJ, Itani R. Prevalence, risk factors, and management practices of primary dysmenorrhea among young females. BMC Womens Health. 2021;21(1). doi:10.1186/s12905-021-01532-w
72. Harel Z. Dysmenorrhea in adolescents and young adults: an update on pharmacological treatments and management strategies. Expert Opin Pharmaco. 2012;13(15):2157–2170. doi:10.1517/14656566.2012.725045
73. Aslam N, Blunt S, Latthe P. Effectiveness and tolerability of levonorgestrel intrauterine system in adolescents. J Obstet Gynaecol. 2010;30(5):489–491. doi:10.3109/01443615.2010.484107
74. Gao L, Xiao ZR, Jia CH, Wang W. A comparison of the efficacy of Chinese herbal medicines in the treatment of primary dysmenorrhea A network meta-analysis protocol. Medicine. 2019;98(14). doi:10.1097/MD.0000000000015100
75. Huang X, Su S, Duan JA, et al. Effects and mechanisms of Shaofu-Zhuyu decoction and its major bioactive component for Cold - Stagnation and Blood - Stasis primary dysmenorrhea rats. J Ethnopharmacol. 2016;186:234–243. doi:10.1016/j.jep.2016.03.067
76. Lee H, Choi TY, Myung CS, Lee JA, Lee MS. Herbal medicine (Shaofu Zhuyu decoction) for treating primary dysmenorrhea: a systematic review of randomized clinical trials. Maturitas. 2016;86:64–73. doi:10.1016/j.maturitas.2016.01.012
77. Wang SF, Lee JP, Hwa HL. Effect of transcutaneous electrical nerve stimulation on primary dysmenorrhea. Neuromodulation. 2009;12(4):302–309. doi:10.1111/j.1525-1403.2009.00226.x
78. Smith CA, Armour M, Zhu XS, Li X, Lu ZY, Song J. Acupuncture for dysmenorrhoea. Cochrane Db Syst Rev. 2016;4. doi:10.1002/14651858.CD007854.pub3
79. Armour M, Dahlen HG, Zhu X, Farquhar C, Smith CA, Scherer RW. The role of treatment timing and mode of stimulation in the treatment of primary dysmenorrhea with acupuncture: an exploratory randomised controlled trial. PLoS One. 2017;12(7):e0180177. doi:10.1371/journal.pone.0180177
80. Yang M, Chen X, Bo L, et al. Moxibustion for pain relief in patients with primary dysmenorrhea: a randomized controlled trial. PLoS One. 2017;12(2):e0170952. doi:10.1371/journal.pone.0170952
81. Fisher C, Adams J, Hickman L, Sibbritt D. The use of complementary and alternative medicine by 7427 Australian women with cyclic perimenstrual pain and discomfort: a cross-sectional study. BMC Complem Altern M. 2016;16(1). doi:10.1186/s12906-016-1119-8
82. Nahid K, Fariborz M, Ataolah G, Solokian S. The effect of an Iranian herbal drug on primary dysmenorrhea: a clinical controlled trial. J Midwifery Wom Heal. 2009;54(5):401–404. doi:10.1016/j.jmwh.2008.12.006
83. Jia W, Wang X, Xu D, Zhao A, Zhang Y. Common traditional Chinese medicinal herbs for dysmenorrhea. Phytother Res. 2006;20(10):819–824. doi:10.1002/ptr.1905
84. Zhu X, Proctor M, Bensoussan A, Wu E, Smith CA. Chinese herbal medicine for primary dysmenorrhoea. Cochrane Database Syst Rev. 2008;2:CD005288. doi:10.1002/14651858.CD005288.pub3
85. Chen HY, Lin YH, Su IH, Chen YC, Yang SH, Chen JL. Investigation on Chinese herbal medicine for primary dysmenorrhea: implication from a nationwide prescription database in Taiwan. Complement Ther Med. 2014;22(1):116–125. doi:10.1016/j.ctim.2013.11.012
86. Lee HW, Jun JH, Kil KJ, Ko BS, Lee CH, Lee MS. Herbal medicine (Danggui Shaoyao San) for treating primary dysmenorrhea: a systematic review and meta-analysis of randomized controlled trials. Maturitas. 2016;85:19–26. doi:10.1016/j.maturitas.2015.11.013
87. Yeh LL, Liu JY, Lin KS, et al. A randomised placebo-controlled trial of a traditional Chinese herbal formula in the treatment of primary dysmenorrhoea. PLoS One. 2007;2(8):e719. doi:10.1371/journal.pone.0000719
88. Liu P, Duan J, Wang P, et al. Biomarkers of primary dysmenorrhea and herbal formula intervention: an exploratory metabonomics study of blood plasma and urine. Mol Biosyst. 2013;9(1):77–87. doi:10.1039/c2mb25238d
89. Ji HR, Park KS, Woo HL, et al. Herbal medicine (Taohong Siwu Tang) for the treatment of primary dysmenorrhea: a systematic review and meta-analysis. Explore-NY. 2020;16(5):297–303. doi:10.1016/j.explore.2020.05.013
90. Chai CZ, Hong F, Yan Y, et al. Effect of traditional Chinese medicine formula GeGen decoction on primary dysmenorrhea: a randomized controlled trial study. J Ethnopharmacol. 2020;261:113053. doi:10.1016/j.jep.2020.113053
91. Jin L, Yang X, Liu P, et al. Dynamic abnormalities of spontaneous brain activity in women with primary dysmenorrhea. J Pain Res. 2017;10:699–707. doi:10.2147/JPR.S121286
92. Tu CH, Niddam DM, Yeh TC, et al. Menstrual pain is associated with rapid structural alterations in the brain. Pain. 2013;154(9):1718–1724. doi:10.1016/j.pain.2013.05.022
93. Liu P, Liu Y, Wang G, et al. Changes of functional connectivity of the anterior cingulate cortex in women with primary dysmenorrhea. Brain Imaging Behav. 2018;12(3):710–717. doi:10.1007/s11682-017-9730-y
94. Tu CH, Niddam DM, Chao HT, et al. Brain morphological changes associated with cyclic menstrual pain. Pain. 2010;150(3):462–468. doi:10.1016/j.pain.2010.05.026
95. Yu SY, Xie MG, Liu SQ, et al. Resting-state functional connectivity patterns predict acupuncture treatment response in primary dysmenorrhea. Front Neurosci Switz. 2020;14. doi:10.3389/fnins.2020.559191
96. Tu CH, Lee YC, Chen YY, et al. Acupuncture treatment associated with functional connectivity changes in primary dysmenorrhea: a resting state fMRI study. J Clin Med. 2021;10(20):4731. doi:10.3390/jcm10204731
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







