Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 12
Initiation of Breast Milk Expression and Associated Factors Among Mothers of Preterm and Low Birth Weight Neonates Admitted to Neonatal Intensive Care Units of Government Hospitals in Addis Ababa, Ethiopia,2020
Authors Hirpha M, Mekonnen H , Fenta FA
Received 27 November 2020
Accepted for publication 8 April 2021
Published 4 May 2021 Volume 2021:12 Pages 213—221
DOI https://doi.org/10.2147/PHMT.S294032
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Misgana Hirpha, Hussen Mekonnen, Fikrtemariam Abebe Fenta
School of Nursing and Midwifery, College Health Science, Addis Ababa University (AAU), Addis Ababa, Ethiopia
Correspondence: Hussen Mekonnen Tel: +251911631634
Email [email protected]
Background: In early preterm and very low birth weight, breast milk expression is an optimal solution to continue with breastfeeding. This study aimed to assess the initiation of breast milk expression and associated factors among preterm and low birth weight mothers in the neonatal intensive care units of public hospitals in Addis Ababa.
Methods: Institution-based cross-sectional study was performed in selected public hospitals, Addis Ababa, among 124 breast feeding mothers chosen from different public health facilities of Addis Ababa; from April 5 to May 15, 2020. Information was collected using questionnaires administered by the interviewer, double data entry was performed using Epi Info version 4.6.02 software, cleaned finally exported to SPSS statistics version 26 for analysis. To predict the association of research variables, logistic regression models were used and adjusted for potential confounders.
Results: All respondents were started milk expression after six hours following delivery. Getting instruction on the method of their choice (AOR=0.55; CI=0.31 to 0.96) and gestational age ≤ 32 weeks (AOR=2.39; CI=1.34 to 4.24) were factors significantly associated with initiation of milk expression.
Conclusion: The study indicated breast milk expression was poor. Inter-departmental collaboration is required in order to promote good practice of breast milk expression among mothers of neonates with preterm and low birth weight.
Keywords: initiation, breast milk expression, preterm, low birth weight, neonatal intensive care unit
Introduction
World Health Organization recommends that breastfeeding should start within the first hour of birth, that all infants should be exclusively breastfed from birth to six months of age, and should continue until two years or beyond with complementary feeding.1 However, due to neuronal immaturity, preterm neonates have impaired sucking and swallowing control and have diminished oromotor tone, producing lower intraoral pressures after sucking. Full oral feeding can be achieved by most infants at 34 to 36 weeks of gestation.2 In such circumstances, newborns have to get expressed breast milk that can be supplemented by enteral feeding or drop of milk by syringe.3
Early initiation of breast milk expression promotes consumption human milk specifically colostrum. Human milk is a fresh, living food with many antioxidant, antibacterial, prebiotic, probiotic, and immune-boosting properties in addition to nutrients.4 In addition, colostrum immunoglobulin, like immunoglobulin A, immunoglobulin G,5 and immunoglobulin M (IgM) which protects against infection.
Even though Mother’s own milk (MOM) is the best form of nutrition for preterm infants and low birth weight infants,6 initiation of breast milk feeding within one hour is affected by different factors. Among these factors, mode of delivery, educational status of the mother, poor latching (preterm and very low birth weight infants) significantly affected early initiation.7,8 The other reasons for delayed initiation of breastfeeding are lack of milk, ill child and the baby get to sleep.9
Very low birth weight (VLBW) newborns are protected from different health problems by feeding their own mother’s milk. They are at a decreased risk of feeding intolerance, late onset of sepsis, necrotizing enterocolitis (NEC), and decreased hospital stay. Despite this mothers of VLBW infants often do not initiate expression early within one hour following delivery which can lead to formula feeding.10 Feeding formula milk increases the risk of necrotizing enterocolitis among VLBW neonates, whereas preterm infants who receive human milk instead of formula milk are less likely to develop necrotizing enterocolitis.11
Early breast milk expression has a similar role as early initiation of breastfeeding in long-term exclusive breastfeeding. It increases milk supply which is the concern of several mothers as they stop breastfeeding with the first six months after birth.12 It is also helpful to start trophic feeding which improves both gastrointestinal structural and functional development in preterm delivery lactogenesis-II production is delayed.13 Early milk expression also facilitates the oropharyngeal administration of colostrum which can decrease clinical sepsis among neonates.14
Lactation initiation and maintenance is more complicated for preterm infants’ mothers. Milk production (lactogenesis II) has to be initiated by an expression because at-breastfeeding is not possible due to infants’ immaturity and medical condition. Early initiation of regular breast milk expression, is a useful intervention for mothers at risk of early-onset breastfeeding failure lactogenesis II established by day 3. However, early initiation of breastfeeding is low among mothers who give birth by cesarean section, preterm, and low birth weight. Only 3.3% of mothers of preterm neonate have started breast expression within one hour after delivery in the study conducted in North India.15
A cross-sectional study conducted in Finland revealed that 36% of mothers start breast milk expression within six hours following delivery,16 whereas the study done in Japan showed only 17% of mothers start milk expression within six hours following delivery.17
A study done in Finland revealed that prior neonatal intensive care unit experience of mothers was a risk factor for late initiation of breast milk expression.16 Contrary to this, another study indicated that previous neonatal intensive care unit (NICU) experience as a facilitator of early initiation of breast milk expression among mothers of preterm infants admitted to neonatal intensive care unit.18
But in Ethiopia, there are limited data on the initiation of breast milk expression among mothers of preterm and low birth weight neonates admitted to the neonatal intensive care unit. Mothers of these groups of infants do not initiate breastfeeding because of poor coordination of sucking and swallowing. Initiation of breast milk expression has a similar role to initiate and maintain lactation with the initiation of breastfeeding. Thus, this study aimed at assessing the initiation of breast milk expression and associated factors among mothers of preterm and low birth weight neonates in Addis Ababa, Ethiopia.
Methods and Materials
Study Area
The survey was undertaken in Addis Ababa, Ethiopia’s capital city, and the seat of the African Union Charter. It has 10 sub-cities and the city’s population estimate for 2020 is 3.6 million, according to the central statistics agency.19 Presently, a total of thirteen hospitals are available in the city of which five hospitals are governed by the Federal Ministry of Health, six of them under the Addis Ababa City Health Bureau, one owned by the police department, and one owned by the Defense Army. Of them, ten hospitals have neonatal intensive care unit service.
Study Design and Procedures of Sampling
Institution-based cross-sectional study was performed in selected public hospitals, Addis Ababa, from April 5 to May 15, 2020.
The sample size was determined by using single proportion formula (n=Zα2*p(1-p)/d2 with assumptions of breast milk expression practice being 50%, with 5% level of significance and margin of error 5%. Since the total population size was less than 10,000, an adjustment formula (nf=n/(1+n/N) and an addition of 10% non-response rate. With these assumptions, the minimum required sample size was 130.
Respondents were selected from hospitals having neonatal intensive care unit. Primarily, identification number was given to each public hospital. Lottery methods was used to select a total of four public hospitals; then proportion of sample size allocations was carried out according the patient load in each public hospital. To choose the research participants from selected intensive care units, systematic random sampling was used.
All mothers of preterm (<34 weeks) and low birth weight infants admitted to neonatal intensive care unit during the study period and have difficulty of breast feeding were included, whereas mothers of preterm infants who were ≥34 weeks of gestational age, mothers’ whose infant medically kept nothing by mouth and whose option was to feed only formula milk were excluded.
Operational Definition
Initiation of breast milk expression. It is time for the mother to begin expressing breast milk, which was measured by requesting the mother and cross-checking the newborn chart with the record time.
Family support is any support giving: food, supporting in daily living activities, buying medicines, cleaning and buying equipment used to express and store breast milk, given to the mother starting from the time she gives birth to the time she interviewed from (husband, mother, sister).
Care provider support: is support directly related to milk expression like in case of pumping assembling pumping kits, collecting drop of milk and storing the collected milk.
Instruction: any instruction given to the mother on breast milk expression method she choice, by health care provider, the instruction can be supported with guideline, video or pictures.
Worried about the amount of milk if she think/worry that the expressed milk is not enough for the baby, measured by “yes”/”no” options.
Worried about health status of the baby: if she has concern about health status of her baby assuming that her baby is very sick, measured by “yes”/”no” options.
Data Collection
Interviewers administered structured questionnaire was used to collect the data. From previous similar studies, the data collection tool was adopted15,20–23 and modified into the local context. The instrument for data collection was prepared in English and translated into the local language (Amharic), by language expert and back translated to English by another person, to confirm consistency and accuracy. Data collectors were recruited based on their previous experience in data collection, relevance of their qualification, additional training on care of newborn and ability of the local language.
Training was given for three consecutive days in order to make data collectors and supervisors familiar to the tool and interview techniques. Ethical concerns, the wellbeing of participants and interviewers, avoiding under-reporting and ensuring confidentiality were also stressed. The data collection methods were pre-tested at 10% of the sample size in the randomly chosen neonatal intensive care unit outside the study site. The pretest helped to modify the questionnaire and make data collectors familiar with the tool.
Measurements
The outcome variable was the initiation time of breast milk expression which is a time at mothers start expressing breast following delivery. It was measured by asking the mother when she start breast milk expression and cross-checked on patient’s chart at the time of first feeding. Based on the response, the time of initiation was recorded.
Age, education, family support, care provider support, knowledge, method of pumping, relaxation, lack of privacy, health status of the neonate, stress, concern about the neonatal condition and complications of pregnancy were independent variables of this study.
Family support: was measured by asking the mother whether she gets any support (giving food, supporting in daily living activities, buying medicines, cleaning and buying equipments used to express and store breast milk) from her family starting from the time she gave birth to the time she interviewed. The response options “yes” or “no”.
Care provider support: this was measured by asking her whether she has got instruction/support on the techniques (based on method she used, handling the kits, how to collect drop of milk, positions) of breast milk expression during the start of breast milk expression. The response option was “yes” or “no” She also asked whether she knows the benefits of colostrum or not. The response option was “yes” or “no”.
Data Analysis
In EPI Info version 4.6.0.2 program, the pre-coded responses were double entered to verify their consistency and then exported to SPSS for window version 26 for statistical analysis used for percentage, frequency, bivariate and multivariate logistic regression analysis. Variables found to be significant at bivariate level (P<0.05) were selected and included into multiple logistic regression models. Then, logistic regression analysis models were used to measure the odds ratio to estimate association and to control the potential confounding variables with a 95% confidence interval. Using odds ratios compared to the comparison group and 95% confidence levels, the strength and direction of the relationship is presented.
Ethical Considerations
The research has been accepted by the Institutional Review Board (IRB) of the School of Nursing and Midwifery, College of Health Sciences, Addis Ababa University for scientific and ethical honesty including the verbal informed consent process. Ethical consent has been received from the Public Health Research and Emergency Response Directorate of Addis Ababa Health Bureau. Written approval was received from the Addis Ababa city government’s health bureau. Consent was sought at each health institution from medical directors and related unit heads. Prior to data collection, verbal consent was also obtained from Specific clients who participated in the study. Each participant was given sufficient information in order to make informed decisions. For each piece of information, confidentiality was strictly maintained and the interview was performed in a strict private location. General information, referral and follow-up linkages were made for those in need at the conclusion of the interview. The investigators would like to confirm that this study was conducted in accordance with the Declaration of Helsinki.
Results
Socio-Cultural Characteristics of Study Participants
A total of 130 women have been contacted to join the study (Table 1), of which 124 (95.4%) agreed to involve in the study. Seventy-four (57.7%) were from 18 to 30 years of age, with a mean age of 29.13 years (±5.54 SD) for the respondents.
 |
Table 1 Socio-Cultural Data Among Mothers of Preterm and Low Birth Weight Neonates Admitted to Neonatal Intensive Care Unit (NICU) of Government Hospitals in Addis Ababa, Ethiopia, 2020 (n=124) |
The participants 66 (53.2%) and 47 (37.9%) were predominantly housewife and grade 9–12 by level of education, respectively. Forty-eight (38.7%) were para I (number of birth). Ninety-four (75.8%) got support from their family when they express milk. Ninety-six (77%) respondents were reported antenatal care follow-up on current pregnancy, among these only 16 (16.7%) of them got advice on breast milk expression. Ninety-one (73.4%) were using the hand expression method and around 39 (32%) respondents got instruction/support on the method of their preference (Table 1).
Neonatal Characteristics
When we see the characteristics of preterm and low birth weight neonates admitted to the neonatal intensive care unit were very low birth weight 61 (49.2%) and low birth weight 61 (49.2%). With a mean birth weight of 1455.75 (+259.16 SD) grams, the minimum and maximum birth weight were 800 g and 2250 g, respectively. Two-thirds of the respondents gave birth to spontaneous vaginal delivery and in the late neonatal period there were about 86 (70%) of their neonates. About half of neonates were in fair condition and more than half of 68 (54.6%) of neonates were able to suck the breasts of their mothers (Table 2).
 |
Table 2 Neonatal Characteristics of Preterm and Low Birth Weight Neonates Admitted to the Neonatal Intensive Care Unit of Government Hospitals in Addis Ababa, Ethiopia, 2020 (n=124) |
Psychological Factors
With regard to the psychological condition of mothers admitted to the neonatal intensive care unit of government hospitals of preterm and low birth weight neonates. Approximately half of 68 (54.8%) respondents were worried about the amount of milk they expressed, whilst around 56 (45%) respondents were worried about the health status of their infant. Nearly sixty percent of respondents were not concerned about their baby’s prognosis, although about 38 (39%) were concerned about their baby’s prognosis (Figure 1).
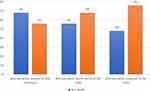 |
Figure 1 Psychological data among mothers of preterm and low birth weight neonates admitted to the neonatal intensive care unit of government hospitals in Addis Ababa, Ethiopia, 2020 (n=124). |
Maternal Factors
Nearly all mothers had births between the gestational age of 28–34 weeks, of which 45 (36.3%) were fewer or equal to 32 weeks and 79 (63.7%) were more than 32 weeks. Approximately 43 (35%) of respondents suffered complications linked to pregnancy, while pregnancy-induced hypertension was the most frequent complication (Table 3).
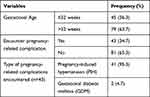 |
Table 3 Pregnancy-Related Data Among Mothers of Preterm and LBW Neonates Admitted to the NICU of Government Hospitals in Addis Ababa, Ethiopia, 2020 |
Initiation of Breast Milk Expression
All of the respondents started milk expression after 6 hours following delivery, of these more than half 71 (57.3%) started milk expression after 48 hours. The minimum and maximum time to start breast milk expression were 8 hours and 10 days, respectively (Figure 2).
Factors Associated with the Initiation of Breast Expression
None of the respondents started breast milk expression before 6 hours of the postpartum period. All of the respondents started breast expression after six hours (late initiation of breast expression) of the postpartum period. For the sake of analyses, late initiation of breast expression is grouped as less than 48 hours and 2 days and above (Table 4).
Getting instruction on the method of their choice (AOR=0.55; CI=0.31 to 0.96) and gestational age ≤32 weeks (AOR=2.39; CI=1.34 to 4.24) were identified as factors significantly associated with time to start breast milk expression among mothers of preterm and low birth weight neonates. Mothers who get instruction on the method of their choice were less like to start breast expression after two days when compared to those who did not get instruction. Mothers who gave birth at gestational age ≤32 weeks were 2.39 times more likely to start breast milk expression after two days of the postpartum period than those who gave birth at >32 weeks of gestational age (Table 4).
Discussion
The current study found that none of the respondents began expressing milk within 6 hours after delivery. After 6 hours, all (100%) respondents begin expressing milk. This could be attributed to mothers being followed in the maternity ward for the first six hours after giving birth, so this may be the cause. This result varies from the studies performed in Showa University Hospital and North India, which found that 17% and 3.3% of respondents started milk expression within 6 hours of delivery, respectively.15,17 In another study, it was identified that 36% of participants started breast expression within 6 hours after delivery.16 This disparity could be attributed to good support for lactation when being in the labor and neonatal intensive care unit.
Factors that significantly affect the initiation time of breast milk expression were to gain instruction on the method of breast milk expression and gestational age < 32 weeks. Compared to those who did not undergo instruction, having advice on the form of breast expression they preferred was a major facilitator for beginning breast expression within 6–48 hours. About two out of five mothers receiving training began to express milk within 6–48 hours. This may be because the difficulty of breast expression is made simple by instruction.
Breast milk expression 48 hours after the delivery was 2.39 times more among lower gestational age (≤32 weeks) when compared to those >32 weeks of gestational age. This may be attributed to insufficient lactation support during follow-up of antenatal care and during neonatal intensive care unit stay. This is contrary to other research that indicated a higher risk factor of late initiation of breast expression for gestational age.16 In addition, research showed that prior involvement in the neonatal intensive care unit was used as a facilitator and risk factor for late breast expression initiation.18 But in this study, these factors were not statistically significant in relation to late breast milk expression.
Limitations
Our study has several limitations, due to the cross-sectional nature of the study; it is difficult to determine the direction of the association between the study variables. There was a risk of social desirability bias whereby mothers may over or under report the time of initiation. So, further study should be carried out to explore the detailed initiation time of breast expression by observing initiation through multiple methods. As a strength of this study, the participants were chosen by random sampling methods. Care has been taken during the identification of experienced data collectors.
Conclusion and Recommendation
The present research found that the initiation of breast milk expression was poor because all respondents commenced milk expression after six hours child birth. Of these, 53 (42.7%) began to express milk within two days after delivery, while 71 (57.3%) began two days after delivery, this causes delayed lactogenesis II (two). Among mothers who give birth at less than or equal to 32 weeks of age, the risk of initiating milk expression after two days following delivery was greater.
For all mothers who are at risk of having preterm and low birth weight infants, antenatal care providers should have health education on initiation of milk expression. In the labor and delivery ward, staff should have to continue encouraging early initiation of breast milk expression and giving instruction on method of breast milk expression the mother want to use. In addition, to encourage early initiation of milk expression, healthcare professionals must pay attention to all mothers who give birth before or at 32 weeks of gestational age, and longitudinal research to determine the reasons for late initiation would be of future concern.
Acknowledgment
We are very thankful to Addis Ababa University for sponsoring this research. We would like to express our most heartfelt thanks to the women who participated in this study and for sharing such useful information. Our gratitude and appreciation go to all the data collectors involved in the study. This is the extract of thesis entitled “Breast Milk Expression Practice and Factors Affecting It Among Mothers of Preterm and Low Birth Weight Neonates Admitted to Neonatal Intensive Care Unit of Government Hospitals in Addis Ababa, Ethiopia, 2020” / and presented as thesis which available in Addis Ababa University archive but is not published. It is the common work of the three authors of this manuscript see URI: http://etd.aau.edu.et/handle/123456789/24204)24
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report that there is no financial or non-financial competing interest associated with this study.
References
1. WHO. Guideline: Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services. Geneva: World Health Organization; 2017.
2. Lehtonen. L. Assessment and optimization of neurobehavioral development in preterm infants. In: Fanaroff & Martin’s Neonatal-Perinatal Medicine. Philadelphia: Elsevier; 2015.
3. Kumar RKSA, Vaidya U, Banerjee S, Anwar F, Rao S. Optimizing nutrition in preterm low birth weight infants—consensus summary. Front Nutr. 2017;4:20. doi:10.3389/fnut.2017.00020
4. Anne ELS. ABM clinical protocol #8: human milk storage information for home use for full-term infants, Revised 2017. ABM Protocol. 2017;12(7).
5. Kirsty V, Biggs KH, Matthews E, et al. Formula milk supplementation on the postnatal ward: a cross-sectional analytical Study. MDPI. 2018;10(608).
6. Xu WJM, Maas K, Hussain N, McGrath JM, Henderson WA, Cong X. Systematic review of the effect of enteral feeding on gut microbiota in preterm infants. HHS Public Access. 2018;473:12.
7. Gebremeskel SGGT, Gebrehiwot BG, Meles HN, et al. Early initiation of breastfeeding and associated factors among mothers of aged less than 12 months children in rural eastern zone, Tigray, Ethiopia:. BMC Res Notes. 2019;12(1):671. doi:10.1186/s13104-019-4718-x
8. Alzaheb R. Factors associated with the initiation of breastfeeding within the first 48 hours of life in Tabuk, Saudi Arabia. Int Breastfeed J. 2016;11(1):21. doi:10.1186/s13006-016-0079-4
9. Bee MSA, Hill Z. Neonatal care practices in sub-Saharan Africa: a systematic review of quantitative and qualitative data. J Health Public Nutr. 2018;37(9).
10. Parker LASS, Krueger C, Mueller M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants. Breastfeed Med. 2015;10(2).
11. Bode L. Human milk oligosaccharides in the prevention of necrotizing enterocolitis: a journey from in vitro and in vivo models to mother-infant cohort Studies. Front Pediatr. 2018;6:385. doi:10.3389/fped.2018.00385
12. Brown CR, Dodds L, Legge A, Bryanton J, Semenic S. Factors influencing the reasons why mothers stop breastfeeding. Can J Public Health. 2014;105(3):e179–e85. doi:10.17269/cjph.105.4244
13. Akram SNFB, Niloofar S, Morteza G, Golnesa S. Early versus late trophic feeding in very low birth weight preterm infants. Iran J Pediatr. 2012;22(2):7.
14. Lee J, Jung HS, Choi YH, et al. Oropharyngeal colostrum administration in extremely premature infants: an RCT. Pediatrics. 2015;135(2):e357–e66. doi:10.1542/peds.2014-2004
15. Daljeet KAK, Geetanjli K, Praveen K. Current practices related to feeding preterm neonates with expressed breast milk: a pilot project. COJ Nurse Health Care. 2018;3(3).
16. Ikonen RP, Helminen E, Kaunonen M. Preterm infants’ mothers’ initiation and frequency of breast milk expression and exclusive use of mother’s breast milk in neonatal intensive care units. J Clin Nurs. 2018;27(3–4):e551–e8. doi:10.1111/jocn.14093
17. Murase MLN, Morrow AL, Hatsuno M, et al. Predictors of low milk volume among mothers who delivered preterm. J Hum Lact. 2014;30(4):10. doi:10.1177/0890334414543951
18. Ikonen R, Paavilainen E, Kaunonen M, et al. Preterm infants mothers experiences with milk expression and breast feeding. Wolters Kluwer. 2015;15(6):12.
19. Centeral Statistical Agency E. Population projections for Ethiopia 2007–2037. Addis Ababa; 2013.
20. Alves E, Magano R, Amorim M, Nogueira C, Silva S. Factors influencing parent reports of facilitators and barriers to human milk supply in neonatal intensive care units. J Hum Lact. 2016;32(4):695–703. doi:10.1177/0890334416664071
21. Sisk P, Quandt S, Parson N, Tucker J. Breast milk expression and maintenance in mothers of very low birth weight infants: supports and barriers. J Hum Lact. 2010;26(4):368–375. doi:10.1177/0890334410371211
22. Becker GESH, Cooney F. Methods of milk expression for lactating women. Cochrane Database Syst Rev. 2016;9.
23. Parker LA, Krueger C, Kelechi T, Mueller M. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants: a pilot study. J Perinatol. 2012;32:4. doi:10.1038/jp.2011.78
24. Misgana Hirpha Kedida HMA, Fanta FA. Breast milk expression practice and factors affecting it among mothers of preterm and low birth weight neonates admitted to neonatal intensive care unit of government hospitals in Addis Ababa, Ethiopia; 2020. Available from: http://etd.aau.edu.et/handle/123456789/24204.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.