Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Information Needs in COPD After an Educational Programme: Influence in Exacerbations and Admissions
Authors Amado CA , Pérez-García C, Tamayo Fernández B , Agüero-Calvo J, Muñoz-Cacho P , Golpe R
Received 11 August 2020
Accepted for publication 25 September 2020
Published 27 October 2020 Volume 2020:15 Pages 2663—2671
DOI https://doi.org/10.2147/COPD.S275002
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Carlos Antonio Amado,1 Cecilia Pérez-García,2 Begoña Tamayo Fernández,3 Juan Agüero-Calvo,3 Pedro Muñoz-Cacho,4 Rafael Golpe5
1Hospital Universitario Marqués de Valdecilla, Servicio de Neumología, Universidad de Cantabria, Santander, Spain; 2Universidad de Cantabria, Santander, Spain; 3Hospital Universitario Marqués de Valdecilla, Servicio de Neumología, Santander, Spain; 4Servicio Cántabro de Salud, Santander, Spain; 5Hospital Universitario Lucus Augusti, Servicio de Neumología, Grupo C039 Biodiscovery HULA-USC, Instituto de Investigación Sanitaria de Santiago de Compostela (IDIS), Santander, Spain
Correspondence: Carlos Antonio Amado
Servicio de Neumología, Hospital Universitario Marqués de Valdecilla, Avenida Valdecilla SN, Santander 39001, Cantabria, Spain
Email [email protected]
Introduction: Improving patients’ information needs (IN) may contribute to better control in COPD. This study analyses IN using Lung Information Needs Questionnaire (LINQ) following an educational intervention, evaluates how clinical characteristics modify IN, and studies high IN as a prognostic factor for COPD exacerbations and hospital admissions.
Methods: Cohort of 143 patients with initial diagnosis of COPD included in a structured educational program. Two months after completing the program, IN was assessed using LINQ. Correlations between IN and clinical variables of COPD and distribution of IN in different clinical groups were analyzed. Univariate and multivariate analysis was performed to determine influence of IN on exacerbations and COPD admissions over the following year.
Results: LINQ scored 6.3± 2.9. There were no differences in LINQ scoring between different clinical groups, but LINQ score positively correlated with age (r=0.184, p=0.029). High IN was a predictor of COPD hospitalizations (HR 2.3 [95% CI 1.1– 5.1] (p=0.029)) but not of less severe exacerbations (p=0.334).
Conclusion: IN was not associated with any clinical variables, but it correlated with age. High IN proved to be an independent predictor of admissions.
Keywords: COPD, education, COPD exacerbation
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is one of the main causes of morbidity and mortality worldwide.1 Exacerbation risk reduction is one of the key objectives for the management of the disease as stated by clinical guidelines.2,3 Exacerbations influence on the deterioration of respiratory function tests4 and on the disease prognosis.5,6
COPD patient education programs improve self-management, exercise capacity, quality of life, levels of anxiety,7 and reduce treatment costs.8 Despite this, structured education programs in this disease and its evaluation are scarce. The Lung Information Needs Questionnaire (LINQ)9 is a self-administered questionnaire consisting of 16 questions divided into 6 domains: Knowledge about the disease, medications, self-management, exercise, diet and smoking. It has been used to evaluate respiratory rehabilitation programs,10 in other types of educational programs for patients with COPD in outpatient clinics11,12 or during hospital admissions.13 This questionnaire has been previously validated9 and translated into several languages including Spanish.14 However, the LINQ has never been used to assess which COPD Characteristics are correlated with information needs (IN), nor how IN influence moderate COPD exacerbations or admissions due to exacerbations.
In our clinical setting patients receive a standard educational cycle on COPD performed by a specialized educational nurse based on recommendations from clinical guidelines2,3 and LINQ domains, assessing treatment posology and technique, self-management, diet, exercise, vaccination and progression of the disease. Two months after this intervention, patients are tested using the LINQ questionnaire.
The objective of this study is to determine whether IN after having been diagnosed and having received a standard educational cycle on their disease influence in respiratory exacerbations or admissions and to assess whether IN correlates with any clinical variable of the disease or if they are typical of any of the phenotypes described in the disease management guidelines.2
Methods
Retrospective longitudinal cohort study in which the medical records of patients treated consecutively in the COPD monographic clinics – which attend patients referred from Primary care or Hospitalization due to suspected COPD – from a Spanish third level hospital with 800 beds belonging to the public health system. This study was approved by the Ethics Committee of Cantabria (2019.112). Informed consent was obtained from participants to perform all procedures related to the study and it was conducted in accordance with the Declaration of Helsinki.
Participants
The patients included in the study had a COPD diagnosis confirmed by spirometry carried out according to SEPAR criteria15 with a post-bronchodilator FEV1/FVC ratio of less than 0.7. After the initial disease diagnosis, and after the indication of pharmacological treatment, patients attended a complementary nursing consultation, in which the educational programme was performed, addressing issues such as smoking, exacerbations, the use of inhaled therapy and other useful aspects in order to have better self-management. Two months after this intervention, patients were tested using the LINQ questionnaire to determine their degree of knowledge about the disease and were included in the study. The study was carried out between December 2016 and January 2018 with a subsequent review of the medical records to identify exacerbations and admissions during the year after completing the questionnaire.
Variables
Collected clinical variables (2 months after COPD diagnosis): Age, Sex, Post-bronchodilator spirometric variables: Maximum expiratory volume in the first second (FEV1), Forced Vital Capacity (FVC), FEV1/FVC, COPD Assessment Test (CAT) quality of life questionnaire,16 dyspnea according to the modified Medical Research Council (mMRC) dyspnea scale,17 number of moderate COPD exacerbations in the year prior to the visit (moderate exacerbations were defined as respiratory exacerbations which required antibiotic treatment and/or systemic corticosteroids recorded in patient’s electronic medical records in the year prior to the LINQ questionnaire), number of admissions for COPD exacerbation in the year prior to the visit recorded in patient’s electronic medical history, diagnosis of cognitive impairment prior to the visit, Pharmacological treatment for COPD, Charlson Comorbidity Index,18 LINQ questionnaire total score and in each of its 6 domains: Disease knowledge (questions 1 to 4 and score between 0 and 4 points), Medicines (questions 5 to 7 and score between 0 and 5 points), Self-management (questions 8 to 9 and score between 0 and 6 points), Smoking (questions 10 to 12 and score 0–3 points), Exercise (questions 13 to 15 and score between 0 and 5 points), Diet (question 16 and score between 0 and 2 points). The minimum score is 0 (it indicates lowest information needs), while the maximum score is 25 points (highest information needs).14
The number of moderate exacerbations and hospital admissions for COPD exacerbation during the year after the answer to the LINQ questionnaire were collected. The study schedule is shown in Figure 1.
 |
Figure 1 Study schedule. |
Clinical Groups
The patients were divided into groups according to clinical variables proposed by the GesEPOC (Spanish COPD guidelines) and GOLD guidelines2,3 based on: FEV1: mild COPD (FEV1 ≥ 80% of predicted value), moderate (50% ≤ FEV1 <80% of predicted value), severe (30% ≤ FEV1 <50% of predicted value), or very severe (FEV1 <30% of the predicted value). CAT: Non-symptomatic: score ≤ 9 or less, symptomatic:>9 points. mMRC Dyspnoea score, dyspneic: score 2 or more. Non-dyspneic: score 0–1.
Patients with 2 or more exacerbations were considered exacerbators, patients with 1 or none were considered non-exacerbators.
Patients with a score higher than the 75th percentile of our sample on the LINQ questionnaire were considered patients with high IN.
Statistical Analysis
The Kolmogorov–Smirnov technique was used to assess the data adjustment to a normal distribution. Parametric variables were presented as mean ± standard deviation and non-parametric variables as median (interquartile range). T-student test for unpaired samples was used to establish the differences in variables with normal distribution, and the Mann–Whitney U-test was used to determine differences between variables with a non-parametric distribution. To study the correlations between the different clinical variables, the Spearman test was used for non-parametric variables and the Pearson test for parametric variables. A univariate and multivariate analysis was implemented to determine which variables intervene as predictors of exacerbation and admission using the Cox regression test. Two-tailed tests were used and a level of p <0.05 was considered statistically significant. Statistical analysis was developed with the SPSS program (version 25.0 for pc).
Results
A total of 170 medical records of patients seen in outpatient Pneumology clinics at the Marqués de Valdecilla University Hospital were analyzed. Twenty-seven patients were excluded from the study due to different reasons: Patients moved to other area (1 case), absence of subsequent follow-up at the referral hospital (6 cases), patients who did not answer the LINQ questionnaire due to presenting a previous diagnosis with moderate-severe cognitive impairment (5 cases), and patients whose LINQ questionnaire score had not been collected in the electronic history due to technical problems (15 cases). A total of 143 patients were finally included in the study. Seven patients did not complete the follow-up study due to death (four patients due to severe COPD exacerbations, two patients due to lung cancer and colon cancer in one patient). Six of the deceased patients showed an admission due to COPD exacerbation prior to death (Figure 2).
 |
Figure 2 Flowchart of patient selection. |
Clinical Characteristics of the Patients Included in the Study
The most relevant characteristics of the patients included in the study are shown in Table 1. Four patients included in the study had mild cognitive impairment.
 |
Table 1 Demographic Characteristics of Patients Included in the Study (N=143) |
Information Needs in COPD After Biosanitary Education
Table 2 shows the IN of the patients included in the study estimated by LINQ. The total score and the score of the different LINQ domains are included.
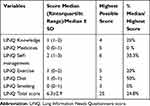 |
Table 2 LINQ Score and Domains |
LINQ Score Correlations with Relevant Clinical Variables
The LINQ score was weakly but significantly positively correlated with age (r = 0.184, p = 0.029) but not with CAT (p = 0.180), Charlson comorbidity index (p = 0.878), FEV1 (%) (p = 0.052), number of previous admissions (p = 0.477), number of previous exacerbations (p = 0.641) or mMRC degree of dyspnea (p = 0.510). Figure 3 shows the scatter plot of the correlation between age and LINQ.
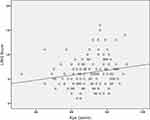 |
Figure 3 Scatter plot showing correlation between age and LINQ score. |
Differences in LINQ Score Between Different Clinical Groups
They are shown in Table 3. No statistically significant differences were found among the different clinical groups. There were also no statistically significant differences in the LINQ score in patients with different degrees of GOLD obstruction (p = 0.141) (Figure 4) or different GOLD ABCD classification (p= 0.757) (Figure 5).
 |
Table 3 LINQ (Lung Information Needs Questionnaire) Score in Different Clinical Groups |
 |
Figure 4 LINQ score in different GOLD Obstruction patients. *Outlier. |
 |
Figure 5 LINQ score in different GOLD ABCD Classification patients. |
LINQ Score as a Predictor of Exacerbations and Admissions per Year
During the follow-up period, 79 patients suffered a respiratory exacerbation and 38 were admitted to the hospital due to exacerbation of their COPD. The patients were divided according to their LINQ score into patients with high IN (patients with a LINQ score of 8 or more, corresponding to the upper quartile of the patients included in the study n = 34) and the rest of patients. Seventeen patients in the group with high IN presented an exacerbation of their COPD, while in the rest of the patients, 62 had COPD exacerbations. Thirteen patients with high IN were admitted, while 25 patients in the group without high IN showed an admission (Table 4).
 |
Table 4 Number of exacerbations and hospital admissions according to LINQ score. |
Univariate analysis using Cox regression showed that Age (p = 0.049), FEV1 (p = 0.001), the history of having presented 2 previous exacerbations (p = 0.008), or the mMRC degree of dyspnea (p = 0.002) were risk factors for COPD exacerbation, but gender (p = 0.724), high IN (p = 0.425), and Charlson (p = 0.062) were not. Multivariate analysis using Cox regression showed that FEV1 (p = 0.012) was an independent risk factor for COPD exacerbation (Table 5).
 |
Table 5 Cox Regression Analysis of Predictors of COPD Exacerbation |
Univariate analysis using Cox regression showed that high IN (p = 0.008), age (p <0.001), previous admissions due to COPD exacerbation (p <0.001), FEV1 (p = 0.006), Charlson index (p <0.001) and the mMRC dyspnoea score (p <0.001) were risk factors for admission due to exacerbation of COPD, but not sex (p = 0.884). Multivariate analysis using Cox regression showed that high need for information (p = 0.029), age (0.01), Charlson (p = 0.026) and the history of previous admissions (p = 0.004) were independent risk factors for admission due to COPD exacerbation (Table 6, Figure 6).
 |
Table 6 Cox Regression Analysis of Predictors of Hospitalization Due to COPD Exacerbation |
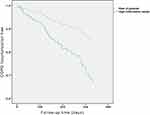 |
Figure 6 The curve representation for hospitalization due to COPD exacerbation. High information needs=LINQ Score ≥ 8. |
Discussion
COPD is a disease associated with a high consumption of health resources and which has a great impact on the quality of life and patient survival, so it is essential to control all its dimensions that are susceptible to improvement. Biosanitary education is a key element in the management of these patients. It aims to achieve a proactive attitude towards their pathology, but its influence on clinical results has not been sufficiently investigated. This study has found that our educational program is similar in terms of educational results to programs carried out in other countries such as Canada or Sweden;11–13 despite the fact that patients included in our study, had a recent diagnosis and had not received information previously about their disease. The domains of the questionnaire in which patients have the greatest IN are “Diet” and “Self-care”. These results are similar to previously presented data19 and highlight the need to have a more exhaustive impact on this information.
It is important to explore which patient features are associated with a greater or lesser degree of IN, after a first educational visit. This would be very useful to design custom-made educational programs which affect those groups with less knowledge of their pathology, allowing health resources to be managed more efficiently, and to advance in medical care customization to which precision medicine aspires. This study has not shown differences in IN, evaluated with the LINQ questionnaire, among different groups, defined by clinical variables commonly used in subjects with COPD categorisation (eg, degree of dyspnea or bronchial obstruction). This result contrasts with a previous study12 which found that patients with a higher degree of bronchial obstruction had greater information needs. The different setting of that study (primary care) and the different evaluation strategy of the patients with respect to our study (subjects in different phases of clinical follow-up, and not exclusively assessed after the disease diagnosis) could explain these differences. This suggests that it is daring to generalize the results of educational programs in COPD, and that these should be evaluated in the specific area in which they will be implemented.
However, our study found that age correlates with knowledge needs. Younger patients had less IN, after initial education, than older subjects. The practical implication would be that older patients would need more intensive educational programs. The explanation for this, possibly lies in sociocultural factors, or in undetected cognitive disorders. Therefore, our results suggest that sociodemographic aspects could influence the acquisition of knowledge about COPD more than clinical variables. A single previous study has analyzed this aspect and, consistent with this hypothesis, showed that the knowledge of the disease (in this case evaluated with the Mount Sinai Hospital Questionnaire) was higher in patients who had completed secondary education studies.19 Also, it has been shown that Patients’ knowledge can be improved in older patients with COPD using specific rehabilitation programmes.20
One of the most relevant results of this study is the finding that high IN predicts an increased risk of severe COPD exacerbations (exacerbations resulting in hospital admissions). The potential implications of this observation to design follow-up strategies (intensive educational programs, early referral to respiratory rehabilitation …) which decrease the future risk of patients is evident. On the contrary, we did not find a significant relationship with the risk of suffering moderate exacerbations. When interpreting this last result, we must highlight that our study used an operational definition of moderate exacerbation, based on the prescription of antibiotics or steroids. Although this definition is widely used, it is not suitable, and in some studies, it has been observed that up to 50% of exacerbations, the patient does not look for medical attention and these are not treated, impacting despite this on the quality of life.21 It is plausible that subjects with poorer information about the disease are those who are less likely to consult the doctor when presenting exacerbation symptoms, so they would not receive treatment and exacerbations would not be detected by a retrospective study like this one. Hypothetically, some of these exacerbations not treated early could end up in hospital admission.
Our study has several limitations. Retrospective design implies a risk of information bias. In fact, the number of variables collected has been limited, and has not considered the socioeconomic or cultural level of the subjects studied, being only representative of public health patients. This potential confounding factor could influence both the baseline knowledge of the disease,19 the learning capacity and the risk of exacerbations and admissions.22–25 The scope of performance (monographic clinics, when the patient is first diagnosed by the specialist) also means a risk of selection bias, which limits the generalization of our findings.
In conclusion, IN in our setting were similar to other education programmes from other locations. Age influences negatively in IN, although other important COPD clinical outcomes were not correlated with IN. High IN is an independent predictor for hospital admission due to COPD exacerbation. These results may constitute the starting point for new studies investigating whether the modification of the knowledge of the disease through educational programs can reduce the number of admissions for exacerbation of COPD.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498–1504. doi:10.1016/S0140-6736(96)07492-2
2. Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish COPD guidelines (GesEPOC) 2017. Pharmacological treatment of stable chronic obstructive pulmonary disease. Arch Bronconeumol. 2017;53:324–335. doi:10.1016/j.arbres.2017.03.018
3. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195:557–582.
4. Seemungal T, Donaldson G, Bhowmik A, Jeffries D, Wedzicha J. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;161(5):1608–1613. doi:10.1164/ajrccm.161.5.9908022
5. Arnedillo Muñoz A. Impacto de la agudizaciones e ingresos en la EPOC. ArchBronconeumol. 2010;46:8–14.
6. Soler-Cataluña JJ, Martínez-García MÁ, Sánchez LS, Tordera MP, Sánchez PR. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med. 2009;103(5):692–699. doi:10.1016/j.rmed.2008.12.005
7. Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD002990.
8. Lisspers K, Johansson G, Jansson C, et al. Improvement in COPD management by access to asthma/COPD clinics in primary care: data from the observational PATHOS study. Respir Med. 2008;102(9):1345–1354. doi:10.1016/j.rmed.2014.06.002
9. Hyland ME, Jones RCM, Hanney KE. The lung information needs questionnaire: development, preliminary validation and findings. Respir Med. 2006;100:1807–1816.
10. Jones RCM, Wang X, Harding S, Bott J, Hyland M. Educational impact of pulmonary rehabilitation: lung information needs questionnaire. Respir Med. 2008;102(10):1439–1445. doi:10.1016/j.rmed.2008.04.015
11. Rocker GM, Amar C, Laframboise WL, Burns J, Verma JY. Spreading improvements for advanced COPD care through a Canadian collaborative. Int J Chron Obstruct Pulmon Dis. 2017;12:2157–2164. doi:10.2147/COPD.S140043
12. Sandelowsky H, Krakau I, Modin S, Ställberg B, Nager A. COPD patients need more information about self-management: a cross-sectional study in Swedish primary care. Scand J Prim Health Care. 2019;37(4):459–467. doi:10.1080/02813432.2019.1684015
13. Janaudis-Ferreira T, Carr SJ, Harrison SL, et al. Can patients with COPD assimilate disease-specific information during an acute exacerbation?: results of a pilot randomized controlled trial. Chest. 2018;154:588–596.
14. Wilches Luna EC, Lorena Obregón A, Maria Isabel Delgado H, Diana Fernanda Rebolledo A, Adiela Terreros A. Adaptación cultural del cuestionario linq (Lung Information Needs Questionnaire) en pacientes con enfermedad respiratoria crónica en un programa de rehabilitación pulmonar en Cali, Colombia. Rev Cienc Salud. 2014;12:23–34. doi:10.12804/revsalud12.1.2014.02
15. García-Río F, Calle M, Burgos F, et al. Espirometría (2013). Arch Bronconeumol. 2013;49(9):388–401. doi:10.1016/j.arbres.2013.04.001
16. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34:648–654. doi:10.1183/09031936.00102509
17. Schilling RS, Hughes JP, Dingwall-Fordyce I. Disagreement between observers in an epidemiological study of respiratory disease. BMJ. 1955;1(4905):65–68. doi:10.1136/bmj.1.4905.65
18. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
19. Scott AS, Baltzan MA, Dajczman E, Wolkove N. Patient knowledge in chronic obstructive pulmonary disease: back to basics. COPD. 2011;8(5):375–379. doi:10.3109/15412555.2011.605402
20. Wouters TJ, van Dam van Isselt EF, Achterberg WP. Information needs of older patients living with chronic obstructive pulmonary disease (COPD) indicated for a specific geriatric rehabilitation programme: a prospective cohort study. Int J Palliat Nurs. 2020;26:238–245. doi:10.12968/ijpn.2020.26.5.238
21. Langsetmo L, Platt RW, Ernst P, et al. Underreporting exacerbation of chronic obstructive pulmonary disease in a longitudinal cohort. Am J Respir Crit Care Med. 2008;177(4):396–401. doi:10.1164/rccm.200708-1290OC
22. Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106:196–204. doi:10.7326/0003-4819-106-2-196
23. Agusti A, Faner R, Celli B, Rodriguez-Roisin R. Precision medicine in COPD exacerbations. Lancet Respir Med. 2018;6:657–659.
24. Eisner MD, Blanc PD, Omachi TA, Yelin EH, Sidney S, Katz PP. Socioeconomic status, race and COPD health outcomes. J Epidemiol Community Health. 2011;65:26–34. doi:10.1136/jech.2009.089722
25. Lange P, Marott JL, Vestbo J, Ingebrigtsen TS, Nordestgaard BG. Socioeconomic status and prognosis of COPD in Denmark. COPD. 2014;11:431–437. doi:10.3109/15412555.2013.869580
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
