Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Influence of Pre-Existing Cerebral Small Vessel Disease on the Outcome of Acute Cardioembolic Stroke: A Retrospective Study
Authors Su Y, Guo Y, Chen Z, Zhang M, Liu J, Wang Q, Yao T
Received 24 January 2022
Accepted for publication 1 April 2022
Published 15 April 2022 Volume 2022:18 Pages 899—905
DOI https://doi.org/10.2147/NDT.S359768
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Yan Su,1 Yikun Guo,2 Zhuoyou Chen,2 Min Zhang,2 Jianfang Liu,2 Qian Wang,2 Tian Yao2
1Department of Radiology, The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University, Changzhou, Jiangsu Province, People’s Republic of China; 2Department of Neurology, The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University, Changzhou, Jiangsu Province, People’s Republic of China
Correspondence: Yikun Guo, Department of Neurology, The Affiliated Changzhou No.2 People’s Hospital of Nanjing Medical University, 68# Middle Gehu Road, Changzhou, 213164, Jiangsu Province, People’s Republic of China, Tel +86-519-81087079, Fax +86-519-81087711, Email [email protected]
Purpose: This study was to explore the role of pre-existing small vessel disease (SVD) on the 3-month outcomes of acute cardioembolic stroke (CES) patients.
Patients and Methods: Data of 189 consecutive acute CES patients at a single center were retrospectively enrolled. SVD imaging markers of lacunes, white matter hyperintensities (WMH) and enlarged perivascular spaces (EPVS) were evaluated and their total burden score (0– 3 points) was calculated. Patients were divided into the good functional outcome group (modified Rankin scale, mRS ≤ 2) and the poor functional outcome group (mRS ≥ 3) at 3 months after stroke onset. The effect of each single SVD marker and its total burden score on the outcome was identified using binary logistic regression.
Results: Overall, 100 (52.9%), 52 (27.1%), 28 (14.8%) and 9 (4.8%) patients had 0, 1, 2 and 3 SVD imaging markers. Patients with a total SVD burden score of 2 and 3 were significantly older and had higher baseline National Institutes of Health Stroke Scale (NIHSS) score than those with a score of 0 and 1 (P< 0.01). Forty-seven (24.9%) patients had a poor outcome. Patients in the poor outcome group had significantly higher baseline NIHSS score, increased incidence of stroke associated pneumonia, and heavier burden of lacunes, WMH and EPVS, and thus had elevated total SVD burden score than those in good outcome group (P< 0.05). After adjusting for potential confounders, the WMH (odds ratio [OR] = 2.6777, 95% confidence interval [CI] = 1.052– 6.812, P = 0.039) and the total SVD burden score (OR = 1.717, 95% CI = 1.072– 2.749, P = 0.024) were, respectively, independent risk factors for a poor outcome.
Conclusion: The pre-existing SVD may be associated with the 3-month prognosis of CES.
Keywords: cardioembolic stroke, small vessel disease, imaging marker, total burden score, prognosis
Introduction
Cerebral small vessel disease (SVD) refers to a group of clinical, neuroimaging, and pathological syndromes caused by the damage of cerebral perforating arterioles, capillaries, and venules.1 SVD imaging markers on magnetic resonance imaging (MRI) encompass lacunes, white matter hyperintensities (WMH), microbleeds (MCBs) and enlarged perivascular spaces (EPVS).2 Studies have shown that these markers were associated with cerebral microcirculation disturbance, impaired collateral recruitment, disrupted brain integrity, and reduced network efficiency.1,3–5 In addition, they were highly prevalent in the elderly and were closely related to stroke recurrence and worse clinical outcomes.6,7 As the SVD markers may occur simultaneously in one patient, the total SVD burden score has been proposed to assess their accumulative effect on the brain.8 Some studies have found that it independently predicts higher acute ischemic stroke risk, more severe stroke, and worse outcome.9–11
Cardioembolic stroke (CES) accounts for around 15–30% of ischemic stroke.12 When it occurs, the status of cerebral microcirculation may affect the collateral recruitment, and thus influence the outcome.
However, few studies have focused on the relationship between these pre-existing SVD markers and the functional outcome of CES. We aimed to investigate the effect of pre-existing SVD imaging markers on the 3-month outcomes of acute CES patients with mild to moderate neurological deficit.
Patients and Methods
Subjects
For this single-center, retrospective, observational study, we retrieved data from the stroke center database of Changzhou NO. 2 People’s Hospital, Jiangsu Province, China. This study was approved by the Clinical Research Ethics Committee of the Affiliated Changzhou No. 2 People’s Hospital of Nanjing Medical University (approval number: 2018KY032-01). Written informed consents were obtained from all the patients or their legally authorized representatives. All patient data were de-identified. This study was conducted in accordance with the Declaration of Helsinki.
Consecutive patients with first-ever acute CES within 48 hours of stroke onset from June 2014 to September 2019 were enrolled. All patients had known or newly-diagnosed non-valvular atrial fibrillation, and stroke events were confirmed by MRI and treated in accordance with the corresponding guidelines. Other inclusion criteria were: (1) 18 ≤ age ≤ 80 years, (2) anterior circulation infarction involving at least one side of the middle cerebral artery, and (3) the baseline NIHSS score was 0–14. Patients were excluded if they had reperfusion therapy or had no brain magnetic resonance angiography (MRA) or computed tomography angiography (CTA), which would be essential to estimate the stroke subtype.
Diagnosis of Cardioembolic Stroke
Essential tests like electrocardiogram (ECG), transthoracic echocardiography, cervical vascular ultrasound and cranial MRA/CTA were routinely performed. Thus, the known or newly-diagnosed non-valvular atrial fibrillation was confirmed and the stroke subtype of CES defined by the Trial of Org 10172 in Acute Stroke Treatment (TOAST-criteria) was identified.13
Definition and the Total Burden Score Calculation of SVD Markers
The SVD imaging markers were assessed on MRI and their total burden score was calculated with an ordinal scale (0–3) counting the presence of each of the three SVD markers.10 Specifically, each imaging marker was defined as the following and the total SVD burden score was made accordingly: (1) Lacunes were defined as deep lesions (3–15 mm) with CSF-like signal with hyperintense rim on fluid attenuated inversion recovery (FLAIR) sequence surrounded by white matter or subcortical gray matter. One point was awarded when one or more asymptomatic lacunar infarcts were present. (2) WMH was graded using the Fazekas score on FLAIR sequence and divided into periventricular and deep WMH by the lesion location. One point was awarded in case of the periventricular WMH Fazekas score was 3 (irregular hyperintensities extending into the deep white matter), and/or if the deep WMH Fazekas score was 2 or 3 (confluent white matter hyperintensities). (3) EPVS were defined as fluid-filled spaces with signal intensities similar to that of cerebrospinal fluid on all sequences. They followed the courses of penetrating vessels and were linear, round or ovoid in shape, and with diameters generally smaller than 3 mm. One point was awarded if EPVS in basal ganglia or semiovale were grade 2 or above. MRI evaluation was performed independently by a neurologist and a neuroradiologist.
Clinical Evaluation and Functional Follow-Up
Baseline demographics, vascular risk factors, and clinical and laboratory characteristics were obtained from medical records. Neurological deficit was assessed using the NIHSS score. An intracranial hemorrhage (ICH) was defined as symptomatic (sICH) if the patient had clinical deterioration causing an increase in the NIHSS score by ≥ 4 points and as non-symptomatic (nsICH) otherwise.14 Stroke-associated pneumonia (SAP) was diagnosed in the presence of fever, purulent sputum, abnormal respiratory examination, and pathologic chest X-ray findings and/or leukocytosis or leukopenia (white blood cell count ≥ 10 × 109 or ≤ 4 × 109/L, respectively).15
Functional outcome was evaluated using the modified Rankin scale (mRS) through an outpatient clinic visit or telephone inquiry at 3 months after stroke onset. A doctor and a trained nurse separately judged the functional status of each patient and then achieved a consistent result. Patients were divided into poor outcome group (mRS ≥ 3) and good outcome group (mRS ≤ 2) on the basis of this judgement.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation (SD) or median (interquartile range, IQR). Normally distributed continuous variables were compared using one-way analysis of variance (ANOVA) or Student’s t-test, and the skewed continuous variables were compared using Kruskal–Wallis H-test or Mann–Whitney U-test. Categorical variables were expressed as percentages and compared between groups using Pearson’s χ2 test. Binary logistic regression analysis was performed separately to evaluate the effects of lacunes, WMH, EPVS and the total SVD burden score on the functional outcomes. The results are shown as odds ratio (OR) and 95% confidence intervals (CI). A two-tailed P < 0.05 was considered statistically significant. All statistical analysis was performed on SPSS 22.0.
Results
Baseline Information
A total of 189 patients were included for final analysis, of whom 145 (61.7%) were men. The median age was 72 (IQR67, 76) years and the median admission NIHSS score was 5 (IQR2, 10). As to the total SVD burden score, 100 (52.9%) patients had score 0, 52 (27.1%) had score 1, 28 (14.8%) had score 2, and 9 (4.8%) had score 3. Age, baseline NIHSS score, incidence of SAP and 3-month mRS score were significantly higher in patients with a total SVD burden score of 2 and 3 than those with a score of 0 and 1 (P < 0.05) (Table 1).
 |
Table 1 Comparison of Baseline Data and Clinical Characteristics of Four SVD Burden Groups |
Outcome Distribution of Four SVD Score Groups
At 3 months, 47 (24.9%) patients developed poor outcome. The proportion of patients with poor outcome increased with the increase of the SVD burden score. When the total SVD burden score was 0, 17% patients had poor outcome, while when the score was 3, the proportion of poor outcome hiked to 78% (Figure 1).
 |
Figure 1 Distribution of mRS score at 3 months in 189 patients according to the total SVD burden score. |
Differences of Risk Factors and Clinical Findings Between the Two Outcome Groups
Compared with patients in the good outcome group, those who developed poor outcome had higher baseline NIHSS scores and higher incidence of SAP. Also, they had heavier burden of lacunes, WMH and EPVS, and thus had elevated total SVD burden score (P < 0.05). Additionally, they were older (P < 0.05) (Table 2).
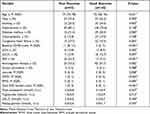 |
Table 2 Differences of Risk Factors and Clinical Findings Between the Two Outcome Groups |
Impact of the Pre-Existing SVD on the 3-Month Outcome in Regression Model
After adjusting for variables with P < 0.2 in the univariate analysis, including age, hypertension, congestive heart failure, baseline NIHSS score, SAP, triglyceride, LDL-C and fasting blood glucose, the WMH (odds ratio [OR] = 2.6777, 95% confidence interval [CI] = 1.052–6.812, P = 0.039) and total SVD burden score (OR = 1.717, 95% CI = 1.072–2.749, P = 0.024) were, respectively, independent risk factors for poor outcome (Table 3).
 |
Table 3 Impact of the Pre-Existing SVD on the 3-Month Prognosis in the Regression Model |
Discussion
The present study described the overall distribution of SVD in CES patients and found that the risk of poor outcome increased with the increase of the SVD burden. WMH and the total SVD burden score were, respectively, independent risk factors for poor prognosis at 3 months.
Different studies have shown that WMH is an indicator of cerebral microcirculation disturbance and is associated with stroke outcome. For example, a study scanned 26 cognitively normal elderly subjects with arterial spin labeling (ASL) sequence, and found that the volume of periventricular WMH was positively correlated with decreased regional cortical blood flow.16 Another study indicated that the severity of leukoaraiosis was negatively associated with leptomeningeal collateral circulation rating in patients with acute large artery occlusion, which further suggested that WMH could disrupt collateral circulation compensation and decrease regional cerebral blood flow.17 As to the effect on stroke outcome, clinical researches indicate that WMH can increase the risk of occurrence and recurrence of stroke, and could hinder its recovery.18,19 Our previous study enrolled CES patients identified by cranial CT or MRI scan and found that WMLs are an independent risk factor for the outcome.20 In this study, patients were evaluated by MRI and it was found that WMH was an independent risk factor for poor prognosis, which was consistent with the results of studies focusing on ischemic stroke with other causes.21
It has been reported that EPVS, one chronic SVD imaging marker in this study, was not associated with the risk of stroke in the general population, nor did it affect the outcome of stroke patients.22 However, it can impact information processing and execution functions.23 In this study, EPVS along with other SVD markers can influence the prognosis of CES, suggesting that there was an accumulative effect caused by multiple SVD markers. To further confirm the accumulative effect, we performed binary regression analysis to investigate the relationship between the total SVD burden score and 3-month prognosis. Results showed that the total SVD burden score was an independent risk factor for the prognosis of CES patients, which was also consistent with previous studies.24,25
Accumulative effect of SVD may influence the outcome of CES patients through the other mechanisms: First, the accumulation of chronic injury of SVD reduces the functional reserve of cerebral tissues.1 Second, it can introduce extensive damage of the brain structure and disrupt the brain neural connections and functional network, so as to impair the brain plasticity and slow down the stroke recovery.26 Lacunes may play a greater role in this aspect, and it was found that they can interrupt the connection of white matter fibers in the deep brain.27 Finally, SVD may impair the cognitive function of patients, lead to post-stroke depression and delay active rehabilitation.28
Our study has some limitations. First, this retrospective study adopted a single center database and had a relatively small sample size, which may increase the selection bias. Second, this study did not assess the CMBs, which, it was shown, may affect the outcome of patients by destroying the vascular brain barrier and increasing the bleeding risk of antithrombotic drugs.29
In conclusion, the pre-existing SVD may be associated with the 3-month prognosis of CES patients. Measures should be taken on the evaluation and management of SVD in such patients.
Abbreviations
ASL, arterial spin labeling; CES, cardioembolic stroke; CI, confidence intervals; CTA, computed tomography angiography; ECG, electrocardiogram; EPVS, enlarged perivascular spaces; FLAIR, fluid attenuated inversion recovery; ICH, intracranial hemorrhage; IQR, interquartile range; MRA, magnetic resonance angiography; MRI, magnetic resonance imaging; mRS, modified Rankin scale; NIHSS, National Institutes of Health Stroke Scale; nsICH, non-symptomatic intracranial hemorrhage; OR, odds ratio; SAP, stroke-associated pneumonia; sICH, symptomatic intracranial hemorrhage; SVD, small vessel disease; WMH, white matter hyperintensities.
Data Sharing Statement
The collected datasets during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Clinical Research Ethics Committee of the Affiliated Changzhou No. 2 People’s Hospital of Nanjing Medical University (approval number: 2018KY032-01). Written informed consents were obtained from all the patients or their legally authorized representatives.
Consent for Publication
A written informed consent for publication was obtained from the patients or their legally authorized representatives. All patient data were de-identified.
Acknowledgment
We thank all the participants and their legally authorized representatives for participating in this study.
Funding
There is no funding to report.
Disclosure
The authors declare that there is no conflict of interest in this work.
References
1. Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18(7):684–696.
2. Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(8):822–838. doi:10.1016/S1474-4422(13)70124-8
3. Lin MP, Brott TG, Liebeskind DS, et al. Collateral recruitment is impaired by cerebral small vessel disease. Stroke. 2020;51(5):1404–1410. doi:10.1161/STROKEAHA.119.027661
4. Tuladhar AM, van Dijk E, Zwiers MP, et al. Structural network connectivity and cognition in cerebral small vessel disease. Hum Brain Mapp. 2016;37(1):300–310. doi:10.1002/hbm.23032
5. Nestor SM, Mišić B, Ramirez J, et al. Small vessel disease is linked to disrupted structural network covariance in Alzheimer’s disease. Alzheimers Dement. 2017;13(7):749–760. doi:10.1016/j.jalz.2016.12.007
6. Cannistraro RJ, Badi M, Eidelman BH, et al. CNS small vessel disease: a clinical review. Neurology. 2019;92(24):1146–1156. doi:10.1212/WNL.0000000000007654
7. Ryu WS, Jeong SW, Kim DE. Total small vessel disease burden and functional outcome in patients with ischemic stroke. PLoS One. 2020;15(11):e0242319. doi:10.1371/journal.pone.0242319
8. Lau KK, Li L, Schulz U, et al. Total small vessel disease score and risk of recurrent stroke: validation in 2 large cohorts. Neurology. 2017;88(24):2260–2267. doi:10.1212/WNL.0000000000004042
9. Huijts M, Duits A, van Oostenbrugge RJ, et al. Accumulation of MRI markers of cerebral small vessel disease is associated with decreased cognitive function. A study in first-ever lacunar stroke and hypertensive patients. Front Aging Neurosci. 2013;5:72. doi:10.3389/fnagi.2013.00072
10. Staals J, Makin SD, Doubal FN, et al. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014;83(14):1228–1234. doi:10.1212/WNL.0000000000000837
11. Huo YC, Li Q, Zhang WY, et al. Total small vessel disease burden predicts functional outcome in patients with acute ischemic stroke. Front Neurol. 2019;10. doi:10.3389/fneur.2019.00808
12. Celeste F, Muratori M, Mapelli M, et al. The evolving role and use of echocardiography in the evaluation of cardiac source of embolism. J Cardiovasc Echogr. 2017;27(2):33–44. doi:10.4103/jcecho.jcecho_1_17
13. Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi:10.1161/01.STR.24.1.35
14. Larrue V, von Kummer RR, Muller A, et al. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001;32(2):438–441. doi:10.1161/01.STR.32.2.438
15. de Montmollin E, Ruckly S, Schwebel C, et al. Pneumonia in acute ischemic stroke patients requiring invasive ventilation: impact on short and long-term outcomes. J Infect. 2019;79(3):220–227. doi:10.1016/j.jinf.2019.06.012
16. Bahrani AA, Powell DK, Yu G, et al. White matter hyperintensity associations with cerebral blood flow in elderly subjects stratified by cerebrovascular risk. J Stroke Cerebrovasc Dis. 2017;26(4):779–786. doi:10.1016/j.jstrokecerebrovasdis.2016.10.017
17. Mark I, Seyedsaadat SM, Benson JC, et al. Leukoaraiosis and collateral blood flow in stroke patients with anterior circulation large vessel occlusion. J Neurointerv Surg. 2020;12(10):942–945. doi:10.1136/neurintsurg-2019-015652
18. Rensma SP, van Sloten TT, Launer LJ, et al. Cerebral small vessel disease and risk of incident stroke, dementia and depression, and all-cause mortality: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;90:164–173. doi:10.1016/j.neubiorev.2018.04.003
19. Song J, Kim KH, Jeon P, et al. White matter hyperintensity determines ischemic stroke severity in symptomatic carotid artery stenosis. Neurol Sci. 2021;42(8):3367–3374. doi:10.1007/s10072-020-04958-6
20. Guo Y, Chen Z, Wang Q, et al. Influence of white matter lesions on the prognosis of acute cardioembolic stroke without reperfusion therapy. BMC Neurol. 2021;21(1):364. doi:10.1186/s12883-021-02372-9
21. Kashima S, Shimizu T, Akiyama H, et al. Magnetic resonance imaging white matter hyperintensity as a predictor of stroke recurrence in patients with embolic stroke of undetermined source. J Stroke Cerebrovasc Dis. 2018;27(12):3613–3620. doi:10.1016/j.jstrokecerebrovasdis.2018.08.033
22. Gutierrez J, Elkind MSV, Dong C, et al. Brain perivascular spaces as biomarkers of vascular risk: results from the northern manhattan study. AJNR Am J Neuroradiol. 2017;38(5):862–867. doi:10.3174/ajnr.A5129
23. Passiak BS, Liu D, Kresge HA, et al. Perivascular spaces contribute to cognition beyond other small vessel disease markers. Neurology. 2019;92(12):e1309–e1321. doi:10.1212/WNL.0000000000007124
24. Song TJ, Kim J, Song D, et al. Total cerebral small-vessel disease score is associated with mortality during follow-up after acute ischemic stroke. J Clin Neurol. 2017;13(2):187–195. doi:10.3988/jcn.2017.13.2.187
25. Liu X, Li T, Diao S, et al. The global burden of cerebral small vessel disease related to neurological deficit severity and clinical outcomes of acute ischemic stroke after IV rt-PA treatment. Neurol Sci. 2019;40(6):1157–1166. doi:10.1007/s10072-019-03790-x
26. Valenti R, Reijmer YD, Charidimou A, et al. Total small vessel disease burden and brain network efficiency in cerebral amyloid angiopathy. J Neurol Sci. 2017;382:10–12. doi:10.1016/j.jns.2017.09.015
27. Reijmer YD, Freeze WM, Leemans A, et al. The effect of lacunar infarcts on white matter tract integrity. Stroke. 2013;44(7):2019–2021. doi:10.1161/STROKEAHA.113.001321
28. Zhi N, Zhang L, Wang Y, et al. Modified cerebral small vessel disease score is associated with vascular cognitive impairment after lacunar stroke. Aging. 2021;13(7):9510–9521. doi:10.18632/aging.202438
29. Wilson D, Ambler G, Lee KJ, et al. Cerebral microbleeds and stroke risk after ischaemic stroke or transient ischaemic attack: a pooled analysis of individual patient data from cohort studies. Lancet Neurol. 2019;18(7):653–665. doi:10.1016/S1474-4422(19)30197-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
