Back to Journals » Journal of Hepatocellular Carcinoma » Volume 10
Inflammation-Related Marker NrLR Predicts Prognosis in AFP-Negative HCC Patients After Curative Resection
Received 13 November 2022
Accepted for publication 20 January 2023
Published 8 February 2023 Volume 2023:10 Pages 193—202
DOI https://doi.org/10.2147/JHC.S393286
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Prof. Dr. Imam Waked
Qionglan Wu,1,2 Jinhua Zeng,2– 4 Jianxing Zeng2,3
1Department of Pathology, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, Fujian, People’s Republic of China; 2Hepatobiliary Medical Center of Fujian Province, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, Fujian, People’s Republic of China; 3Department of Hepatobiliary Surgery, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, Fujian, People’s Republic of China; 4Department of Hepatobiliary Surgery, The First Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian, People’s Republic of China
Correspondence: Jianxing Zeng, Department of Hepatobiliary Surgery, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, 350005, People’s Republic of China, Tel/Fax +86 591 8811 6010, Email [email protected]
Background: The role of inflammation-related markers in alpha-fetoprotein (AFP) negative hepatocellular carcinoma (HCC) is not well known. This study aimed to investigate the clinical significance of inflammation-related markers in AFP-negative HCC patients after curative resection.
Methods: One thousand one hundred and seventy-nine AFP-negative HCC patients after curative resection were included. Survival rate and prognostic analysis were performed using Kaplan-Meier and Cox regression analysis. Propensity score matching (PSM) was used for patient selection.
Results: Multivariate Cox regression showed that neutrophil times γ-glutamyl transpeptidase to lymphocyte ratio (NrLR) was the independent risk factor associated with OS (p = 0.002) and RFS (p = 0.017). Low NrLR groups (n = 628) had lower rates of albumin-bilirubin (ALBI) grade 2 (p < 0.001), lower rates of bleeding and blood transfusion (p < 0.001) than high NrLR groups. Considering tumor features, low NrLR groups had lower AFP levels (p < 0.001), smaller tumor size (p < 0.001), and lower rates of Edmondson grade III–IV (p = 0.024) than high NrLR groups. After PSM, the 1-year, 3 year-, and 5-year OS rates in the low NrLR and high NrLR groups were 96.3%, 86.9%, 64.9%, and 91.4%, 76.7%, 59.5% (p < 0.001), respectively. The 1-year, 3-year, and 5-year RFS rates in the low NrLR and high NrLR groups were 80.0%, 62.9%, 47.5%, and 71.7%, 52.6%, 39.5% (p < 0.001), respectively.
Conclusion: NrLR was a poor prognostic factor for mortality and tumor recurrence in AFP-negative HCC patients after curative resection. The simple and low-cost marker could help physician to determine patients at high risk of tumor recurrence for frequent clinical surveillance.
Keywords: hepatocellular carcinoma, AFP-negative, inflammation, NrLR, liver resection, prognosis
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies worldwide.1 With the development of early diagnosis and treatment of HCC, the long-term survival and quality of life have improved.2,3 Many serum biomarkers have been used for diagnosis and treatment of HCC.4–7
Alpha-fetoprotein (AFP) is the most widely used serum biomarker for HCC in diagnosis and surveillance.8 Elevated AFP is associated with aggressive tumor features and poor prognosis. However, about 35–40% of HCC patients have a negative range of serum AFP (AFP <20ng/mL), which limits the effect of AFP on the diagnosis and prognosis.9 Previous studies have shown that D-dimer, C-reactive protein (CRP), pre-albumin, and some biomarker models can be used as prognostic indicators for AFP-negative HCC patients,10–12 but they are not enough in clinical practice, so it is crucial to look for useful indicators to supervise and predict the outcome of AFP-negative HCC patients.
Inflammation is considered the seventh sign of cancer.13 There is increasing evidence that inflammatory reaction plays an essential part in carcinogenesis.14 Recently, several inflammation-related markers, such as neutrophil to lymphocyte ratio (NLR),15 neutrophil times γ-glutamyl transpeptidase to lymphocyte ratio (NrLR),16 lymphocyte to monocyte ratio (LMR),17 platelet-to-lymphocyte ratio (PLR),18 prognostic nutritional index (PNI),19 and systemic immune-inflammation index (SII)20 have been studied for their prognostic roles among HCC patients. These results show that an unusual relationship between inflammation and HCC. However, the impact of inflammation-related markers on AFP-negative HCC patients is not well known.
To address the issue, we collected a large cohort to investigate the clinical significance of inflammation-related markers in AFP-negative HCC patients after curative resection.
Patients and Methods
Patients
This study was reviewed on patients who underwent R0 liver resection for HCC from January 2008 to December 2014 and was obtained from primary liver cancer big data (PLCBD). The study was performed according to the ethical standards of the Declaration of Helsinki and approved by the institutional ethics committee of Mengchao Hepatobiliary Hospital of Fujian Medical University (NO.:2021_089_01). Informed consent requirement was waived due to the fact that this study did not involve personal privacy or commercial interests and patient data was confidential.
The inclusion criteria included: i) negative level of preoperative serum AFP level (AFP <20ng/mL), ii) no distant metastasis, iii) no macrovascular invasion, iv) curative resection, which was defined as radical hepatectomy of the tumor with normal margins. Exclusion criteria were anticancer therapy, palliative treatment, incomplete data, and lost to follow-up within 2 months after surgery.
Clinicopathologic Variables and Follow-Up
The definition and cut-off value of neutrophil times γ-glutamyl transpeptidase to lymphocyte ratio (NrLR), lymphocyte to monocyte ratio (LMR), platelet to lymphocyte ratio (PLR), prognostic nutritional index (PNI), and systemic immune-inflammation index (SII) are shown in Table 1. We identified the optimal cut-off value for these inflammation-related indexes using the “surv_cutpoint” function from “survminer” R package.
 |
Table 1 The Definition and Cut-off Value of Inflammation-Related Marker |
Patients were followed up once every three months for the first 2 years after discharge from hospitals and every six months in subsequent years. Each visit included physical examination, complete blood count, serum AFP, liver function, abdominal ultrasound, and CT scan. Recurrence was diagnosed on the basis of two concurring imaging techniques or the combination of increased AFP and consistent ultrasonography or CT findings.
Statistical Analysis
The categorical variable was compared by the chi-square test or Fisher’s exact test. Mean (standard deviation, SD) was presented for normally distributed continuous variables and compared using the Student’s t-test. Survival analysis was estimated by the Kaplan–Meier survival method. Prognostic analysis was carried out using the Cox proportional hazards model. A p value of less than 0.05 was considered to be statistically significant. All statistical analyses were performed with R version and SPSS 20.0. The R packages of “table1”, “MatchIt”, “glmnet”, “survminer”, and “survival” were used in this study.
Result
The Study Patients
During the study period, 3961 HCC patients underwent curative resection. A total of 3071 patients who met the inclusion criteria were included in this study. There were 1892 AFP-positive HCC patients and 1179 AFP-negative HCC patients. The flow chart of these patients is shown in Figure 1.
 |
Figure 1 The flow chart in the study. Abbreviations: HCC, hepatocellular carcinoma; AFP, alpha-fetoprotein. |
Independent Factors for OS and RFS in AFP-Negative HCC Patients
Univariate Cox regression analysis for determining the independent factors is shown in Table 2. Multivariate analysis showed that NrLR of >120, PNI of <50, tumor size of ≥5cm, multiple tumor number, MVI, and poor tumor differentiation were the risk factors for OS (Table 3). The NrLR of >120, AFP, tumor size of ≥5cm, multiple tumor number, MVI, and poor tumor differentiation were the risk factors associated with tumor recurrence by multivariate analysis (Table 3). These results showed that NrLR was the independent risk factor associated with OS (p = 0.002) and RFS (p = 0.017) in AFP-negative HCC patients (Table 3).
 |
Table 2 Univariate Cox Regression Analysis of Factors Associated with OS and RFS in AFP-Negative HCC Patients |
 |
Table 3 Multivariable Cox Regression Analysis of Factors Associated with OS and RFS in AFP-Negative HCC Patients |
Comparison of Baseline Features Between Low NrLR and High NrLR Groups in AFP-Negative HCC Patients
As summarized in Table 4, there were 628 NrLR of ≤120 patients (low NrLR groups) and 551 NrLR of >120 patients (high NrLR groups). Low NrLR groups had lower rates of ALBI grade 2 (p < 0.001), lower rates of bleeding and blood transfusion (p < 0.001) than high NrLR groups. Considering tumor features, low NrLR groups had lower rates of elevated AFP levels (p < 0.001), smaller tumor size (p < 0.001), and lower rates of Edmondson grade III–IV (p = 0.024) than high NrLR groups.
 |
Table 4 Baseline Characteristics of Patients |
To minimize potential bias, we matched 435 pairs of patients by propensity score matching. There were no significant differences in baseline characteristics between the low and high NrLR groups (Table 4).
Comparison of Prognosis Between Low NrLR and High NrLR Groups in AFP-Negative HCC Patients
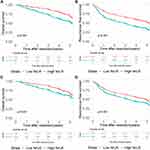
Before PSM, the 1-year, 3-year, and 5-year OS rates in the low NrLR and high NrLR groups were 96.6%, 87.6%, 67.3%, and 91.0%, 73.2%, 53.8% (p < 0.001), respectively (Figure 2A). The 1-year, 3-year, and 5-year RFS rates in the two groups were 82.7%, 66.0%, 51.8%, and 67.6%, 48.4%, 33.8% (p < 0.001), respectively (Figure 2B).
After PSM, the 1-year, 3-year, and 5-year OS rates in the low NrLR and high NrLR groups were 96.3%, 86.9%, 64.9%, and 91.4%, 76.7%, 59.5% (p < 0.001), respectively (Figure 2C). The 1-year, 3-year, and 5-year RFS rates in the two groups were 80.0%, 62.9%, 47.5%, and 71.7%, 52.6%, 39.5% (p < 0.001), respectively (Figure 2D).
Subgroup Analysis
To further compare of prognosis between low NrLR and high NrLR groups in several subgroups, forest plots were performed by tumor features and liver function. In several subgroups (such as hepatitis, ALBI Grade 1, tumor size <5cm, solitary tumor number, MVI, Edmondson-Steiner grade of III–IV, and liver cirrhosis), high NrLR also had worse prognosis than low NrLR, indicating that NrLR could distinguish prognosis in different populations (Figures 3 and 4).
Discussion
Based on our large retrospective cohort study, we found that NrLR was an independent risk factor for OS and RFS in AFP-negative HCC patients after curative resection. A high level of NrLR is associated with more aggressive tumor features, and poorer long-term survival, which was consistently observed in PSM.
Alpha-fetoprotein (AFP) is the most important biomarker used as a screening, diagnostic and prognostic indicator for HCC.21 For healthy adults, elevated AFP is an indication of HCC. For the patients diagnosed with HCC, higher AFP is related to more aggressive tumor features, poorer survival, and poorer treatment responses.22–25 Studies have shown that the long-term outcome of AFP-negative HCC patients was better than AFP-positive patients.26 Even in AFP-negative HCC patients, AFP was still an independent prognostic factor.6 We also found that AFP was associated with recurrence in AFP-negative HCC patients.
At present, the diagnosis and postoperative follow-up of AFP-negative HCC mainly rely on imaging methods.21,27 However, because of the radiation and high cost of CT scanning, it is not recommended to use it in a short period, and ultrasonography is not sensitive to minor lesions, so many clinicians suggest to use other methods, such as hematological biomarkers as the ideal choice for postoperative monitoring.28–30 In this study, we demonstrated that NrLR was the independent risk factor for prognosis in AFP-negative HCC patients. This marker can be calculated from simple, low-cost, and easily obtained blood tests, so this study is of great significance in clinical practice.
NrLR is constituted by neutrophilia count, lymphopenia count, and GGT. Neutrophils and lymphocytes are peripheral blood cells. Studies have shown that neutrophils can accelerate tumor migration and invasion.31,32 On the other hand, lymphocytes play an anti-cancer role in inhibiting tumor recurrence and metastasis.14,33 Moreover, a high level of GGT was related to poor survival.34,35 Accordingly, all of these were adverse factors for HCC patients. The NrLR integration of these three factors can better reflect their impact on HCC. Therefore, NrLR had a strong ability to identify different prognostic groups. However, the mechanism of NrLR in AFP-negative HCC patients remains unclear.
Our study has some limitations. First, it was a retrospective study, which may be affected by bias. Therefore, we used propensity score matching to minimize the difference between two groups. Second, nearly 90% of patients in our cohort were hepatitis B infections, so it should be further validated in different etiology.
In conclusion, our study showed that the NrLR was the significant prognostic factor for OS and RFS in AFP-negative HCC patients after curative resection. The simple and low-cost marker could help physician to determine patients at high risk of tumor recurrence for frequent clinical surveillance.
Data Sharing Statement
All datasets generated for this study are available within the article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Startup Fund for scientific research, Fujian Medical University (2021QH1159), the Medical Innovation Project of Fujian Province (2020CXA055), and the Natural Science Foundation of Fujian Province (2020J011160).
Disclosure
The authors declare no competing interests for this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314.
3. Tandon P, Garcia-Tsao G. Prognostic indicators in hepatocellular carcinoma: a systematic review of 72 studies. Liver Int. 2009;29(4):502–510.
4. Wang K, Guo W, Li N, et al. Alpha-1-fucosidase as a prognostic indicator for hepatocellular carcinoma following hepatectomy: a large-scale, long-term study. Br J Cancer. 2014;110(7):1811–1819.
5. Inagaki Y, Tang W, Makuuchi M, Hasegawa K, Sugawara Y, Kokudo N. Clinical and molecular insights into the hepatocellular carcinoma tumour marker des-γ-carboxyprothrombin. Liver Int. 2011;31(1):22–35.
6. Lin K, Huang Q, Zeng J, et al. Clinical significance of alpha-fetoprotein in alpha-fetoprotein negative hepatocellular carcinoma underwent curative resection. Dig Dis Sci. 2021;66(12):4545–4556.
7. Lu LH, Zhang YF, Wei W, Shi M, Guo RP. Preoperative carbohydrate antigen 19–9: its neglected role in alpha-fetoprotein-negative hepatocellular carcinoma patients. J Gastrointest Surg. 2017;21(12):2025–2032.
8. Galle PR, Foerster F, Kudo M, et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 2019;39(12):2214–2229.
9. Beale G, Chattopadhyay D, Gray J, et al. AFP, PIVKAII, GP3, SCCA-1 and follisatin as surveillance biomarkers for hepatocellular cancer in non-alcoholic and alcoholic fatty liver disease. BMC Cancer. 2008;8:200.
10. She S, Xiang Y, Yang M, et al. C-reactive protein is a biomarker of AFP-negative HBV-related hepatocellular carcinoma. Int J Oncol. 2015;47(2):543–554. doi:10.3892/ijo.2015.3042
11. Wang X, Mao M, He Z, et al. Development and validation of a prognostic nomogram in AFP-negative hepatocellular carcinoma. Int J Biol Sci. 2019;15(1):221–228. doi:10.7150/ijbs.28720
12. Jing W, Peng R, Zhu M, et al. Differential expression and diagnostic significance of pre-albumin, fibrinogen combined with D-Dimer in AFP-negative hepatocellular carcinoma. Pathol Oncol Res. 2020;26(3):1669–1676. doi:10.1007/s12253-019-00752-8
13. Hanahan D, Weinberg R. Hallmarks of cancer: the next generation. Cell. 2011;144:646–674. doi:10.1016/j.cell.2011.02.013
14. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503. doi:10.1016/S1470-2045(14)70263-3
15. Mano Y, Shirabe K, Yamashita Y, et al. Preoperative neutrophil-to-lymphocyte ratio is a predictor of survival after hepatectomy for hepatocellular carcinoma: a retrospective analysis. Ann Surg. 2013;258(2):301–305. doi:10.1097/SLA.0b013e318297ad6b
16. Zeng J, Zeng J, Wu Q, et al. Novel inflammation-based prognostic nomograms for individualized prediction in hepatocellular carcinoma after radical resection. Ann Trans Med. 2020;8(17):1061. doi:10.21037/atm-20-1919
17. Lin Z-X, Ruan D-Y, Li Y, et al. Lymphocyte-to-monocyte ratio predicts survival of patients with hepatocellular carcinoma after curative resection. World J Gastroenterol. 2015;21(38):10898–10906. doi:10.3748/wjg.v21.i38.10898
18. Ma W, Zhang P, Qi J, et al. Prognostic value of platelet to lymphocyte ratio in hepatocellular carcinoma: a meta-analysis. Sci Rep. 2016;6(1):35378. doi:10.1038/srep35378
19. Chan AWH, Chan SL, Wong GLH, et al. Prognostic Nutritional Index (PNI) predicts tumor recurrence of very early/early stage hepatocellular carcinoma after surgical resection. Ann Surg Oncol. 2015;22(13):646–674. doi:10.1245/s10434-015-4516-1
20. Hu B, Yang X-R, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clinl Cancer Res. 2014;20(23):6212–6222.
21. Zhou J, Sun HC, Wang Z, et al. Guidelines for diagnosis and treatment of primary liver cancer in China (2017 edition). Liver Cancer. 2018;7(3):235–260.
22. Cucchetti A, Piscaglia F, Grigioni AD, et al. Preoperative prediction of hepatocellular carcinoma tumour grade and micro-vascular invasion by means of artificial neural network: a pilot study. J Hepatol. 2010;52(6):880–888.
23. Zhu AX, Kang YK, Yen CJ, et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, Phase 3 trial. Lancet Oncol. 2019;20(2):282–296.
24. Zhang B, Zhang B, Zhang Z, et al. 42,573 cases of hepatectomy in China: a multicenter retrospective investigation. Sci China Life Sci. 2018;61(6):660–670.
25. Chan MY, She WH, Dai WC, et al. Prognostic value of preoperative alpha-fetoprotein (AFP) level in patients receiving curative hepatectomy- an analysis of 1182 patients in Hong Kong. Trans Gastroenterol Hepatol. 2019;4:52.
26. Tyson GL, Duan Z, Kramer JR, Davila JA, Richardson PA, El-Serag HB. Level of α-fetoprotein predicts mortality among patients with hepatitis C-related hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2011;9(11):989–994.
27. European Association for the Study of the Liver, Electronic address eee, European Association for the Study of the L. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236.
28. Bialecki ES, Ezenekwe AM, Brunt EM, et al. Comparison of liver biopsy and noninvasive methods for diagnosis of hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2006;4(3):361–368.
29. Liu P, Lu D, Al-Ameri A, et al. Glutamine synthetase promotes tumor invasion in hepatocellular carcinoma through mediating epithelial-mesenchymal transition. Hepatol Res. 2020;50(2):246–257.
30. Toyoda H, Kumada T, Tada T, et al. Clinical utility of highly sensitive Lens culinaris agglutinin-reactive alpha-fetoprotein in hepatocellular carcinoma patients with alpha-fetoprotein <20 ng/mL. Cancer Sci. 2011;102(5):1025–1031.
31. Liang J, Piao Y, Holmes L, et al. Neutrophils promote the malignant glioma phenotype through S100A4. Clin Cancer Res. 2014;20(1):187–198.
32. van der Windt DJ, Sud V, Zhang H, et al. Neutrophil extracellular traps promote inflammation and development of hepatocellular carcinoma in nonalcoholic steatohepatitis. Hepatology. 2018;68(4):1347–1360.
33. Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity. 2004;21(2):137–148.
34. Ma H, Zhang L, Tang B, et al. gamma-Glutamyl transpeptidase is a prognostic marker of survival and recurrence in radiofrequency-ablation treatment of hepatocellular carcinoma. Ann Surg Oncol. 2014;21(9):3084–3089.
35. Fu SJ, Zhao Q, Ji F, et al. Elevated preoperative serum gamma-glutamyl transpeptidase predicts poor prognosis for hepatocellular carcinoma after liver transplantation. Sci Rep. 2016;6:28835.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.