Back to Journals » Journal of Inflammation Research » Volume 16
Inflammation and Coagulation are Two Interconnected Pathophysiological Pathways in Atrial Fibrillation Pathogenesis
Authors Hazarapetyan L , Zelveian PH, Grigoryan S
Received 10 July 2023
Accepted for publication 5 October 2023
Published 31 October 2023 Volume 2023:16 Pages 4967—4975
DOI https://doi.org/10.2147/JIR.S429892
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Lusine Hazarapetyan,1,2 Parounak H Zelveian,2 Svetlana Grigoryan1,2
1Department of Cardiology, Yerevan State Medical University Named After M. Heratsi, Yerevan, Armenia; 2Scientific Research Institute of Cardiology Named After L Hovhannisyan, Yerevan, Armenia
Correspondence: Svetlana Grigoryan, Department of Cardiology, Yerevan State Medical University, 5 P. Sevak Street, Yerevan, 0044, Armenia, Tel +374-91-415 − 123, Email [email protected]
Introduction: Atrial fibrillation (AF) is associated with elevated levels of clotting factors such as tissue factor (TF) and factor XII (FXII). Various inflammation markers, such as interleukin-6 (IL-6), tumor necrosis factor-α (TNF- α), and high-sensitive C-reactive protein (hs-CRP), have also been associated with AF. This study explores the relationship between inflammation markers and coagulation activity, including their impact on heart structural changes in these patients.
Methods: We observed 283 patients with nonvalvular AF who underwent a complete examination at admission, but only 183 patients have successful cardioversion. As a control group, similar patients without AF were examined. The markers of the coagulation and inflammation were studied by ELISA on the analyzer “Stat Fax 303 Plus”. Studies were conducted using l statistical package SPSS 13.0.
Results: It was revealed that patients with AF had significantly higher levels of hs-CRP, IL-6, and TNF-α and had elevated levels of TF and FXII compared with control group. The moderate correlations were observed between IL-6 and left atrial diameter (LAD), IL-6 and LA stiffness, hs-CRP and left atrial volume (LAV), TF and LAV.
Conclusion: We have demonstrated that patients with AF have the relationship between elevated levels of inflammatory markers and coagulation activity, which contributes to structural atrial remodeling.
Keywords: atrial fibrillation, hs-C reactive protein, interleukin-6, tissue factor, factor XII
Introduction
AF is a common arrhythmia and accounts for more than 30% of all types of arrhythmias. This is a heterogeneous type of arrhythmia and is often accompanied by an unfavorable course and severe complications, among which a special place is occupied by heart failure and thromboembolism, in particular stroke. This is evidenced by many studies conducted by various authors. Thus, data from the Framingham Heart Study indicate that AF occurs in more than half of patients with HF, and at the same time, HF occurs in more than a third of patients with AF.1 Overall, AF increases the risk of stroke by five times; however, this risk is heterogeneous and depends on the presence of specific stroke risk factors/modifiers.2 In addition, the odds ratio method showed that non-paroxysmal AF is associated with an increased incidence of thromboembolism (multivariate adjusted HR: 1.38; 95% CI: 1.19–1.61; p < 0.001) compared with paroxysmal AF.3 It is noteworthy that many risk factors for complications associated with AF, in turn, are also risk factors for the occurrence of AF.4 Some authors have concluded that the CHADS2, CHA2DS2-VASc and ABC risk scales have the best evidence for predicting the risk of thromboembolism.5
Currently published data linking the occurrence of thromboembolic risk and its progression with inflammation and fibrosis. Inflammation plays a key role in the initiation and progression of AF. The systemic inflammation markers are easily evaluated and predict AF development. AF is associated with structural and functional anomalies of the myocardium, especially with structural changes in the atria, which may have an inflammatory basis.6,7 Although the role of inflammation in the pathogenesis of AF is still not well understood, it has been found that such classical markers of inflammation as hs-CRP, pro-inflammatory cytokines IL-6 and TNF-α contribute to an increased risk of AF in patients. It was found that their high serum levels increase the risk of AF recurrence in these patients. Therefore, it can be assumed. Those anti-inflammatory mechanisms may provide the basis for new agents that are more likely to prevent recurrent episodes of AF.
Recently, a number of studies have been of great interest, in which the relationship between systemic inflammation and coagulation in patients with AF has been revealed.8 The occurrence of AF is closely related to changes in the blood coagulation system in these patients. There is convincing evidence that inflammation is associated with the onset and maintenance of AF and thrombosis associated with AF. Several prothrombotic factors have been found to be elevated in AF, suggesting abnormal thrombogenesis. So TF is one of the main initiators of coagulation activity. This factor promotes blood coagulation and is involved in the processes of inflammation and angiogenesis.9 TF stimulates and induces the release of pro-inflammatory cytokines. The expression of TF is induced on the surface of endothelial cells and some other cells, as a result of which the “external” pathway of blood coagulation is triggered. TF is a transmembrane glycoprotein and at the same time a surface cell receptor. Its appearance in large quantities in the circulating blood, mainly on the surface of monocytes, is associated with a high risk of thrombosis and thromboembolism.10,11 FXII provides hemostatic balance by participating in the processes of blood coagulation and fibrinolysis. This factor plays a significant role in the subsequent stages of coagulation, namely in the distribution and stabilization of blood clots. FXII regulates inflammatory responses by interacting with the kallikrein-kinin system and initiating the prothrombotic intrinsic pathway of blood clotting. FXII has biological activity in various cells, such as endotheliocytes, platelets, and monocytes, which determines its diverse role in physiological and pathological processes.12,13
This study aims to investigate the relationship between inflammatory markers and coagulation activity in the setting of AF, including the impact of this interaction on clinical presentation and outcome in patients with AF.
Materials and Methods
Ethical Approval of Study Participants
Our study complies with Declaration of Helsinki.
Blood samples were collected from patients with AF in the Department of Arrhythmia at the Research Institute of Cardiology under a protocol (Protocol no.3 of the 28.11.2022) approved by the Ethical Committee of the Research Institute of Cardiology with informed consent from the patients.
Study Patients
We observed 283 patients with ischemic heart disease (IHD) and arterial hypertension (AH) with nonvalvular AF in the Department of Arrhythmia of the Research Institute of Cardiology a year. All instrumental and laboratory studies were performed on patients upon admission to the clinic. After successful cardioversion, 183 patients (average age of 68 ± 6.6 years) with nonvalvular paroxysmal and persistent AF were enrolled. The inclusion criteria also included the presence of ischemic or hypertensive heart disease. Ischemic etiology was defined based on a documented history of myocardial infarction or coronary angiography. ESC guidelines were used to diagnose AH (2018). The exclusion criteria were as follows: ventricular arrhythmia, ventricular tachycardia, acute coronary syndrome, heart failure (functional class more than III by NYHA), bronchial asthma, diabetes, acute inflammatory disease such as influenza, tonsillitis or inflammatory diseases of other organs within the last four months, non-coronary cardiomyopathy (dilated, hypertrophic and obstructive), myocarditis, valvular heart disease, and the thyroid dysfunction. These diseases were excluded based on history, clinical symptoms, and electrocardiogram, echocardiography, and laboratory findings of patients. Patients with paroxysmal AF did not receive anticoagulant therapy, and among the patients with persistent AF only 8 received rivaroxaban (20 mg).
For the gender- and age-matched control group, 88 patients with IHD and AH without AF were examined.
All patients were followed up according to the usual practice of the Arrhythmia Department. All participants underwent a detailed physical examination, including resting 12-lead electrocardiography recording, echocardiography, and 24-hour ambulatory Holter monitoring. BP was calculated from the mean of the second and third readings, and BMI was calculated as weight divided by height and expressed as kg/m². All examined patients were asked to complete a questionnaire about their lifestyle (eg, smoking, drinking, and nutrition) and the presence of potential comorbidities. The clinical characteristics of the patients are presented in Table 1.
 |
Table 1 Baseline Demographics and Clinical Characteristics in Patients with AF and Control Group |
Biochemical and Immunological Blood Measurements
All conventional biochemical analyses were performed on the first-second day of admission to the hospital and carried out in the Research Institute of Cardiology Laboratory. Levels of hs-CRP, IL-6, and TNF-α were measured by ELISA kits according to the manufacturer’s instructions. ELISA kits for the analysis of IL-6 and TNF-α were purchased from BioSource (Belgium) and hs-CRP from DRG International Inc. (USA). The enzyme immunoassay method was used to determine the concentrations of TF and FXII (ELISA, BioMedica Diagnostics, USA, and deficient plasma, native Technoclone, Austria, resp.).
Echocardiography
Standard echocardiography was performed according to the recommendations of the American Society of Cardiology using Medison SonoAce X-6, (Hungary). The size and functional state of the left ventricle (LV), left atrium (LA) and left atrial stiffness (LAs) were determined using the speckle tracking method.14 The LA stiffness was calculated as the ratio of early diastolic mitral inflow velocity-to-early diastolic mitral annular tissue velocity (E/e’) and LA reservoir function (LAS-peak and LAEF-total) (Table 2).
 |
Table 2 Baseline Echocardiographic Characteristics in Patients with AF and Control Group |
Statistical Analysis
Continuous variables were expressed as mean and standard deviation, while categorical variables were presented as numbers or percentages. Comparisons between groups were performed using Student’s t-test for continuous variables as appropriate and χ²-test for categorical variables, and values of p <0.05 were considered statistically significant. The correlation was examined separately in each group using the Pearson method. The correlation coefficient (r) characterizes the value reflecting the degree of relationship between two variables. Studies were conducted based on simple randomized protocols using the universal statistical package SPSS 13.0.
Results
Clinical Characteristics of the Study Participants
Characteristics of patients in the initial state are presented in Table 1. There were no significant differences in age, sex, history of smoking and alcohol consumption, coronary artery disease and hypercholesterolemia. However, in the group of patients with AF, the number of patients with AH and BMI was higher than in the control group, respectively, 88.4 vs 82.7 p < 0.05 and 31.8 vs 28.2 p < 0.05. In both groups of examined patients, there were no differences in heart rate, SBP and DBP at rest, but peak heart rate, peak SBP and DBP significantly increased in AH patients with AF compared with patients without AF, respectively, 122.4 vs 111.2) p < 0.05; 174.1 vs 165.3 and 98.9 p < 0.05 vs 83.4 p < 0.03.
Patients’ baseline echocardiographic characteristics are shown in Table 2. It was revealed that in patients with AF, LAD and LAV were significantly increased compared to those in the control group (LAD: 4.6 ± 1.1* vs 3.8 ± 2.9, p = 0.01; LAV: 61.4 ± 3.1* vs 56.1 ± 2.1, p = 0.043).
EF and LV diastolic and systolic functions were not significantly different between patients with AF and the control group.
Biochemical and Immunological Characteristics of the Study Participants
The analysis of the data showed significant differences between the levels of his-CRP, IL-6, and TNF-α among patients with AF and the control group (7.7 ± 1.4 vs 2.2 ± 0.6, p = 0.002; 37.6 ± 7.1 vs 15.2 ± 5.3, p = 0.03; 1.4 ± 3.1 vs 8.6 ± 4.1, p = 0.01, resp.), indicating an increase in inflammation marker level in patients with AF. The levels of TF and FXII were found to be higher in patients with AF compared to similar patients without AF (1300 ± 50.4 vs 600 ± 11.9, p = 0.026; 231.4 ± 65.4 vs 125.4 ± 46.4, p = 0.033) (Table 3).
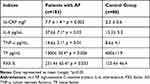 |
Table 3 The Levels of Inflammation Markers and Coagulation Cascade Agents in AF Patients and the Control Group |
We conducted a correlation analysis to identify the relationship between inflammation markers, the coagulation activity and heart structural changes in patients with AF. Accordingly, moderate correlations between IL-6 and LAD (r = 0.464), IL-6 and LA stiffness (r = 0.445), hs-CRP and LAV (r = 0.379), and between TF and LAV (r = 0.543) were found. Moreover, plasma levels of hs-CRP were higher among patients with AF at “high” risk of stroke by CHA2DS2-VASc score (p = 0.003). Furthermore, the levels of hs-CRP and IL-6 are markedly elevated in patients with dilated left atrium (p = 0.001), poorly functioning left atrial appendage (p = 0.023) and longer duration of AF (p = 0.002). Table 3
Discussion
AF is the most common and multifactorial arrhythmia in terms of symptoms and various complications. Among the complications of AF, the most severe are heart failure and thromboembolism, in particular stroke. Acute or chronic hemodynamic, metabolic and electrophysiological processes are considered as pathogenetic mechanisms that can lead to atrial structural remodeling, through which AF develops and progresses. Many predisposing factors have been identified, which can lead to structural remodeling of the atria and then the ventricles, which causes the onset and progression of AF. It has been shown by many authors that dysfunction of the left atrium and ventricles play a significant role in the initiation of AF.15 Currently, identified some metabolic risk factors are known, such as changes in blood coagulation, inflammation, lipid metabolism disorders, which can contribute to the development and recurrence of AF. Some authors indicate that overweight patients often have a higher incidence, prevalence, severity and progression of AF than patients with normal body weight, since obese patients are often a risk factor for AF.16 Arterial hypertension contributes to structural changes in the heart that affect the onset of AF, such as atrial and ventricular remodeling. Arterial hypertension is associated with a 1.8-fold increase in the risk of new-onset AF and a 1.5-fold increase in the risk of progression to permanent AF.17 Regular alcohol consumption is a potentially modifiable risk factor for AF. The researchers found that episodes of AF were associated with a two-fold increase in the likelihood of drinking a single alcoholic drink and a three-fold increase in the likelihood of two or more drinks in the previous four hours. In addition, episodes of AF correlated with increased blood alcohol concentration.18,19
Many researchers believe that inflammation plays a pivotal role in the detection, maintenance and preservation of AF.20–22 Inflammation promotes atrial electrical and structural remodeling via pro-inflammatory cytokines and other inflammatory agents. It also contributes to the increases the substrate for AF in the atria, which leads to the maintenance of AF and further inflammation, which forms a vicious circle, the so-called “AF generates AF”. It is known that such inflammatory markers as his-CRP, IL-6 and TNF-α are multilaterally involved in the formation of the AF substrate.
Among the various biological and immunological markers used in clinical practice to detect active inflammation, a special place is given to CRP, which belongs to the family of proteins of the acute phase of inflammation. The concentration of CRP is considered as the most sensitive and specific laboratory marker of inflammation and tissue damage and correlates with the synthesis of IL-6, which in turn plays an important role in the development of the so-called immune inflammation.
So, hs-CRP is a biomarker that is often used to determine the presence and severity of inflammation. As a classic inflammatory marker, hs-CRP is the major acute-phase protein and sensitive indicator of inflammation. Thus, hs-CRP elevation may be a nonspecific response to any environmental stimulus. Moreover, it may not be directly or indirectly related to the pathogenesis of AF. Its synthesis by the liver is regulated to a large extent by the proinflammatory cytokines, such as IL-6 and TNF-α. In the study,23 an increased level of CRP was found among patients with AF compared with patients with sinus rhythm. It turned out that in patients with paroxysmal and persistent AF, CRP was higher than in the control group in patients without AF. Researchers24 conducted a study in which 5806 patients were involved. Follow-up lasted up to 7.8 years. The role of CRP as a predictor of the development of AF was assessed, which was initially diagnosed in 315 (5%) patients. It turned out that patients with high levels of CRP are more susceptible to the development of AF than patients with low levels of CRP (7.4% vs 3.7%). Thus, CRP is not only associated with the presence of AF but also represents a high risk for the further development of AF. This opinion is shared by many authors.25,26
IL-6 and TNF-as components of inflammation usually determine cell survival, stimulation or inhibition of their growth, differentiation, their functional activation and apoptosis by signaling cells along the signaling pathway. Such activity of cytokines contributes to the development of hypertrophy of cardiomyocytes and leads to disruption of endothelium-dependent vasodilation. It was revealed that the mechanism of action of cytokines is their negative inotropic effect on cardiomyocytes, the effect on heart remodeling, the disruption of endothelium-dependent dilatation of arterioles, and the increased apoptosis of cardiomyocytes.27–29 Meta-analysis showed that high plasma levels of IL-6 were associated with a high risk of AF in the general population and recurrence of AF after electrical cardioversion and radiofrequency ablation30 Many authors believe that with an increase in the level of IL-6, certain disorders are observed that lead to pathological changes, including inflammatory lesions, the formation and rupture of plaques that promote thrombosis. These changes have a stimulating effect on the development of cardiovascular pathology, including AF.29
Recent studies point to a key role for inflammatory signaling in cardiomyocytes in the development of AF, emphasizing the importance of nonleukocyte heart cells in mediating cardiac inflammation. In particular, the NLRP3 inflammasome is involved in cardiomyocyte-mediated inflammatory signaling in AF. In addition, an animal model study indicates that activation of the NLRP3 inflammasome in atrial cardiomyocytes may be a necessary condition for the onset of AF.31 Thus, existing studies prove that inflammation plays a significant role in the pathogenesis of AF and therefore the treatment of its initiating agents can lead to an improvement in the condition of patients with this type of arrhythmia. In all likelihood, inflammatory markers such as hs-CRP, IL-6, and TNF-α can also be considered risk factors for AF recurrence.32–34 In summary, inflammatory markers such as IL-6, TNF-α, and hs-CRP have previously been associated with AF. Our data showed that patients with AF had statistically significant high levels of these markers compared with those in the control group (7.7 ± 1.4 versus 2.2 ± 0.60, p = 0.002; 37.6 ± 7 0.1 vs 15.2 ± 5.3, p = 0.03, 14.6 ± 3.1 vs 8.6 ± 4.1, p = 0.01, respectively).
Moreover, we found the correlation between IL-6 and LAD (r = 0.464), IL-6 and LA stiffness, hs-CRP and LAV (r = 0.379). Atrial remodeling involves electrophysiological and structural abnormalities that promote the development and recurrence of AF. The links between atrial remodeling and inflammation are complex. However, such correlations can be explained by the fact that IL-6 and hs-CRP, as markers of inflammation, are involved in the processes of atrial remodeling, ie, in the formation of atrial hypertrophy and endothelium-dependent vascular dilations. In addition, this confirms the assumption of the authors,35 about the role of inflammatory signaling in cardiomyocytes in the development of AF.
A significant risk of thromboembolic complications is one of the main clinical problems in patients with AF. As is known, the state of blood coagulation activity is of particular importance for the occurrence of AF. Inflammation initiates blood clotting, reduces the activity of natural anticoagulant mechanisms and disrupts the fibrinolytic system. Researchers36 concluded that in patients with AF, high levels of IL-6 are associated with thromboembolism and major bleeding and are an independent risk factor for thromboembolic events.
As we know, the blood coagulation system is activated in response to damage to the vessel in order to preserve its integrity. Tissue factor (TF) formerly known as thromboplastin is one of the primary cellular initiators of blood coagulation. As a result of damage to the vessel wall, TF takes part in the activation of a whole cascade of coagulation proteases, which leads to the deposition of fibrin and activation of platelets. TF is also a trigger for starting the “external” pathway of blood coagulation. TF expression and activity can be induced in endothelial cells, vascular smooth muscle cells, and monocytes by various stimuli, such as cytokines, growth factors, and biogenic amines.11 The intrinsic coagulation pathway is activated by factor XII and the kinin-kallikrein system which is involved in the processes of inflammation, coagulation and arterial pressure regulation. The coagulation factor XII, which functions separately, can independently induce the formation of fibrin thrombi.12 Our data indicate that the concentrations of coagulation activity indices, such as TF and XII, are significantly higher in patients with AF than in similar patients without AF (1300 ± 50.4 vs 600 ± 11.9, p = 0.026; 231, 4 ± 65.4 vs 0.026, 125.4 ± 46.4, p = 0.033). This fact can most likely be explained by the fact that patients with AF have more significant damage to the vascular wall than similar patients without AF. Moreover, elevated levels of inflammatory markers in AF patients play a role in this damage.
Inflammation and coagulation are two defense systems with complementary roles in limiting tissue damage and restoring homeostasis. Extensive cross-relationships exist between these two systems, whereby activation of the coagulation system and ensuing thrombin generation are dependent on the expression of TF. Conversely, activated coagulation proteases may affect specific receptors on inflammatory and endothelial cells, thereby modulating the inflammatory response.37–39 TF can enter the bloodstream with fragmented membrane particles of various cell types, such as leukocytes and platelets, and through the activation of endothelial cells and monocytes. Given the variety of mechanisms that can cause TF contact with inflammatory blood components, such as hs-CRP and IL-6, the high levels of TF in the study patient group could be of multicomponent origin. FXII contributes to the stabilization of thrombosis. The activity of both indicators TF and FXII in the patient group was significantly higher than that in the control group. The deterioration of endothelial function in AF may also be the result of inflammation, which leads to changes in the endothelium and, accordingly, to thromboembolic aggression. TF acting on the damaged subendothelium contributes to an increase in coagulation activity in the atria39,40 Moreover, according to the study,41 pro-inflammatory markers may enhance thrombotic events by upregulating TF expression in endothelial cells and monocytes. In all likelihood, this circumstance can explain the correlation we obtained between TF and LAV: r = 0.543.
Conclusions
We evaluated the relationship between baseline levels of inflammatory markers and coagulation in patients with non-valvular AF compared with similar patients without AF. It turned out that inflammation is one of the most important components of the pathogenesis of AF, which is confirmed by us and probably, by acting on the endothelium of the vessel wall, it causes the activation of such agents of the coagulation activity as TF and FXII. This is why we have demonstrated that elevated plasma levels of inflammation markers are associated with measures of coagulation activity and may promote atrial structural remodeling in patients with AF.
Thus, it can be said that in patients with AF, the processes of inflammation and coagulation are interconnected, represent two systems and interrelated pathways that play an important role in the pathogenesis of the onset and progression of AF.
Abbreviations
AF, atrial fibrillation; AH, arterial hypertension; BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; DT, deceleration time; EF, ejection fraction; HF, heart failure; HR, heart rate; hs-СRP, high-sensitive C-reactive protein; IHD, ischemic heart disease; IL-6, interleukin-6; IVRT, isovolumetric relaxation time; IVST, interventricular septum thickness; FXII, factor XII; LAD, left atrial diameter; LAV, left atrial volume; LA stiffness, left atrial stiffness; LVEDD, left ventricular end-diastolic diameter; LVESD, left ventricular end-systolic diameter; LVPWT, left ventricular posterior wall thickness; SBP, systolic blood pressure; TNF-α, tumor necrosis factor-α; TF, tissue factor.
Ethical Approval of Study Participants
The database is collected from atrial fibrillation patients in the Department of Arrhythmia at the Research Institute of Cardiology named after L. Hovhannisyan (Yerevan, Armenia), approved by the Local Ethical Committee (Protocol no.3 of the 05.11.2022) and with informed consent from the patients.
Acknowledgments
The authors thank the patients who participated in this study and donated their samples, the staff of the Department of Arrhythmia and Immunological laboratory of the Research Institute of Cardiology.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, methodology, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The work was supported by the Science Committee of MESCS RA, in the frames of the research project №21T-3B328.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development of atrial fibrillation: the Framingham heart study. Circulation. 2004;110(9):1042–1046. doi:10.1161/01.cir.0000140263.20897.42
2. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
3. N. GA, P. CD, Hartshorne T, et al. The impact of atrial fibrillation type on the risk of thromboembolism, mortality and bleeding: a systematic review and meta-analysis. Eur Heart J. 2016;37(20):1591–1602. doi:10.1093/eurheartj/ehw007
4. Chao TF, Liao JN, Tuan TC, et al. Incident co-morbidities in patients with atrial fibrillation initially with a CHA2DS2-VASc score of 0 (males) or 1 (females): implications for reassessment of stroke risk n initially ‘low-risk’ patients. Thromb Haemost. 2019;119:1162–1170. doi:10.1055/s-0039-1683933
5. Bone ED, Goode A, Raitz G, et al. Sender G.D Predicting thromboembolic and bleeding event risk in patients with non-valvular atrial fibrillation: a systematic review. Thromb Haemost. 2018;118:2171–2187. doi:10.1055/s-0038-1675400
6. Harada M, Van Wagoner DR, Nattel S. Role of inflammation in atrial fibrillation pathophysiology and management. Circulation. 2015;79(3):495–502. doi:10.1253/circj.CJ-15-0138
7. Choi YJ, Choi EK, Han KD, et al. Increased risk of atrial fibrillation in patients with inflammatory bowel disease: a nationwide population-based study. World J Gastroenterol. 2019;25(22):2788–2798. doi:10.3748/wjg.v25.i22.2788
8. Cianfrocca C, Loricchio ML, Pelliccia F, et al. C-reactive protein and left atrial appendage velocity are independent determinants of the risk of thrombogenesis in patients with atrial fibrillation. Int J Cardiol. 2010;142:22–28. doi:10.1016/j.ijcard.2008.12.052
9. Li YG, Lee SR, Choi EK, G.y L. Stroke prevention in atrial fibrillation: focus on Asian patients. Korean Circ J. 2018;48:665–684. doi:10.4070/kcj.2018.0190
10. Foley JH, Conway EM. Cross talk pathways between coagulation and inflammation. Circ Res. 2016;118:1392–1408. doi:10.1161/CIRCRESAHA.116.306853
11. Lin KB, Fan FH, Cai MQ, et al. Systemic immune inflammation index and system inflammation response index are potential biomarkers of atrial fibrillation among the patients presenting with ischemic stroke. Eur J Med Res. 2022;27(1):106. doi:10.1186/s40001-022-00733-9
12. Mailer RK, Rangaswamy C, Konrath S, Emsley J, Renné TH. An update on factor XII-driven vascular inflammation. Biochim Biophys Acta Mol Cell Res. 2022;1869(1):119166. doi:10.1016/j.bbamcr.2021.119166
13. Ma L, Willey J. The interplay between inflammation and thrombosis in COVID-19: mechanisms, therapeutic strategies, and challenges. Thrombosis Update. 2022;8:100117. doi:10.1016/j.tru.2022.100117
14. Zhu S, Lin Y, Zhang Y, et al. Prognostic relevance of left atrial function and stiffness in heart failure with preserved ejection fraction patients with and without diabetes mellitus. Front Cardiovasc Med. 2022;14:947639. doi:10.3389/fcvm.2022.947639.;
15. Brandes A, Smit MD, Nguyen BO, Rienstra M, Van Gelder IC. Risk factor management in atrial fibrillation. Arrhythm Electrophysiol Rev. 2018;7(2):118–127. doi:10.15420/aer.2018.18.2
16. Jones NR, Taylor KS, Taylor CJ, Aveyard P. Weight change and the risk of incident atrial fibrillation: a systematic review and meta-analysis. Heart. 2019;105(23):1799–1805. doi:10.1136/heartjnl-2019-314931
17. Ogunsua AA, Shaikh AY, Ahmed M, McManus DD. Atrial fibrillation and hypertension: mechanistic, epidemiologic, and treatment parallels. Methodist DeBakey Cardiovasc J. 2015;11(4):228–234. doi:10.14797/mdcj-11-4-228
18. Kim YG, Han K, Choi JI, et al. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: a nationwide population-based study. EP Europace. 2020;22(2):216–224. doi:10.1093/europace/euz256
19. Csengeri D, Sprünker NA, Castelnuovo AD, et al. Alcohol consumption, cardiac biomarkers, and risk of atrial fibrillation and adverse outcomes.European. Heart Journal. 2021;42(12):1170–1177. doi:10.1093/eurheartj/ehaa953
20. Lee KWJ, Hill JS, Walley KR, et al. Relative value of multiple plasma biomarkers as risk factors for coronary artery disease and death in an angiography cohort. CMAJ. 2006;174:461–466. doi:10.1503/cmaj.050880
21. Ihara K, Sasano T. Role of inflammation in the pathogenesis of atrial fibrillation. Front Physiol. 2022;13:862164. doi:10.3389/fphys.2022.862164
22. Yao Y, Yang M, Liu D, et al. Immune remodeling and atrial fibrillation. Front Physiol. 2022;13:927221. doi:10.3389/fphys.2022.927221
23. Boss CHJ, Anderson RA, Lip GYH. Is atrial fibrillation an inflammatory disorders? Eur Heart J. 2006;27:136–149. doi:10.1093/eurheartj/ehi645
24. Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108(24):3006–3010. doi:10.1161/01.CIR.0000103131.70301.4F
25. Boyalla V, Harling L, Snell A, et al. Biomarkers as predictors of recurrence of atrial fibrillation post ablation: an updated and expanded systematic review and meta-analysis. Clin Res Cardiol. 2022;111(6):680–691. doi:10.1007/s00392-021-01978-w
26. Pauklin P, Zilmer M, Eha J, Tootsi K, Kals M, Kampus P. Markers of inflammation, oxidative stress, and fibrosis in patients with atrial fibrillation. Oxid Med Cell Longev. 2022;2022:4556671. doi:10.1155/2022/4556671
27. Terrell AM, Crisostomo PR, Wairiuko GM, Wang M, Morrell ED, Meldrum DR. Jak/STAT/SOCS signaling circuits and associated cytokine-mediated inflammation and hypertrophy in the heart. Shock. 2006;26:226–234. doi:10.1097/01.shk.0000226341.32786.b9
28. Fontes JA, Rose NR, Čiháková D. The varying faces of IL-6: from cardiac protection to cardiac failure. Cytokine. 2015;74(1):62–68. doi:10.1016/j.cyto.2014.12.024
29. Su JH, Luo MY, Liang N, et al. Interleukin-6: a novel target for cardio-cerebrovascular diseases. Front Pharmacol. 2021;12:745061. doi:10.3389/fphar.2021.745061
30. Wu N, B. X, Xiang Y, et al. Association of inflammatory factors with occurrence and recurrence of atrial fibrillation: a meta-analysis. Int J Cardiol. 2013;169(1):62–72. doi:10.1016/j.ijcard.2013.08.078
31. Dobrev D, Heijman J, Hiram R, et al. Inflammatory signalling in atrial cardiomyocytes: a novel unifying principle in atrial fibrillation pathophysiology. Nat Rev Cardiol. 2023;20:145–167. doi:10.1038/s41569-022-00759-w
32. Dzeshka MS, Lip GY, Snezhitskiy V, Shantsila E. Cardiac fibrosis in patients with atrial fibrillation: mechanisms and clinical implications. J Am Coll Cardiol. 2015;66(8):943–959. doi:10.1016/j.jacc.2015.06.1313
33. Jalife J, Kaur K. Atrial remodeling, fibrosis, and atrial fibrillation. Trends Cardiovasc Med. 2015;25(6):475–484. doi:10.1016/j.tcm.2014.12.015
34. Nso N, Kaveh R, Bookani MM, Radparvar F. Role of inflammation in atrial fibrillation: a comprehensive review of current knowledge. J Arrhythmia. 2021;37:1. doi:10.1002/joa3.12473
35. Guzel T, Kış M, Şenöz O. The correlation between the left atrial volume index and atrial fibrillation development in heart failure with mildly reduced ejection fraction and long-term follow-up results. Acta Cardiol. 2022;77(7):647–654. doi:10.1080/00015385.20222.2067674
36. Aulin J, Siegbahn A, Hijazi Z, et al. Interleukin-6 and C-reactive protein and risk for death and cardiovascular events in patients with atrial fibrillation. Am Heart J. 2015;170(6):1151–1160. doi:10.1016/j.ahj.2015.09.018
37. Li X, Peng S, Wu X, et al. C-reactive protein and atrial fibrillation: insights from epidemiological and Mendelian randomization studies Meta-Analysis. Nutr Metab Cardiovasc Dis. 2022;32(6):1519–1527. doi:10.1016/j.numecd
38. Vojacek JF. Should we replace the terms intrinsic and extrinsic coagulation pathways with tissue factor pathway? Clin Appl Thromb Hemost. 2017;23(8):922–927. doi:10.1177/1076029616673733
39. Stark K, Massberg S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat Rev Cardiol. 2021;18:666–682. doi:10.1038/s41569-021-00552-1
40. Yau JW, Teoh H, Verma S. Endothelial cell control of thrombosis. BMC Cardiovasc Disord. 2015;15:130. doi:10.1186/s12872-015-0124-z
41. D’Alessandro E, Posma JJN, Spronk HMH, Ten Cate H. Tissue factor (Factor VIIa) in the heart and vasculature: more than an envelope. Thromb Res. 2018;168:130–137. doi:10.1016/j.thromres.2018.06.020
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
