Back to Journals » Nature and Science of Sleep » Volume 15
Individualized Treatment Patterns for Patients with Narcolepsy Treated with Oxybate: A Clinical Practice Perspective
Authors Roy A, Ito D , Morris S, Candler S, Profant J, Bae C
Received 10 March 2023
Accepted for publication 8 August 2023
Published 29 September 2023 Volume 2023:15 Pages 767—778
DOI https://doi.org/10.2147/NSS.S411727
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Sarah L Appleton
Asim Roy,1 Diane Ito,2 Susan Morris,3 Shawn Candler,4 Judi Profant,3 Charles Bae5
1Ohio Sleep Medicine Institute, Dublin, OH, USA; 2Stratevi LLC, Santa Monica, CA, USA; 3Jazz Pharmaceuticals, Palo Alto, CA, USA; 4Jazz Pharmaceuticals, Philadelphia, PA, USA; 5Penn Sleep Center, University of Pennsylvania, Philadelphia, PA, USA
Correspondence: Asim Roy, Ohio Sleep Medicine Institute, 4975 Bradenton Avenue, Dublin, OH, 43017, USA, Tel +1 614-766-0773, Fax +1 614-766-2599, Email [email protected]
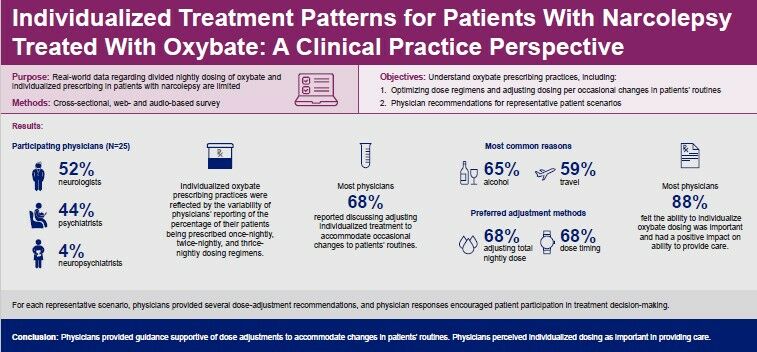
Purpose: Real-world data regarding divided nightly dosing of oxybate and individualized prescribing in patients with narcolepsy are limited. Study objectives were to understand oxybate prescribing practices, including optimizing dose regimens and adjusting dosing per occasional changes in patients’ routines, and physician recommendations for representative patient scenarios.
Patients and Methods: A cross-sectional, web- and audio-based survey of physicians treating ≥ 2 patients with narcolepsy, prescribed nightly oxybate (sodium oxybate) dosing for ≥ 6 months, was conducted. Physicians were surveyed on patients’ usual oxybate dosing regimens, frequency of and reasons for oxybate dosing-related discussions, and preferred methods for and perceptions of adjusting oxybate dosing. Physicians provided dosing-related guidance for 4 representative scenarios.
Results: Participating physicians (N=25) were neurologists (52%), psychiatrists (44%), and neuropsychiatrists (4%). Individualized oxybate prescribing practices were reflected by the variability of physicians’ reporting of the percentage of their patients being prescribed once-nightly, twice-nightly, and thrice-nightly dosing regimens. Most physicians (68%) reported discussing adjusting individualized treatment to accommodate occasional changes to patients’ routines; the most common reasons were consuming contraindicated beverages (alcohol; 65%) and travel (59%). Adjusting total nightly dose (68%) and dose timing (68%) were preferred adjustment methods. Most physicians (88%) felt the ability to individualize oxybate dosing was important and had a positive impact on ability to provide care. For each representative scenario, physicians provided several dose-adjustment recommendations, and physician responses encouraged patient participation in treatment decision-making.
Conclusion: Physicians provided guidance supportive of oxybate dose adjustments to accommodate occasional changes in patients’ routines, and perceived individualized dosing as important in providing care.
Plain Language Summary: Why was the research needed?
Narcolepsy is an uncommon condition that causes individuals to feel sleepy throughout the day. Other symptoms may include sudden muscle weakness. There is no cure for narcolepsy, but there are several treatments, including medicines known as oxybates. This study focused on how doctors use oxybate to treat patients with narcolepsy.
How was the research done?
This study was an online survey of doctors who were treating 2 or more patients with narcolepsy. Patients had been taking oxybate for at least 6 months. The survey asked doctors about their patients’ normal oxybate usage, how often and why they discussed oxybate treatment, and which ways oxybate treatment was usually adjusted.
What are the results?
Twenty-five doctors took part in this study. Most doctors said they discuss personalized treatment to help with occasional changes in their patients’ daily lives. The most common reasons for making treatment changes were consuming alcohol and travel. The most common changes were total nightly amount and timing of oxybate. Most doctors said the ability to personalize oxybate treatment is important and has a positive impact.
What does the research mean?
This study provides valuable knowledge on real-world oxybate treatment patterns and the conditions when doctors make clinical decisions about treating patients with narcolepsy.
Keywords: sodium oxybate, low-sodium oxybate, calcium, magnesium, potassium, sodium oxybates, prescribing patterns, personalized dosing
Graphical Abstract:
Introduction
Narcolepsy is a lifelong neurological disorder characterized by excessive daytime sleepiness (EDS), sleep paralysis, disrupted nighttime sleep, hypnagogic or hypnopompic hallucinations, cataplexy (defined as a sudden loss of muscle tone most often elicited by strong emotion), and automatic behaviors.1,2 Narcolepsy consists of 2 subtypes: type 1 (with cataplexy) and type 2 (without cataplexy).3 While prevalence estimates vary, narcolepsy has been estimated to affect up to 0.05% of the general population, or 200,000 people in the United States (US).1,4
American Academy of Sleep Medicine practice parameters and guidelines for narcolepsy have recommended that the major objectives of treatment should be to alleviate daytime sleepiness and control cataplexy, hallucinations, sleep paralysis, and disrupted nocturnal sleep.5,6 The overall goal should be to enable patients to function normally at work, school, and home, and socially, to the fullest extent possible.5 Equally notable, treatment recommendations from narcolepsy experts cite a need to individualize therapy by considering additional factors, such as the patient’s age, psychosocial circumstances, treatment goals and preferences, and other lifestyle situations.1,7,8 Individualization of pharmacologic treatment for narcolepsy may involve the tailoring of the timing, regimen, and dosage of treatments.1,9
Although there is currently no cure for narcolepsy, many treatment options are available to manage symptoms.10 Multiple well-controlled clinical studies have demonstrated that oxybates (sodium oxybate [Xyrem®, SXB]; calcium, magnesium, potassium, and sodium oxybates [Xywav®, low-sodium oxybate, LXB]) are effective in the treatment of cataplexy and EDS in adult and pediatric patients with narcolepsy; both are approved by the US Food and Drug Administration (FDA) for the treatment of cataplexy or EDS in patients 7 years of age and older with narcolepsy.11–21 SXB has shown improvements in polysomnography and patient-reported nocturnal sleep, both features of disrupted nighttime sleep.22 SXB has also displayed decreases in body mass index (BMI) in patients with narcolepsy type 1, particularly in those with higher BMI.23 LXB and SXB are individually titrated to each patient’s most effective and tolerable (optimal) dose. The prescribing information for patients with narcolepsy recommends that LXB and SXB be taken twice nightly, with the total nightly dose divided into 2 doses (equal or unequal for LXB only).17,18 Twice-nightly dosing provides physicians the capability to individualize patients’ treatment to optimize dosing regimens and/or to accommodate occasional changes in patients’ routines, such as those that might arise from social activities or personal obligations. The ability to adjust treatment regimens may motivate patients to become active participants in their treatment, and may increase adherence and success in achieving treatment goals and outcomes.24–26 It is important to better understand the clinical practitioner’s considerations in individualizing dosing regimens or specific dose adjustments, and under which circumstances they make these decisions.
Currently, there are few published studies of oxybate treatment patterns in the clinical practice setting. Real-world dosing was reported in 2 studies of SXB in clinical practice: a single-site retrospective study in 90 patients with refractory narcolepsy with cataplexy27 and a multisite non-interventional study of 670 patients with narcolepsy.28 In an analysis of self-reported oxybate use in the Nexus Narcolepsy Registry, 95% of patients reported taking SXB twice nightly.29 In a recent observational study of 23 patients with narcolepsy type 1, the mean SXB dose was <6 g/night.30 However, these studies provided few details regarding dosing regimens for individual patients across the duration of treatment.
This study was conducted to assess physicians’ treatment patterns for oxybate optimization in patients with narcolepsy and to understand dosing adjustment guidance that physicians provide to patients to accommodate changes in patients’ lifestyles.
Materials and Methods
Study Design
The study was conducted from September 2018 until July 2019 and consisted of a web- and phone-based, cross-sectional survey administered to 25 US-based, board-certified sleep medicine physicians meeting the following inclusion criteria: previously treated at least 10 patients with narcolepsy; treated at least 5 patients with narcolepsy in the past 12 months; prescribed oxybate (SXB, the only approved and available oxybate during this study period) for at least 3 patients with narcolepsy in the past 12 months; and currently treating at least 2 patients with narcolepsy with oxybate who have been taking oxybate for at least 6 months. The goal of these inclusion criteria was to ensure that participating physicians have adequate experience in prescribing divided doses of oxybate for patients with narcolepsy.
Data collected from the web-based survey included physician demographics, practice characteristics, oxybate prescribing practices (usual regimen and dose adjustments), circumstances of dosing adjustments, perceptions of dosing adjustment, perceptions of impact of ability to vary dosing, and effectiveness of dosing adjustment (physicians provided subjective responses based on their experiences). In addition to the web-based survey, physician participants were also presented with 4 patient vignettes representative of situations/circumstances experienced by patients with narcolepsy during the course of treatment and were asked to provide their commentary on these vignettes via an automated voice response system. The patient scenarios were confirmed to be representative based on the findings of an additional real-world evidence study.31 Each vignette featured a patient with narcolepsy prescribed oxybate who had been on a stable optimal dose and also had a specific life event or circumstance for which the patient contacted the prescribing physician to seek individualized dosing guidance. These life events included getting up early to catch a flight, attending a late-evening work event, waking up in the middle of the night to care for a child, and being able to drink alcohol on occasion with friends (Table 1). After dialing a designated phone number, participants verbally recorded the treatment guidance that they would provide to each of these representative patients.
 |
Table 1 Physician Recommendations for Oxybate Dosing Adjustments for Representative Patient Vignettes |
Statistical Analysis
As this was an exploratory study, descriptive statistics were used to summarize the results. For continuous variables such as number of patients treated and number of years in practice, results included number of respondents (n), mean, standard deviation (SD), minimum, median, and maximum. For categorical variables such as physician specialty and practice setting, results included frequency and percentage. Content analysis was conducted on the qualitative voice response data to identify emergent themes and patterns. All quantitative analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA). Given the observational nature of this study, power calculations were not conducted to determine the optimal target sample size. A target of 25 participants was considered adequate to generate estimates of study endpoints with reasonable precision of study endpoint data.
Results
Twenty-five board-certified US physicians with a primary specialty of neurology, psychiatry, or neuropsychiatry and a mean (±SD) of 16 (±8) years in practice participated in the study (Table 2). On average, participating physicians were treating 25 (±27) patients with oxybate.
 |
Table 2 Physician and Practice Characteristics |
Oxybate Usual Dosing Prescribing Patterns
With respect to oxybate dosing regimen capability, on average, physicians reported that 50% (±30%) of their patients had been prescribed a twice-nightly dosing regimen, 39% (±29%) had been prescribed a once-nightly regimen, and 10% (±17%) had been prescribed a thrice-nightly regimen while on treatment (Figure 1), which highlights the importance of individualized treatment. Physicians reported that, on average, 69% (±28%) of their patients were prescribed equally divided (equal) doses, and 30% (±29%) were prescribed unequally divided (unequal) doses (Figure 2). Two (8%) physicians reported that all (100%) of their patients were prescribed a twice-nightly dosing regimen (Figure 1), and 8 (32%) physicians reported that all (100%) of their patients who take multiple nightly doses were prescribed equally divided dosing regimens.
 |
Figure 1 Physician-reported percentages of patients with once-, twice-, and thrice-nightly oxybate dosing regimens. |
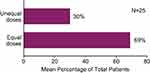 |
Figure 2 Patients with equal and unequal oxybate dosing. |
Individualized Dosing to Achieve Efficacy and Accommodate Patient Lifestyles
Physicians described dosing-adjustment conversations with patients as a common occurrence. Physicians felt that adjustments due to lifestyle changes were patient initiated, whereas adjustments based on achieving efficacy were generally physician initiated. Seventeen (68%) physicians reported discussing oxybate dosing adjustments to accommodate occasional changes in their patients’ routines, whereas 4 (16%) had not; 4 (16%) could not recall. Consuming contraindicated beverages (alcohol) (65%) and needing to travel (59%) were the most common situations for discussing oxybate dosing adjustments (Figure 3). Other circumstances included eating food within 2 hours of bedtime (47%), attending a work event/working late or early (47%), attending a social event (47%), spending the night with a bed partner (47%), and needing to take another medication (47%). For many physicians, there was more than 1 reason to adjust their patients’ dosing regimens as implied by the spread of responses.
 |
Figure 3 Circumstances discussed with patients regarding dose adjustments. *Only respondents who answered “Yes” to whether or not they discussed dose adjustment with patients received this question. |
Most physicians considered multiple approaches to providing guidance for dosing adjustment (Figure 4). For example, 17 (68%) physicians noted individualizing the timing of the doses and/or the total nightly dose, for reasons including time change in travel, a new bed partner, schedule changes, concomitant medications (eg, sedatives), reduction of daytime drowsiness, shift work, and to achieve other goals. Just under half (48%) of physicians recommended changing the number of doses (ie, taking a single dose rather than 2, or 2 doses rather than 3), for reasons including encouraging adherence, improving wakefulness the next day, work responsibilities, family obligations, a late bedtime, and alcohol consumption. Around a third (36%) of physicians recommended changing the division of the total nightly dose (ie, unequally divided rather than equally divided) for reasons including efficacy and safety/tolerability (eg, prescribing a higher initial dose and lower second dose to achieve better treatment response).
 |
Figure 4 Types of individualized dosing guidance considered by physicians. |
Physician Perceptions Regarding Ability to Adjust Oxybate Dosing Regimen
Physician perceptions regarding the ability to individualize oxybate dosing regimens to accommodate their patients’ lifestyle were positive (few were neutral, none were negative). The majority of physicians indicated that the ability to adjust oxybate dosing was important or very important (88%; Figure 5) and had a positive impact on providing care (88%; Figure 6). Most physicians (80%) perceived that the dosing regimen adjustments they recommended were effective in addressing the specific patient situation.
 |
Figure 5 Importance of the ability to adjust oxybate dosing to accommodate occasional changes in a patient’s typical routine. 5 = very important; 1 = not at all important. |
 |
Figure 6 Impact of the ability to vary oxybate dosing regimen on the ability to provide care for your patients. |
Guidance Provided by Physicians for Representative Patient Vignettes
Table 1 describes the 4 representative patient vignettes that were presented and the summarized recommendations that were provided by the participating physicians via the audio response system. Overall, the physicians employed a collaborative approach with patients in tailoring their oxybate dosing regimens to meet the patients’ needs. In many instances, physicians provided multiple options for the patient to consider; in particular, recommendations were made to change the amount, timing, and/or number of doses to fit the needs of the patient in each vignette. Qualitative assessment of the physicians’ voice responses revealed that the physicians often responded “in role” (ie, they addressed the patient directly using the name provided in the vignette) and employed a shared rather than directive approach, encouraging patient participation in treatment decision-making and offering different suggestions with a “try and see” approach to arrive at a solution that might work best for each particular situation.
Discussion
This is the first study of its kind (to our knowledge) to elicit physician feedback regarding clinical practice (real-world) oxybate prescribing patterns for patients with narcolepsy as well as the circumstances surrounding, and perceptions regarding, oxybate dosing individualization to accommodate the patients’ lifestyles. The results showed that 64% of physicians reported that a majority of their patients were on equally divided dosing as recommended in the SXB prescribing information,17 although some were prescribed unequal dosing. This demonstrates that physicians are able to apply the flexibility of oxybate dosing to individualize treatment to meet the needs of their patients.
Individualization of oxybate dosing has also been reported in a real-world, non-interventional surveillance study of oxybate (SXB) use in routine clinical practice in Europe (730 patients).28 Oxybate dosing generally followed the prescribing information,17,32 although some deviations were noted;28 27.1% of patients were prescribed oxybate differently from the recommended twice-nightly, equally divided regimen on at least an occasional basis. Adjustments were noted as occurring daily (7.2%), a few days per week (6.4%), or a few days per month or less (13.3%). Similarly, patients deviated from the recommended timing of taking oxybate relative to meals (2–3 hours after eating); 19.3% reported taking oxybate within 2 hours of food consumption, and reported that deviations occurred daily (4.3%), a few days per week (6.1%), or a few days per month or less (8.7%). In an analysis of the Nexus Narcolepsy Registry, 17% of patients self-reported asymmetric oxybate dosing.29 The results of the current study are broadly consistent with these findings, with a substantial number of physicians in real-world clinical practice reporting that their patients were prescribed oxybate on a regimen other than that recommended in the prescribing information. In contrast to SXB, LXB, composed of calcium, magnesium, potassium, and sodium oxybates (granted FDA approval after the present study was conducted), has a recommendation for equal or unequal dosing as part of its prescribing information.17,18 It should be noted that a fixed-dose, high-sodium oxybate (FD-SXB) formulation has also recently been approved by the FDA.33,34
Physicians in this study described their dosing-individualization interactions with patients as common and mostly patient initiated. The results indicate that physicians deal with these dosing-adjustment situations with some frequency, and that the requests for adjustment guidance are patient driven, situation dependent, and separate from the patient education/instruction on oxybate treatment that they proactively provide to the patient. Many physicians adjusted their patients’ oxybate dosing regimen to accommodate occasional changes to usual routines. The majority of physicians recommended adjusting the total nightly dose and/or the timing of the doses when providing personalized oxybate dosing guidance. The circumstances of the needed adjustments varied and included traveling, attending work/work events, caring for family members, accommodating mealtimes, romance with a bed partner, and dealing with unexpected situations. When providing recommendations to the representative patient vignettes, physicians often responded in role, provided multiple options for adjustments, and adopted a collaborative approach to individualizing oxybate regimens to meet the needs of their patients. This collaborative approach is indicative of physicians’ commitment to addressing these patient needs, which is facilitated by the flexibility afforded by SXB and LXB dosing to personalize treatment for their patients.
Physicians in this study perceived the ability to adjust oxybate dosing regimens to accommodate occasional changes in patients’ routines as important/very important and indicated that this ability has a positive impact on their capacity to provide care to their patients; no physicians had a negative impression regarding the ability to adjust dosing regimens. This has implications for positively impacting quality of care. Studies assessing the impact of individualized interventions tailored to address specific situations or treatment decisions on patient adherence, outcomes, and/or satisfaction with treatment have previously reported a benefit of individualized treatment on patient outcomes.24–26 The current results provide evidence that physicians in clinical practice are individualizing therapy by taking into consideration patients’ psychosocial circumstances and other lifestyle situations when making treatment recommendations. This in turn may facilitate patients’ adherence to their oxybate treatment and improve patient outcomes and satisfaction.
An important consideration in providing individualized dosing adjustment guidance to accommodate various patient situations is the confidence and comfort level of the treating physician who is providing this guidance. In this study, the sample included sleep physicians who were largely experienced clinicians (ie, an average of 16 years in practice) and had considerable experience treating patients with oxybate (an average of 25 patients who were prescribed oxybate). This may partially account for the high percentage of physicians who discussed dosing adjustments with patients and the types of adjustments they have recommended. The multiple options they recommended for the representative patient scenarios suggested that the physicians were fairly well versed in providing recommendations to patients on ways to adjust their oxybate dosing regimens to address different types of life situations. Sleep physicians who are new to treating patients with narcolepsy using LXB may benefit from the guidance of experienced oxybate prescribers. Due to its composition of calcium, magnesium, potassium, and sodium oxybates, LXB contains 92% less sodium content than high-sodium oxybates (SXB and FD-SXB). In June 2021, the FDA’s Office of Orphan Products Development granted Orphan Drug Exclusivity to LXB, summarizing that LXB is clinically superior to SXB by means of greater safety because LXB provides a greatly reduced sodium burden, and the differences in chronic sodium intake will be clinically meaningful in reducing cardiovascular morbidity in a substantial proportion of patients for whom the drug is indicated.35 The FDA recognizes that FD-SXB33 contains the same amount of sodium as SXB;17 therefore, the difference in the sodium content between LXB18 and FD-SXB is likely to be clinically meaningful in all patients with narcolepsy. Head-to-head trials between LXB and SXB or FD-SXB were not conducted.
Limitations of the study include the cross-sectional design, which precluded collection of data on specific patient circumstances and the context in which dosing adjustment guidance occurred for each situation. The use of representative patient vignettes to collect data on physician recommendations regarding dosing adjustment was appropriate within the context of a cross-sectional study design. While this evaluation yielded important insights into how physicians frame the guidance they provide, it is based on representative rather than actual patient situations, and it is possible that physicians may respond differently to a representative patient vignette compared with a real-life situation. Information regarding the impact of adjustments on narcolepsy symptoms was not collected, as the survey focused on physician prescribing practices and not clinical response or effectiveness. Finally, the study sample of 25 US-based physicians may limit the generalizability of these findings to a larger physician population, particularly in international settings.
Conclusion
In summary, the results of this cross-sectional study provide a valuable overview of real-world oxybate physician prescribing patterns and the frequency and circumstances for providing dose adjustment guidance. Further investigation is needed to improve the individualized dosing guidance that physicians provide, in their clinical practice, to patients, and more mentorship would be helpful for physicians newly treating patients with oxybate. Additionally, future studies evaluating similar prescribing practices in pediatric patients may be worthwhile.
Abbreviations
BMI, body mass index; EDS, excessive daytime sleepiness; FDA, Food and Drug Administration; FD-SXB, fixed-dose, high-sodium oxybate; LXB, low-sodium oxybate (calcium, magnesium, potassium, and sodium oxybates); SD, standard deviation; SXB, sodium oxybate; US, United States.
Data Sharing Statement
All relevant data are provided within the article. Jazz has established a process to review requests from qualified external researchers for data from Jazz-sponsored clinical trials in a responsible manner that includes protecting patient privacy, assurance of data security and integrity, and furthering scientific and medical innovation. Additional details on Jazz Pharmaceuticals data sharing criteria and process for requesting access can be found at: https://www.jazzpharma.com/science/clinical-trial-data-sharing/.
Ethics Approval and Informed Consent
Centralized institutional review board approval for this study was obtained by the New England Independent Review Board (Needham, MA). All participants provided electronic informed consent to participate in the study. Participants received an honorarium for their participation in this study.
Acknowledgments
The authors would like to thank the physicians for their participation in this study. The authors also gratefully acknowledge the contributions of Diane Menno of Jazz Pharmaceuticals for her review and approval of the statistical analysis plan and assistance in interpretation of the results, as well as Jessica Vu, Jeremy Franz, Beth Baldys, and Fabio Gratton from inVibe for their work in recruitment and execution of the study and their assistance in analyzing the qualitative data from the study. Under the direction of the authors, Sean Anderson, PhD, and Michael Theisen, PhD, of Peloton Advantage, LLC, an OPEN Health company, provided medical writing and editorial support, which was funded by Jazz Pharmaceuticals.
Author Contributions
All authors have substantially revised or critically reviewed the article; have agreed on the journal to which the article will be submitted; reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage; and agreed to take responsibility and be accountable for the contents of the article.
A Roy: Conceptualization (equal); Methodology (equal); Investigation (equal); Writing – review and editing (equal).
D Ito: Conceptualization (equal); Methodology (equal); Formal analysis (equal); Investigation (equal); Writing – review and editing (equal).
S Morris: Conceptualization (equal); Methodology (equal); Investigation (equal); Writing – review and editing (equal).
S Candler: Writing – review and editing (equal).
J Profant: Conceptualization (equal); Methodology (equal); Formal analysis (equal); Investigation (equal); Writing – review and editing (equal).
C Bae: Conceptualization (equal); Methodology (equal); Investigation (equal); Writing – review and editing (equal).
Funding
This study was sponsored by Jazz Pharmaceuticals.
Disclosure
AR has received consultancy fees from Jazz Pharmaceuticals and Harmony Biosciences. DI is an employee of Stratevi, a consulting firm that has received research funding from Jazz Pharmaceuticals to conduct this study. SM and JP are former employees of Jazz Pharmaceuticals who, in the course of their employment, received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals plc. SC is a current employee of Jazz Pharmaceuticals who, in the course of his employment, has received stock options exercisable for, and other stock awards of, ordinary shares of Jazz Pharmaceuticals plc. CB has received consultancy fees from Jazz Pharmaceuticals. The authors report no other conflicts of interest in this work.
References
1. Thorpy MJ, Dauvilliers Y. Clinical and practical considerations in the pharmacologic management of narcolepsy. Sleep Med. 2015;16(1):9–18. doi:10.1016/j.sleep.2014.10.002
2. Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007;369(9560):499–511. doi:10.1016/S0140-6736(07)60237-2
3. Thorpy MJ, Hiller G. The medical and economic burden of narcolepsy: implications for managed care. Am Health Drug Benefits. 2017;10(5):233–241.
4. Narcolepsy fact sheet; 2017. Available from: https://catalog.ninds.nih.gov/pubstatic/17-1637/17-1637.pdf.
5. Morgenthaler TI, Kapur VK, Brown T, et al. Practice parameters for the treatment of narcolepsy and other hypersomnias of central origin. Sleep. 2007;30(12):1705–1711. doi:10.1093/sleep/30.12.1705
6. Maski K, Trotti LM, Kotagal S, et al. Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(9):1881–1893. doi:10.5664/jcsm.9328
7. Mignot EJ. A practical guide to the therapy of narcolepsy and hypersomnia syndromes. Neurotherapeutics. 2012;9(4):739–752. doi:10.1007/s13311-012-0150-9
8. Bassetti CLA, Kallweit U, Vignatelli L, et al. European guideline and expert statements on the management of narcolepsy in adults and children. J Sleep Res. 2021;30:e13387. doi:10.1111/jsr.13387
9. Turner K, Zambrelli E, Lavolpe S, Baldi C, Furia F, Canevini MP. Obstructive sleep apnea: neurocognitive and behavioral functions before and after treatment. Funct Neurol. 2019;34(2):71–78.
10. Pellitteri G, de Biase S, Valente M, Gigli GL. How treatable is narcolepsy with current pharmacotherapy and what does the future hold? Expert Opin Pharmacother. 2021;22(12):1517–1520. doi:10.1080/14656566.2021.1915987
11. Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006;29(7):939–946. doi:10.1093/sleep/29.7.939
12. Plazzi G, Ruoff C, Lecendreux M, et al. Treatment of paediatric narcolepsy with sodium oxybate: a double-blind, placebo-controlled, randomised-withdrawal multicentre study and open-label investigation. Lancet Child Adolesc Health. 2018;2(7):483–494. doi:10.1016/S2352-4642(18)30133-0
13. U.S. Xyrem Multicenter Study Group. A randomized, double blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25(1):42–49.
14. U.S. Xyrem Multicenter Study Group. Sodium oxybate demonstrates long-term efficacy for the treatment of cataplexy in patients with narcolepsy. Sleep Med. 2004;5(2):119–123. doi:10.1016/j.sleep.2003.11.002
15. Xyrem International Study Group. A double-blind, placebo-controlled study demonstrates sodium oxybate is effective for the treatment of excessive daytime sleepiness in narcolepsy. J Clin Sleep Med. 2005;1(4):391–397. doi:10.5664/jcsm.26368
16. Bogan RK, Thorpy MJ, Dauvilliers Y, et al. Efficacy and safety of calcium, magnesium, potassium, and sodium oxybates (lower-sodium oxybate [LXB]; JZP-258) in a placebo-controlled, double-blind, randomized withdrawal study in adults with narcolepsy with cataplexy. Sleep. 2021;44(3):zsaa206. doi:10.1093/sleep/zsaa206
17. Jazz Pharmaceuticals. Xyrem® (Sodium Oxybate) Oral Solution, CIII [Prescribing Information]. Palo Alto, CA: Jazz Pharmaceuticals, Inc.; 2023.
18. Jazz Pharmaceuticals. Xywav® (Calcium, Magnesium, Potassium, and Sodium Oxybates) Oral Solution, CIII [Prescribing Information]. Palo Alto, CA: Jazz Pharmaceuticals, Inc.; 2023.
19. Szarfman A, Kuchenberg T, Soreth J, Lajmanovich S. Declaring the sodium content of drug products. N Engl J Med. 1995;333(19):1291. doi:10.1056/NEJM199511093331917
20. US Food and Drug Administration. Quantitative labeling of sodium, potassium, and phosphorus for human over-the-counter and prescription drug products. Guidance for industry; 2022. Available from: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/quantitative-labeling-sodium-potassium-and-phosphorus-human-over-counter-and-prescription-drug.
21. US Food and Drug Administration. Clinical review for Binosto, NDA 202344; 2012. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/202344Orig1s000MedR.pdf.
22. Roth T, Dauvilliers Y, Guinta D, Alvarez-Horine S, Dynin E, Black J. Effect of sodium oxybate on disrupted nighttime sleep in patients with narcolepsy. J Sleep Res. 2017;26(4):407–414. doi:10.1111/jsr.12468
23. Schinkelshoek MS, Smolders IM, Donjacour CE, et al. Decreased body mass index during treatment with sodium oxybate in narcolepsy type 1. J Sleep Res. 2019;28(3):e12684. doi:10.1111/jsr.12684
24. Linn AJ, van Dijk L, van Weert JCM, Gebeyehu BG, van Bodegraven AA, Smit EG. Creating a synergy effect: a cluster randomized controlled trial testing the effect of a tailored multimedia intervention on patient outcomes. Patient Educ Couns. 2018;101(8):1419–1426. doi:10.1016/j.pec.2018.03.017
25. Violette PD, Agoritsas T, Alexander P, et al. Decision aids for localized prostate cancer treatment choice: systematic review and meta-analysis. CA Cancer J Clin. 2015;65(3):239–251. doi:10.3322/caac.21272
26. Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and outcomes in poorly controlled asthma. Am J Respir Crit Care Med. 2010;181(6):566–577. doi:10.1164/rccm.200906-0907OC
27. Drakatos P, Lykouras D, D’Ancona G, et al. Safety and efficacy of long-term use of sodium oxybate for narcolepsy with cataplexy in routine clinical practice. Sleep Med. 2017;35:80–84. doi:10.1016/j.sleep.2017.03.028
28. Mayer G, Plazzi G, Iranzo A, et al. Long-term compliance, safety, and tolerability of sodium oxybate treatment in patients with narcolepsy type 1: a postauthorization, noninterventional surveillance study. Sleep. 2018;41(9). doi:10.1093/sleep/zsy128
29. Ohayon MM, Thorpy MJ, Short SA, et al. Sodium oxybate dosing utilization patterns in the Nexus Narcolepsy Registry [abstract 0605]. Sleep. 2019;42(suppl 1):A241. doi:10.1093/sleep/zsz067.603
30. Peraita-Adrados R, Bellón JM, Lillo-Triguero L, López-Esteban P, Medrano-Martínez P. Long-term follow-up on the effects of sodium oxybate on daytime sleepiness and sleep architecture in patients with narcolepsy type 1. Rev Neurol. 2023;76(2):35–40. doi:10.33588/rn.7602.2022315
31. Roy A, Profant J, Morris S, et al. Sodium oxybate prescribing adjustments by physicians in a real world clinical setting [abstract]. Sleep Med. 2019;64(suppl 1):S329–S330. doi:10.1016/j.sleep.2019.11.921
32. UCB Pharma. Xyrem [Summary of Product Characteristics]. Brussels, Belgium: UCB Pharma; 2022.
33. Avadel CNS Pharmaceuticals. LumryzTM (Sodium Oxybate) for Extended-Release Oral Solution, CIII [Prescribing Information]. Chesterfield, MO: Avadel CNS Pharmaceuticals; 2023.
34. Avadel Pharmaceuticals Announces Final FDA Approval of LUMRYZ™ (sodium oxybate) for Extended-Release Oral Suspension as the First and Only Once-at-Bedtime Oxybate for Cataplexy or Excessive Daytime Sleepiness in Adults with Narcolepsy [press release]; 2023. Available from: https://investors.avadel.com/news-releases/news-release-details/avadel-pharmaceuticals-announces-final-fda-approval-lumryztm.
35. Clinical superiority findings; 2021. Available from: https://www.fda.gov/industry/designating-orphan-product-drugs-and-biological-products/clinical-superiority-findings.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
