Back to Journals » Infection and Drug Resistance » Volume 16
Increased Incidence and Risk Factors of Infections by Extended-Spectrum β-Lactamase-Producing Enterobacterales During the COVID-19 Pandemic: A Retrospective Case-Control Study
Authors Geng Y, Li F , Chen C, Liu Z, Ma X, Su X, Meng H, Lu W, Wang X, Pan D, Liang P
Received 26 May 2023
Accepted for publication 7 July 2023
Published 20 July 2023 Volume 2023:16 Pages 4707—4716
DOI https://doi.org/10.2147/IDR.S421240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Yuhui Geng,1,* Furong Li,2,* Chen Chen,3 Zhuo Liu,1 Xiaojuan Ma,1 Xinya Su,1 Hua Meng,1 Wenwen Lu,1 Xingtian Wang,1 Dongfeng Pan,4 Peifeng Liang5
1School of Public Health, Ningxia Medical University, Yinchuan, People’s Republic of China; 2Department of Clinical Laboratory, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, People’s Republic of China; 3Department of Public Health, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, People’s Republic of China; 4Department of Emergency Medicine, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, People’s Republic of China; 5Department of Medical Records and Statistics, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Peifeng Liang, Department of Medical Records and Statistics, People’s Hospital of Ningxia Hui Autonomous Region, Yinchuan, People’s Republic of China, Tel +86 951 13895085519, Email [email protected]
Purpose: To investigate changes in the incidence of infections by extended-spectrum β-lactamase-producing Enterobacterales (ESBL-E) and analyzed whether there was an association between endogenous changes in the organism due to COVID-19 infection and the infections by ESBL-E.
Patients and Methods: The study was a single-center retrospective case-control design. A total of 107 patients infected by ESBL-E during the COVID-19 pandemic were selected as the case group, while 214 uninfected patients selected by 1:2 propensity score matching (PSM) acted as the control group. Univariate analysis, LASSO logistic regression, and multivariate logistic regression were used to determine the risk factors for ESBL-E infection. An interrupted time series was used to analyze the changes in the incidence of ESBL-E infections in hospitalized patients during the COVID-19 pandemic.
Results: The incidence of infection with ESBL-E showed a significant increase during COVID-19 (3.42 vs 4.92 per 1000 patients, p = 0.003). The incidence of ESBL-E infections increased at an average rate of 0.45 per 1000 patients per week compared to the pre-pandemic period (p = 0.022). Multivariate logistic regression analysis showed that a length of hospitalization ≥ 15 days (OR: 2.98 (1.07– 8.28), chronic kidney disease (OR: 4.25 (1.32– 13.70), white blood cell (WBC) > 9.5× 10^9/L (OR: 3.04 (1.54– 6.01), use of hormonal drugs (OR: 2.38 (1.04– 5.43), antibacterial drug use 1 type (OR: 5.38 (2.04– 14.21), antibacterial drug use 2 types (OR: 23.05 (6.71– 79.25) and antibacterial drug use ≥ 3 types (OR: 88.35 (8.55– 912.63) were independent risk factors for infection with ESBL-E, while chronic obstructive pulmonary disease (COPD) was a protective factor (OR: 0.14 (0.03– 0.66). COVID-19 was not an independent risk factor for infection by ESBL-E.
Conclusion: During the COVID-19 pandemic, the incidence of infections by ESBL-E increased significantly. Increased exposure to traditional risk factors were the main reasons, however, COVID-19 was not an independent risk factor for ESBL-E infection.
Keywords: β-lactamases, COVID-19, risk factor, antibacterial drugs, case-control study, LASSO
Introduction
Extended-spectrum β-lactamases (ESBLs) are enzymes produced by certain bacteria that hydrolyze penicillins, cephalosporins, and monocyclic amides antibiotics, and are usually strongly inhibited by clavulanic acid.1,2 They are mainly found in gram-negative bacilli, of which Escherichia coli and Klebsiella pneumoniae are the most common.3,4 The prevalence of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E) is increasing worldwide and has become one of the public health issues of global concern.5 A case-control study in Canada found that ESBL-E infection was associated with longer hospital stays, increased hospital costs, and higher mortality.6
Since December 2019, cases of coronavirus disease 2019 (COVID-19) have emerged worldwide and rapidly formed a worldwide pandemic in a short period of time, posing a serious threat to public safety.7,8 During the pandemic when hospitals experienced personal protective equipment (PPE) supply challenges, staffing shortages, and extended patient stays, there may have been a shift in clinical focus of infection control to prevent respiratory transmission and a decrease in antimicrobial surveillance and stewardship.9,10 A multi-center, retrospective cohort analysis in 271 healthcare facilities in the United States showed that antibiotic multidrug resistance rates were significantly higher during the COVID-19 pandemic than before the pandemic.11 The authors also emphasized that the results of this study were limited to the United States and that further investigations were needed to determine whether or not antibiotic multidrug resistance rates had also increased in hospitalized patients in other countries during the COVID-19 pandemic. COVID-19 caused a reduction in the immunity of patients making them prone to combined or secondary bacterial and fungal infections, with some patients needing to use catheters and ventilators more frequently and for longer periods of time.12–14 These conditions also increased the risk of multidrug resistance. Therefore, it is vital to prevent, identify and monitor infections by ESBL-E, especially during the COVID-19 epidemic. There are many studies on the risk factors for ESBL-E infection. According to a published systematic review, the most commonly reported risk factors for ESBL-E colonization and infection were previous exposure to antimicrobial drugs and recent hospitalization or surgical treatment.15 However, there are few studies on risk factors for ESBL-E infection during the COVID-19 pandemic.
The purpose of this study was to investigate the changes in the incidence of ESBL-E infections and the risk factors during the COVID-19 pandemic. The study also evaluated whether endogenous changes in the organism due to COVID-19 infection are potential independent risk factors for ESBL-E infection.
Patients and Methods
Patient Selection and Data Collection
The study was a retrospective, case-control design that included patients admitted to a tertiary care general hospital in Ningxia between December 8, 2022, to February 1, 2023. Patients identified as positive for an ESBL-E infection determined by a drug sensitivity test were selected as the case group (n = 107). Non-infection patients were included as the control group (n = 214) and were selected using age and sex as matching variables with a caliper value of 0.02 and propensity score matching (PSM) according to the 1:2 nearest neighbor matching method. Inclusion criteria for all the patients were: (1) length of hospitalization > 24 h; (2) the case group included patients with positive ESBL-E confirmed by strain identification and a drug sensitivity test. Exclusion criteria: (1) presence of duplicate strains in the same patient; (2) patient previously included in the study.
Patients with a positive drug sensitivity test for ESBL-E were identified through the hospital LIS testing system, and their clinical information then extracted from the electronic medical record system according to case number. The following study indicators were identified based on previous relevant studies: general characteristics (sex, age, length of hospitalization, previous hospitalization, intensive care unit [ICU] admission, COVID-19, and nutritional status); underlying diseases (hypertension, diabetes mellitus, chronic kidney disease, chronic obstructive pulmonary disease [COPD]); comorbidities (hypoproteinemia, respiratory failure, and sepsis); invasive operations (mechanical ventilation, central venous placement, retained urinary catheter, and tracheal intubation); treatment and drug use (surgery, blood transfusion, whether antibacterial drugs were used and the length of use and type of antibacterial drugs administered, combination of antibacterial drugs, and whether hormonal drugs were used and length of use); laboratory tests (serum albumin and lactate levels, and white blood cell [WBC] count).
Antimicrobial Susceptibility Testing and Phenotypic Detection of ESBL-E
The strains were cultured and identified with reference to the National Clinical Laboratory Practice (4th edition), with the drug susceptibility test performed by the Kirby-Bauer disk diffusion method. The criteria for an ESBL-E infection included: (1) Primary screening test: Drug-sensitive disks containing cefpodoxime (10 µg) and ceftazidime (30 µg) were selected. Muller-Hinton (MHA) agar and standard disk diffusion method were used to test the diameter of the inhibition ring. A ring diameter for cefpodoxime of ≤ 17 mm and ≤ 22 mm for ceftazidime was highly suspected as indicating the presence of an ESBLs strain, with further tests needed to confirm the diagnosis. (2) Phenotype confirmation test: Ceftazidime (30 µg) and ceftazidime plus clavulanic acid (30 µg and 10 µg), and cefotaxime (30 µg) and cefotaxime plus clavulanic acid (30 µg and 10 µg) were used to measure the diameter of the inhibition rings of the two disks either alone or with clavulanic acid. Any group with clavulanic acid was considered to be infected with ESBL-E if the increase in inhibition diameter was ≥ 5 mm compared to that measured without clavulanic acid.
COVID-19 Definition
According to the diagnostic criteria of the Novel Coronavirus Pneumonia Treatment Protocol (Trial Version 9)16 developed by the National Health Commission, a suspected case with one of the following pathogenic or serological findings can be diagnosed as a confirmed case of COVID-19: (1) Positive nucleic acid test for a novel coronavirus; (2) Novel coronavirus-specific IgM and IgG antibodies positivity in patients who had not received the novel coronavirus vaccine.
Statistical Analysis
The raw data were entered and collated using Microsoft Excel (Office 2021) software. The continuous variables were expressed as median (M) and quartile interval (P25, P75), while the categorical variables were expressed as frequency (n) and percentage (%). Univariate and multivariate logistic regression analyses were performed using SPSS 26.0. The Mann–Whitney U-test was used to test for differences between continuous variables, while the chi-square test was used for comparison of categorical variables. Significant independent variables were screened using the LASSO logistic regression model, with the screened independent variables then included in a multivariate logistic regression model for analysis. An interrupted time series was used to analyze the changes in the incidence of ESBL-E infections in hospitalized patients during the COVID-19 pandemic. R software version 4.2.2 and the “glint” package were used for the LASSO regression analysis. Interrupted time series analysis was performed using stataMP17 analysis. A p value < 0.05 was considered statistically significant.
Results
Sociodemographic and Clinical Characteristics of Study Participants
A total of 321 hospitalized patients during the COVID-19 pandemic (December 8, 2022 to February 1, 2023) were included as subjects in this study. The case group included 52 males (48.6%) and 55 females (51.4%) and the control group included 103 males (48.13%) and 111 females (51.87%). There was no significant difference in the sex ratio between the two groups (p = 0.937). The median age of both the case and control groups was 67 years, and the difference was not statistically significant (p = 0.983) (Table 1). During the COVID-19 pandemic, ESBL-E infections were mainly Escherichia coli and Klebsiella pneumoniae, with a detection rate of 53.13% (85/160) and 11.40% (20/194), respectively.
 |
Table 1 Univariate Analysis of Risk Factors for Extended-Spectrum β-Lactamase Producing Enterobacterales (ESBL-E), n (%) |
Incidence of Infections by ESBL-E Before and During COVID-19
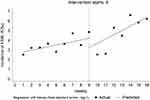
A total of 38,325 patients were hospitalized before the pandemic (December 8, 2021 to February 1, 2022), of which 131 patients with ESBL-E infection were detected. During the COVID-19 pandemic (December 8, 2022 to February 1, 2023) 27,865 patients were hospitalized, of which 137 patients with ESBL-E infection were detected. Although the number of hospitalized patients decreased during the pandemic, the incidence of ESBL-E infections increased significantly (3.42 vs 4.92 per 1000 patients, p = 0.003). Interrupted time series analysis showed that the incidence of ESBL-E infection increased at an average rate of 0.18 per 1000 patients per week before the pandemic (p = 0.015). The incidence of ESBL-E infection showed a decrease immediately after the start of the pandemic (0.96 per 1000 patients, p = 0.936) and then increased at a rate of 0.45 per 1000 patients weekly (p = 0.022) (Figure 1).
Factors Associated with Infections by ESBL-E
In Table 1, possible risk factors associated with ESBL-E infection are listed, including general characteristics, underlying diseases, comorbidities, laboratory indicators, invasive operations, and treatment and drug use. The results of univariate analysis showed that the age and sex of the case group and the control group were balanced and comparable (p > 0.05). Differences between the two groups were observed for the length of hospitalization (41.1% vs 5.1%, p < 0.001), ICU admission (19.6% vs 6.5%, p < 0.001), COVID-19 (57.0% vs 41.1%, p = 0.007), nutritional status (26.2% vs 12.1%, p = 0.002), diabetes mellitus (28.0% vs 17.3%, p = 0.026), chronic kidney disease (12.1% vs 3.7%, p = 0.004), sepsis (10.3% vs 1.9%, p = 0.001), respiratory failure (23.4% vs 7.9%, p < 0.001), hypoproteinemia (45.8% vs 17.8%, p < 0.001), albumin < 40 g/L (88.8% vs 79.4%, p = 0.038), and WBC > 9.5×10^9/L (47.7% vs 22.0%, p < 0.001). Some patients received invasive operations such as mechanical ventilation and central venous line placement, and the differences between the two groups compared were statistically significant (p < 0.001). In addition, differences between two groups were reported for blood transfusion (18.7% vs 7.0%, p = 0.002), use of antimicrobial drugs (94.4% vs 46.7%, p < 0.001), length of antimicrobial drug use ≥ 7 days (62.6% vs 10.7%, p < 0.001), antibacterial drug combination ≥ 2 (31.8% vs 5.6%, p < 0.001), ≥ 3 types of antibacterial drugs (24.3% vs 0.5%, p < 0.001), use of hormonal drugs (40.2% vs 10.7%, p < 0.001), and length of hormonal drug use ≥ 7 days (11.2% vs 2.3%, p = 0.001) (Table 1).
We used a LASSO logistic regression model to construct the risk factor selector (Figure 2a). The number of corresponding variables screened out by the model is shown in Figure 2b. After the LASSO regression model analysis, 13 variables with non-zero coefficients were screened at a lambda.min of 0.021, including length of hospitalization, diabetes mellitus, COPD, chronic kidney disease, hypoproteinemia, serum lactate level > 2.2 mmol/L, WBC > 9.5×10^9/L, blood transfusion, surgery, length of antimicrobial drug use, antibacterial drug combination, types of antibacterial drugs, and use of hormonal drugs (Figure 2b).
Multivariate logistic regression analysis was performed with the infection status of ESBL-E as the dependent variable, COVID-19 as the reference variable, and the variables screened by LASSO regression as the independent variables. The independent variables were included step-wise in the multivariate logistic regression model to determine whether COVID-19 was an independent risk factor for ESBL-E infections. The results showed that the difference caused by COVID-19 in the model was not statistically significant (p > 0.05). Multi-variate analysis showed that a length of hospitalization ≥ 15 days (OR: 2.98; 95% CI: 1.07–8.28), COPD (OR: 0.14; 95% CI: 0.03–0.66), chronic kidney disease (OR: 4.25; 95% CI: 1.32–13.70), WBC > 9.5×10^9/L (OR: 3.04; 95% CI: 1.54–6.01), use of hormonal drugs (OR: 2.38; 95% CI: 1.04–5.43), use of one type of antibacterial drug (OR: 5.38; 95% CI: 2.04–14.21), use of two types of antibacterial drugs (OR: 23.05; 95% CI: 6.71–79.25) and ≥ 3 types of antibacterial drugs (OR: 88.35; 95% CI: 8.55–912.63) were independently associated with the development of an ESBL-E infection (Table 2).
 |
Table 2 Multivariate Logistic Regression Analysis of Risk Factors for Extended-Spectrum β-Lactamase Producing Enterobacterales (ESBL-E), OR (95% CI) |
Discussion
Antimicrobial resistance has become one of the major public health problems and is a global public health crisis.17,18 ESBL-E is an important pathogen causing nosocomial infections. On the one hand, there is the rapid spread and dissemination of drug-resistant mechanisms, and on the other hand, there is the unwise overuse of antimicrobial agents and inadequate infection control measures, especially in healthcare settings.19,20
This study showed that the incidence of ESBL-E infection during the COVID-19 pandemic showed a significant increase compared to that observed in the pre-pandemic period (p = 0.003), and a significantly higher rate of increase (0.18 vs 0.45 per 1000 patients weekly). A review by Chih-Cheng Lai et al21 in 2021 indicated a rapid increase in the incidence of ESBL Klebsiella pneumoniae infection during the COVID-19 period, a finding similar to that of our study. A gradual increase in the incidence of ESBL-E infections was reported before the emergence of COVID-19, with the increase during the COVID-19 pandemic possibly being a continuation of the pre-pandemic growth trend.22,23 Alternatively, this increase may also be attributable to increased exposure to risk factors for ESBL-E infections during the COVID-19 pandemic, such as increased antimicrobial drug use and longer hospital stays.21 According to previous reports, 62% of COVID-19 patients received antimicrobial therapy, with antimicrobial prescriptions often for broad-spectrum agents.24 Therefore, inappropriate use of antimicrobial drugs may also have contributed to the increased incidence of ESBL-E infections during the COVID-19 epidemic.25
Using multivariate regression analysis, our study showed that a length of hospitalization ≥ 15 days, having chronic kidney disease, using hormonal drugs or ≥ 1 type of antibacterial drugs, and WBC > 9.5×10^9/L were independent risk factors for ESBL-E infection, whereas COPD was a protective factor. Our study found that COVID-19 is not an independent risk factor for ESBL-E infection. A systematic review published in 2022 showed that the increase in multi-drug resistant pathogens during the COVID-19 pandemic may have been due to disruptions in infection control measures and high rates of antibiotic use.26 Therefore, the increase in the incidence of ESBL-E infection during the COVID-19 pandemic may have been caused by increased exposure to traditional risk factors and not by endogenous changes in the organism due to COVID-19 infection.
In our study, the median number of days of hospitalization was 13.00 (8.00, 21.00) days for patients in the case group and 6.00 (3.00, 8.25) days for patients in the control group. The multivariate analysis showed that a length of hospitalization ≥ 15 days was a risk factor for ESBL-E infection, a result similar to the findings of Kizilates F et al.27 On the one hand, hospitals are high-risk places for cross-infection, with longer periods of hospitalization being associated with a higher risk of infection by pathogenic microorganisms. On the other hand, patients who are hospitalized for a long period of time will receive more medical operations, while patients with low immunity are more likely to be infected by pathogens. Therefore, shortening the hospitalization time of patients, reducing the loss of the body weight, and strictly implementing the requirements for aseptic operations are potentially effective measures for preventing the occurrence of hospital ESBL-E infection.
Antimicrobial drug abuse is considered a major cause of antimicrobial resistance, and limiting its use is essential to reduce the emergence and spread of resistance. During the COVID-19 pandemic, irrational use of antibiotics was also one of the risk factors for hospital-acquired ESBLs infections.28 Previous studies have reported that during the COVID-19 pandemic, prophylactic and empirical use of antimicrobial drugs was often used by physicians to combat infection.29 This reduced the incidence of infection and patient mortality, but the administration of antimicrobial drugs increased significantly. Our study showed that the use of more types of antibiotics was associated with a higher risk of ESBL infections. Although the duration of antimicrobial use was not statistically significant in our multivariate logistic regression analysis, the p value of 0.06 was very close to the critical value of statistical difference, a result which may have been due to the influence of other uncontrolled confounding factors. The prolonged use of antimicrobial drugs and the use of multiple antimicrobial drugs can lead to dysbiosis in the human body, as well as induce secondary infections by the organism. These changes provide conditions for the colonization and infection of drug-resistant bacteria. As a consequence, the rational use of antimicrobial drugs and improving supervision of antimicrobial drug administration are important measures for reducing the occurrence of multi-drug resistance in hospitals.
Our study also showed that chronic kidney disease was an independent risk factor for ESBL-E infections. Patients with chronic kidney disease were approximately 4.25 folds more likely to be infected with ESBL-E compared to other patients. The finding consistent with the those of Kiddee et al.30 This association may be due to the low autoimmune function of patients with chronic kidney disease and their frequent visits to hospitals for invasive operations such as hemodialysis. Therefore, patients with chronic kidney disease have an increased chance of being exposed to an environment contaminated with pathogenic bacteria. In addition, previous studies have demonstrated that chronic kidney disease is usually associated with Enterobacteriaceae carriage of ESBL-E.31,32 Our study found that the use of hormonal drugs was an independent risk factor for the development of ESBL-E infection in hospitalized patients. In a systematic review by Welte T et al,33 it was common for patients with COVID-19 to receive high doses of steroids during the COVID-19 pandemic. Moreover, Xu et al34 reported that the use of glucocorticoids was a risk factor for infections caused by ESBL-producing Escherichia coli, as their application could lead to low immune function and cause intestinal flora translocation. This creates favorable conditions for the development of ESBL-E infections in hospitalized patients.
Our study had some limitations. First, it was a single center study with a relatively small sample size. Second, it was a retrospective, case-control study, and although the effects of some potential confounders were controlled by subject matching and multivariate regression analysis, there is still a possibility that the effects were attributable to unknown confounders. Third, the time period of this study was relatively short and it is possible that the effects of some influencing factors may not yet have emerged, resulting in limitations of our findings. Therefore, a multicenter prospective study is required to further refine our findings.
Conclusion
In summary, the incidence of ESBL-E infections in hospitalized patients increased significantly during the COVID-19 pandemic. In addition, prolonged hospitalization, having chronic kidney disease, and irrational use of hormones and antimicrobials were independent risk factors for ESBL-E infections. Also, we found that the increased incidence of ESBL-E infection in the period of the COVID-19 pandemic was influenced by increased exposure to traditional risk factors rather than due to endogenous changes in the organism caused by COVID-19. Therefore, the control of ESBL-E infections still needs to be based on the management of risk factors and the development of programs and policies for the rational use of antimicrobial drugs.
Ethical Approval Statement
The study was performed in compliance with the Declaration of Helsinki and was approved by the Medical Ethics Committee of People’s Hospital of Ningxia Hui Autonomous Region (Approval No.:2017-008). Written informed consent was waived by the Ethics Committee of People’s Hospital of Ningxia Hui Autonomous Region as the study exclusively focused on bacteria.
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
Funding
This work was supported by the National Natural Science Foundation of China (81760608).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ghafourian S, Sadeghifard N, Soheili S, Sekawi Z. Extended spectrum beta-lactamases: definition, classification and epidemiology. Curr Issues Mol Biol. 2015;17:11–21.
2. Adler A, Katz DE, Marchaim D. The continuing plague of extended-spectrum β-lactamase producing enterbacterales infections: an update. Infect Dis Clin North Am. 2020;34(4):677–708. doi:10.1016/j.idc.2020.06.003
3. Ayari K, Bourouis A, Chihi H, Mahrouki S, Naas T, Belhadj O. Dissemination and genetic support of broad-spectrum beta-lactam-resistant Escherichia coli strain isolated from two Tunisian hospitals during 2004–2012. Afr Health Sci. 2017;17(2):346–355. doi:10.4314/ahs.v17i2.8
4. Bush K, Bradford PA. Epidemiology of β-lactamase-producing pathogens. Clin Microbiol Rev. 2020;33(2). doi:10.1128/cmr.00047-19
5. Bush K. Alarming β-lactamase-mediated resistance in multidrug-resistant Enterobacteriaceae. Curr Opin Microbiol. 2010;13(5):558–564. doi:10.1016/j.mib.2010.09.006
6. Maslikowska JA, Walker SA, Elligsen M, et al. Impact of infection with extended-spectrum β-lactamase-producing Escherichia coli or Klebsiella species on outcome and hospitalization costs. J Hosp Infect. 2016;92(1):33–41. doi:10.1016/j.jhin.2015.10.001
7. Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi:10.1016/s0140-6736(20)30260-9
8. Patel A, Jernigan DB. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak - United States, December 31, 2019-February 4, 2020. Am J Transplant. 2020;20(3):889–895. doi:10.1111/ajt.15805
9. Mazdeyasna H, Nori P, Patel P, et al. Antimicrobial stewardship at the core of COVID-19 response efforts: implications for sustaining and building programs. Curr Infect Dis Rep. 2020;22(9):23. doi:10.1007/s11908-020-00734-x
10. Furukawa D, Graber CJ. Antimicrobial stewardship in a pandemic: picking up the pieces. Clin Infect Dis. 2021;72(10):e542–e544. doi:10.1093/cid/ciaa1273
11. Bauer KA, Puzniak LA, Yu KC, et al. A multicenter comparison of prevalence and predictors of antimicrobial resistance in hospitalized patients before and during the severe acute respiratory syndrome coronavirus 2 pandemic. Open Forum Infect Dis. 2022;9(11):ofac537. doi:10.1093/ofid/ofac537
12. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi:10.1016/s0140-6736(20)30211-7
13. Donà D, Di Chiara C, Sharland M. Multi-drug-resistant infections in the COVID-19 era: a framework for considering the potential impact. J Hosp Infect. 2020;106(1):198–199. doi:10.1016/j.jhin.2020.05.020
14. Phua J, Weng L, Ling L, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8(5):506–517. doi:10.1016/s2213-2600(20)30161-2
15. Biehl LM, Schmidt-Hieber M, Liss B, Cornely OA, Vehreschild MJGT. Colonization and infection with extended spectrum beta-lactamase producing Enterobacteriaceae in high-risk patients – review of the literature from a clinical perspective. Crit Rev Microbiol. 2016;42(1):1–16. doi:10.3109/1040841x.2013.875515
16. New coronavirus pneumonial prevention and control program (9th ed). In Chinese. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202203/b74ade1ba4494583805a3d2e40093d88.shtml.
17. Knight GM, Glover RE, McQuaid CF, et al. Antimicrobial resistance and COVID-19: intersections and implications. Elife. 2021;10. doi:10.7554/eLife.64139
18. Ansari S, Hays JP, Kemp A, et al. The potential impact of the COVID-19 pandemic on global antimicrobial and biocide resistance: an AMR Insights global perspective. JAC Antimicrob Resist. 2021;3(2):dlab038. doi:10.1093/jacamr/dlab038
19. Singh SR, Teo AKJ, Prem K, et al. Epidemiology of extended-spectrum beta-lactamase and carbapenemase-producing enterobacterales in the greater Mekong subregion: a systematic-review and meta-analysis of risk factors associated with extended-spectrum beta-lactamase and carbapenemase isolation. Front Microbiol. 2021;12:695027. doi:10.3389/fmicb.2021.695027
20. Sheu -C-C, Lin S-Y, Chang Y-T, Lee C-Y, Chen Y-H, Hsueh P-R. Management of infections caused by extended-spectrum β–lactamase-producing Enterobacteriaceae: current evidence and future prospects. Expert Rev Anti Infect Ther. 2018;16(3):205–218. doi:10.1080/14787210.2018.1436966
21. Lai C-C, Chen S-Y, Ko W-C, Hsueh P-R. Increased antimicrobial resistance during the COVID-19 pandemic. Int J Antimicrob Agents. 2021;57(4):106324. doi:10.1016/j.ijantimicag.2021.106324
22. Bayraktar B, Pelit S, Bulut ME, Aktaş E. Trend in antibiotic resistance of extended-spectrum beta-lactamase-producing Escherichiacoli and Klebsiellapneumoniae bloodstream infections. Sisli Etfal Hastanesi Tip Bul. 2019;53(1):70–75. doi:10.14744/semb.2018.60352
23. Martischang R, François P, Cherkaoui A, et al. Epidemiology of ESBL-producing Escherichia coli from repeated prevalence studies over 11 years in a long-term-care facility. Antimicrob Resist Infect Control. 2021;10(1):148. doi:10.1186/s13756-021-01013-7
24. Abu-Rub LI, Abdelrahman HA, Johar A-RA, Alhussain HA, Hadi HA, Eltai NO. Antibiotics prescribing in intensive care settings during the COVID-19 era: a systematic review. Antibiotics. 2021;10(8). doi:10.3390/antibiotics10080935
25. Darwish RM, Matar SG, Snaineh AAA, et al. Impact of antimicrobial stewardship on antibiogram, consumption and incidence of multi drug resistance. BMC Infect Dis. 2022;22(1):916. doi:10.1186/s12879-022-07906-1
26. Abubakar U, Al-Anazi M, Alanazi Z, Rodríguez-Baño J. Impact of COVID-19 pandemic on multidrug resistant gram positive and gram-negative pathogens: a systematic review. J Infect Public Health. 2023;16(3):320–331. doi:10.1016/j.jiph.2022.12.022
27. Kizilates F, Yakupogullari Y, Berk H, Oztoprak N, Otlu B. Risk factors for fecal carriage of extended-spectrum beta-lactamase-producing and carbapenem-resistant Escherichia coli and Klebsiella pneumoniae strains among patients at hospital admission. Am J Infect Control. 2021;49(3):333–339. doi:10.1016/j.ajic.2020.07.035
28. Langford BJ, So M, Raybardhan S, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–531. doi:10.1016/j.cmi.2020.12.018
29. Shbaklo N, Corcione S, Vicentini C, et al. An observational study of MDR hospital-acquired infections and antibiotic use during COVID-19 pandemic: a call for antimicrobial stewardship programs. Antibiotics. 2022;11(5). doi:10.3390/antibiotics11050695
30. Kiddee A, Assawatheptawee K, Na-Udom A, et al. Risk factors for extended-spectrum β-lactamase-producing Enterobacteriaceae carriage in patients admitted to intensive care unit in a tertiary care hospital in Thailand. Microb Drug Resist. 2019;25(8):1182–1190. doi:10.1089/mdr.2018.0318
31. Razazi K, Derde LP, Verachten M, Legrand P, Lesprit P, Brun-Buisson C. Clinical impact and risk factors for colonization with extended-spectrum β-lactamase-producing bacteria in the intensive care unit. Intensive Care Med. 2012;38(11):1769–1778. doi:10.1007/s00134-012-2675-0
32. Armand-Lefèvre L, Angebault C, Barbier F, et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013;57(3):1488–1495. doi:10.1128/aac.01823-12
33. Welte T, Ambrose LJ, Sibbring GC, Sheikh S, Mullerova H, Sabir I. Current evidence for COVID-19 therapies: a systematic literature review. Eur Respir Rev. 2021;30(159). doi:10.1183/16000617.0384-2020
34. Xu M, Fan Y, Wang M, Lu X. Characteristics of extended-spectrum β-lactamases-producing Escherichiacoli in fecal samples of inpatients of Beijing Tongren Hospital. Jpn J Infect Dis. 2017;70(3):290–294. doi:10.7883/yoken.JJID.2016.023
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.