Back to Journals » International Journal of General Medicine » Volume 16
Incidence of Postoperative Sore Throat and Associated Factors Among Pediatric Patients Undergoing Surgery Under General Anesthesia at Hawassa University Comprehensive Specialized Hospital, a Prospective Cohort Study
Authors Hailu S , Shiferaw A , Regasa T, Getahun YA , Mossie A , Besha A
Received 14 November 2022
Accepted for publication 9 February 2023
Published 18 February 2023 Volume 2023:16 Pages 589—598
DOI https://doi.org/10.2147/IJGM.S397519
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Woon-Man Kung
Seyoum Hailu,1 Adanech Shiferaw,2 Teshome Regasa,1 Yayeh Adamu Getahun,1 Addisu Mossie,2 Aschalew Besha2
1Department of Anesthesiology, Dilla University, Dilla, Ethiopia; 2Department of Anesthesia at Hawassa University, Hawassa, Ethiopia
Correspondence: Seyoum Hailu, Email [email protected]
Background: Postoperative sore throat is one of the common postoperative complications following general anesthesia. Postoperative sore throat causes decreased patient satisfaction, and it affects patients’ well-being after surgery, thus identifying its incidence and predictors helps to distinguish the preventable causes of postoperative sore throat. This study aimed to assess the incidence and associated factors of postoperative sore throat among pediatric patients undergoing surgery under general anesthesia at Hawassa university comprehensive specialized hospital.
Methods: A prospective cohort study was conducted among children in the age range 6– 16 years old who underwent emergency and elective surgical procedures under general anesthesia. Data were entered and analyzed using SPSS version 26 software packages. Univariate and multivariate analyses were performed to investigate the independent predictors. The presence and severity of postoperative sore throat were assessed by using a four-point categorical pain scale at the 2nd, 6th, 12th, and 24th-hour postoperative time.
Results: A total of 102 children were recruited in this study, from which 27 children (26.5%) complained of sore throat postoperatively. This study found that endotracheal intubation (P value: 0.030; AOR: 3.155; 95% CI [1.114– 8.933]) and several attempts greater than one (P value: 0.027 and AOR: 4.890; 95% CI: [1.203– 19.883]) had statistically significant association with a postoperative sore throat.
Conclusion: The overall incidence of postoperative sore throat was 26.5%. Endotracheal intubation and the number of attempts greater than one were independent factors that were significantly associated with the occurrence of postoperative sore throat in this study.
Keywords: sore throat, throat pain, pharyngeal morbidity, pediatric patients
Corrigendum for this paper has been published.
Background
Postoperative Sore throat (POST) is one of the common and minor but unpleasant postoperative complications that contribute to postoperative morbidity following general anesthesia.1 POST can be defined as a feeling of pain or discomfort in the larynx or pharynx during the postoperative time, while a sore throat is simply defined as a nonprofessional explanation of pharyngitis that may include a range of symptoms including laryngitis, tracheitis, cough, hoarseness, or dysphagia.2 POST in children is one of the serious problems that need to be explained to the kids and their caregivers or parents before surgery.3
Postoperative sore throat has a complex etiology. POST may result from airway instrumentation, such as laryngoscopy, intubation, and suctioning, as well as their irritating effect that cause airway edema, tracheal perforation, desquamation of the airway mucosa, nerve injury (lingual, hypoglossal, or recurrent laryngeal) and increased mucosal pressure.2–4 The increased pharyngeal mucosal pressure caused by airway instrumentation may result in progressively reduced pharyngeal mucosal perfusion and mucosal ischemia; which accounts for the occurrence of sore throat.5
The degree of injury sustained during laryngoscopy, the type of endotracheal tube used, and the extent of oropharyngeal suctioning all increase the risk of postoperative sore throat.4 In contrast to LMA, POST is more common after ETT and younger age, female sex, the use of a double-lumen tube, high ETT cuff pressures, prolonged duration of anesthesia, and the presence of a blood-stained laryngoscope or tracheal tube on extubation are risk factors that increase the incidence of POST in adults undergoing GA (general anesthesia) with ETT.3 The majority of POST symptoms go away on their own, however moderate to severe postoperative sore throat pain and dysphagia may be treated with a gargle containing local anesthetics, dexamethasone, and analgesics such as benzydamine hydrochloride.6–9
The incidence of POST in children is varied from study to study, with a range of 3.3% to 50.7% in studies performed in developed countries.10,11 A study done in England in 2019 found the incidence of POST was 36.5% among pediatrics undergoing surgery under general anesthesia.11 Children have a high risk of developing POST since they have relatively smaller airways and lower mucosal perfusion pressure compared to adults, the likelihood of mucosal hypo perfusion and subsequent edema caused by airway instrumentation and cuff hyperinflation would be exaggerated in children.12
A postoperative sore throat will result in delayed oral intake, and patient dissatisfaction, and it affects patients’ well-being after surgery during the immediate postoperative period.11,13 One study shows that 30% of pediatric patients reporting a sore throat had delayed oral intake due to difficulty in swallowing, with no statistical difference between ETT and LMA use.11 The delayed oral intake on the other hand will result in dehydration and can progress to delayed wound healing and increased hospital stay and increased cost.14
Despite the clinical consequences of POST, evidence is scarce regarding the incidence and contributing factors of postoperative sore throat in children in developing countries where the resource is scarce, including Ethiopia as far as our search covers. Although most studies have been performed in developed countries, still studies in developing countries are needed as racial differences may contribute to the occurrence of some postoperative complications.15,16 Conducting this study will help to recognize the preventable causes of POST and to look forward to preventive strategies by generating awareness among health professionals or anesthetists giving care to these patients. It will also help to provide input for future researchers. This study aims to assess the incidence and associated factors of postoperative sore throat among pediatric patients undergoing surgery under general anesthesia at Hawassa university comprehensive specialized hospital.
Methodology
A single-arm prospective cohort study was conducted from February 2022 to June 2022 at Hawassa university’s comprehensive and specialized hospital, that located 273 km south of Addis Ababa city.17 After a Support letter and ethical clearance were obtained from the institutional review board (IRB) of Dilla University College of medicine and health science, which is a sponsoring university, with Protocol Unique No: duirb/055/22-02, all pediatric patients with ASA I and II physical status and age range between 6 and 16 years old that undergone both emergency and elective surgeries under general anesthesia during the study period were included. Informed assent of the children and informed consent from the family was taken to collect the data. Those patients with any history of upper respiratory tract infection (URTI), surgical procedures involving airway packing, children who cannot self-report their pain (children with a learning difficulty), and patients with a congenital anomaly in the airway were excluded from the study. This study has been presented in line with the STROCSS 2021 guideline18 and registered according to the Declaration of Helsinki 2013.19 The study was also registered on the research registry and has got a unique identifying number of the researchregistry8483 https://www.researchregistry.com/browse-the-registry#home/.
Sample Size and Sampling Technique
The sample size was calculated by using the single population proportion formula, taking a confidence interval of 95% and a margin of error of 0.05, since we were not sure regarding the presence of a comparable study; we take proportion as 50% and the sample size became n = 384. Our situational analysis from the logbook shows an estimated total number of 123 pediatric patients with an age range of 6–16 were undergone surgery under GA at HUCSH for the last three months. Accordingly, the population is estimated to be less than 10,000; by applying a correction formula, the sample size was n = 93. After adding a 10% non-response rate, the final sample size was n = 102 patients. The selection of study participants was carried out at HUCSH by using a consecutive sampling method by which all pediatric patients that undergone surgeries and fulfilled inclusion criteria were included.
Data Collection
Data were collected by structured questionnaires from parents and children who had undergone surgery under general anesthesia. The information regarding the study was explained to both study participants and their parents before surgery. Information about the study’s benefit, harm, and objective of the study prepared in English and translated into Amharic was explained to the study participants and their parents. Two trained data collectors and one supervisor were involved in the data collection process.
Preoperatively pre-anesthetic evaluation information regarding any history of URTI, type of surgery, investigations, history of POST, and any pertinent physical examination were recorded. Written informed consent was obtained just before anesthesia from the study participant’s family. Intraoperatively airway technique used, type of airway material used, number of attempts, any difficulty during airway instrumentation, and any bleeding on airway equipment on extubation were recorded. Any intraoperative airway incidents such as accidental extubation and reintubation were recorded. Postoperatively duration of surgery and anesthesia, any incident during extubation such as coughing, laryngospasm, vomiting, and stridor were recorded. After the patient was discharged from Operation Theater; the presence or absence of POST was assessed by the data collector with yes or no questions. Children who documented suffering from a sore throat at any point since waking up went on to complete a more detailed questionnaire regarding the severity of POST. The severity of postoperative sore throat was assessed by a four-point categorical pain scale, where 0 = for no sore throat; 1 = mild (complains of sore throat only after asking); 2 = moderate (complains of sore throat on his/her own); 3 = severe (change of voice associated with throat pain).10,20,21
Data Quality Assurance
To assure the quality of data, training on the objectives and relevance of the study and brief orientations were provided for data collectors. A pre-test of the data collection tool (questionnaire) was tested on 5% of patients who were not included in the main study during data collection. During data collection, each questionnaire was revised by the investigator for being complete and appropriate. Incomplete data won't be entered, data clean-up and cross-checking were done before analysis by SPSS.
Data Analysis and Interpretation
Statistical analyses were performed using SPSS version 26 software packages. The normality of the continuous variable was tested by using Shapiro–Wilk test. Non-normally distributed data were described in terms of medians and interquartile range. Data were summarized and presented in terms of frequency tables and graphs. The possible associated factors for POST were assessed using bivariate and multivariate analysis using logistic regression. Multivariate analysis was performed for those variables with a P-value <0.25 in bivariate analysis to identify strong predictors of POST. A p-value less than 0.05 were considered statistically significant.
Operational Definition
Postoperative sore throat: any pain or discomfort in the throat in the postoperative period or score ≥1.
Pediatrics: children with an age range of 6–16 were used because self-reporting pain is more reliable in ages greater than 4.22
Four-point categorical pain scale: is a categorical pain assessment tool graded as 0 for no pain, 1 for mild pain, 2 for moderate, and 3 for severe pain.
Result
Demographic and Perioperative Characteristics Distribution
A total of 102 patients were included in this study, of which 68 patients were male. The median weight of the patients included in the study was 24.5%, and the median age was 8. The majority of the procedures were ophthalmologic surgeries (Figure 1).
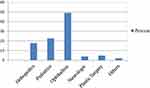 |
Figure 1 Frequency distribution of type of surgical procedures among pediatric surgical patients operated under general anesthesia in HUCSH, Hawassa, Ethiopia from February–June 2022. |
According to ASA classification, the majority of the patients were ASA class I (95.1%) and OPV (Mallampati) I (68.6%). Most of the patients had ETT and no use of oral or nasal airway and face mask anesthesia was reported. Cricoid pressure was applied in 21 patients (20.6%), and introducers (stylet and bogie) were used in 24.5% of sampled patients. Water-soluble lubricant jelly (KY jelly) was used in all patients that had undergone surgery using LMA. Lidocaine spray or injection was not used in any of the cases. The anesthetic used for induction was Propofol in half of the included patients, followed by a ketamine-Propofol combination, whereas maintenance was halothane in the majority of patients (Table 1).
 |
Table 1 Demographic and Perioperative Characteristics of Pediatric Surgical Patients Operated Under General Anesthesia in HUCSH, Hawassa, Ethiopia from February–June 2022 |
Postoperative Outcome
Postoperative sore throat occurred in 27 patients (26.5%) within the twenty-four hours postoperatively, regardless of severity scale (Figure 2).
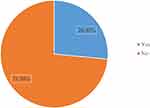 |
Figure 2 Incidence of postoperative sore throat in pediatric surgical patients operated under general anesthesia in HUCSH, Hawassa, Ethiopia from February–June 2022. |
The maximum report of postoperative sore throat was at the 6th hour postoperative time and the severe sore throat was reported only at the 6th and 12th hr (2% and 1% respectively). The majority of the complaint was mild sore throat (Figure 3). The incidence of other common postoperative complications was vomiting at 6.9%, cough at 5.9%, PH at 2.9%, and dysphagia at 4.9% was reported.
Factors Associated with a Postoperative Sore Throat
Independent variables such as gender, OPV, suctioning on extubation, cough at extubation, use of and inflation volume of LMA compared with standard manufacturer’s recommendation had no association with the occurrence of POST with a p-value greater than 0.25. The other associated factors of POST with p <0.25 were presented in Table 2.
 |
Table 2 The Factors Associated with Postoperative Sore Throat in Pediatric Surgical Patients Operated Under General Anesthesia in HUCSH, Hawassa, Ethiopia from February–June 2022 |
Endotracheal intubation and the number of attempts greater than one were statistically significant independent predictors of POST in this study with P values of 0.030 and 0.027, respectively (Table 3). Multivariate analysis omits independent variables such as blood on ETT/LMA or laryngoscope, use of introducer, duration of intubation, vomiting on extubation, dexamethasone, and cricoid pressure from associated factors of POST (p > 0.05).
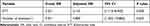 |
Table 3 The Independently Associated Factors of Postoperative Sore Throat in Pediatric Surgical Patients Operated Under General Anesthesia in HUCSH, Hawassa, Ethiopia from February–June 2022 |
Discussion
Postoperative sore throat is one of the common patient complaints that happens after airway instrumentation.3,11 In this current study, the overall incidence of POST complaints was 26.5% while endotracheal intubation and the number of attempts greater than one were the statistically significant independent predictors of POST (P = 0.03 and P = 0.027 respectively) in this study. ETT had a three times risk of developing sore throat than LMA. A study by Calder et al reported the incidence of POST after ETT was 22.6% among pediatrics undergoing surgery under general anesthesia.23 This finding is comparable with this present study.
Another prospective observational cohort study by Miskovich reported that the overall incidence of POST after both LMA and ETT was 36.5% with greater incidence in ETT compared with LMA (54.7% vs 22.5%).11 The overall incidence (both in ETT and LMA) in this current study was smaller, however, regarding ETT vs LMA patients who had ETT were significantly associated with POST (35% vs 14.3%). Dexamethasone was used in 73.5% of patients in the current study, but in a previous study by Miskovich et al, only 55.3% of patients take dexamethasone as a premedication. Dexamethasone can decrease the risk of POST24,25 and it might be the possible reason for the relatively decreased incidence of POST in this study may be due to the almost routine practice of dexamethasone premedication in this study area.
The incidence of POST in patients who had LMA was 14.3% (6/42) and it was relatively lower than in those who had ETT in this study. Patel et al found a 0% incidence of POST in the LMA group in their comparative study comparing ETT with Proseal LMA and this study reported the incidence of POST in ETT at 13.33%.26 The reported incidence in the Patel study was lower than in our current study. The sample size of their study was 60 children in the age range of 3–10 years old, the likely reason for the discrepancy of POST incidence with our study could be the difference in the sore throat assessment method they used for their age group.
The result of this study also demonstrated the number of attempts greater than one significantly increased the risk of developing POST in our findings. Repeated number of attempts had four times the risk of developing POST in this study (OR: 4.890; 95% CI: [1.203–19.883]). Although there was no inline study within the same population as ours, the cross-sectional study conducted by Gemechu et al at Gondar among adult populations found that Patients who had a repeated attempt were 3 times more likely to develop POST than patients who were intubated during the first attempt (AOR = 3.291; P = 0.003).27 The finding of this present study is in contrast with a study done by Calder et al that reported the number of intubation attempts did not associate with POST.23 This difference may be attributable to the practical difference between developed and developing countries regarding the availability of difficult intubation materials that decrease the risk of a repeated attempt. The increased risk of developing POST could be due to airway mucosal injury from repeated airway manipulation and instrumentation and the immature nature of the pediatric airway.3
This study shows no significant association between gender and the occurrence of POST. In line with this, a study done by Calder et al also found gender was not significantly associated with POST.23 However, the study done by Higgins et al reported that the female gender had more risk of developing POST (p < 0.05) than the male.28 In our current study, the number of the included female patient was not proportional to that of men (33.3% vs 66.7%), which might be one of the reasons our study contrasts with the result of Higgin’s study regarding female gender.
Endotracheal tube cuff pressure was a strong predictor of postoperative sore throat in a previous study done by Calder et al in the pediatric population with ETT intubation (p < 0.0001).23 The cuff pressure both for ETT and LMA was not monitored in our cohort since there were no routine practices and equipment for cuff pressure measurement resulting in difficulty to measure the cuff pressure. In this regard, it was not possible to know whether the cuff pressure is independently associated with factors for POST or not in our study. However, instead of cuff pressure, cuff inflation volume for LMA was measured and analyzed. When compared to the maximum inflation volume standard recommended by the manufacturer for each LMA size, the inflation volume did not associate with the occurrence of POST in this current study (p = 0.328). A study by Wong et al on the impact of LMA cuff pressure on the incidence of POST in children found that compared to LMA cuffs with lower inflation, hyperinflated LMA resulted in increased airway morbidity.12 The likely pathophysiology could be that hyper-inflated LMA causes an increase in LMA cuff pressure and if this pressure exceeds the pharyngeal wall perfusion pressure it may result in pharyngeal ischemia which is manifested by the sore throat.5
Limitations of the Study
This study has some limitations including the absence of monitoring cuff pressure which was a strong predictor of POST in previous studies; the low sample size and heterogeneity of the study were other limitations of the study. Other airway techniques such as nasal intubation and oral and nasal airway were not found in our cohort because of the coincidence and practical matter.
Conclusion
The overall incidence of Postoperative sore throat was 26.5% and the maximum reported time is at the sixth postoperative hour. Endotracheal intubation and the number of attempts greater than one were independent factors that were significantly associated with the occurrence of POST in this study.
Recommendations
Health professionals are recommended to consider the findings of this study as input to advance POST preventive strategies by reducing the aforementioned factors. Further research with large multicenter studies to determine the incidence of POST for all pediatric age groups including infants, toddlers and young children who are unable to self-report their pain should be done. For hospital policymakers, we recommend incorporating the possible preventive techniques, assessment, and treatment of sore throat as routine practice.
Abbreviations
ASA, American Society of Anesthesiologists; BMI, Body mass index; ETT, Endotracheal tube; FM, Face mask; GA, General Anesthesia; Hrs., Hours; LMA, Laryngeal mask airway; OPV, Oropharyngeal view; PACU, Post anesthesia care unit; PH, Postoperative hoarseness; POST, Postoperative sore throat; URTI, Upper respiratory tract infection; HUCSH, Hawassa university comprehensive specialized hospital.
Data Sharing Statement
All datasets used and analyzed during this study are available from the corresponding author upon reasonable request.
Ethical Approval
Support letter and ethical clearance with reference number duchm/irb/055/2022 were secured from Dilla University institutional review board. It has been registered with the unique identifying number of research registry 8483 https://www.researchregistry.com/browse-The-registry#home/.
Acknowledgments
We would like to thank Dilla University for sponsoring this research project. We would like to extend our deepest gratitude to all advisors, colleagues, and friends who supported us in this work. We would also like to express appreciation to Hawassa university’s comprehensive specialized hospital for allowing us to collect data and perform this research at their hospital.
Funding
There is no financial support from any institution to conduct this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chinachoti T, Pojai S, Sooksri N, Rungjindamai C. Risk factors of post-operative sore throat and hoarseness. J Med Assoc Thailand. 2017;100(4):463–468.
2. Scuderi PE. Postoperative sore throat: more answers than questions. Anesth Analg. 2010;111(4):831–832. doi:10.1213/ANE.0b013e3181ee85c7
3. El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anesthesia. 2016;71(6):706–717. doi:10.1111/anae.13438
4. Barash PG. Clinical Anesthesia, 8e: EBook Without Multimedia. Lippincott Williams & Wilkins; 2017.
5. Brimacombe J, Keller C, Pühringer F. Pharyngeal mucosal pressure and perfusion: a fiberoptic evaluation of the posterior pharynx in anesthetized adult patients with a modified cuffed oropharyngeal airway. J Am Soc Anesthesiol. 1999;91(6):1661.
6. McHardy F, Chung F. Postoperative sore throat: cause, prevention, and treatment. Anesthesia. 1999;54(5):444–453. doi:10.1046/j.1365-2044.1999.00780.x
7. Zuccherelli L. Postoperative upper airway problems. South African J Anaesthes Analges. 2003;9(2):12–16. doi:10.1080/22201173.2003.10873000
8. Chen C-Y, Kuo C-J, Lee Y-W, Lam F, Tam K-W. Benzydamine hydrochloride on postoperative sore throat: a meta-analysis of randomized controlled trials. Can J Anesthes. 2014;61(3):220–228. doi:10.1007/s12630-013-0080-y
9. Mostafa RH, Saleh AN, Hussein MM. A comparative study of three nebulized medications for the prevention of postoperative sore throat in the pediatric population. Open Anesthes J. 2018;12(1):85–93. doi:10.2174/2589645801812010085
10. Yhim HB, Yoon SH, Jang Y-E. Effects of benzydamine hydrochloride on postoperative sore throat after extubation in children: a randomized controlled trial. BMC Anesthesiology. 2020;20(1):77. doi:10.1186/s12871-020-00995-y
11. Miskovic A, Johnson M, Frost L, Fernandez E, Pistorio A, Disma N. A prospective observational cohort study on the incidence of postoperative sore throat in the pediatric population. Paediatr Anaesth. 2019;29(12):1179–1185. doi:10.1111/pan.13757
12. Wong JGL, Heaney M, Chambers NA, et al. Impact of laryngeal mask airway cuff pressures on the incidence of sore throat in children. Pediatr Anesthes. 2009;19(5):464–469. doi:10.1111/j.1460-9592.2009.02968.x
13. Chawaka HJ, Temesgen MH. Predictors of postoperative sore throat among surgical patients at Ethiopian teaching hospitals. J Clin Med Res. 2016;8(1):1–11. doi:10.5897/JCMR2016.0280
14. AlQahtani RM, Abdalla M, Azzam YH, Elsherif AA, Altulayhi RI. Pharmacological interventions for post-operative sore throat (POST): a network meta-analysis. Signa Vitae. 2021;17(1):169–177.
15. Pelletier SJ, Isaacs RB, Raymond DP, et al. Ethnic disparities in outcome from posttransplant infections. Shock. 2004;22(3):197–203. doi:10.1097/01.shk.0000135257.44570.39
16. Stone ML, LaPar DJ, Kane BJ, Rasmussen SK, McGahren ED, Rodgers BM. The effect of race and gender on pediatric surgical outcomes within the United States. J Pediatr Surg. 2013;48(8):1650–1656. doi:10.1016/j.jpedsurg.2013.01.043
17. Mengistu K, Geleta D. Prevalence of preoperative hypertension and its intraoperative anesthetic management among patients undergoing elective surgery at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia. Int J Med Med Sci. 2019;11(2):11–19.
18. Agha R, Mathew G. STROCSS 2021: strengthening the reporting of a cohort, cross-sectional and case-control studies in surgery. Int J Surg. 2021;96:106165. doi:10.1016/j.ijsu.2021.106165
19. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
20. Hameed M, Samad K, Ullah H. Comparison of two supraglottic airway devices on the postoperative sore throat in children: a prospective randomized controlled trial. Rev Bras Anestesiol. 2020;70:240–247.
21. Mokhtar AMM, Choy C. Postoperative sore throat in children: comparison between Proseal TM LMA and Classic TM LMA. Middle East J Anaesthesiol. 2013;22:65–70.
22. Drendel AL, Kelly BT, Ali S. Pain assessment for children: overcoming challenges and optimizing care. Pediatr Emerg Care. 2011;27(8):773–781. doi:10.1097/PEC.0b013e31822877f7
23. Calder A, Hegarty M, Erb TO, von Ungern‐Sternberg BS. Predictors of postoperative sore throat in intubated children. Pediatr Anesthes. 2012;22(3):239–243. doi:10.1111/j.1460-9592.2011.03727.x
24. Lee J, Park HP, Jeong MH, Kim HC. Combined intraoperative paracetamol and preoperative dexamethasone reduce postoperative sore throat: a prospective randomized study. J Anesth. 2017;31(6):869–877. doi:10.1007/s00540-017-2411-6
25. Zhao X, Cao X, Li Q. Dexamethasone for the prevention of postoperative sore throat: a systematic review and meta-analysis. J Clin Anesth. 2015;27(1):45–50. doi:10.1016/j.jclinane.2014.06.014
26. Patel MG, Swadia V, Bansal G. Prospective randomized comparative study of the use of PLMA and ET tube for airway management in children under general anesthesia. Indian J Anaesth. 2010;54(2):109–115. doi:10.4103/0019-5049.63643
27. Gemechu BM, Gebremedhn EG, Melkie TB. Risk factors for postoperative throat pain after general anesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, 2014. Pan Afr Med J. 2017;27. doi:10.11604/pamj.2017.27.127.10566
28. Higgins P, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anesthes. 2002;88(4):582–584. doi:10.1093/bja/88.4.582
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

