Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Incidence of Postoperative Cognitive Dysfunction Following Inhalational vs Total Intravenous General Anesthesia: A Systematic Review and Meta-Analysis
Authors Negrini D , Wu A, Oba A, Harnke B , Ciancio N, Krause M, Clavijo C, Al-Musawi M, Linhares T, Fernandez-Bustamante A, Schmidt S
Received 24 May 2022
Accepted for publication 9 July 2022
Published 15 July 2022 Volume 2022:18 Pages 1455—1467
DOI https://doi.org/10.2147/NDT.S374416
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Daniel Negrini,1,2,* Andrew Wu,1 Atsushi Oba,1,3 Ben Harnke,4 Nicholas Ciancio,1 Martin Krause,5 Claudia Clavijo,6 Mohammed Al-Musawi,7 Tatiana Linhares,1 Ana Fernandez-Bustamante,6 Sergio Schmidt8,*
1Division of Surgical Oncology, Department of Surgery, University of Colorado, Anschutz Medical Campus, Aurora, CO, USA; 2Department of Anesthesiology, Federal University of the State of Rio de Janeiro, Rio de Janeiro, RJ, Brazil; 3Department of Hepatobiliary and Pancreatic Surgery, Cancer Institute Hospital, Japanese Foundation for Cancer Research, Tokyo, Japan; 4Strauss Health Sciences Library, University of Colorado, Anschutz Medical Campus, Aurora, CO, USA; 5Department of Anesthesiology, University of California San Diego, La Jolla, CA, USA; 6Department of Anesthesiology, University of Colorado, Anschutz Medical Campus, Aurora, CO, USA; 7Department of Surgery-Division of Cardiothoracic Surgery, School of Medicine, University of Colorado, Aurora, CO, USA; 8Department of Neurology, Federal University of the State of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
*These authors contributed equally to this work
Correspondence: Sergio Schmidt, Department of Neurology, Federal University of the State of Rio de Janeiro, Rua Mariz e Barros 775, Maracanã, Rio de Janeiro, RJ, 22270-004, Brazil, Email [email protected]
Abstract: Postoperative cognitive dysfunction (POCD) has been increasingly recognized as a contributor to postoperative complications. A consensus-working group recommended that POCD should be distinguished between delayed cognitive recovery, ie, evaluations up to 30 days postoperative, and neurocognitive disorder, ie, assessments performed between 30 days and 12 months after surgery. Additionally, the choice of the anesthetic, either inhalational or total intravenous anesthesia (TIVA) and its effect on the incidence of POCD, has become a focus of research. Our primary objective was to search the literature and conduct a meta-analysis to verify whether the choice of general anesthesia may impact the incidence of POCD in the first 30 days postoperatively. As a secondary objective, a systematic review of the literature was conducted to estimate the effects of the anesthetic on POCD between 30 days and 12 months postoperative. For the primary objective, an initial review of 1913 articles yielded ten studies with a total of 3390 individuals. For the secondary objective, four studies with a total of 480 patients were selected. In the first 30 days postoperative, the odds-ratio for POCD in TIVA group was 0.46 (95% CI = 0.26– 0.81; p = 0.01), compared to the inhalational group. TIVA was associated with a lower incidence of POCD in the first 30 days postoperatively. Regarding the secondary objective, due to the small number of selected articles and its high heterogeneity, a metanalysis was not conducted. Given the heterogeneity of criteria for POCD, future prospective studies with more robust designs should be performed to fully address this question.
Keywords: postoperative cognitive dysfunction, POCD, total intravenous anesthesia, TIVA, inhalational anesthesia, postoperative complications, psychometric tests
Introduction
Postoperative cognitive dysfunction (POCD) is a common condition after surgery and anesthesia.1,2 Recent studies showed an incidence of POCD between 10% and 18%.3–7 The International Study of Post-Operative Cognitive Dysfunction (ISPOCD-1) has estimated the incidence of POCD after non-cardiac surgery is as high as 9.9% at three months.8
Regarding the choice of the type of general anesthesia, previous studies have identified a possible role of propofol in attenuating the inflammatory cascade.9,10 Moreover, an increase in various cytokines, including IL-6, TNF-α, IL-8, and IL-10, have been found to be associated with the presence of POCD.11,12 Consequentially, TIVA may be hypothesized as being protective against POCD.
A consensus-working group published recommendations from a panel of specialists suggesting that cognitive assessments on POCD should be distinguished into delayed cognitive recovery (DCR), ie, evaluations up to 30 days postoperative, and postoperative neurocognitive disorder (pNCD), ie, assessments performed between 30 days and 12 months after surgery. The consensus-working group stressed that cognitive decline after the first 30 days postoperatively might potentially be linked to long-term consequences and should, therefore, also be a topic for research.13
The primary objective of this study was to conduct a systematic review of the literature and a meta-analysis on the clinical impact of the choice of general anesthesia on the incidence of POCD-DCR, either inhalational or total intravenous anesthesia (TIVA) in the first 30 days, excluding assessments on the same day of surgery. As a secondary goal, we conducted a systematic review of the literature to study the impact of the choice of anesthetic on the incidence of POCD-pNCD between 30 days and 12 months postoperatively.
Methods
Search Strategy
The 2020 updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed when performing and reporting this study.14 A health sciences librarian (BH) conducted an initial literature search on March 6, 2020, and an updated search on May 24, 2021. The following databases were queried: Ovid MEDLINE(R); Embase.com; Web of Science, Google Scholar. Conference abstracts/papers were excluded in Embase. No other limits were applied.
All retrieved records were organized using the citation management software Endnote version 20 (Clarivate, London, U.K.). For removal of duplicates Covidence (Melbourne, Australia), a systematic review citation reviewing and screening software, was used.
The search strategy was designed to capture the association between post-operative cognitive dysfunction (POCD) with surgical anesthetics, specifically propofol and inhalational agents. The full search strategy is presented in Figure 1.
 |
Figure 1 The complete search strategy. |
Searches were supplemented by hand searching and retrieval of any additional articles meeting eligibility criteria that were cited in our reference lists.
The full protocol for this systematic review and meta-analysis is registered and approved at the PROSPERO database under the registration number CRD42021239283.
Study Selection
Only randomized controlled trials (RCT) comparing the impact on POCD between TIVA and inhalational anesthesia were selected. All papers including cardiac, carotid, or neurosurgical procedures, and non-adult patients were excluded. Studies that only assessed cognitive function on the same day of surgery were also excluded. If the title and/or abstract suggested that a paper matched the inclusion and exclusion criteria, the full article was screened and assessed for eligibility.
Primary Objective
For our primary objective, we considered POCD-DCR assessed in the first 30 days postoperatively. When assessments were performed multiple times in the postoperative period, we selected the first measurement after surgery, excluding assessments on the same day of surgery.
Secondary Objective
For our secondary aim, we focused only on papers evaluating POCD-pNCD between 30 days and 12 months postoperatively.
Methodological Quality and Risk of Bias Analysis
The methodological quality of the included studies for both objectives was assessed using the Cochrane Collaboration’s tool for assessing risk of bias in randomized trials,15 which accounts for six potential risks of bias: selection, performance, detection, attrition, reporting, and other sources of bias. Ultimately, each domain was assessed as low, high, or unclear.
Two investigators (DN and YAW) independently selected the studies, extracted the relevant information from the included trials, and assessed the risk of bias. In the case of disagreement, a third investigator (AO) resolved the conflict. Studies judged with an unknown or high risk of bias were excluded.
Outcomes
The outcome for the primary objective was the incidence of POCD-DCR, as described by the authors of the primary studies, in patients exposed to either TIVA or inhalational anesthesia in the first 30 days postoperatively. For the primary objective, we estimated the odds ratio of POCD between the two groups. For the secondary objective, the outcome was POCD – pNCD, also as defined the authors of the primary studies.
Data Synthesis and Statistical Analysis
All analyses were performed using Stata version 15.1 (StataCorp LLC, College Station, Texas, USA). The percentage of the total variability in the set of effect sizes due to true heterogeneity was tested with the I2 statistic. Random Effects Mantel-Haenszel model was used to estimate adjusted odds ratio and 95% confidence intervals for the pooled data for the primary objective.
Assessment of the Quality of Evidence
The quality of evidence was evaluated using the GRADE system, which accounts for four different levels of evidence, ie, high, moderate, low, and very low.16
Results
The flowchart for data extraction is shown in Figure 2. We identified 3381 total citations. After removal of duplicates, 1913 total unique citations were selected. After screening for eligibility criteria based on the title and/or the abstract, 17 potentially eligible articles were retrieved in full text, with 2 additional studies being further included after hand searching on our reference lists. Ten published studies were then selected for the primary objective. Four studies were selected for the secondary objective.
 |
Figure 2 PRISMA® flow chart showing article selection process. Notes: Adapted from: Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372. doi:https://doi.org/10.1136/bmj.n160.14 Copyright © 2021, BMJ Publishing Group Ltd. Creative Commons CC BY 4.0 license (https://creativecommons.org/licenses/by/4.0/legalcode). |
Primary Objective
Overall, ten RCTs compared TIVA vs inhalational anesthesia reporting the incidence of POCD-DCR in both groups (Table 1). The mean sample size among those studies was 339 subjects, considering both groups. In total, 1660 participants were assigned to the TIVA group and 1730 to inhalational anesthesia. The range of age among all the ten studies varied from 18 to 86 years, with median age of 70 years. In the TIVA group, the median age was 70.58 years (18–86) whereas in the inhalational group, the median age was 69.43 years (24–85). The pooled incidence of POCD in the TIVA group was 11.4%, while in the Inhalational group was 27.7%.
 |
Table 1 Characteristics of Included Articles in the Review and Meta-Analysis |
Nine out of the ten studies seemed to favor TIVA. Moreover, three of those nine studies reached statistical significance.7,17,18 None of the included studies favored inhalational anesthesia. The pooled OR significantly favored the use of TIVA 0.46 (95% CI = 0.26–0.81; p = 0.01) (Figure 3). Additionally, since one of the included studies contributed with nearly half of the total amount of subjects included in the pooled analysis,17 we conducted a separate analysis, excluding this study, to evaluate the overall effect measure this paper could potentially have on the pooled odds ratio. Our results indicated that we still found a significant association favoring TIVA (0.67; 95% CI = 0.51–0.87; p < 0.01), even after excluding this paper (Figure 4).
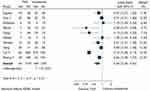 |
Figure 3 Forest plot presented OR, for each of the ten studies included for primary objective, and pooled data (TIVA vs Inhalational). |
 |
Figure 4 Forest plot presented OR, for each of the nine studies included for primary objective, excluding “Cai et al”, and pooled data (TIVA vs Inhalational). |
The Random Effects Mantel-Haenszel model was used to estimate adjusted OR and 95% confidence intervals for the pooled data based on the value of the I2 statistic, which was judged as high. We assumed a cut-off value of 75% for I2 statistic to choose between models.
Two studies used the Mini-Mental state examination (MMSE) as the only tool for evaluation.18,19 Specific tests used by different authors in their respective studies are summarized in Table 1. When more than one assessment of cognitive performance was conducted in the postoperative period, we chose the measurement closest to the day of surgery. Among studies with multiple testing in the first 30 postoperative days,6,17,18 results were similar in all assessments, apart from one study,17 in which cognitive decline was observed in inhalational group, compared to propofol, only in postoperative days one, two and three, but not in day ten. Consequently, we used data from 1st day after surgery from four studies,4,18,19 day 2 from three studies,6,7,20 day 7 from four studies3,5,21 and day 10 in a single study.22
The definition used to diagnose POCD-DCR varied a lot among those studies, ranging from a statistical difference in the means between pre- and postoperative values in MMSE, up to more sophisticated concepts, such as the Z-score or more than one SD in at least two different tests evaluating different cognitive domains, between pre- and postoperative values. Four studies used health controls not submitted to any surgery or anesthesia in the comparison.3,5,19,21 All included studies used monitoring of the level of consciousness, except for one.19
In all included studies, the type of opioids and regimen of administration were similar between groups. Most studies used sevoflurane as inhalational agent. Two studies used isoflurane,17,18 and one used desflurane.20 In most studies, usual clinical doses of inhalational agents were always used and titrated to maintain an adequate level of consciousness based on the BIS monitor. In particular, the one study that admitted in the inhalational group doses of Isoflurane ranging two to three percent, the BIS monitor was also used to titrate the adequate level of consciousness.17
The overall risk of bias in the included studies for the meta-analysis (Figure 5) was considered low in all the ten included studies. As mentioned earlier, studies assessed with an unknown or high risk of bias were excluded. Two studies were excluded during the extraction phase based on these criteria.3,23 We have also estimated the impact of the use of TIVA and POCD including those two studies, and still found an association between TIVA and a lower incidence of POCD, with OR = 0.60 (95% CI = 0.40–0.91; p = 0.02).
 |
Figure 5 Cochrane collaboration’s tool for assessing risk of bias for the included studies. |
The quality of the evidence with found based on the GRADE system,16 estimating the association between the use of TIVA and a lower incidence of POCD, was judged as moderate (Figure 6).
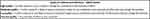 |
Figure 6 Application of the GRADE system to our findings. We believe our evidence should be classified as moderate. |
Secondary Objective
Characteristics of eligible studies for the secondary objective are shown in Table 1. From the four included articles (4–7), a total of 480 patients were included, 238 in the TIVA group, with a median age of 68.15 years (20–85), and 242 in the inhalational group, with a median age of 67.83 years (24–81). The range of age of the participants enrolled in all four studies varied from 18 to 85 years.
As previously mentioned, the type of opioids used, and the regimen of administration were similar in both groups for all included studies. All included studies for the secondary objective used sevoflurane as inhalational agent.
The overall risk of bias for the included studies (Figure 5) indicated that the risk was low in all the four included studies. One study was excluded based on the risk of bias, judged as unknown, during the extraction phase.3
In the study by Kletecka et al,4 postoperative measurements were conducted at 42 days postoperatively, but authors only considered a diagnosis of POCD-pNCD if three of the following tests were altered: the Digital Span Test (Forward and Backward), the Letter Number Sequence Test, the Verbal Fluency, the Trail Making Test (TMT), A and B, and the Stroop Test. Egawa et al6 conducted another study using a definition of POCD-pNCD when there was a difference in means of test scores of at least 20% between postoperative and preoperative scores. Postoperative measurements were performed three months after surgery. The tests used were the TMT (A and B), the Digit Span Forward and Backward, the Grooved Pegboard Test, as well as the MMSE. An additional study by Guo et al5 used a difference of at least one SD preoperatively and three months postoperatively in two of the following tests: the Verbal Learning Test (Learning Trial and Delay), the Concept Shifting Task (part C), the Stroop Color Word test (Part 3), and the Letter Digit Coding. The author did not mention which specific tests were altered in the postoperative period. Finally, in the study conducted by Micha et al,7 the authors diagnosed POCD based on a significant statistical difference between means of tests performed at 9 months postoperatively, compared to the preoperative results. Among the tests used, the ones reported as altered were: The Controlled Oral Word Association Test (COWAt), the Stroop Neuropsychological Screening, the Clock Test, the Three Word-Three Shapes, the Babcock Story Recall, the Instrumental Activities Daily Living (IADLS) and the Trail Making-B.
Discussion
The results from our systematic review and meta-analysis suggested that the incidence of POCD-DCR following the use of TIVA may be lower compared to inhalational anesthesia in the first 30 postoperative days. Even though we have succeeded in including a high total number of subjects in our review and meta-analysis, the heterogeneity in definitions of POCD-DCR, different psychometric tests used and its cuff-off values, among other factors, limit the reach of our conclusions. This is reflected in our heterogeneity analysis (I2 = 85%). Our study suggests that the concept of POCD should be redefined into a more objective definition. Moreover, it would be of interest to evaluate a more basic cognitive domain, such as attention, in all awake and alert individuals, since it is well known from the literature that attention plays a pivotal role to the functions of all other cognitive domains. It is reasonable to assume that specific cognitive deficits, such as memory, executive function, among others, may reflect a subjacent attention impairment. Future research should focus on objective attention measurements prior to other specific cognitive domains. This would allow a reduction in heterogeneity on POCD research.
Our results agree with a previous Cochrane systematic review on the same topic published in 2018,24 before the consensus stressed the importance of subclassifying POCD definitions according to time in the postoperative period.13 This explains why these authors only analyzed the period up to 30 days postoperative, since the late postoperative period, ie, between 30 days and 12 months postoperative, only came into focus for researchers after the 2018 consensus. Additionally, this is the reason why we included 10, instead of only 7 studies in the previous mentioned review paper. Moreover, we decided to conduct a systematic review in the period between 30 days and 12 months postoperative. Just like in our paper, those authors decided to define the outcome measure, ie, POCD, based on author’s definition in each individual included study, as a binary variable (yes or no), to proceed with the meta-analysis.
The potential benefits of propofol and TIVA in POCD might be mediated through its positive effects in diminishing the inflammatory cascade. Evidence has shown that propofol has anti-inflammatory properties compared to inhalation agents25 as in vivo study results have shown lower levels of circulating cytokines and other mediators of inflammation in animals injected with propofol.11 Inflammation has been associated with POCD in many different studies. An increase in various cytokines, including IL-6, TNF-α, IL-8, and IL-10, have been correlated with postoperative cognitive impairment.26 Recently, a meta-analysis was conducted assessing the association between various inflammatory biomarkers and POCD and concluded that higher postoperative C-reactive protein (n = 11 studies) and IL-6 (n = 17 studies) were associated with POCD.27 It is true that the possible role of the anesthetics in the inflammatory cascade is still yet to be clarified, with some evidence favoring the use of inhalational agents, such as sevoflurane, specifically in ischemia-reperfusion cell models.28 However, data favouring inhalational anesthetics in ischemia-reperfusion models were produced in the scenario of cardiopulmonary bypass surgeries, in which the etiopathogenesis of POCD is far more complex and diverse.29
The population enrolled in our review has a high median age, consequentially to the fact that most of the research on POCD involves elder individuals. Only one of the included studies admitted patients younger than 60 years old,4 and we did not have enough information to perform a subgroup analysis stratified by age. Even though all included studies relied on comparisons of the results of psychometric tests postoperative with the preoperative evaluation, only five studies used healthy controls not submitted to surgery or anesthesia in its study design,3,5,19,21,22 to make sure the cognitive decline was not consequence of the advanced age itself.
One limitation that must be stressed refers to the fact that propofol was used in both groups in all included studies, at least as a single bolus agent at the induction phase of anesthesia. It is uncertain if a single dose of propofol might exert any potential beneficial effects on POCD, consequentially to its potential effects at the inflammatory cascade, even considering that in TIVA group propofol is used in a continuous infusion through all the duration of the procedure. Maybe future studies in POCD should consider using another induction agent in the inhalational group, at the study design phase.
Regarding our secondary aim, we decided to proceed only with a systematic review of the literature, considering the few studies included and, consequently, the small number of subjects, given that the recommendations for testing between 30 days and 12 months postoperatively are relatively recent. Further studies, considering this testing period, are necessary in the future.
Most of these psychometric tests aim at a specific domain of cognitive function (Supplementary Table 1). Many of these tests have been validated in different clinical scenarios, including the postoperative period.30–37 It seems reasonable to hypothesize that different psychometric tests, targeting different cognitive domains, might differ in their ability to diagnose POCD. In addition, little attention has been spent on which specific tests and cognitive domains would be most likely altered in the postoperative period. So far, we have scarce evidence of which cognitive domains are more susceptible to POCD, with few data pointing towards the attention domain and executive function as potentially more affected in the postoperative period.38 As mentioned earlier, the attention domain plays a pivotal role in cognition since its proper function is essential to the functioning of all other domains. However, all the studies included in this review established the diagnosis of POCD accepting any altered domain as equally valid. This should, as well, be an important topic for future research.
Only two authors in our review reported which specific tests showed a significant difference in their postoperative assessment. One study reported that tests most frequently altered were the Semantic Verbal Fluency and the Letter Number Sequence Test, which measures the executive function and speed and visual space working memory cognitive domains.4 Another author reported that the COWAT, the Stroop Neuropsychological Screening, the Clock Test, the Three Word-Three Shapes, the Babcock Story Recall, the Instrumental Activities Daily Living (IADLS), and the TMT-B as the tests showed a difference in their postoperative assessment.7
Additionally, the application of psychometric tests for diagnosis of POCD that relies on a cut-off, such as one SD from the mean, or similar, could be insensitive for detecting minor but significant changes in cognitive status in the postoperative period. We hypothesize that the use of a test more focused on the attention domain, a pre-requisite for the proper function of all the other cognitive domains, could potentially be more sensitive in detecting subtle changes in the cognitive function perioperatively. This should be an additional relevant topic for future research.
It should be emphasized that nine out of the ten studies that we included in our present review titrated the level of anesthesia in both groups with the use of EEG-derived monitors, such as the BIS, all studies targeting a value between 40 and 60. The use of these devices might potentially lead to improved titration of anesthesia.3 Therefore, our results cannot be explained as a consequence of monitoring the level of consciousness on a particular group.
We considered it was appropriate to judge the quality of the evidence we found based on the GRADE system.16 Systematic reviews of RCTs are usually classified as a high level of evidence. However, the assessment of POCD is still a matter of controversy due to the difficult to select adequate instruments to evaluate basic cognitive domains, such as the attention domain. Consequently, we acknowledge that the quality of evidence produced in our study is most likely moderate, and the strength of recommendations based on our findings should be cautious. We believe that the evidence we found in this study should lead to future research on the association between TIVA and a potential lower incidence of POCD, with more objective definition and assessment of the outcome.
In conclusion, TIVA might be associated with a lower incidence of POCD, compared with inhalational anesthesia, at least in the first 30 postoperative days. However, future studies investigating POCD should focus on assessments of attention because the proper functioning of other cognitive subdomains (eg, memory, executive functions, etc.) relies on attention integrity. This could also potentially reduce heterogeneity on POCD research.
Disclosure
Ana Fernandez-Bustamante reports grants from NIH/NHLBI, Merck, and US DoD, outside the submitted work. The authors report no other potential conflicts of interest in relation to this work.
References
1. Glumac S, Kardum G, Karanovic N. Postoperative cognitive decline after cardiac surgery: a narrative review of current knowledge in 2019. Med Sci Monit. 2019;25:3262–3270. doi:10.12659/MSM.914435
2. Ballard C, Jones E, Gauge N, et al. Optimised anaesthesia to reduce post operative cognitive decline (POCD) in older patients undergoing elective surgery, a randomised controlled trial. PLoS One. 2012;7(6):e37410. doi:10.1371/journal.pone.0037410
3. Konishi Y, Evered LA, Scott DA, Silbert BS. Postoperative cognitive dysfunction after sevoflurane or propofol general anaesthesia in combination with spinal anaesthesia for Hip arthroplasty. Anaesth Intensive Care. 2018;46(6):596–600. doi:10.1177/0310057X1804600610
4. Kletecka J, Holeckova I, Brenkus P, Pouska J, Benes J, Chytra I. Propofol versus sevoflurane anaesthesia: effect on cognitive decline and event-related potentials. J Clin Monit Comput. 2019;33(4):665–673. doi:10.1007/s10877-018-0213-5
5. Guo L, Lin F, Dai H, et al. Impact of sevoflurane versus propofol anesthesia on post-operative cognitive dysfunction in elderly cancer patients: a double-blinded randomized controlled trial. Med Sci Monit. 2020;26:e919293. doi:10.12659/MSM.919293
6. Egawa J, Inoue S, Nishiwada T, et al. Effects of anesthetics on early postoperative cognitive outcome and intraoperative cerebral oxygen balance in patients undergoing lung surgery: a randomized clinical trial. Can J Anaesth. 2016;63(10):1161–1169. doi:10.1007/s12630-016-0700-4
7. Micha G, Tzimas P, Zalonis I, Kotsis K, Papdopoulos G, Arnaoutoglou E. Propofol vs Sevoflurane anaesthesia on postoperative cognitive dysfunction in the elderly. A randomized controlled trial. Acta Anaesthesiol Belg. 2016;67(3):129–137.
8. Moller JT, Cluitmans P, Rasmussen LS, et al. Long-term postoperative cognitive dysfunction in the elderly ISPOCD1 study. International study of post-operative cognitive dysfunction. Lancet. 1998;351(9106):857–861. doi:10.1016/S0140-6736(97)07382-0
9. Chen RM, Chen TG, Chen TL, et al. Anti-inflammatory and antioxidative effects of propofol on lipopolysaccharide-activated macrophages. Ann N Y Acad Sci. 2005;1042:262–271. doi:10.1196/annals.1338.030
10. Inada T, Hirota K, Shingu K. Intravenous anesthetic propofol suppresses prostaglandin E2 and cysteinyl leukotriene production and reduces edema formation in arachidonic acid-induced ear inflammation. J Immunotoxicol. 2015;12(3):261–265. doi:10.3109/1547691X.2014.938874
11. Skvarc DR, Berk M, Byrne LK, et al. Post-operative cognitive dysfunction: an exploration of the inflammatory hypothesis and novel therapies. Neurosci Biobehav Rev. 2018;84:116–133. doi:10.1016/j.neubiorev.2017.11.011
12. Kline R, Wong E, Haile M, et al. Peri-operative inflammatory cytokines in plasma of the elderly correlate in prospective study with postoperative changes in cognitive test scores. Int J Anesthesiol Res. 2016;4(8):313–321. doi:10.19070/2332-2780-1600065
13. Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Br J Anaesth. 2018;121(5):1005–1012. doi:10.1016/j.bja.2017.11.087
14. Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
15. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi:10.1136/bmj.d5928
16. Guyatt GH, Oxman AD, Vist GE, et al.; GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi:10.1136/bmj.39489.470347.AD
17. Cai Y, Hu H, Liu P, et al. Association between the apolipoprotein E4 and postoperative cognitive dysfunction in elderly patients undergoing intravenous anesthesia and inhalation anesthesia. Anesthesiology. 2012;116(1):84–93. doi:10.1097/ALN.0b013e31823da7a2
18. Geng YJ, Wu QH, Zhang RQ. Effect of propofol, sevoflurane, and isoflurane on postoperative cognitive dysfunction following laparoscopic cholecystectomy in elderly patients: a randomized controlled trial. J Clin Anesth. 2017;38:165–171. doi:10.1016/j.jclinane.2017.02.007
19. Zhang Y, Shan GJ, Zhang YX, et al. Propofol compared with sevoflurane general anaesthesia is associated with decreased delayed neurocognitive recovery in older adults. Br J Anaesth. 2018;121(3):595–604. doi:10.1016/j.bja.2018.05.059
20. Rohan D, Buggy DJ, Crowley S, et al. Increased incidence of postoperative cognitive dysfunction 24 hr after minor surgery in the elderly. Can J Anaesth. 2005;52(2):137–142. doi:10.1007/BF03027718
21. Tanaka P, Goodman S, Sommer BR, Maloney W, Huddleston J, Lemmens HJ. The effect of desflurane versus propofol anesthesia on postoperative delirium in elderly obese patients undergoing total knee replacement: a randomized, controlled, double-blinded clinical trial. J Clin Anesth. 2017;39:17–22. doi:10.1016/j.jclinane.2017.03.015
22. Tang N, Ou C, Liu Y, Zuo Y, Bai Y. Effect of inhalational anaesthetic on postoperative cognitive dysfunction following radical rectal resection in elderly patients with mild cognitive impairment. J Int Med Res. 2014;42(6):1252–1261. doi:10.1177/0300060514549781
23. Qi Liu C-L-L, Yang XY, Ji J-W, Peng S. Influence of sevoflurane anesthesia on postoperative recovery of the cognitive disorder in elderly patients treated with non-cardiac surgery. Biomed Res. 2017;28(9):4107–4110.
24. Miller D, Lewis SR, Pritchard MW, et al., Intravenous versus inhalational maintenance of anaesthesia for postoperative cognitive outcomes in elderly people undergoing non‐cardiac surgery. Cochrane Database Syst Rev. 2018;(8):CD012317. doi:10.1002/14651858.CD012317.pub2
25. Lee CJ, Tai YT, Lin YL, Chen RM. Molecular mechanisms of propofol-involved suppression of no biosynthesis and inducible iNOS gene expression in LPS-stimulated macrophage-like raw 264.7 cells. Shock. 2010;33(1):93–100. doi:10.1097/SHK.0b013e3181a6eaf5
26. Tang JX, Baranov D, Hammond M, Shaw LM, Eckenhoff MF, Eckenhoff RG. Human Alzheimer and inflammation biomarkers after anesthesia and surgery. Anesthesiology. 2011;115(4):727–732. doi:10.1097/ALN.0b013e31822e9306
27. Liu X, Yu Y, Zhu S, Ma D. Inflammatory markers in postoperative delirium (POD) and cognitive dysfunction (POCD): a meta-analysis of observational studies. PLoS One. 2018;13(4):e0195659. doi:10.1371/journal.pone.0195659
28. Li W, Zhang Y, Hu Z, Xu Y. Overexpression of NLRC3 enhanced inhibition effect of sevoflurane on inflammation in an ischaemia reperfusion cell model. Folia Neuropathol. 2020;58(3):213–222. doi:10.5114/fn.2020.100064
29. Tang S, Huang W, Zhang K, Chen W, Xie T. Comparison of effects of propofol versus sevoflurane for patients undergoing cardiopulmonary bypass cardiac surgery. Pak J Med Sci. 2019;35(4):1072–1075. doi:10.12669/pjms.35.4.1279
30. Chun MM, Golomb JD, Turk-Browne NB. A taxonomy of external and internal attention. Annu Rev Psychol. 2011;62:73–101. doi:10.1146/annurev.psych.093008.100427
31. Hanning CD. Postoperative cognitive dysfunction. Br J Anaesth. 2005;95(1):82–87. doi:10.1093/bja/aei062
32. Vide S, Gambus PL. Tools to screen and measure cognitive impairment after surgery and anesthesia. Presse Med. 2018;47(4 Pt 2):e65–e72. doi:10.1016/j.lpm.2018.03.010
33. Schmidt SL, Schmidt GJ, Padilla CS, et al. Decrease in attentional performance after repeated bouts of high intensity exercise in association-football referees and assistant referees. Front Psychol. 2019;10:2014. doi:10.3389/fpsyg.2019.02014
34. Schmidt SL, Simões EN, Novais Carvalho AL. Association between auditory and visual continuous performance tests in students with ADHD. J Atten Disord. 2019;23(6):635–640. doi:10.1177/1087054716679263
35. Simões EN, Carvalho ALN, Schmidt SL. The role of visual and auditory stimuli in continuous performance tests: differential effects on children with ADHD. J Atten Disord. 2021;25(1):53–62. doi:10.1177/1087054718769149
36. Simões EN, Padilla CS, Bezerra MS, Schmidt SL. Analysis of attention subdomains in obstructive sleep apnea patients. Front Psychiatry. 2018;9:435. doi:10.3389/fpsyt.2018.00435
37. Harvey PD. Domains of cognition and their assessment. Dialogues Clin Neurosci. 2019;21(3):227–237. doi:10.31887/DCNS.2019.21.3/pharvey
38. Silverstein JH, Steinmetz J, Reichenberg A, Harvey PD, Rasmussen LS. Postoperative cognitive dysfunction in patients with preoperative cognitive impairment: which domains are most vulnerable? Anesthesiology. 2007;106(3):431–435. doi:10.1097/00000542-200703000-00006
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
