Back to Journals » Infection and Drug Resistance » Volume 17
Incidence of and Risk Factors for Third-Generation Cephalosporin-Resistant Escherichia coli Bloodstream Infections in Children
Authors Cheng J, Liu Y, Li S, Pu K, Yang L, Tan L
Received 14 November 2023
Accepted for publication 6 February 2024
Published 9 February 2024 Volume 2024:17 Pages 543—550
DOI https://doi.org/10.2147/IDR.S449731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jie Cheng,1 Ya Liu,2 Shaojun Li,1 Kaibin Pu,1 Lin Yang,1 Liping Tan1
1Department of Emergency, National Clinical Research Center for Child Health and Disorders, Ministry of Education Key Laboratory of Child Development and Disorders, Chongqing Key Laboratory of Child Rare Diseases in Infection and Immunity, Children’s Hospital of Chongqing Medical University, Chongqing, 400014, People’s Republic of China; 2Department of Pediatrics, Chongqing Youyoubaobei Women and Children’s Hospital, Chongqing, 401147, People’s Republic of China
Correspondence: Liping Tan, Tel +86-23-63630194, Email [email protected]
Objective: Third-generation cephalosporin-resistant (3GC-R) bloodstream infection (BSI) is associated with poor prognosis. We investigated the incidence of and risk factors for 3GC-R Escherichia coli (E. coli) BSI in children.
Methods: Patients with E. coli BSIs who were hospitalized at the Children’s Hospital of Chongqing Medical University were retrospectively enrolled. Univariate and multivariate logistic regression analyses were used to identify the independent risk factors for 3GC-R BSI.
Results: Two hundred fifty-two children with E. coli BSIs were enrolled. The mortality rate was 11.51% (29/252). The infection rate of 3GC-R E. coli was 48.81% (123/252), and the incidence of E. coli BSI during hospitalization was 18.58 per 1000 person-days. Approximately half (47.22%, 119/252) of the children were infected with extended-spectrum beta-lactamases (ESBLs) produced by E. coli. More than one-third (37.30%, 94/252) of the children were unnecessarily administrated carbapenems. According to our logistic regression analysis, a history of carbapenem administration, an elevated Pediatric Sequential Organ Failure Assessment (pSOFA) score ≥ 2, and antimicrobial agent administration before blood culture were independently associated with 3GC-R BSI (odds ratio [OR] 2.05, 95% confidence interval [CI] 1.08– 3.94, P=0.029; OR 2.00, 95% CI 1.10– 3.71, P=0.025, OR 1.86, 95% CI 1.02– 3.42, P=0.044, respectively).
Conclusion: In this study, the incidence of 3GC-R E. coli BSI among children was retrospectively evaluated. Patients with a history of carbapenem administration, an elevated pSOFA score ≥ 2 and who were administrated antimicrobial agents before blood culture had an increased risk of 3GC-R E. coli BSI.
Keywords: third-generation cephalosporin-resistant, inappropriate use of carbapenems, Escherichia coli, bloodstream infection, children
Introduction
Bloodstream infection (BSI) is responsible for more than 2 million deaths per year, and Escherichia coli (E. coli) is one of the most common pathogens causing BSIs.1 The immediate administration of broad-spectrum antimicrobial agents may be crucial to avoid delayed antimicrobial therapy.2 However, as the antibiotic administration time window for BSIs has been emphasized in recent years,3,4 overtreatment may be also be an urgent problem for clinicians.5
Third-generation cephalosporins are among the most frequently used broad-spectrum antimicrobial agents in critical patients with gram-negative bacterial infections.6 The emergence of third-generation cephalosporin-resistant (3GC-R) isolates may worsen the prognosis,7 especially in areas with limited medical resources.8 For E. coli isolates, the resistance rate to third-generation cephalosporins is approximately 40% in China,9 thus, more intensive antimicrobial agents (such as carbapenems) may be a reasonable option. However, antibiotic associated adverse events should also be considered by clinicians,10 because antibiotic overuse may harm patients.11 Reducing antimicrobial overtreatment is an urgent problem with major challenges.12 Approximately one-third of children receive antimicrobial treatment during hospitalization, and one-quarter of antimicrobial therapy is not the optimal choice.13 Both overly narrow and unnecessarily broad regimens may increase mortality.11 How to balance the benefits of antimicrobial agents and their side effects has yet to be resolved. Rottier et al14 constructed two prediction scoring systems for 3GC-R Enterobacteriaceae bacteraemia, and those systems were further developed by Deelen et al.15 However, these two prediction systems14 and their external validation study15 included only adult patients, and few studies have reported any prediction models for children with 3GC-R BSIs. Choosing the adequate antimicrobial therapy for children with E. coli BSIs is still difficult for paediatricians, and early recognition of 3GC-R E. coli BSIs is urgently needed.
In this study, we investigated the incidence of and risk factors for the occurrence of 3GC-R E. coli BSIs in children, which may help clinicians predict the efficacy of third-generation cephalosporins for treating E. coli BSIs while avoiding the overuse of carbapenems as much as possible.
Methods
Study Design and Population
This was a retrospective, observational cohort study, conducted at the Children’s Hospital of Chongqing Medical University, the National Clinical Research Center for Child Health and Disorders. Patients with E. coli BSIs were enrolled from August 2015 to October 2022. The inclusion criteria were as follows: (i) hospitalized children; (ii) aged >1 month; (iii) had an E. coli BSI. The exclusion criteria were as follows: (i) incomplete clinical information; (ii) polymicrobial BSI. This study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University. (approval number (2023–423)). The requirement for informed consent was waived because this was a retrospective study. This study did not involve any human or animal experiments.
Data Collection and Definitions
We retrospectively collected demographic characteristics, patterns of admission, underlying conditions, sources of infection, antimicrobial therapy, susceptibility test results, Paediatric Sequential Organ Failure Assessment (pSOFA) scores and mortality data. An E. coli BSI was defined as the presence of E. coli in the blood.16 The unnecessary use of carbapenems was defined as the administration of carbapenems to patients with third-generation cephalosporin-sensitive (3GC-S) BSIs.15 An E. coli BSI occurring more than 48 hours after admission was considered a hospital-acquired infection.3 The sources of BSI were defined according to the Centers for Disease Control and Prevention/National Healthcare Safety Network (CDC/NHSN) surveillance guidelines.17 The pSOFA score was used to evaluate the severity of illness.18 Antibiotic susceptibility testing and identification of extended-spectrum beta-lactamase (ESBL) isolates were based on the Clinical and Laboratory Standards Institute guidelines.19 Multidrug resistance (MDR) was defined as acquired nonsusceptibility to three or more classes of antimicrobial agents.20
Statistical Analysis
The categorical variables are expressed as numbers (n) and percentages (%) and were compared by using Pearson’s χ2 test or Fisher’s exact test. Continuous variables are expressed as medians and interquartile ranges (IQRs), and were compared by using the Mann–Whitney U-test or the Student’s t test. Variables with P values ≥ 0.10 in univariate logistic regression analysis were included in univariate analysis. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) were calculated. All significance tests used a P-value<0.05 (2-sided). Analyses were conducted using R software (version 4.3.0, R Foundation for Statistical Computing Platform, China).
Results
Study Population
A total of 2785 pathogenic strains were isolated from blood cultures of patients hospitalized at the Children’s Hospital of Chongqing Medical University from August 2015 to October 2022. All the details are presented in Figure 1. There were 273 children with E. coli BSIs. Twenty-one patients were excluded: twelve patients with incomplete clinical information and nine patients with polymicrobial BSIs. Finally, two hundred fifty-two patients were enrolled in our study (Figure 2).
 |
Figure 1 Distribution of pathogens isolated from blood cultures. |
 |
Figure 2 Flowchart of the study population selection process. |
Clinical Characteristics of Children with E. Coli BSIs
The median age was 1.84 (IQR 0.22–8.52) years, and males accounted for 62.30% (157/252) of the population. The median length of stay before blood culture was 0.02 (IQR 0.00–0.58) days, and the overall median length of stay was 21.94 (IQR 12.75–34.92) days. The overall mortality was 11.51% (29/252). A total of 14.29% (36/252) of the patients were admitted from the emergency department, and 12.70% (32/252) of the patients were transferred from other medical institutions.
Many patients had bone marrow inhibition after chemotherapy (126/252, 50.00%) or after carbapenem administration (78/252, 30.95%). Approximately one sixth of patients had a history of BSI (40/252, 15.87%) or congenital heart disease (39/252, 15.48%). Nearly half of the E. coli BSIs occurred in the hospital (115/252, 45.63%) and more than half of the E. coli BSIs were with no specific source of infection (132/252, 52.38%). More than one-quarter (64/252, 25.40%) of patients had an elevated pSOFA score ≥2. The ESBL isolates accounted for 47.22% (119/252) of the isolates, and the third-generation cephalosporin resistance rate reached 48.81% (123/252). The incidence of 3GC-R E. coli BSI during hospitalization was 18.58 per 1000 person-days. A total of 28.17% (71/252) of patients were administrated with antimicrobial agents before blood culture, but only 9.92% (25/252) of patients received adequate antimicrobial agents before blood culture. Most of the children were administrated carbapenems or third-generation cephalosporins (182/252, 72.22%; 49/252, 19.44%; respectively). However, approximately one-third (94/252, 37.30%) of patients received unnecessary carbapenem treatment. All the detailed characteristics are shown in Table 1.
 |
Table 1 Characteristics of 252 Children with E. Coli Bloodstream Infection (BSI) |
Comparisons of Clinical Characteristics Between the 3GC-R and 3GC-S Groups
Table 2 shows the differences in clinical characteristics between the 3GC-R and 3GC-S groups. The patients with 3GC-R E. coli BSIs had significantly greater proportions of carbapenem administration history and BSI history than did those with 3GC-S E. coli BSIs (39.02% vs 23.26%, P=0.010; 21.95% vs 10.08%, P=0.016; respectively). There were significantly more 3GC-R E. coli BSI patients with an elevated pSOFA score ≥2 than 3GC-S E. coli BSI patients (33.33% vs 17.83%, P=0.007). Patients in the 3GC-S group had a remarkably greater rate of unnecessary carbapenem administration than did those in the 3GC-R group (72.87% vs 0.00%, P<0.001). The demographic data, patterns of admission, sources of infection, incidence of nosocomial infection, antimicrobial therapy, susceptibility test results, length of stay, length of stay before blood culture and mortality were not significantly different between the 3GC-R group and the 3GC-S group.
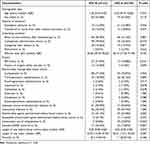 |
Table 2 Comparisons of Clinical Characteristics of 252 Children with E. Coli BSI Between Third-Generation Cephalosporin-Resistant (3GC-R) and Third-Generation Cephalosporin-Sensitive (3GC-S) Groups |
Risk Factors for 3GC-R E. Coli BSI
Table 3 presents the logistic analysis of 3GC-R E. coli BSI in children. According to the univariate analysis, a history of carbapenems administration, an elevated pSOFA score ≥2, antimicrobial agent administration before blood culture, a history of BSI and a history of surgery within one year were associated with an increased risk of 3GC-R E. coli BSI (P<0.1). According to multivariate logistic analysis, carbapenem administration history, an elevated of pSOFA score ≥2 and antimicrobial agents administrated before blood culture were independently correlated with the presence of 3GC-R E. coli BSI (OR 2.05, 95% CI 1.08–3.94, P=0.029; OR 2.04, 95% CI 1.10–3.71, P=0.025; OR 1.86, 95% CI 1.02–3.42, P=0.044, respectively).
 |
Table 3 Logistic Regression Analysis of Risk Factors for 3GC-R E. Coli BSI in Children |
Discussion
E. coli was the most common pathogen isolated from blood culture, and approximately 40% of the isolates were resistant to third-generation cephalosporins.9 However, few studies have reported the incidence of 3GC-R E. coli BSI. In this study, the incidence of 3GC-R E. coli BSI during hospitalization was 18.58 per 1000 person-days. These findings may help clinicians evaluate the medical burden of 3GC-R E. coli BSIs in children.
Intensive antimicrobial treatment is sometimes a double-edged sword. Although timely treatment can save lives,3,4 antimicrobial therapy that is too aggressive may also increase the risk of mortality.11 Furthermore, several broad-spectrum antibiotics (eg, carbapenems) are scarce medical resources in developing areas. When administrating the antimicrobial therapy, clinicians must balance the risks of overprescribing carbapenems and inappropriate empiric antibiotics. Tauzin et al reported that the extensive administration of a broad-spectrum antibiotic was associated with the emergence of drug-resistant bacteria.21 The presence of drug-resistant bacteria may be attributed to the antibiotic-related sequelae, similar to the selection pressure for resistant organisms or changes in the microbiome leading to dysbiosis and increased susceptibility to colonization.22 In our study, we also found that a history of carbapenem administration increased the risk of 3GC-R E. coli BSI 2.05-fold, and for patients who received antimicrobial agents before blood culture, the risk increased 1.86-fold. Although receiving extended-spectrum antimicrobial agents may increase the incidence of 3GC-R E. coli, 1-hour or 3-hour regimens are still recommended for patients with severe BSIs.2 Appropriate antimicrobial de-escalation may also help to decrease the unnecessary use of carbapenems.
Patients in more critical conditions are recommended to receive more intensive antimicrobial therapy.2 In this study, many patients were had bone marrow inhibition after chemotherapy (126/252, 50.00%) and a history of BSI (40/252, 15.87%) or congenital heart disease (39/252, 15.48%), and up to 72.22% (182/252) for whom carbapenem was used in our study seemed reasonable. However, 37.30% (94/252) of the children in this study did not need to be treated with carbapenems. The pSOFA is one of the most common prognostic scoring systems for children.18 Aleidan et al23 reported that a higher SOFA score indicated an increased risk of resistant infection. In this study, we found that patients with an elevated pSOFA score ≥2 had a 2.00-fold increased risk of 3GC-R E. coli BSI. To avoid overtreatment, patients without an elevated of pSOFA score ≥2 may not need treatment with carbapenem.
Aggressive antimicrobial therapy may save lives, but antibiotic associated adverse events should also be considered.10 Tribble et al reported that treating one-quarter of hospitalized children was not the optimal choice.13 Early recognition of 3GC-R E. coli BSI is urgently needed. Rottier et al14 constructed two prediction scoring systems for 3GC-R Enterobacteriaceae bacteraemia, however, they14 did not include the children in their study. It is widely known that the disease spectrum, pathophysiological process and the antimicrobial therapy used in children are different from those used in adult patients. Moreover, there are no reported prediction criteria for 3GC-R BSI in children. In this study, we identified three risk factors for 3GC-R E. coli BSI in children. These risk factors are clinical predictors that are readily available before the initiation of empirical antimicrobial treatment. These findings may help clinicians predict the efficacy of third-generation cephalosporins for treating E. coli BSIs, and avoid unnecessary use of carbapenems as much as possible.
There were several limitations in our study. First, this was a retrospective, small sample, single-centre study, which may limit the generalizability of our results, and a prospective, large-sample, multicentre study is expected to strengthen our conclusions. Second, we focused only on children in our study, therefore, our results may not be generalizable to newborns or adult patients. Third, the risk factors found in our study were applied to predict the possibility of 3GC-R in patients with E. coli BSI, and these risk factors may not be applicable for other infections.
Conclusion
The incidence of 3GC-R E. coli BSI in children was retrospectively evaluated in this study. A history of carbapenem administration, an elevated pSOFA score ≥2 and antimicrobial agent administration before blood culture were associated with 3GC-R E. coli BSI. When these conditions are met, third-generation cephalosporins may be avoided, and carbapenems may be a reasonable option.
Abbreviations
BSI, Bloodstream infection; CI, Confidence interval; ESBL, Extended spectrum beta-lactamase; IQR, Interquartile range; MDR, Multidrug resistance; OR, Odds ratio; pSOFA, Paediatric Sequential Organ Failure Assessment; 3GC-R, Third-generation cephalosporin resistant; 3GC-S, Third-generation cephalosporin sensitive.
Data Sharing Statement
The data from this study can be obtained from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The requirement for informed consent was waived by the Ethics Committee of the Children’s Hospital of Chongqing Medical University, as only anonymized data were utilized in this retrospective study to protect individuals. This study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University. (approval number (2023-423)). All the authors declare that this study did not involve any human or animal experiments. All methods were carried out in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Acknowledgments
We thanks to American Journal Experts for their valuable advice to the linguistic revision of this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Chongqing Municipal Health Commission (2022-WSJK-053) and the National Clinical Research Center for Child Health and Disorders (NCRCCHD-2022-GP-0X). The funders of the study had no role in the study design; data collection or analysis; or article writing, submission or revision.
Disclosure
The authors have no competing interests to declare for this work.
References
1. Ikuta KS, Swetschinski LR, Aguilar GR, et al. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2022;400(10369):2221–2248. doi:10.1016/s0140-6736(22)02185-7
2. Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediat Crit Care Med. 2020;21(2):e52–e106. doi:10.1097/pcc.0000000000002198
3. Cheng J, Li Q, Zhang G, et al. Time to appropriate antimicrobial therapy serves an independent prognostic indicator in children with nosocomial Klebsiella pneumoniae bloodstream infection. BMC Pediatric. 2022;22(1):568. doi:10.1186/s12887-022-03622-6
4. Timsit J-F, Ruppé E, Barbier F, Tabah A, Bassetti M. Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med. 2020;46(2):266–284. doi:10.1007/s00134-020-05950-6
5. Chiotos K, Blumenthal J, Boguniewicz J, et al. Antibiotic indications and appropriateness in the pediatric intensive care unit: a 10-center point prevalence study. Clin Infect Dis. 2023;76(3):e1021–e1030. doi:10.1093/cid/ciac698
6. Chan EL, Birk RJ, Zabransky RJ. The comparative in vitro susceptibility of cefazolin-resistant organisms to six cephalosporins, four penicillins, and three aminoglycosides. Diagn Microbiol Infect Dis. 1985;3(6):525–533. doi:10.1016/s0732-8893(85)80010-9
7. MacKinnon MC, McEwen SA, Pearl DL, et al. Increasing incidence and antimicrobial resistance in Escherichia coli bloodstream infections: a multinational population-based cohort study. Antimicrob Resist Infect Control. 2021;10(1):131. doi:10.1186/s13756-021-00999-4
8. Lester R, Musicha P, Kawaza K, et al. Effect of resistance to third-generation cephalosporins on morbidity and mortality from bloodstream infections in Blantyre, Malawi: a prospective cohort study. Lancet Microbe. 2022;3(12):e922–e930. doi:10.1016/s2666-5247(22)00282-8
9. Hu F, Yuan L, Yang Y, et al. A multicenter investigation of 2773 cases of bloodstream infections based on China antimicrobial surveillance network (CHINET). Front Cell Infect Microbiol. 2022;12:1075185. doi:10.3389/fcimb.2022.1075185
10. Tamma PD, Avdic E, Li DX, Dzintars K, Cosgrove SE. Association of adverse events with antibiotic use in hospitalized patients. JAMA Intern Med. 2017;177(9):1308–1315. doi:10.1001/jamainternmed.2017.1938
11. Pak TR, Rhee C, Klompas M. Timing and spectrum of antibiotic treatment for suspected sepsis and septic shock: why so controversial? Infect Dis Clin North Am. 2022;36(4):719–733. doi:10.1016/j.idc.2022.08.001
12. Tarrant C, Krockow EM. Antibiotic overuse: managing uncertainty and mitigating against overtreatment. BMJ Qual Saf. 2022;31(3):163–167. doi:10.1136/bmjqs-2021-013615
13. Tribble AC, Lee BR, Flett KB, et al. Appropriateness of antibiotic prescribing in United States children’s hospitals: a national point prevalence survey. Clin Infect Dis. 2020;71(8):e226–e234. doi:10.1093/cid/ciaa036
14. Rottier WC, van Werkhoven CH, Bamberg YRP, et al. Development of diagnostic prediction tools for bacteraemia caused by third-generation cephalosporin-resistant enterobacteria in suspected bacterial infections: a nested case-control study. Clin Microbiol Infect. 2018;24(12):1315–1321. doi:10.1016/j.cmi.2018.03.023
15. Deelen JWT, Rottier WC, Giron Ortega JA, et al. An international prospective cohort study to validate 2 prediction rules for infections caused by third-generation cephalosporin-resistant enterobacterales. Clin Infect Dis. 2021;73(11):e4475–e4483. doi:10.1093/cid/ciaa950
16. See LL. Bloodstream infection in children. Pediatr Crit Care Med. 2005;6(3 Suppl):S42–44. doi:10.1097/01.Pcc.0000161945.98871.52
17. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008;36(5):309–332. doi:10.1016/j.ajic.2008.03.002
18. Matics TJ, Sanchez-Pinto LN. Adaptation and validation of a pediatric sequential organ failure assessment score and evaluation of the sepsis-3 definitions in critically ill children. JAMA Pediat. 2017;171(10):e172352. doi:10.1001/jamapediatrics.2017.2352
19. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: 24th Informational Supplement. Clinical and Laboratory Standards Institute; 2014.
20. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
21. Tauzin M, Ouldali N, Béchet S, Caeymaex L, Cohen R. Pharmacokinetic and pharmacodynamic considerations of cephalosporin use in children. Expert Opin Drug Metab Toxicol. 2019;15(11):869–880. doi:10.1080/17425255.2019.1678585
22. Omulo S, Ita T, Mugoh R, et al. Risk factors for colonization with extended-spectrum cephalosporin-resistant and carbapenem-resistant enterobacterales among hospitalized patients in Kenya: an antibiotic resistance in communities and hospitals (ARCH) study. Clin Infect Dis. 2023;77(Suppl 1):S97–s103. doi:10.1093/cid/ciad258
23. Aleidan FAS, Alkhelaifi H, Alsenaid A, et al. Incidence and risk factors of carbapenem-resistant Enterobacteriaceae infection in intensive care units: a matched case-control study. Exp Rev Anti-Infective Ther. 2021;19(3):393–398. doi:10.1080/14787210.2020.1822736
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
