Back to Journals » Clinical Epidemiology » Volume 9
Incidence, clinical presentation, and outcome of HIV-1-associated cryptococcal meningitis during the highly active antiretroviral therapy era: a nationwide cohort study
Authors Touma M, Rasmussen LD , Martin-Iguacel R, Engsig FN, Stærke NB , Stærkind M, Obel N, Ahlström MG
Received 21 February 2017
Accepted for publication 3 May 2017
Published 21 July 2017 Volume 2017:9 Pages 385—392
DOI https://doi.org/10.2147/CLEP.S135309
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Irene Petersen
Madeleine Touma,1 Line D Rasmussen,2 Raquel Martin-Iguacel,2 Frederik Neess Engsig,3 Nina Breinholt Stærke,4 Mette Stærkind,5 Niels Obel,1 Magnus Glindvad Ahlström1
1Department of Infectious Diseases, Rigshospitalet, Copenhagen University Hospital, Copenhagen, 2Department of Infectious Diseases, Odense University Hospital, Odense, 3Department of Infectious Diseases, Copenhagen University Hospital, Hvidovre, 4Department of Infectious Diseases, Aarhus University Hospital, Aarhus, 5Department of Infectious Diseases, Aalborg University Hospital, Aalborg, Denmark
Background: Human immunodeficiency virus (HIV) infection with advanced immunosuppression predisposes to cryptococcal meningitis (CM). We describe the incidence, clinical presentation, and outcome of CM in HIV-infected individuals during the highly active antiretroviral therapy (HAART) era.
Methods: A nationwide, population-based cohort of HIV-infected individuals was used to estimate incidence and mortality of CM including risk factors. A description of neurological symptoms of CM at presentation and follow-up in the study period 1995–2014 was included in this study.
Results: Among 6,351 HIV-infected individuals, 40 were diagnosed with CM. The incidence rates were 3.7, 1.8, and 0.3 per 1000 person-years at risk in 1995–1996, 1997–1999, and 2000–2014, respectively. Initiation of HAART was associated with decreased risk of acquiring CM [incidence rate ratio (IRR), 0.1 (95% CI, 0.05–0.22)]. African origin was associated with increased risk of CM [IRR, 2.05 (95% CI, 1.00–4.20)]. The main signs and symptoms at presentation were headache, cognitive deficits, fever, neck stiffness, nausea, and vomiting. All individuals diagnosed with CM had a CD4+ cell count <200 cells/µl [median 26; interquartile range (IQR), 10–50)]. Overall, mortality following CM was high and mortality in the first 4 months has not changed substantially over time. However, individuals who survived generally had a favorable prognosis, with 86% (18/21) returning to the pre-CM level of activity.
Conclusion: The incidence of HIV-associated CM has decreased substantially after the introduction of HAART. To further decrease CM incidence and associated mortality, early HIV diagnosis and HAART initiation seems crucial.
Keywords: cryptococcal meningitis, highly active antiretroviral therapy, HIV
Background
Cryptococcal meningitis (CM) is caused by the encapsulated yeast Cryptococcus (C.) neoformans and is generally diagnosed in individuals with cellular immune deficiencies, such as human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS).1 CM is the most common cause of meningitis in some areas of sub-Saharan Africa, where the occurrence of CM is the highest in the world.2 An estimated one million new cases are diagnosed each year and, worldwide, the disease causes >600,000 deaths yearly.3 The incidence of HIV-associated CM is lowest in Western countries and has declined considerably in North America and Western Europe after the introduction of highly active antiretroviral therapy (HAART).4–9 Incidence rates ranged from 2.5/1000 person-years at risk (PYR) in the pre-HAART era to 1.5/1000 PYR in the post-HAART era.10
There has been a general decrease in mortality in HIV-infected individuals in Denmark during the HAART era.11 The substantial reduction in HIV-associated mortality due to HAART resulted in a notable shift in causes of death among HIV-infected individuals.12 HIV-infected individuals are more vulnerable to age-, disease-, and/or treatment-related morbidities.13,14 The main focus in HIV care in the post-HAART era has been HAART-related problems such as toxicity, drug–drug interactions, and antiretroviral drug resistance.15
The use of HAART in high-income countries has improved the long-term survival of HIV-infected individuals with CM, but the mortality rate remains high during the first 3 months of CM.16 This highlights the importance of diagnosing HIV-infected individuals during an early stage, before they develop severe immunodeficiency, to avoid AIDS-associated diseases such as CM. To prevent and control CM in the future, it is imperative to gain insight into the epidemiology of CM. We used a nationwide, population-based cohort of HIV-infected individuals to determine incidence, clinical presentation, and prognosis of CM. Furthermore, we collected data on choice of treatment regimens of CM.
Methods
Study design
This nationwide cohort study is divided into two parts. In the first part of the study, we estimated the incidence of CM in a cohort of HIV-infected individuals in the period 1995–2014. In the second part of the study, the study population comprised HIV-infected individuals diagnosed with CM, and the outcomes were neurological symptoms and mortality. We used a study design that has been described previously.17
Setting
On December 31, 2014, Denmark had a population of 5.6 million citizens and the estimated prevalence of HIV-infection in the adult population was 0.1%.18 Antiretroviral treatment is provided free of charge in Denmark to all HIV-infected individuals in one of the country’s eight specialized HIV-care centers. HIV-infected individuals are seen on an outpatient basis at intended intervals of 12–24 weeks. The national criteria for initiating HAART has been described elsewhere.19
Data extraction
Participants were included from the Danish HIV Cohort Study (DHCS) – a prospective study that includes all HIV-infected individuals ≥16 years since January 1, 1995. Data include demographics, date of HIV diagnosis, AIDS-defining events, antiretroviral treatment, CD4+ cell counts, viral loads, and so on. Individuals are consecutively enrolled and data are updated annually. All Danish citizens are provided with a unique 10-digit personal identification number (PIN) at birth or immigration, which prevents multiple registrations in the DHCS. The DHCS has been described in detail previously.19
Study population
All HIV–1 infected individuals who 1) were registered in the DHCS prior to December 31, 2014; 2) lived in Denmark at study inclusion; and 3) had been assigned a PIN were included in this study.
Outcome and statistical analysis
Part 1
In the first part of the study, the outcome was time to first diagnosis of CM. A diagnosis of CM was defined as detection of C. neoformans in the cerebrospinal fluid (CSF) by microscopy, culture, or antigen-test; the test was performed at Statens Serum Institut, were they used a latex agglutination test.20
The PYR was calculated from HIV diagnosis or from January 1, 1995, whichever came last until a diagnosis of CM, death, emigration, or December 31, 2014, whichever came first. Incidence rates (IRs) for CM and 95% confidence intervals (95% CI) were calculated for the periods 1995–1996, 1997–1999, and 2000–2014, which corresponds to the pre-, early-, and late HAART periods, data from previous studies have indicated that the use of HAART has changed substantially between these time periods.21 For the individuals that received HAART during the study period, we calculated IRs from initiation of HAART to CM.
In addition to this, we stratified the analyses based on gender and origin (African and non-African).
Part 2
In the second part of the study, outcome measures were neurological symptoms and mortality among HIV-infected individuals with CM. Information about laboratory results, treatment, and neurological symptoms at the presentation of CM were extracted from patient records.
Individuals diagnosed with CM were followed for a total of 3 years or until death, emigration, or December 31, 2014 whichever came first.
Neurological symptoms were estimated 4 months and 3 years after CM diagnosis. Neurological status was defined as deteriorated, unchanged, better, or resolved compared to their pre-CM status.
Poisson regression analysis was used to calculate incidence rate ratios (IRRs) as estimates of the impact of risk factors on incidence of CM in the HIV-infected population. Multivariate models included the following covariates: gender, age (≤40 years vs >40 years), origin (African vs non-African), route of transmission [injection drug user vs heterosexual vs men who have sex with men (MSM)], and year of CM diagnosis (before vs after January 1, 1997).
Statistical analyses were undertaken with Stata statistical software: Release 11 (StataCorp. 2009, StataCorp LP, College Station, TX, USA).
Ethics statement
The study was approved by the Danish Data Protection Agency (journal no. 2008-41-1781). According to Danish legislations individual consent is not required to perform register based studies.
Results
During screening, 6,351 HIV-infected individuals fulfilled the study inclusion criteria. Of these, 2,015 (32%) individuals were diagnosed with HIV before January 1, 1995; 1,115 (18%) individuals died and 138 (2%) emigrated during follow-up. A total of 4,829 (76%) were men, 2,952 (46%) were MSM, 611 (10%) were injection drug users, and 4,970 (78%) were Caucasian. The median age at study inclusion was 35.0 years [interquartile range (IQR), 28.5–43.1 years; Table 1].
Part 1
Incidence of CM
Forty individuals were diagnosed with CM during the study period; 15 were diagnosed with CM between 1995 and 1996, 8 between 1997 and 1999, and 17 in the years 2000–2014.
The overall incidence decreased from the pre-HAART era [IR 3.7/1000 PYR (95% CI, 2.2–6.1)] to the early- [IR 1.8/1000 PYR (95% CI, 0.9–3.6)] and late-HAART era [IR 0.3/1000 PYR (95% CI, 0.2–0.5)] (Table 2).
In individuals in whom HAART was initiated, the incidence of CM was 0.2/1000 PYR (95% CI, 0.1–0.3). The IR was 0.5/1000 PYR (95% CI, 0.3–0.7) for individuals of non-African origin and 1.1/1000 PYR (95% CI, 0.6–2.0) for individuals of African origin.
HAART was associated with a substantial reduction in risk of acquiring CM [IRR 0.1 (95% CI, 0.05–0.22)]. When we adjusted for potential confounders (gender, age, origin, and route of transmission), the impact of HAART on the risk of CM did not change substantially [IRR, 0.09 (95% CI, 0.05–0.19)]. African origin was associated with increased risk of CM [IRR, 2.05 (95% CI, 1.00–4.20); Table 2].
Part 2
Characteristics
Characteristics of the HIV-infected individuals diagnosed with CM are summarized in Table 1. All individuals had late-stage HIV disease at CM presentation with a CD4+ cell count <200 cells/µl [median 26 (IQR, 10–50)]. The median viral load at diagnosis was 4.8 (IQR, 3.0–5.4) log10 copies/mL. Thirty-three percent (13/40) were diagnosed with AIDS prior to CM. Thirty-three percent (13/40) were late presenters – that is, they were diagnosed with CM at HIV-diagnosis ± 30 days.
The median time from HIV diagnosis to CM was 2.24 years (IQR, 0.02–6.55). Seventy-three percent (29/40) of CM individuals were men, 40% (16/40) were MSM, and 53% (21/40) were heterosexual. The median age at CM diagnosis was 38.0 years (IQR, 32.3–44.3).
Diagnostic methods
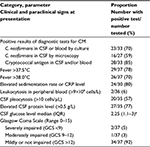
Patient records and, thereby, clinical and paraclinical data were missing for 3 out of 40 individuals with CM. Diagnostic results and neurological symptoms are, therefore, only available for a maximum of 37 HIV-infected individuals with CM.
Among those tested, 85% (28/33) tested positive for cryptococcal antigen in CSF and/or blood (Table 3); 70% (23/33) were diagnosed by culture for C. neoformans in CSF or blood, and three individuals had a positive blood culture only. Fifty-nine percent (16/27) were diagnosed by microscopy of the CSF for C. neoformans and 14 of those had a positive India ink report. The diagnosis was mainly based on a combination of different diagnostic methods.
Seventy-eight percent (29/37) presented with fever and 80% (24/30) had elevated sedimentation rate or C-reactive protein (CRP) level. In contrast, only few individuals had leukocytosis in peripheral blood. CSF pleocytosis was seen in 57% (20/35). Seventy-five percent (15/20) with CSF pleocytosis had leukocyte differentiation, with a predominance of lymphocytes in 10 out of 15 individuals, whereas neutrophils predominated in the latter five individuals. Seventy-seven percent (27/35) had elevated CSF protein levels. The median CSF glucose level was 2.25 (IQR, 1.1–3) mmol/L.
Neurological symptoms
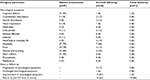
The most frequent signs and symptoms were fever, headache, nausea, and vomiting cognitive deficits and neck stiffness. Other neurological signs and symptoms such as coordination disturbance, speech disturbance, visual impairment, facial palsy, limb paresis, seizures, photophobia, and papilledema occurred less frequently (Table 4). Only two individuals presented with a Glasgow Coma Scale <9, and these individuals were admitted to the intensive care units at presentation of CM (Table 3).
After 4 months of follow-up, the main symptoms were nausea, vomiting, and headache. Eighty-one percent (13/16) had an improvement of symptoms, and 62% (10/16) reconstituted to their pre-CM level of activity. Two individuals showed progression of neurological symptoms and one had the same symptoms as at the onset of CM.
Within 3 years of follow-up, 86% (18/21) had returned to their pre-CM level of activity (Table 4). Table 1 shows antifungal therapy and reasons for stopping maintenance therapy.
Mortality
Fifty-three percent (21/40) of individuals diagnosed with CM died during the study period; in eight of these cases, death was due to CM. Ten individuals died due to other HIV-related causes such as progressive multifocal leukoencephalopathy (PML), Kaposi sarcoma, lymphoma, anal cancer, bacterial infection, and pneumonia. One individual died due to traumatic brain injury and, in two cases, the cause of death was unknown.
Twelve individuals died within the first 4 months of follow-up, and two additional individuals died within the subsequent 3-year period.
Discussion
This nationwide, population-based cohort study demonstrates that both incidence and mortality of CM among HIV-infected individuals in Denmark have decreased dramatically during the last 20 years (1995–2014).
Furthermore, CM was observed in individuals with advanced HIV disease and severe immunodeficiency, documented by a low median CD4+ cell count and a high viral load. As in findings from other studies,22 the most frequent signs and symptoms were fever, headache, nausea and vomiting, cognitive deficits, and neck stiffness. Our study showed that the sensitivity of CSF pleocytosis in individuals diagnosed with CM was 57%. Other observations made by a French study found that 25% of all CM individuals in France had a normal CSF cell count.23 The absence of pronounced inflammation could be regarded as an argument against CNS infection; however, our findings indicate that a normal CSF cell count does not exclude a CM diagnosis. Other European studies found that cryptococcal antigen testing in HIV-infected individuals with low immunity might represent a strategy to expedite the diagnosis of CM.24 However, cryptococcal antigen testing in CSF and/or blood had a sensitivity of 85% in our study.
A low CD4+ cell count was the strongest predictor for being diagnosed with CM. It is most likely that the observed reduction in CM incidence among HIV-infected individuals is due to improved management of HIV by increased use of HAART and decreased antiretroviral resistance in Denmark.25 These findings suggest that early detection of HIV followed by HAART initiation is essential to avoid severe immunodeficiency and, thereby, life-threatening HIV-associated diseases such as CM. The main focus in the management of CM should be the prophylactic effect of maintaining a high CD4+ cell count. Our study shows that 33% of all CM individuals during the study period presented for care with an AIDS-defining event. If these late presenters were diagnosed before severe immunodeficiency and HAART was initiated shortly thereafter, these cases could probably be avoided.
African origin was associated with a higher incidence of CM, which corresponds well with the findings of other studies.7,26,27 CM is a subacute infection, with a long subclinical phase.28 The increased risk in individuals of African origin most likely reflects that immigrants import the disease in the subclinical phase that then develops to manifest disease after arriving in Denmark.
We generally observed high mortality following HIV-associated CM, and were unable to identify a reduction in mortality of HIV-associated CM over time; specifically, the mortality in the first 4 months did not seem to have changed substantially. However, our statistical power to show a difference was small.
A previous study in Denmark described the outcome of CM in HIV-infected individuals treated at two university hospitals in Copenhagen between 1988 and 2008.29 In accordance with our study, they found that long-term survival after CM improved significantly with the use of HAART. Our study shows that most survivors recovered with only few neurological complications. This emphasizes the importance of early detection of CM and initiation of aggressive therapy including HAART. However, to further decrease CM incidence and associated mortality, early HIV diagnosis and HAART initiation seems crucial.
To our knowledge, this is the first study to present nationwide population-based data on the incidence of CM in HIV-infected individuals as well as clinical presentation and outcome of CM during the HAART era in Denmark. Our study’s major strengths are the nationwide, population-based design, the long and nearly complete follow-up, and completeness of data.
Our study has some weaknesses. Neurological symptoms were examined retrospectively from patient records. Consequently, the degree of neurological symptoms at presentation of CM and sequelae after the diagnosis of CM may have been even worse than what we have observed. Our study population predominantly included Caucasians (78%) and our results could, therefore, not be generalized to geographical regions such as Africa and Asia.
In conclusion, this study shows that the overall incidence and mortality of CM decreased from the pre- to the late-HAART era. Although CM is a very rare disease in Denmark, it could be connected to an initial manifestation of HIV infection or AIDS and should still be suspected in all HIV-infected individuals with low CD4+ cell count presenting with neurological symptoms, headache, and fever.
Acknowledgments
This work was supported by Preben og Anne Simonsens Foundation, NOVO Nordisk Foundation, Rigshospitalet, Copenhagen University, The Danish AIDS Foundation, and The Augustinus Foundation.
Study centers of the Danish HIV Cohort Study: Departments of Infectious Diseases at Copenhagen University Hospitals, Rigshospitalet (J Gerstoft, N Obel) and Hvidovre (G Kronborg), Odense University Hospital (C Pedersen), Aarhus University Hospitals, Skejby (CS Larsen) and Aalborg (G Pedersen), Herning Hospital (R Mohey), Hillerød Hospital (L Nielsen), and Kolding Hospital (J Jensen).
Disclosures
NO has received research funding from Roche, Bristol-Myers Squibb, Merck Sharp & Dohme, GlaxoSmithKline, Abbott, Boehringer Ingelheim, Janssen-Cilag, and Swedish Orphan. MGA has received research funding from the research board of Copenhagen University Hospital, Rigshospitalet, and from the Bjørn Astrups fund, and has received travel grants from GSK and Janssen.
The sponsors had no role in the design, conduct, or analysis of the study nor in the decision to publish the manuscript. The authors report no other conflicts of interest in this work.
References
Bicanic T, Harrison TS. Cryptococcal meningitis. Br Med Bull. 2005;72:99–118. | ||
Veltman JA, Bristow CC, Klausner JD. Meningitis in HIV-positive patients in sub-Saharan Africa: a review. J Int AIDS Soc. 2014;17:19184. | ||
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23(4):525–530. | ||
Dromer F, Mathoulin-Pélissier S, Fontanet A, Ronin O, Dupont B, Lortholary O; French Cryptococcosis Study Group. Epidemiology of HIV-associated cryptococcosis in France (1985–2001): comparison of the pre- and post- HAART eras. AIDS. 2004;18(3):555–562. | ||
Antinori S, Ridolfo A, Fasan M, et al. AIDS-associated cryptococcosis: a comparison of epidemiology, clinical features and outcome in the pre- and post-HAART eras. Experience of a single centre in Italy. HIV Med. 2009;10(1):6–11. | ||
van Elden LJ, Walenkamp AM, Lipovsky MM, et al. Declining number of patients with cryptococcosis in the Netherlands in the era of highly active antiretroviral therapy. AIDS. 2000;14(17):2787–2788. | ||
Mirza SA, Phelan M, Rimland D, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992–2000. Clin Infect Dis. 2003;36(6):789–794. | ||
Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997–2009. PLoS One. 2013;8(2):e56269. | ||
d’Arminio Monforte A, Cinque P, Mocroft A, et al; EuroSIDA Study Group. Changing incidence of central nervous system diseases in the EuroSIDA cohort. Ann Neurol. 2004;55(3):320–328. | ||
Sacktor N, Lyles RH, Skolasky R, et al; Multicenter AIDS Cohort Study. HIV-associated neurologic disease incidence changes: Multicenter AIDS Cohort Study, 1990–1998. Neurology. 2001;56(2):257–260. | ||
Lohse N, Hansen AB, Pedersen G, et al. Survival of persons with and without HIV infection in Denmark, 1995–2005. Ann Intern Med. 2007;146(2):87–95. | ||
Zwahlen M, Lundgren JD. Commentary: death in the era of potent antiretroviral therapy: shifting causes, new challenges. Int J Epidemiol. 2005;34(1):130–131. | ||
Deeks SG, Phillips AN. HIV infection, antiretroviral treatment, ageing, and non-AIDS related morbidity. BMJ. 2009;338:a3172. | ||
Hasse B, Ledergerber B, Furrer H, et al; Swiss HIV Cohort Study. Morbidity and aging in HIV-infected persons: the Swiss HIV Cohort Study. Clin Infect Dis. 2011;53(11):1130–1139. | ||
Marzolini C, Elzi L, Gibbons S, et al; Swiss HIV Cohort Study. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antivir Ther. 2010;15(3):413–423. | ||
Lortholary O, Poizat G, Zeller V, et al. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS. 2006;20(17):2183–2191. | ||
Engsig FN, Hansen AB, Omland LH, et al. Incidence, clinical presentation, and outcome of progressive multifocal leukoencephalopathy in HIV-infected patients during the highly active antiretroviral therapy era: a nationwide cohort study. J Infect Dis. 2009;199(1):77–83. | ||
Statistics Denmark [homepage on the Internet] Population and elections. Available from: http://www.statistikbanken.dk. Accessed February 16, 2017. | ||
Omland LH, Ahlström MG, Obel N. Cohort profile update: the Danish HIV Cohort Study (DHCS). Int J Epidemiol. 2014;43(6):1769–9e. | ||
Cryptococcus Antigen Testing [webpage] Available from: http://www.ssi.dk/Diagnostik/DiagnostiskHaandbog/0-99/058.aspx. Accessed February 16, 2017. | ||
Helleberg M, Häggblom A, Sönnerborg A, Obel N. HIV care in the Swedish-Danish HIV cohort 1995–2010, closing the gaps. PLoS One. 2013;8(8): e72257. | ||
Seboxa T, Anemu S, Assefa A, Asefa A, Diro E. Cryptococcal meningitis in patients with acquired immuno-deficiency syndrome in preHAART era at Gondar College of Medical Sciences Hospital north-west Ethiopia. Ethiop Med J. 2010;48(3):237–241. | ||
Darras-joly C, Chevret S, Wolff M, et al. Cryptococcus neoformans infection in France: epidemiologic features and early prognostic parameters for 76 patients who were infected with human immunodeficiency virus. Clin Infect Dis. 1996;23(2):369–376. | ||
Katchanov J, von Kleist M, Arastéh K, Stocker H. “Time-to-amphotericin B” in cryptococcal meningitis in a European low-prevalence setting: analysis of diagnostic delays. QJM. 2014;107(10):799–803. | ||
Lohse N, Obel N, Kronborg G, et al. Declining risk of triple-class antiretroviral drug failure in Danish HIV-infected individuals. AIDS. 2005;19(8):815–822. | ||
Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. AIDS. 2007;21(16):2119–2129. | ||
Kisenge PR, Hawkins AT, Maro VP, et al. Low CD4 count plus coma predicts cryptococcal meningitis in Tanzania. BMC Infect Dis. 2007;7:39. | ||
Meya DB, Manabe YC, Castelnuovo B, et al. Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count < or =100 cells/microL who start HIV therapy in resource-limited settings. Clin Infect Dis. 2010;51(4):448–455. | ||
Mathiesen IHM, Knudsen JD, Gerstoft J, Cowan S, Benfield T. Outcome of HIV-1-associated cryptococcal meningitis, Denmark 1988–2008. Scand J Infect Dis. 2012;44(3):197–200. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.