Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Incidence and Predictors of Loss to Follow-Up Among Adults on Antiretroviral Therapy in South Gondar Governmental Hospitals, Ethiopia: Retrospective Cohort Study
Authors Zeleke S , Demis S , Eshetie Y, Kefale D , Tesfahun Y , Munye T , Kassaw A
Received 17 April 2023
Accepted for publication 15 June 2023
Published 22 June 2023 Volume 2023:16 Pages 1737—1748
DOI https://doi.org/10.2147/JMDH.S414194
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Shegaw Zeleke,1 Solomon Demis,2 Yeshiambaw Eshetie,1 Demewoz Kefale,3 Yohannes Tesfahun,4 Tigabu Munye,1 Amare Kassaw3
1Department of Adult Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 2Department of Maternity and Neonatal Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 3Department of Pediatrics and Child Health Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia; 4Department of Emergency and Critical Care Nursing, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Correspondence: Shegaw Zeleke, Email [email protected]
Background: Approximately 38.4 million adult people worldwide live with HIV, of which the majority live in Africa. In Ethiopia increasing the quality of life to HIV patients and preventing HIV transmission are challenging. Even though test-and-treat strategy is applied for early enrollment to ART, poor retention and loss to follow-up are hindering the care.
Objective: This study examined the incidence and predictors of loss to follow-up among adult HIV patients on ART in South Gondar governmental hospitals, September 11, 2017–September 10, 2022.
Methods: A multi-facility-based retrospective follow-up study was conducted. Study subjects were assigned using simple random sampling methods by their medical record numbers. The data were entered into EPI data version 3.0.2 and exported to STATA version 17 for analysis. The Kaplan–Meier failure function was employed to determine the overall failure estimates. Cox proportional hazard model was tailored for both bi-variable and multivariable. Variables at p-value < 0.05 with 95% CI were significantly associated with loss to follow-up.
Results: In this study, about 559 adult HIV survivors were included, and the response rate was 98%. The mean age and standard deviation (±SD) of study subjects were 36.6± 9.3 years. The incidence rate of loss to follow-up was 6.7 per 100 person-years (95% CI: 5.6, 8.1). Educational status [AHR: 1.68 (95% CI: 1.04, 2.72)], substance use [AHR: 2.38 (95% CI: 1.50, 3.75)], and ART adherence [AHR: 3.33 (95% CI: 1.38, 8.08)] were significant determinants to loss to follow-up.
Conclusion: In conclusion, the study finding reported that the incidence of loss to follow-up was low. HIV patients who did not have formal education, substance users, and poor ART adherence were at greater hazard of being lost to follow-up. In order to mitigate the rate of loss to follow-up, it is recommended to strengthen the available intervention modalities.
Keywords: HIV/AIDS, ART, lost follow-up, predictors, adults, Ethiopia
Introduction
Globally, human immunodeficiency virus is the major public health issue and burden.1 However, globally antiretroviral therapy is scaled-up for full preventive and therapeutic benefits against the virus.2–5 In 2015, the World Health Organization (WHO) endorsed the “treat-all policy”, in which all individuals who have HIV shall start ART as soon as the diagnosis is confirmed regardless of WHO clinical staging or CD4 cell status.3 Meanwhile, treatment starts as soon as possible, the drug gives good and long viral load decrement, restores and preserves immune function, improves the life of the HIV patient, and prevents transmissions.6
In people who are already on ART treatment, loss to follow-up (LTFU) is a major challenge for patient drug adherence.7 Many HIV patients are unduly exposed with mental health problems and substance use disorders aggravated by the doubts and anxiety related to COVID-19 pandemic.8 LTFU of patients on ART can result in serious consequences such as drug toxicity, treatment failure due to poor adherence, drug resistance, increased HIV/AIDS-associated diseases, death, and admissions.9,10
Retaining HIV patients through their life on ART treatment requires much collaboration among healthcare providers and patients. Once the patient is lost to follow-up, it is difficult to trace them due to limited resources and such patients cannot easily be found in most cases, as they have decided to stop their treatment.11 The incidence rate of LTFU is still high; and predictors of LTFU were CD4 count and viral load,12 underweight, health facilities, telephone contact, stigmatization, long waiting times,13,14 substance abuse, adherence, isoniazid prophylaxis, functional status, opportunistic infections, drug regimen, and male gender.15,16
Even though there have been a lot of modifications and changes regarding HIV treatment, there is a high incidence rate of LTFU across different parts of Ethiopia, and the magnitude of LTFU ranges from 3.7%17 to 26.6%.18 Although Ethiopia still has a high national HIV prevalence of 1.54%, the incidence and predictors of LTFU after initiation of ART are not well documented in many areas of Ethiopia.2 In our study setting (South Gondar Zone), adult HIV patients’ LTFU has not been well studied or documented. Thus research-based findings that avert LTFU in developing countries will maximize the management effects and adherence in an efficient way. Due to this reason, the researchers embarked on this study to investigate the incidence and predictors of loss to follow-up among adult HIV patients on ART in South Gondar governmental hospitals.
Methods
Study Design, Area, and Period
A multi-facility-based retrospective follow-up study was done in South Gondar Zone Governmental Hospitals between September 11, 2017 and September 10, 2022. South Gondar Zone is located in the northwest of Ethiopia, and its capital city is Debre Tabor. South Gondar zone has an estimated population of 2,051,738 based on the 2007 Ethiopian statistics report, of which 1,041,061 are men and 1,010,677 are women. In this zone, there are nine primary hospitals and one comprehensive specialized hospital. There are 6633 HIV/AIDS patients attending ART clinics in this zone, and among those 4011 HIV patients are attending those public hospitals. The data were collected from patient charts from September 12, 2022–October 11, 2022.
Sample Size Determination, Sampling Method, and Participants
Double population proportion formula was used for sample size calculation using Epi Info™ version 7 software, and considering the following assumptions: level of precision 5%, CI 95%, power 80%, the proportion of exposed (CD4<350) 39.75%,19 the proportion of non-exposed (CD4≥350) 28%,19 and assuming non-response rate of 10%. Hence, a sample size of 559 was computed with a 10% non-response rate included. All HIV-infected adults (age >15 years) who were registered at the South Gondar Zone governmental hospitals ART clinic from September 11, 2017–September 10, 2022 were eligible. Five hospitals were selected randomly, and adult HIV patients on ART were allocated proportionally. Then, study subjects were assigned using simple random sampling methods using their medical record numbers. Study subjects who had at least one ART follow-up visit were included to the study. Subjects with missed-registration of their ART initiation specific time and unavailability of baseline record data and transferred-in with incomplete baseline data were excluded from the study.
Variable Definitions and Data Collection Procedures
The dependent variable was a loss to follow-up and defined as missing ART refill for 3 months or longer from the last attendance for a refill and not yet classified as dead or transferred out.20 A patient was classified as being lost to follow-up if he/she developed the outcome (LTFU), and censored if he/she dies while on antiretroviral therapy or is transferred out to other health institutions after the beginning of the study or individuals on ART at the end of the study.
The predictor variables assessed were baseline socio-demographic factors (age, sex, religion, marital status, educational status, occupation status, family size, telephone contact, caregiver relationship, residence, and disclosure status), baseline clinical-related factors (WHO clinical stages, viral load, CD4 Level, hemoglobin level, body mass index, and functional status), and patients’ follow-up clinical and treatment-related characteristics (opportunistic infection, TB status, drug regimen, cotrimoxazole prophylaxis therapy (CPT), isoniazid (INH) prophylaxis therapy, hemoglobin level, viral load, ART drug adherence, and substance use).
Adherence was classified as follows: Good adherence: ≥95% adherence (missing only 1 out of 30 doses), fair adherence: 85–94% adherence (missing 2–4 doses out of 30), and poor adherence: less than 85% adherence (missing ≥5 doses out of 30).6
Functional measurement was as per WHO criteria: working (able to perform usual work inside or outside the home), ambulatory (able to perform the activity of daily living but not able to work), and bedridden (not able to perform the activity of daily living).15
Substance use was stated as any history of harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs.15
Five BSc nurse professionals collected the data from adult HIV patients' ART charts using a checklists designed based on the national standardized ART entry and follow-up form, which is now applied in ART clinics. Data quality was controlled by giving training to the data collectors (BSc nurses) and the supervisors about how the data are extracted based on the study objectives. The data collection tools/checklists were also pretested before the actual data collection period.
Data Processing and Analysis
Data were entered using Epi-Data version 3.0.2, and analysis was done using STATA version 17 statistical software. Data were cleaned and edited before analysis. Study subjects' characteristics were presented using mean or median, and standard deviation and also in frequency distribution for categorical data. The outcome of each subject was dichotomized into censored and lost to follow-up. The Kaplan–Meier failure estimate curve was used to determine the failure time after beginning of ART. Bivariate Cox proportional hazards regression model was tailored for individual illustrative variables. Furthermore, a variable with a p-value ≤0.2 in the bivariable analysis was fitted to the multivariable Cox proportional hazards regression model. Hazard ratio with its 95% CI and p-values <0.05 was used to declare its significance.
Ethical Consideration
Ethical approval was obtained from the Ethical Review Committee of Debre Tabor University. Since this study used an extraction of secondary data from survivors' card/chart, informed consent is waived. Confidentiality was maintained by not mentioning their names and other personal identifiers to the data collection tools.
Results
Socio-Demographic Characteristics of the Study Subjects
Of a total of 559 study participants, 548 were included in the final analysis, giving a response rate of 98%. The mean age (±SD) of study participants was 36.6±9.3 with the age range of 18–65 years. Moreover, about two-thirds (61.3%) of participants were females. Three-fourths (75.4%) of HIV patients were urban by residency, and the majority (83.4%) were Orthodox Christianity followers. In this study, 211 (38.5%) participants have college and above in their educational status, and most (84%) of the study subjects have revealed their HIV status (Table 1).
 |
Table 1 Baseline Socio-Demographic Characteristic of Adult HIV Patients on ART at South Gondar Zone Public Hospitals, Ethiopia, September 11, 2017–September 10, 2022 |
Baseline Adult HIV/AIDS Patients’ Clinical Characteristics
In this study, more than half (58.4%) of the study participants have a baseline viral load ≤1000 copies/mL. Just one-fourth (25.0%) of the study participants had baseline body mass index below <18.5 kg/m2 (underweight). About three-fourths (75.73%) of the study subjects had also a working functional status, and 331 (60.51%) of study subjects had <10 g/dL baseline hemoglobin level (Table 2).
 |
Table 2 Baseline Clinical Characteristics of HIV-Positive Adults on ART at South Gondar Zone Public Hospitals, Ethiopia, Sept 11, 2017–Sept 10, 2022 |
Adult HIV/AIDS Patients’ Follow-Up Characteristics
About 427 (77.9%) study subjects had current viral load ≤1000 copies/mL, and 39 (7.12%) of the study participants were also tuberculosis-positive. About 355 (64.8%) and 206 (37.6%) of study subjects were on CPT and IPT, respectively. More than half 302 (55.1%) of study participants had good adherence to ART drugs (Table 3).
 |
Table 3 Follow-Up Clinical and Treatment-Related Characteristics of Adult HIV Patients on ART at South Gondar Zone Public Hospitals, Ethiopia, September 11, 2017–September 10, 2022 |
Incidence of Loss to Follow-Up from ART
This study reported that the total follow-up time was 1,678.197 person-years observation with an incidence rate of 6.7 per 100 person-years (95% CI: 5.6, 8.1). The study participants were followed for a minimum of 0.25 years and a maximum of 5 years after initiation of ART with 4.98 years median follow-up time. During the five years follow-up period, 38 (6.93%) died, and the cumulative incidence of LTFU was 113 (20.62%), whereas the majority 370 (67.52%) of the study subjects were alive (Figure 1).
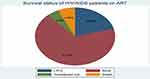 |
Figure 1 Cumulative incidence of adult HIV patients on ART at South Gondar Zone Public Hospitals, Ethiopia, Sept 11, 2017–Sept 10, 2022. |
In this study, LTFU was higher as the time to follow-up year increased. The incidence rate at 1, 2, 3, 4, and 5 years follow-up at 95% CI was 1.3% (0.61%, 2.7%), 3.4% (2.1%, 5.5%), 7.2% (4.9%, 10.5%), 23.4% (17.5%, 31.1%), and 25.5% (15%, 42.3%) per 100 person-years, respectively (Figure 2). The incidence density of LTFU in adult HIV patients on ART who use substance was 11.2/100 person-years, whereas for those not using substance it was 4.7/100 person-years (Figure 3).
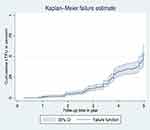 |
Figure 2 Overall cumulative probability of failure estimates among adult HIV patients on ART at South Gondar Zone Public Hospitals, Ethiopia, Sept 11, 2017–Sept 10, 2022. |
 |
Figure 3 Kaplan–Meier failure estimates by substance use among adult HIV patients on ART at South Gondar Zone Public Hospitals, Ethiopia, Sept 11, 2017–Sept 10, 2022. |
Predictors of Loss to Follow-Up Among Adult HIV Patients on ART
After fitting a bivariable Cox regression analysis model, ten predictor variables that have a p-value ≤0.2 were transported into multivariable Cox regression analysis, and variables such as educational status, substance use, and drug adherence level were significant determinants of loss to follow-up at 95% CI and 5% significance level.
In this study, for adult HIV patients on ART who have no formal education, the hazard ratio of LTFU is 1.68 times higher compared to those adults whose educational level was college and above [AHR = 1.68 (95% CI: 1.04, 2.72)]. Adult HIV patients on ART who had poor ART drug adherence were 3.33 times more at risk of loss to follow-up as compared to the cohort with good ART drug adherence [AHR: 3.33 (95% CI: 1.38, 8.08)]. Furthermore, patients who use substances were 2.38 times more at risk of loss to follow-up compared to those patients who do not use substances [AHR: 2.38 (95% CI: 1.50, 3.75)] (Table 4).
 |
Table 4 Bivariable and Multivariable Cox Regression Analysis for Predictors of LTFU Among Adult HIV Patients on ART at South Gondar Zone Public Hospitals, Ethiopia, Sept 11, 2017–Sept 10, 2022 |
Discussion
This study assessed the incidence and predictors of LTFU among adult HIV patients on ART in South Gondar Zone public hospitals, Ethiopia. The overall incidence rate of loss to follow up was 6.7 per 100 person-years. This finding is consistent with other studies conducted in North Shewa Zone,21 Gondar,22 Axum,16 Woldia,23 and Cameron,24 but the LTFU incidence density of this study is higher than in the studies done in Arba Minch,25 Debre Markos,26 and Southern Ethiopian public hospitals.27 Moreover, this study finding is lower than the study findings done in Gondar,15 Jigjiga town,18 Pawi Hospital,28 Kenya,29 Sub-Saharan Africa,30 and South‑Eastern Nigeria Hospital.31 Certainly, it is possible that this variation in incidence rate is caused by a variety of factors, including differences in setting, time variations, follow-up periods, health-seeking behaviors, socio-demographic characteristics, and the standardization of the implementation of ART services based on WHO guidelines. However, this study found a lower incidence rate compared to other reports listed below, maybe as a result of improved ART drug adherence, trace-back of adult HIV patients after LTFU, and earlier treatment initiation (test-start implementation approach since 2016 in Ethiopia).
Based on previous studies done in different parts of the world including Ethiopia, many socio-demographic factors were the risk factors to LTFU for adult HIV patients on ART. For instance, female sex,12 male sex,16,18,32 being jobless,15,19 age 15–28 years,19,28 rural residentce,19 non-disclosure of HIV status,19,33 and underweight (<18.5 kg/m2)15 were among the significant predictors of LTFU.
In this study, adult HIV patients who have no formal education were two times as likely to be lost to follow-up as compared to those adults whose educational level were college and above. This finding is congruent with studies done in Ethiopia.34,35 This is because those people who are uneducated may have difficulty understanding instructions and may not recognize the importance of ART drug adherence and complications related to discontinuation of ART drugs.36,37 Those with no formal education might also prefer to discontinue their medication, and turn to religion instead, such as holy water or Quran. In this regard, improving HIV patients’ knowledge could be an effective intervention for retaining and re-engaging HIV patients38.
In the previous studies, baseline follow-up clinical factors and treatment-related factors were considered more hazardous factors for LTFU, such as CD4 count <200 cells/mm3,12 CD4 count >200 cells/mL,5,15 viral load >1000 copies/mL, WHO clinical stage III and VI,5,19,28 WHO stage I and II,29 hemoglobin level <10 g/dL,39 not having ART adverse effect,5 and not receiving isoniazid prophylaxis therapy.15,28
In our study, substance abusers with HIV were two times more likely to suffer LTFU than were non-abusers. This finding is consistent with another study conducted in Ethiopia.15,34 It is because substance abuse causes negligence and decreases the likelihood of patients following up on their treatment.40 Another possible reason is that substance users do not fully engage in the HIV care continuum, have poor adherence to ART, and cannot follow a daily HIV treatment regimen, forgetting their drugs and follow-up time. Furthermore, substance abusers are more likely to expose themselves to risky sexual behaviors, and this might facilitate poor HIV/AIDS prognosis and subsequently prevent them from seeking HIV care services.41
In this study adult HIV patients who had poor ART drug adherence were three times more at risk of LTFU than were those who had good adherence. This finding is in support of studies done in Ethiopia,15 Nigeria,42 and Vietnam.43 This may be due to socio-demographic and clinical problems that can affect their adherence.44 The other possible reason might be, besides, as HIV treatment adherence is a key to staying healthy and to achieve appropriate viral suppression, HIV patients with poor drug adherence may worsen their problems and they lose the trust to the drug to be helpful which can result in them being lost to follow-up and they might turn to cultural beliefs or religious places instead.
Strength and Limitation
As this study relied on chart review, those without complete baseline data were excluded. Viral load, which is the key factor to ensure adherence and viral suppression, was included in the study; this is considered as a strength.
Conclusions
In this study area, loss to follow-up was low as compared to other previous research conducted in other settings of Ethiopia. Adult HIV patients not having formal education, substance users, and those with poor ART adherence level were significantly associated with loss to follow-up. Even if the density of LTFU is low as compared to other studies, still, it needs greater attention by ministry of health, regional and zonal heath service administrators, and clinicians who gave the direct service to retain adult HIV patients on follow-up. In order to mitigate the rate of LTFU, it is recommended to pay special attention to the risk groups and strengthen the available intervention modalities. Moreover, a future study should investigate strategies to reduce poor retention after ART initiation, improve ART medication adherence, and trace and re-engage individuals who have discontinued ART.
Abbreviations
AIDS, acquired immunodeficiency syndrome; ART, anti-retroviral therapy; HIV, human immunodeficiency virus; HR, hazard ratio; LTFU, loss to follow-up; WHO, World Health Organization.
Data Sharing Statement
The datasets used in this study are available from the corresponding author and can be accessible through reasonable request.
Ethics Approval and Consent to Participate
The research proposal was approved by Debre Tabor University research ethical committee. This study was conducted in accordance with the Declaration of Helsinki: study participants’ confidentiality was maintained; no personal identifiers were used in the data collection questionnaire/checklist, and codes were used in place of them.
Acknowledgments
The authors are grateful to the data collectors and study participants.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article and revising it and agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. Hønge BL, Jespersen S, Nordentoft PB, et al. Loss to follow-up occurs at all stages in the diagnostic and follow-up period among HIV-infected patients in Guinea-Bissau: a 7-year retrospective cohort study. BMJ Open. 2013;3(10):e003499. doi:10.1136/bmjopen-2013-003499
2. Alene KA, Elagali A, Barth DD, et al. Spatial codistribution of HIV, tuberculosis and malaria in Ethiopia. BMJ Global Health. 2022;7(2):e007599. doi:10.1136/bmjgh-2021-007599
3. World Health Organization. WHO Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV; 2015.
4. Ending A. Progress towards the 90–90–90 targets–global AIDS update. Geneva: Joint United Nations Programme on HIV. AIDS; 2017.
5. Mberi MN, Kuonza LR, Dube NM, et al. Determinants of loss to follow-up in patients on antiretroviral treatment, South Africa, 2004–2012: a cohort study. BMC Health Serv Res. 2015;15(1):1–11. doi:10.1186/s12913-015-0912-2
6. Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med. 2016;375(9):830–839. doi:10.1056/NEJMoa1600693
7. Ahmed I, Gugsa ST, Lemma S, et al. Predictors of loss to follow-up before HIV treatment initiation in Northwest Ethiopia: a case control study. BMC Public Health. 2013;13(1):1–9. doi:10.1186/1471-2458-13-867
8. Yao H, Chen J-H, Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi:10.1016/S2215-0366(20)30090-0
9. Assefa Y, Jerene D, Lulseged S, et al. Rapid scale-up of antiretroviral treatment in Ethiopia: successes and system-wide effects. PLoS Med. 2009;6(4):e1000056. doi:10.1371/journal.pmed.1000056
10. Assefa Y, Kiflie A, Tesfaye D, et al. Outcomes of antiretroviral treatment program in Ethiopia: retention of patients in care is a major challenge and varies across health facilities. BMC Health Serv Res. 2011;11:1–7. doi:10.1186/1472-6963-11-81
11. Wubshet M, Berhane Y, Worku A, et al. High loss to followup and early mortality create substantial reduction in patient retention at antiretroviral treatment program in north-west Ethiopia. Int Scholar Res Notices. 2012;2012:9.
12. Gerver SM, Chadborn TR, Ibrahim F, et al. High rate of loss to clinical follow up among African HIV-infected patients attending a London clinic: a retrospective analysis of a clinical cohort. J Int AIDS Soc. 2010;13(1):1–10. doi:10.1186/1758-2652-13-29
13. Opio D, Semitala FC, Kakeeto A, et al. Loss to follow-up and associated factors among adult people living with HIV at public health facilities in Wakiso district, Uganda: a retrospective cohort study. BMC Health Serv Res. 2019;19(1):1–10. doi:10.1186/s12913-019-4474-6
14. Kweyamba M, Buregyeya E, Kusiima J, et al. Loss to follow-up among HIV positive pregnant and lactating mothers on lifelong antiretroviral therapy for PMTCT in rural Uganda. Adv Public Health. 2018;2018:1–9. doi:10.1155/2018/7540587
15. Mekonnen N, Abdulkadir M, Shumetie E, et al. Incidence and predictors of loss to follow-up among HIV infected adults after initiation of first line anti-retroviral therapy at University of Gondar comprehensive specialized Hospital Northwest Ethiopia, 2018: retrospective follow up study. BMC Res Notes. 2019;12(1):1–7. doi:10.1186/s13104-019-4154-y
16. Tadesse K, Fisiha H. Predictors of loss to follow up of patients enrolled on antiretroviral therapy: a retrospective cohort study. J AIDS Clin Res. 2014;5(393):2.
17. Birhanu MY, Leshargie CT, Alebel A, et al. Incidence and predictors of loss to follow-up among HIV-positive adults in northwest Ethiopia: a retrospective cohort study. Trop Med Health. 2020;48(1):78. doi:10.1186/s41182-020-00266-z
18. Seifu W, Ali W, Meresa B. Predictors of loss to follow up among adult clients attending antiretroviral treatment at Karamara general hospital, Jigjiga town, Eastern Ethiopia, 2015: a retrospective cohort study. BMC Infect Dis. 2018;18(1):1–8. doi:10.1186/s12879-018-3188-4
19. Megerso A, Garoma S, Eticha T, et al. Predictors of loss to follow-up in antiretroviral treatment for adult patients in the Oromia region, Ethiopia. HIV/AIDS Res Palliat Care;2016. 83–92. doi:10.2147/HIV.S98137
20. World Health Organization. Retention in HIV programmes: defining the challenges and identifying solutions: meeting report, 13–15 September 2011; 2012.
21. Shiferaw WS, Belete AM, Adela A, et al. Incidence and predictors of loss to follow-up among adult HIV-infected patients taking antiretroviral therapy at North Shewa zone public Hospitals, Northeast Ethiopia: a retrospective follow-up study. Afr Health Sci. 2022;22(2):12–26. doi:10.4314/ahs.v22i2.3
22. Teshale AB, Tsegaye AT, Wolde HF, Price MA. Incidence and predictors of loss to follow up among adult HIV patients on antiretroviral therapy in University of Gondar Comprehensive Specialized Hospital: a competing risk regression modeling. PLoS One. 2020;15(1):e0227473. doi:10.1371/journal.pone.0227473
23. Dejen D, Jara D, Yeshanew F, et al. Attrition and its predictors among adults receiving first-line antiretroviral therapy in Woldia town public health facilities, Northeast Ethiopia: a retrospective cohort study. HIV/AIDS Res Palliat Care;2021. 445–454. doi:10.2147/HIV.S304657
24. Bekolo CE, Webster J, Batenganya M, et al. Trends in mortality and loss to follow-up in HIV care at the Nkongsamba Regional hospital, Cameroon. BMC Res Notes. 2013;6(1):1–16. doi:10.1186/1756-0500-6-512
25. Gebremichael MA, Gurara MK, Weldehawaryat HN, et al. Predictors of loss to follow-up among HIV-infected adults after initiation of the first-line antiretroviral therapy at Arba Minch General Hospital, Southern Ethiopia: a 5-year retrospective cohort study. Biomed Res Int. 2021;2021:1–12. doi:10.1155/2021/8659372
26. Birhanu MY, Leshargie CT, Alebel A, et al. Incidence and predictors of loss to follow-up among HIV-positive adults in northwest Ethiopia: a retrospective cohort study. Trop Med Health. 2020;48(1):1–10.
27. Dessu S, Mesele M, Habte A, et al. Time until loss to follow-up, incidence, and predictors among adults taking ART at public hospitals in Southern Ethiopia. HIV/AIDS Res Palliat Care. 2021;Volume 13:205–215. doi:10.2147/HIV.S296226
28. Assemie MA, Muchie KF, Ayele TA. Incidence and predictors of loss to follow up among HIV-infected adults at Pawi General Hospital, northwest Ethiopia: competing risk regression model. BMC Res Notes. 2018;11(1):1–6. doi:10.1186/s13104-018-3407-5
29. Saumu WM, Maleche-Obimbo E, Irimu G, et al. Predictors of loss to follow-up among children attending HIV clinic in a hospital in rural Kenya. Pan Afr Med J. 2019;32(1). doi:10.11604/pamj.2019.32.216.18310
30. Asiimwe SB, Kanyesigye M, Bwana B, et al. Predictors of dropout from care among HIV-infected patients initiating antiretroviral therapy at a public sector HIV treatment clinic in sub-Saharan Africa. BMC Infect Dis. 2015;16(1):1–10. doi:10.1186/s12879-016-1392-7
31. Eguzo K, Lawal A, Umezurike C, et al. Predictors of loss to follow‑up among HIV‑infected patients in a rural South‑Eastern Nigeria Hospital: a 5‑year Retrospective Cohort Study. Ann Med Health Sci Res. 2015;5(6):373–378. doi:10.4103/2141-9248.177988
32. Nuwagira E, Lumori BAE, Muhindo R, et al. Incidence and predictors of early loss to follow up among patients initiated on protease inhibitor-based second-line antiretroviral therapy in southwestern Uganda. AIDS Res Ther. 2021;18(1):7. doi:10.1186/s12981-021-00331-5
33. Mutanga JN, Mutembo S, Ezeamama AE, et al. Predictors of loss to follow-up among children on long-term antiretroviral therapy in Zambia (2003–2015). BMC Public Health. 2019;19(1):1–13. doi:10.1186/s12889-019-7374-0
34. Gesesew HA, Ward P, Hajito KW, et al. Discontinuation from antiretroviral therapy: a continuing challenge among adults in HIV care in Ethiopia: a systematic review and meta-analysis. PLoS One. 2017;12(1):e0169651. doi:10.1371/journal.pone.0169651
35. Valenzuela C, Ugarte-Gil C, Paz J, et al. HIV stigma as a barrier to retention in HIV care at a general hospital in Lima, Peru: a case–control study. AIDS Behav. 2015;19:235–245. doi:10.1007/s10461-014-0908-7
36. Jimmy B, Jose J. Patient medication adherence: measures in daily practice. Oman Med J. 2011;26(3):155. doi:10.5001/omj.2011.38
37. Praska JL, Kripalani S, Seright AL, et al. Identifying and assisting low-literacy patients with medication use: a survey of community pharmacies. Ann Pharmacother. 2005;39(9):1441–1445. doi:10.1345/aph.1G094
38. Barragán M, Hicks G, Williams MV, et al. Low health literacy is associated with HIV test acceptance. J Gen Intern Med. 2005;20(5):422–425. doi:10.1111/j.1525-1497.2005.40128.x
39. Nuwagira E, Amir A, Muzoora C. Predictors of Loss To FollOw up among HIV infected patients initiated on second line ART in Southwestern Uganda. HIV Curr Res. 2018;3(2):1–5.
40. Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr. 2006;43(4):411. doi:10.1097/01.qai.0000243121.44659.a4
41. Doku D. Substance use and risky sexual behaviours among sexually experienced Ghanaian youth. BMC Public Health. 2012;12:1–7. doi:10.1186/1471-2458-12-571
42. Agbaji O, Abah I, Falang K, et al. Treatment discontinuation in adult HIV-infected patients on first-line antiretroviral therapy in Nigeria. Curr HIV Res. 2015;13(3):184–192. doi:10.2174/1570162X1303150506181945
43. Tran DA, Ngo AD, Shakeshaft A, et al. Trends in and determinants of loss to follow up and early mortality in a rapid expansion of the antiretroviral treatment program in Vietnam: findings from 13 outpatient clinics. PLoS One. 2013;8(9):e73181. doi:10.1371/journal.pone.0073181
44. Fonsah JY, Njamnshi AK, Kouanfack C, et al. Adherence to antiretroviral therapy (ART) in Yaoundé-Cameroon: association with opportunistic infections, depression, ART regimen and side effects. PLoS One. 2017;12(1):e0170893. doi:10.1371/journal.pone.0170893
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
