Back to Journals » Advances in Medical Education and Practice » Volume 10
Improving knowledge, attitudes, and practice of nurses in medication administration through enteral feeding tubes by clinical pharmacists: a case–control study
Authors Hossaini Alhashemi S, Ghorbani R, Vazin A
Received 12 February 2019
Accepted for publication 3 June 2019
Published 9 July 2019 Volume 2019:10 Pages 493—500
DOI https://doi.org/10.2147/AMEP.S203680
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Samira Hossaini Alhashemi, Raana Ghorbani, Afsaneh Vazin
Department of Clinical Pharmacy, Faculty of Pharmacy, Shiraz University of Medical Sciences, Shiraz, Iran
Purpose: Administering drugs and food to patients with swallowing disabilities via enteral tubes requires special skills. This task is a nursing duty and vital to ensure that they do this safely. An integrated program training nurses by a clinical pharmacist is likely to result in improved quality of oral drug administration via enteral feeding tubes. This quantitative study was undertaken to determine the efficacy of a clinical pharmacist educational program for improving nurses’ knowledge, attitudes, and practice (KAP) concerning administrating medication via feeding tubes.
Methods: This case–control study was performed to evaluate KAP of intensive-care nurses with regard to drug delivery through enteral feeding tubes before and after their training program. A questionnaire focusing on nurses’ KAP was prepared by a clinical pharmacist and reviewed by 18 nurses for its reliability. Then, an educational program was designed for the case group. Two months later, nurses’ KAP in the case and control groups were reevaluated. Nurses’ practice regarding drug administration through feeding tube was observed three times.
Results: This study was carried out with 82 nurses working in six intensive-care units in two major training hospitals in Shiraz, Iran. The overall knowledge of nurses increased significantly after the training program in the case group, with adequate awareness regarding solid dosage–form crushing increasing from 14% to 63.2% (P˂0.001), tube flushing and drug dilution from 32.6% to 81.6% (P˂0.001), and knowledge about mixing crushed drugs through a feeding tube from 23.3% to 55.3% (P˂0.001). On the contrary, there was no change in the control group. After intervention, nurses’ attitudes in the case group had changed significantly, and 50% of them consulted with pharmacists regarding drug administration.
Conclusion: An in-service education program by clinical pharmacists can lead to substantial improvements in administration of drugs via enteral feeding tubes.
Keywords: clinical pharmacy, drug administration, education, enteral feeding tube, KAP, nurses
Introduction
Enteral feeding is recommended for malnourished patients who are unable to consume an adequate or safe oral diet. It is beneficial for critically ill or postoperative patients, as it can provide cost-effective care, which can improve gastrointestinal mucosal structure and function by preventing gut atrophy.1 Although physicians, pharmacists, and nurses are generally responsible for administration of medication via enteral tubes, this is principally a nursing duty. To utilize digestive tubes appropriately, one needs to have a number of skills, including verification of tube placement, tube flushing, and characteristics of different drug-dosage forms by considering the associated complications, such as catheter obstruction and other side effects.2 If medications are not given appropriately via the enteral route, it may result in harmful consequences. These consequences include tube occlusion, diarrhea, aspiration pneumonia, drug inefficiency, drug side effects, and even mortality,3 all of which can lead to an increase in patient usage of hospital equipment and also length of stay, resulting in an increase in costs of the health-care system. Therefore, this demands a more efficient performance by the nursing staff, in order to achieve optimum results.
Crushing some dosage forms like controlled-release and enteric-coated tablets is not appropriate. Grinding these types of tablets not only changes the medication’s pharmacokinetics and pharmacological action but might also result in toxicity, treatment failure, and tube obstruction.4
Health-care staff knowledge, attitudes, and practice (KAP) regarding enteral medication administration is essential to reduce patient morbidity and mortality.2 Surveys suggest that hands-on practice differs significantly from guidelines, and several common practices could interfere with appropriate medication delivery. For example, previous surveys have suggested that only 5%–43% of practitioners use flush tubes before or between medications, only 32%–51% administer drugs separately from one another, only 44%–64% dilute liquid medication, and only 75%–85% avoid crushing modified-release dosage forms.3–6
A previous study in the intensive care units of Nemazee Hospital showed disparities between nurses’ knowledge, self-reported practice, and proper performance in drug administration through an enteral feeding tube.7 Therefore, this quantitative descriptive study was conducted to determine the efficacy of a clinical pharmacist educational program to improve KAP of ICU nurses, concerning medication administration via feeding tube.
Methods
This case–control study was performed to evaluate KAP of ICU nurses concerning drug delivery through enteral feeding tubes before and after a training program in Nemazee and Shahid Faghihi hospitals.
The study population included all 82 nurses working in six different ICUs at two major training hospitals affiliated with Shiraz University of Medical Sciences (SUMS), the main referral centers for patients in southern Iran, from March 2014 to May 2016. Participant collaboration was voluntary, and they were assured about the anonymity and confidentiality of their data. Then, all participants provided written consent to participate in the study, having been ensured of the confidentiality of the presented information. The local ethics committee approved the written consent and study protocol (code EC-9388–8458).
A 25-question multiple-choice researcher-constructed questionnaire was prepared by reviewing the literature.2,8–11 The questionnaire focused on the knowledge and attitudes of nurses. Questions relating to nurses’ knowledge consisted of medication preparation (two items), tube flushing and drug dilution (two items), drug–food or drug–drug interaction (three items), and selection of correct dosage forms (five items). Questions regarding nurses’ self-reported practice included correct tube position, medication preparation, tube flushing, drug-dosage forms, factors that obstruct enteral tubes, and drug–food interactions. Questions concerning attitudes were on having a reliable person for inquiries about medication-administration problems (one item), ways to improve the quality of medication-administration services (one item) and factors important to the nurses in choosing the volume of water used for the patient (one item).
The questionnaire was reviewed by 18 ICU nurses to test its reliability. There was a 2-week interval between the test and retest. Reliability testing revealed Cronbach’s α of 0.79 for knowledge questions and 0.68 for practice questions. Some modifications were made to the questionnaire based on feedback from nurses. The final questionnaire required 20 minutes to complete. Questionnaires were completed by the case and control groups before the educational program.
Our checklist was developed to evaluate nurses’ practice of drug administration via enteral feeding tubes based on direct observation. This had three parts. In the first part, demographic information about patients and their medications was collected. In the second part, the investigator (an educated pharmacist) wrote his observations about medication administration through enteral feeding tubes by nurses, and the third part was developed to evaluate nurses’ practices regarding drug administration via enteral feeding tubes based on direct observation. Criteria selected for the checklist were also extracted from an extensive literature review. The third part of the checklist consisted of 22 items (14 yes/no questions and six multiple-choice questions) that were divided into different categories, and took about 15 minutes to completes. These categories included medication preparation (how nurses prepare and administer drugs, seven items), drug–food and drug–drug interaction (three items), tube flushing and drug dilution (four items), safety considerations in drug administration via enteral feeding tubes (one item), how nurses open occluded tubes (two items), how to determine the correct tube position (one item), type of liquid used for tube flushing and drug dilution (two items), crushing unsuitable drugs (one item) and patient restrictions in consumption of liquid (one item). Nurse practices were observed three times to remove some parameters, affecting nurse practices.
Based on the results, an educational program was designed for the case group by a clinical pharmacist (a leading author), including preparing an evidence-based booklet and classes for case-group nurses. After each training session, a list of drugs that were not to be crushed and work instructions were given to the participating nurses.12,13 Nurses in the control group did not receive any education program or booklet. Two months later, KAP of the nurses were reevaluated using the same questionnaire. SPSS version 18 was used for data analysis. Independent-sample t-tests were used to compare demographic data between two groups. For comparison of mean scores, paired t-tests weres used. Percentages of nurses with correct answers before and after the educational program were compared in each group by McNemar’s test. P<0.05 was considered statistically significant.
Results
During the preintervention phase of this study, 43 and 39 nurses participated in the case and control groups, respectively. There was no significant difference regarding demographic information between the two groups (P>0.05). The mean age of nurses was 32 years, and 53 (64.6%) were women. The vast majority of participants in both groups had a bachelor’s degree in nursing (86.6%). Additionally, participants’ mean experience in an ICU and as a nurse was 2 and 5 years, respectively. Table 1 shows the characteristics of the participants. The questionnaire and checklist could be found in the supplementary materials.
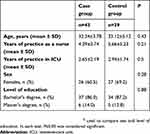 |
Table 1 Demographic information of nurses in the case and control groups at the commencement of the study |
During the postintervention phase, 38 nurses in the case group and 39 in the control group participated in this study. Five nurses in the case group could not participate in the training programs due to maternity leave, and hence were excluded.
The relationship between sex and level of education in both phases of the study was evaluated. There was no relationship between demographic information of the nurses and knowledge in either phase (P>0.05). Mean scores of nurses’ knowledge and practice in both groups before clinical pharmacist intervention were compared. Mean scores for nurses’ baseline knowledge between the groups was not significantly different, except in selecting the best dosage forms, which was significantly better in the case group (P˂0.05).
Groups were compared with each other before and after pharmacist intervention regarding the main domains in this study. Mean scores for nurses’ knowledge in each domain were compared (Table 2). Mean scores increased significantly after training program in the case group: adequate awareness regarding solid dosage–form crushing from 4.49±1.03 to 7.26±0.68 (P˂0.001), tube flushing and drug dilution from 1.12±0.73 to 1.9±0.311 (P˂0.001), and knowledge about mixing crushed drugs through feeding tubes from 1.00±0.845 to 2.65±0.48 (p˂0.001). On the contrary, there was no significant change in the control group.
 |
Table 2 Scores of nurses with acceptable knowledge in different domains in the case and control groups before and after clinical pharmacist intervention |
Table 2 shows numbers and percentages of nurses with correct answers concerning different knowledge domains. In contrast to the control group, the percentage of nurses with acceptable knowledge increased after the training program in the case group.
Mean scores and percentages of nurses with acceptable practice regarding self-report or researcher observations was compared between the two groups (Tables 3 and 4). As demonstrated in Table 3, mean scores for nurses’ practice regarding their reports about different domains increased significantly after the training program in the case group: adequate practice regarding solid dosage–form crushing from 1.744±1.311 to 4.947±1.723 (P˂0.001), tube flushing and drug dilution from 5.163±1.632 to 7.342±0.781 (P˂0.001), mixing crushed drugs through feeding tubes onverted from 3.070±1.653 to 5.947±1.355 (P˂0.001), and practice regarding verification of he feeding tube position onverted from 7.62±1.865 to 16.474±2.06 (P˂0.001). However, there was no significant change in the control group.
 |
Table 3 Scores of nurses with acceptable practice in different domains at pre- and postintervention in the case and control groups |
 |
Table 4 Scores of nurses with acceptable practice regarding researcher observation |
Nurses’ attitudes regarding three parameters were evaluated. Answers to who is the first person to ask questions of before drug administration via feeding tubes were significantly different between the two groups. In the preintervention phase, 15.8% of the case group selected their supervisors and 59.0% of the control group selected physicians. However, after intervention, nurses’ attitudes in the case group changed significantly, and 50.0% of them selected pharmacists as the first person to consult about drug administration (P˂0.001). Almost all nurses selected the overall condition of a patient when making decisions about the volume of water with which to flush the tube in both groups. In addition, nurses in both groups reported that increased collaboration between nurses and pharmacists could improve practice.
Discussion
Our study attained desirable results in nurses' KAP with regard to drug administration via enteral tubes after the training program, as mean scores on knowledge and practice significantly increased in the case group in comparison with the control group. For critically ill patients who cannot consume or have an oral diet, finding ways to administer drugs through the enteral feeding tube presents a challenge. Although administration of medication via enteral tube is specifically a nursing responsibility, they had limited baseline knowledge about pharmaceutical form, drug dosage, or interaction.4,5,10,14
Poor knowledge about the different codes used by drug companies and consequences of crushing drugs can result in unpredictable blood levels, in addition to an increased risk of catheter obstruction.3 Therefore, alternative administration routes have to be selected to deliver each drug to its specific sites correctly. We found that <20% of the participants in this study had adequate awareness regarding solid dosage–form crushing before the intervention program. As in previous surveys, when pharmacists promoted nurses’ knowledge, it resulted in a reduced percentage of medications being crushed.3,4,15 Inadequate awareness regarding medication-dosage forms might be related to flawed academic education, in particular medication-administration techniques.16 On the other hand, lack of sufficient information in the literature and data from manufacturers has led to the usage of empirical recommendations.17
Verifying the feeding tube position before any procedure is critical to prevent pharmacokinetic alteration of the prescribed drug and future complications, such as respiratory aspiration.18 Various methods are available to check nasogastric tube location, such as pH values that aspirate from the feeding catheter, auscultation, and radiography. Although radiography is the gold standard, its usage is limited, due to radiographic exposure and additional expenses.19 Since auscultation is an unreliable method,20 the National Patient Safety Agency in the UK and the American Association of Critical Care Nurses have banned this method.2 Testing aspirated pH and its color is an acceptable method to confirm tube location if the patient is not taking pH-altering agents.21 In this study, only 32.6% of nurses had acceptable practices regarding verifying feeding tube position before the intervention, after which this figure was 68.4% (P˂0.001).
Feeding tubes tend to clog because of short intervals between drug and meal administration. Mixing drugs through an enteral feeding tube due to lack of time not only changes therapeutic drug effects but also increases the risks of chemical inconsistency. Therefore, tubes should be flushed before and after drug administration with at least 15 mL water and drugs administered separately to prevent any possible interaction with food or tube obstruction.22,23 In the current survey, only 23.3% of nurses had acceptable knowledge on this topic before the intervention, after which this figure was 55.3%.
Nurses need the foremost accessible source of information to improve their practice. In a previous study in our ICUs at Nemazee Hospital, it was shown that nurses’ attitudes toward medication administration via an enteral tube were inappropriate: 43.1% hought that the physician was the best person to answer their questions and 34.1% believed that the pharmacist was the best option.7 Belknap et al showed that the main source of information for 56.9% of nurses was personal experience and that 21.7% of them consulted with their coworkers.4 In our study, nurse attitudes in the case group changed significantly, and half selected pharmacists as the first person to consult about drug administration.
Mean scores and percentages of nurses with acceptable practice regarding researcher observations was significantly improved in the control group. Training how to dilute medication is an important aspect, and tap water is not appropriate to prepare prescriptions, due to contamination.22 In addition, leaving drugs in purified water or saline for long periods till dissolved might expose medication to environmental conditions, altering chemical structure due to hydrolyzation in humid sites.17 The raining program led to improved nurse practices — from 9.3% to 52.6% — in the drug-dilution domain (P<0.001) regarding researcher observation. In 2011, a survey was conducted using a random sample of acute-care nurses at two large metropolitan hospitals in Melbourne, Australia. A majority reported administering enteric‐coated and slow- or extended-release forms of medication, and giving solid forms of medication when liquid form was available. Nearly all (96%) reported flushing a tube after giving medication, 28% before, and 12% always flushed between each medication.2 The education program by the clinical pharmacist significantly improved nurses’ knowledge in all features, including correct dosage-form selection, solid dosage–form crushing, tube flushing, and drug–drug/food interactions. This increased knowledge was consistent with previous findings.9,10,24
Advantages of the current study were having a control group and a logical time interval between the two phases of the study to reduce time trends.10,24,25 In contrast to previous research,2,3,17,26,27 this study not only depended on self-report but also assessed nurse practices through concealed observation. This might have helped to reduce potential bias and to show the fact that there is a theory–practice gap due to nurse stress in applying immediate care to patients in ICUs.17The main limitation in our study was the small number of nurses who participated in the surveys. Nevertheless, in comparison with findings in other settings, where it was reported that in addition to acute-care nurses,9,10 even community pharmacists28 had poor knowledge on correct medication administration via enteral feeding tubes, our results can be generalized in different health-care settings. Finally, patient morbidity and mortality should be measured as clinical end points in future studies.
Implications for practice
This study provides insight into improvements in KAP of nurses working in an ICU before and after education regarding drug administration through a nasogastric tube. The current study revised the need for regular in-service training in order to strengthen drug administration via a nasogastric tube. The study also highlights the importance of regular mandatory teaching sessions, continuous ward visits, and institutional policy changes to minimize medication errors while administrating drugs though nasogastric feeding tubes.
Conclusion
Medication errors through feeding catheters due to insufficient nurse knowledge could have a negative impression on patient safety. An in-service education program delivered by a clinical pharmacist led to substantial improvement in administration of drugs via enteral feeding tubes. Clinical pharmacists should collaborate with physicians and nurses in regular mandatory teaching sessions, continuous ward visits, and institutional policy changes to ensure that best practice is followed.
Acknowledgments
The authors wish to thank Mr H Argasi at the Research Consultation Center (RCC) of Shiraz University of Medical Sciences for his invaluable assistance in editing this manuscript. This study was a part of Raana Ghorbani's PharmD thesis at Shiraz University of Medical Sciences (thesis grant 93-01-05-8458). The authors thank all nurses who contributed to this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? systematic review of the literature. Nutrition. 2004;20(10):843–848. doi:10.1016/j.nut.2004.06.003
2. Phillips NM, Endacott R. Medication administration via enteral tubes: a survey of nurses’ practices. J Adv Nurs. 2011;67(12):2586–2592. doi:10.1111/j.1365-2648.2011.05688.x
3. Seifert CF, Johnston BA. A nationwide survey of long-term care facilities to determine the characteristics of medication administration through enteral feeding catheters. Nutr Clin Pract. 2005;20(3):354–362. doi:10.1177/0115426505020003354
4. Belknap DC, Seifert C, Petermann M. Administration of medications through enteral feeding catheters. Am J Crit Care. 1997;6(5):382–392.
5. Schmieding NJ, Waldman RC. Nasogastric tube feeding and medication administration: a survey of nursing practices. Gastroenterol Nurs. 1997;20(4):118–124.
6. Seifert CF, Johnston BA, Rojas-Fernandez C. Drug administration through enteral feeding catheters. Am J Health Syst Pharm. 2002;59(4):378–379. doi:10.1093/ajhp/59.4.378
7. Khani J, Vazin A, Shafiekhani M. Evaluating knowledge, attitude and practice of intensive care unit nurses in administering medications via enteral tubes. Trends Pharm Sci. 2016;2(3):195–204.
8. Clarke S. Drug administration via nasogastric tube. Paediatr Nurs. 2008;20(7):32.
9. Dashti-Khavidaki S, Badri S, Eftekharzadeh S-Z, Keshtkar A, Khalili H. The role of clinical pharmacist to improve medication administration through enteral feeding tubes by nurses. Int J Clin Pharm. 2012;34(5):757–764. doi:10.1007/s11096-012-9673-8
10. Hanssens Y, Woods D, Alsulaiti A, Adheir F, Al-Meer N, Obaidan N. Improving oral medicine administration in patients with swallowing problems and feeding tubes. Ann Pharmacother. 2006;40(12):2142–2147. doi:10.1345/aph.1H342
11. Phillips NM, Nay R. Nursing administration of medication via enteral tubes in adults: a systematic review. Int J Evid Based Healthc. 2007;5(3):324–353. doi:10.1111/j.1479-6988.2007.00072.x
12. Bourgault AM, Ipe L, Weaver J, Swartz S, O’Dea PJ. Development of evidence-based guidelines and critical care nurses’ knowledge of enteral feeding. Crit Care Nurse. 2007;27(4):17–29.
13. Gilbar PJ. A guide to enteral drug administration in palliative care. J Pain Symptom Manage. 1999;17(3):197–207.
14. Naysmith MR, Nicholson J. Nasogastric drug administration. Prof Nurse. 1998;13(7):424–427.
15. Stechmiller J, Treloar D, Derrico D, Yarandi H, Guin P. Interruption of enteral feedings in head injured patients. J Neurosurg Nurs. 1994;26(4):224–229. doi:10.1097/01376517-199408000-00006
16. Adhikari R, Tocher J, Smith P, Corcoran J, MacArthur J. A multi-disciplinary approach to medication safety and the implication for nursing education and practice. Nurse Educ Today. 2014;34(2):185–190. doi:10.1016/j.nedt.2013.10.008.
17. Mota MLS, Barbosa IV, Studart RMB, Melo EM, Lima FET, Mariano FA. Evaluation of intensivist-nurses knowledge concerning medication administration through nasogastric and enteral tubes. Rev Lat Am Enfermagem. 2010;18(5):888–894.
18. Ellett MLC. Important facts about intestinal feeding tube placement. Gastroenterol Nurs. 2006;29(2):112–124.
19. Metheny NA, Titler MG. Assessing placement of feeding tubes. Am J Nurs. 2001;101(5):36–45.
20. Boeykens K, Steeman E, Duysburgh I. Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud. 2014;51(11):1427–1433. doi:10.1016/j.ijnurstu.2014.03.004
21. Metheny N, Williams P, Wiersema L, Wehrle MA, Eisenberg P, McSweeney M. Effectiveness of pH measurements in predicting feeding tube placement. Nurs Res. 1988;38(5):280–285.
22. Bankhead R, Boullata J, Brantley S, et al. ASPEN enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33(2):122–167. doi:10.1177/0148607108330314
23. Kohn-Keeth C. How to keep feeding tubes flowing freely. Nursing. 2000;30(3):58–59.
24. Van den Bemt P, Cusell M, Overbeeke P, et al. Quality improvement of oral medication administration in patients with enteral feeding tubes. Qual Saf Health Care. 2006;15(1):44–47. doi:10.1136/qshc.2004.013524
25. Idzinga J, De Jong A, Van Den Bemt P. The effect of an intervention aimed at reducing errors when administering medication through enteral feeding tubes in an institution for individuals with intellectual disability. J Intellect Disabil Res. 2009;53(11):932–938. doi:10.1111/j.1365-2788.2009.01212.x
26. Gupta B, Agrawal P, Soni KD, et al. Enteral nutrition practices in the intensive care unit: understanding of nursing practices and perspectives. J Anaesthesiol Clin Pharmacol. 2012;28(1):41. doi:10.4103/0970-9185.92433
27. Teresi ME, Morgan DE. Attitudes of Healthcare Professionals toward Patient Counseling on Drug-Nutrient Interactions. Thousand Oaks, CA: Sage; 1994.
28. Joos E, Verbeke S, Mehuys E, et al. Medication administration via enteral feeding tube: a survey of pharmacists’ knowledge. Int J Clin Pharm. 2016;38(1):10–15. doi:10.1007/s11096-015-0196-y
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
