Back to Journals » Neuropsychiatric Disease and Treatment » Volume 16
Improvement of Negative Symptoms in Schizophrenia with Paliperidone Palmitate 1-Month and 3-Month Long-Acting Injectables: Results from a Phase 3 Non-Inferiority Study
Authors Gopal S , Gogate J, Pungor K , Kim E , Singh A , Mathews M
Received 7 August 2019
Accepted for publication 4 January 2020
Published 6 March 2020 Volume 2020:16 Pages 681—690
DOI https://doi.org/10.2147/NDT.S226296
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Srihari Gopal,1 Jagadish Gogate,1 Katalin Pungor,2 Edward Kim,3 Arun Singh,1 Maju Mathews1
1Janssen Research and Development, LLC, Titusville, NJ, USA; 2Medical Affairs, EMEA, Janssen-Cilag, Neuss, Germany; 3Janssen Scientific Affairs, Janssen Pharmaceuticals, Titusville, NJ, USA
Correspondence: Srihari Gopal
Janssen Research and Development, LLC, 1125 Trenton Harbourton Road, Titusville, NJ 08560, USA
Email [email protected]
Background: Negative symptoms in schizophrenia are associated with impairments in social and cognitive functioning leading to substantial long-term disability. Available antipsychotic treatments have demonstrated only modest benefit in the improvement of negative symptoms.
Objective: To compare improvements in negative symptoms among patients treated with paliperidone palmitate 3-month (PP3M) or paliperidone palmitate 1-month (PP1M) long-acting injectable (LAI) formulations.
Methods: Data from a randomized double-blind (DB), phase-3, non-inferiority study in patients with schizophrenia were analyzed. Following screening, patients entered a 17-week open-label (OL) phase to receive flexibly dosed PP1M followed by a 48-week DB phase where patients were randomized (1:1) to receive either PP1M or PP3M. Positive and Negative Syndrome Scale (PANSS) total scores with emphasis on 7-item negative subscale scores for PP1M vs PP3M were assessed.
Results: Of 1429 patients enrolled, 1016 were randomized to receive PP3M (n=504) or PP1M (n=512). At baseline, mean (SD) PANSS negative subscale was 23.2 (4.60) and negative symptom factor score was 22.3 (4.87), indicating moderate-to-severe negative symptoms. Negative subscale and symptoms factor scores showed continuous improvements throughout OL (15.9 [4.99]) and DB (14.9 [4.81]) phases. Mean (SD) changes from DB baseline in the PANSS negative subscale score were comparable between PP1M (– 1.4 [3.67]) and PP3M (– 1.4 [3.63]) treatment groups.
Conclusion: Treatment with PP3M or PP1M demonstrated comparable improvement in negative symptoms in patients with moderate-to-severe negative symptoms and in patients with prominent negative symptoms. Long-term treatment with PP3M demonstrated benefit, suggesting that continuous antipsychotic medication treatment for > 1 year is needed to achieve greater benefit for negative symptoms.
Trial Registration: ClinicalTrials.gov Identifier: NCT01515423.
Keywords: negative symptoms, paliperidone palmitate 3-month formulation, paliperidone palmitate 1-month formulation
Introduction
Negative symptoms are among the primary contributors of disability in schizophrenia owing to impairments in cognitive functioning and inability to perform day-to-day functional tasks.1 Negative symptoms are intrinsic to schizophrenia and may persist for long time periods; resolution of negative symptoms has been identified as a central prerequisite for functional recovery.2 Limited cognitive abilities, such as compromised mental flexibility and inability to pay attention, and social withdrawal, are closely related to negative symptoms that impact real-world functioning in patients with schizophrenia.3,4 The relationship between negative symptoms and cognitive performance is not fully understood. Negative symptoms may overlap with cognitive symptoms, and efforts to identify, define and measure negative symptoms and to differentiate them from other symptom domains and establish effective treatments, are underway.2,5 While antipsychotic treatments have demonstrated substantial benefit for positive schizophrenia symptoms, effective treatment outcomes for negative symptoms have proven challenging. Therefore, a focus on finding pharmacological treatments or delivery systems that could favorably influence negative symptoms is gaining impetus.2,6 Treatment of negative symptoms is emerging as a key assessment in the design and conduct of clinical studies of antipsychotic therapies.6 Second generation antipsychotics are generally acknowledged as having greater ability to improve negative symptoms compared to first-generation antipsychotics.7 The main issue, however, is that the effect sizes seen with second-generation antipsychotics have generally been too small to be of clinical relevance (approximately −0.5 points standardized mean difference).7
The National Institute of Mental Health Measurement and Treatment Research to Improve Cognition in Schizophrenia (NIMH-MATRICS) consensus panel has defined five-negative symptoms: blunted affect (diminished facial and emotional expression), alogia (decrease in verbal output or verbal expressiveness), asociality (lack of involvement in social relationships of various kinds), avolition (a subjective reduction in interests, desires, and goals and a behavioral reduction of self-initiated and purposeful acts), and anhedonia (inability to experience pleasure from positive stimuli).8 Several validated assessment tools are available for clinicians to identify the severity of negative symptoms and systematically evaluate symptom improvement along with treatment response in patients with schizophrenia, including the Brief Negative Symptom Scale (BNSS) and Positive and Negative Syndrome Scale (PANSS). The 30-item PANSS scale is the most widely used instrument for measuring severe psychopathology in schizophrenia9–11 and has been validated to standardize positive and negative symptom assessment and aid clinicians to evaluate, in comparison, positive and negative symptoms and general illness severity.10,12 PANSS has been used in various studies to evaluate treatment effects on symptoms including moderate/severe negative symptoms of schizophrenia.13,14 Furthermore, the negative subscale of the PANSS was found to have adequate psychometric properties and that each of the subscales of the PANSS formed independent constructs.6,15
Appropriate management of negative symptoms is a critical unmet need, primarily because the functional impairment due to negative symptoms cannot be appropriately addressed by treating positive symptoms alone.2 With the use of LAIs, additional improvements in negative symptoms may be possible as compared with oral therapies. Results of a large, double-blind, phase 3 study previously demonstrated that treatment with PP3M is non-inferior to PP1M in terms of efficacy for preventing relapse in clinically stable patients with schizophrenia over a 48-week period.16 In this post-hoc analysis, PANSS data from the study were examined to evaluate the potential benefits of PP1M and PP3M for negative symptoms. Since this was the longest available dataset where negative symptoms were measured longitudinally in a controlled fashion, this study was ideal to analyze the long-term effects of LAIs on these symptoms. We present data in this analysis showing that improvements in negative symptoms are seen gradually and take longer to improve compared to positive symptoms.
Methods
Study Design and Participants
This post-hoc analysis was performed on data from the 48-week, DB, parallel-group, multicenter, phase 3 non-inferiority study of PP3M vs PP1M in patients with schizophrenia, details of which are published.16 Briefly, patients (men and women aged 18–70 years, inclusive) diagnosed with schizophrenia (by Diagnostic and Statistical Manual of Mental Disorders; Fourth Edition, Text Revision [DSM-IV-TR] criteria) for at least 1 year before screening, PANSS total score between 70 and 120 with a body mass index (BMI) ≥17.0 kg/m2 at screening were enrolled. Patients who discontinued previous antipsychotic therapy due to inadequate efficacy and safety profile were also eligible to participate in the study.16
An independent ethics committee or institutional review board (listed in Supplementary file) at each study site approved the study protocol. The study was conducted in accordance with the ethical principles originating in the Declaration of Helsinki and International Conference on Harmonization Good Clinical Practice guidelines, applicable regulatory requirements, and in compliance with the protocol. All patients (or their legally acceptable representatives, if required by local regulations) provided written informed consent.
Randomization and Masking
This study consisted of 4 phases: a screening phase (≤3 weeks), an open-label (OL) stabilization phase (17 weeks), a randomized DB phase (48 weeks, fixed doses), and a follow-up phase (4–12 weeks). In the OL phase, all patients received PP1M (day 1: 150 mg eq. [deltoid]; day 8: 100 mg eq. [deltoid]; weeks 5 and 9: flexibly dosed [50, 75, 100, or 150 mg eq., deltoid or gluteal]; week 13: same dose as administered at week 9; Figure 1). Following the OL stabilization phase, clinically-stable patients who achieved a PANSS total score <70, PANSS item (P1, P2, P3, P6, P7, G8, G14) scores ≤4, and reduction in CGI-S score by ≥1 from OL baseline entered the DB phase and were randomized to receive fixed doses of PP3M (175, 263, 350, or 525 mg eq. [3.5×PP1M dose received at week 13]) or PP1M (same dose as week 13) once every 4 weeks. Randomization was performed using a computer-generated randomization scheme, balanced using permuted blocks across the 2 groups and stratified by study center. To maintain blinding, patients on PP3M received active medication every 3 months and received matched placebo injections (20% Intralipid) monthly.16
 |
Figure 1 Study profile. Abbreviations: PP1M, paliperidone palmitate 1-month formulation; PP3M, paliperidone palmitate 3-month formulation. |
Procedures and Outcomes
At each assessment time point between DB baseline and DB endpoint (every 4 weeks), the PANSS total score, subscale scores (PANSS negative and PANSS positive subscales, Table 1), and 5 PANSS Marder factor scores were calculated.17
 |
Table 1 PANSS Scale Structure |
Sums of the item scores for the derived subscales were calculated as
Positive subscale (range: 7–49): sum of items P1 to P7 in the positive subscale
Negative subscale (range: 7–49): sum of items N1 to N7 in the negative subscale
General psychopathology subscale (range: 16–112): sum of items G1 to G16 in the general psychopathology subscale
The PANSS Marder factor scores were evaluated based on the positive symptoms, negative symptoms, disorganized thoughts, uncontrolled hostility/excitement, and anxiety/depression. For the factor scores, the sums of the item scores were calculated as follows:
Positive symptoms factor (range: 8 to 56): P1-delusions, P3-hallucinatory behavior, P5-grandiosity, P6-suspiciousness or persecution, N7-stereotyped thinking, G1-somatic concern, G9-unusual thought content, G12-lack of judgment and insight
Negative symptoms factor (range: 7 to 49): N1-blunted affect, N2-emotional withdrawal, N3-poor rapport, N4-passive social withdrawal, N6-lack of spontaneity, G7-motor retardation, G16-active social avoidance
Disorganized thoughts factor (range: 7 to 49): P2-conceptual disorganization, N5-difficulty in abstract thinking, G5-mannerisms and posturing, G10-disorientation, G11-poor attention, G13-disturbance of volition, G15-preoccupation
Uncontrolled hostility/excitement factor (range: 4 to 28): P4-excitement, P7-hostility, G8-uncooperativeness, G14-poor impulse control
Anxiety/depression factor (range: 4 to 28): G2-anxiety, G3-guilt feelings, G4-tension, G6-depression.
Criteria for severe negative symptoms were based on the PANSS subscales and PANSS Marder factor scores. Negative symptoms were to be classified as severe if a patient displayed a baseline negative factor score of ≥25. A cutoff of 25 points was used to distinguish between severe and less severe as this was the midpoint (median) for all PANSS negative ratings, collected at baseline in the study.
Statistical Methods
Analysis Sets
The intent-to-treat (OL) analysis set (ITT-OL) included all patients who had received at least one dose of PP1M. The modified intent-to-treat (DB) analysis set (mITT-DB), included all patients who were randomly assigned to treatment during the DB phase, and who received at least one dose of study drug during the DB phase. Efficacy analyses were performed using the ITT-OL and mITT-DB analysis set for the respective phases. Safety analyses were performed using the safety analysis set (included all patients who were randomly assigned to treatment during the DB phase and received ≥1 dose of DB study drug). For the OL phase, all patients who received ≥1 dose of study drug in that phase were included in the summary of safety assessments for that phase.
Statistical Analysis
Demographic and baseline characteristics were summarized descriptively. Treatment effects were estimated based on the least square means 95% confidence interval (95% CI) and the PANSS scores were compared among the two treatment groups using ANCOVA for continuous variables or Chi-squared tests for categorical variables. No adjustments were made for multiplicity. For each time point in the DB phase, PANSS negative subscale was presented using descriptive statistics. Safety parameters were summarized descriptively.
Results
Demographics and Baseline Characteristics
Of the 1716 screened patients with schizophrenia, 1429 (83%) were enrolled and dosed in the OL phase, of which 1016 (71%) continued into the DB phase and were randomized 1:1 (PP1M: 512; PP3M: 504). Withdrawal of consent (n = 118, 8%) and lack of efficacy (n = 117, 8%) were the most common reasons for discontinuation during the OL phase. A similar proportion of patients completed the DB phase (PP1M: n=420 [82%]; PP3M: n=422 [84%]) and the most common reason for discontinuation from the study was withdrawal of consent (PP1M: 53/92 [58%]; PP3M: 50/82 [61%]). At OL baseline, the mean (SD) total PANSS score for the PP1M group was 85.7 (10.73) in the OL ITT population. At DB baseline, the total PANSS score was 57.3 (8.57) for the PP3M group and was 58.2 (9.07) for the PP1M group mITT population.16 Of the1429 patients enrolled in the OL phase 782 (55%) were men; the majority of the enrolled patients were white (55%) with a mean (SD) age of 38.4 (11.86) years. The mean (SD) PANSS total score at OL baseline was 85.7 (10.73) and at DB baseline was 57.8 (8.83). Demographics and baseline characteristics were similar between the PP3M and PP1M groups in the OL and DB phases and have been published earlier.16
Negative Symptoms
At the OL baseline, the mean (SD) negative symptom factor was 22.3 (4.87) and the mean (SD) negative subscale score was 23.2 (4.60). At DB baseline, following stabilization with PP1M, the negative symptom factor declined to 16.2 (3.98) and the negative subscale score declined to 17.3 (4.20). The total score for negative subscale at OL baseline ranged from 10 to 41 with a mean (SD) of 23.2 (4.60), indicating a moderate to severe burden of disease (Figure 2).
 |
Figure 2 Negative symptom factor vs subscale scores over time (ITT analysis set). Abbreviations: DB, Double blind; ITT, intent-to-treat, OL, Open-label. |
Following treatment with PP1M to OL endpoint, the negative symptom factor declined significantly (p<0.0001) to 17.7 (5.12). A further significant decline (p<0.0001) from OL endpoint in the negative symptom factor to 14.9 (4.81) at DB endpoint was observed for all patients (PP1M and PP3M treated).
Similarly, at OL endpoint, negative subscale scores declined significantly (p<0.0001) to 18.9 (5.20) following PP1M stabilization; negative subscale scores further declined to 15.9 (4.99) at DB endpoint from OL endpoint.
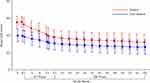
The mean (SD) change from baseline values for negative symptoms factor and negative subscale score were comparable at both OL endpoint (–4.5 [4.93] vs –4.4 [4.79]) and DB endpoint (–7.3 [5.47] vs –7.2 [5.28]). The negative subscale score and negative symptoms factor declined over time in parallel to the decline observed in the total PANSS scores (Figure 3A and B). Following stabilization with PP1M, negative subscale scores were comparable between PP1M (17.4 [4.18]) and PP3M (17.3 [4.23]) groups at DB baseline. These negative subscale scores declined over time for both PP1M and PP3M patients (Table 2). At DB endpoint, negative subscale scores were 15.9 (4.93) for PP1M and 15.8 (5.05) for PP3M groups. The mean (SD) change in negative subscale score from DB baseline to DB endpoint was significant (p<0.0001) and was comparable for both treatment groups over (PP1M: –1.4 [3.67] vs PP3M: –1.4 [3.63], Figure 4). Furthermore, PANSS negative symptom item scores (N1 to N7) showed comparable improvements from DB baseline to DB endpoint in patients treated with PP1M or PP3M (Supplementary Table 1).
 |
Table 2 Negative Subscale Scores and Change from Baseline Over Time (mITT-DB Analysis Set) |
Patients with negative symptom factor score of ≥25 at OL baseline were included in the severe negative symptom group. In the PP1M and PP3M groups at DB baseline, a total of 282 patients displayed severe negative symptoms with a negative symptom factor of ≥25 and more than twice as many patients (n=723) displayed less severe negative symptoms. At the end of the 48-week DB treatment phase, the mean (SD) negative symptom factors were similar for both patient groups (severe: 16.1 (4.67), less severe: 13.3 (4.13), Figure 5).
Discussion
Negative symptoms account for long-term morbidity and poor functional outcomes in patients with schizophrenia. Results of this post-hoc analysis of PP1M and PP3M highlight improvements in the PANSS negative subscales and negative symptom factors in patients with moderate to severe negative symptoms of schizophrenia over the observed timepoints; both PP3M and PP1M demonstrated similar improvements. Furthermore, treatment with PP3M or PP1M significantly improved negative symptoms (p<0·0001) when compared to baseline, and this improvement was seen regardless of symptom severity. Improvements in negative subscale scores (for all subscales N1 to N7) were comparable for both PP1M and PP3M treatment. Patients with higher symptom severity showed greater improvements in negative symptoms with PP1M or PP3M over time.
Negative symptoms in schizophrenia have been historically recognized as difficult to diagnose and treat with antipsychotics. Among the accumulating evidence supporting this concept, the largest meta-analysis conducted to date reported small improvements in negative symptoms (numerically 0.5 points on the negative subscale score that were not clinically relevant).7 However, most previous studies involved oral antipsychotics, with which treatment non-adherence is common and difficult to detect.18 Hence, it has been unclear whether the observed degree of benefit for negative symptoms may have been limited by discontinuous treatment. In the present study, we found that continuous antipsychotic use (with PP1M or PP3M) ensured medication adherence that resulted in improvements in negative symptoms that were of much greater magnitude. While a portion of patients withdrew consent during the study, medication adherence could be verified during participation because PP1M and PP3M treatments, unlike oral antipsychotics, were administered by a healthcare professional. Numerical changes of approximately 2.0 points in negative subscale score from baseline to endpoint were reported at several timepoints during the 48-week treatment period. This corresponds to a greater improvement in negative subscale score as compared with the meta-analysis findings,7 suggesting that negative symptoms take much longer to change (duration of intervention: 48 weeks [PP3M] vs 12.4 weeks in the meta-analysis), and improve steadily over time.
The PANSS scoring system is one of the most widely used assessment techniques in randomized, controlled studies for evaluating the effects of antipsychotic medications in schizophrenia.10 It is amongst the most sensitive instruments that provide a balanced representation of positive and negative symptoms and gauges the relationship of both to general psychopathology.10 Following stabilization with PP1M, a decline in the PANSS negative subscales and negative symptom factors scores were observed for both PP1M- and PP3M-treated patients and the changes in PANSS negative symptoms scores were comparable between PP1M and PP3M. Although this analysis was not limited to patients with severe negative symptoms, more improvement was observed in patients with severe negative symptoms as compared to those with less severe negative symptoms. This finding suggests that treatments with LAIs PP1M or PP3M may substantially benefit patients with negative symptoms. These observations for LAIs, PP1M and PP3M are consistent with those observed for risperidone LAI (RLAI). Significant improvement in negative symptom severity was observed following 6 months of treatment with RLAI in patients with prominent negative symptoms.19 Additionally, improvements in negative symptoms following treatment with paliperidone LAI are in accordance with those observed with paliperidone ER.14,20
Individuals with negative symptoms are known to show poor adherence to their prescribed antipsychotic therapy. Achieving good treatment adherence is therefore critical when treating patients with predominant negative symptoms.21 The use of LAI antipsychotics has been associated with substantial improvements in treatment adherence.22 The results of the current analysis highlight continued improvements in negative symptoms during long-term treatment with LAI’s, both PP1M or PP3M. These findings support previous studies demonstrating that consistent, long-term treatment with LAIs is associated with substantial improvements in functional outcomes in patients with negative symptoms of schizophrenia.19
Secondary causes of negative symptoms can include adverse effects such as EPS. Since an overall decrease in EPS-related TEAEs was reported post PP1M and PP3M treatments,16 a correlation between improvements in negative symptoms and its association with improvements in EPS-related effects is required. Patients included in this post-hoc analysis demonstrated improvements in clinically relevant symptoms of schizophrenia. However, it is difficult to determine whether the improvements in negative symptoms were attributable to a specific effect of PP1M or PP3M or due to improvements in compliance. Also, this post-hoc analysis was conducted using studies that were not designed to specifically examine patients with predominant negative symptoms. Thus, additional long-term prospective studies which could assess the long-term efficacy of PP3M on negative symptom in patients with predominant negative symptoms are warranted.
Conclusion
The burden of negative symptoms can adversely impact patients with schizophrenia. Negative symptoms can be difficult to treat and can lead to substantial functional impairments in patients. This post-hoc analysis suggests that treatment with long-acting injectables (such as PP3M or PP1M) may be associated with continued improvement in negative symptoms over time that may facilitate improved functioning and quality of life in patients with schizophrenia. However, long-term prospective studies to assess the long-term benefits of these LAIs in resolving negative symptoms are warranted.
Data Sharing Statement
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at http://yoda.yale.edu.
Acknowledgments
The authors thank Shweta Pitre, MPharm, CMPP™, for providing writing assistance and Ellen Baum, PhD (Janssen Research & Development, LLC), for additional editorial support for the development of this manuscript. The authors also thank the study participants, without whom this study would not have been accomplished, and all the investigators for their participation in this study. A part of this data was previously presented at the 6th Biennial Conference of Schizophrenia International Research Society (SIRS) 2018, Italy as a poster presentation. The poster’s abstract was published in Schizophrenia Bulletin, 44, Issue suppl, April 2018, Page S311. https://doi.org/10.1093/schbul/sby017.761
These data were also presented as encore posters at the following conferences:
- 73rd Society of Biological Psychiatry Annual Meeting, 2018, New York – Biological Psychiatry 83, (9), Suppl, May 2018, Pg S316 https://doi.org/10.1016/j.biopsych.2018.02.813
- Annual Meeting of the American Psychiatric Association (APA) 2018, New York
- Canadian College of Neuropsychopharmacology, 2018, Canada;
- 31st European College of Neuropsychopharmacology (ECNP) Congress, 2018, Spain – European Neuropsychopharmacology 29, Suppl, 2019, Pg S101-S102 https://doi.org/10.1016/j.euroneuro.2018.11.1087
- US Pysch Congress, 2018, Florida, USA – Psychiatry & behavioral health learning network: https://www.psychcongress.com/posters/phase-3-non-inferiority-study-comparing-paliperidone-palmitate-1-month-vs-3-month-long
Author Contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was funded by Janssen Research & Development, LLC. All authors had full access to the data in the study and final responsibility for the decision to submit for publication.
Disclosure
SG, MM, AS and JG are employees of Janssen Research and Development, USA, EK is an employee of Janssen Scientific affairs, USA and KP is an employee of Janssen-Cilag, Germany; all authors hold company stocks. The authors report no other conflicts of interest in this work.
References
1. Mitra S, Mahintamani T, Kavoor AR, Nizamie SH. Negative symptoms in schizophrenia. Ind Psychiatry J. 2016;25(2):135–144. doi:10.4103/ipj.ipj_30_15
2. Remington G, Foussias G, Fervaha G, et al. Treating negative symptoms in Schizophrenia: an update. Curr Treat Options Psychiatry. 2016;3:133–150. doi:10.1007/s40501-016-0075-8
3. Trivedi JK. Cognitive deficits in psychiatric disorders: current status. Indian J Psychiatry. 2006;48(1):10–20. doi:10.4103/0019-5545.31613
4. Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. 2012;11(2):73–79. doi:10.1016/j.wpsyc.2012.05.004
5. Capatina OO, Miclutia IV. Are negative symptoms in schizophrenia a distinct therapeutic target? Clujul Med. 2018;91(1):58–64. doi:10.15386/cjmed-864
6. Galderisi S, Mucci A, Buchanan RW, Arango C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry. 2018;5(8):664–677. doi:10.1016/S2215-0366(18)30050-6
7. Fusar-Poli P, Papanastasiou E, Stahl D, et al. Treatments of negative symptoms in schizophrenia: meta-analysis of 168 randomized placebo-controlled trials. Schizophr Bull. 2015;41(4):892–899. doi:10.1093/schbul/sbu170
8. Kirkpatrick B, Fenton WS, Carpenter WT
9. Harvey PD, Khan A, Keefe RSE. Using the positive and negative syndrome scale (PANSS) to define different domains of negative symptoms: prediction of everyday functioning by impairments in emotional expression and emotional experience. J Clin Neurosci. 2017;14(11–12):18–22.
10. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi:10.1093/schbul/13.2.261
11. Emsley R, Rabinowitz J, Torreman M; Group R-I-EPGW. The factor structure for the positive and negative syndrome scale (PANSS) in recent-onset psychosis. Schizophr Res. 2003;61(1):47–57. doi:10.1016/S0920-9964(02)00302-X
12. Buchanan RW. Persistent negative symptoms in schizophrenia: an overview. Schizophr Bull. 2007;33(4):1013–1022. doi:10.1093/schbul/sbl057
13. Earley W, Guo H, Daniel D, et al. Efficacy of cariprazine on negative symptoms in patients with acute schizophrenia: a post hoc analysis of pooled data. Schizophr Res. 2018.
14. Canuso CM, Bossie CA, Turkoz I, Alphs L. Paliperidone extended-release for schizophrenia: effects on symptoms and functioning in acutely ill patients with negative symptoms. Schizophr Res. 2009;113(1):56–64. doi:10.1016/j.schres.2009.05.021
15. Peralta V, Cuesta MJ. Psychometric properties of the positive and negative syndrome scale (PANSS) in schizophrenia. Psychiatry Res. 1994;53(1):31–40. doi:10.1016/0165-1781(94)90093-0
16. Savitz AJ, Xu H, Gopal S, et al. Efficacy and safety of paliperidone palmitate 3-month formulation for patients with schizophrenia: a randomized, multicenter, double-blind, noninferiority study. Int J Neuropsychopharmacol. 2016;19(7):pyw018. doi:10.1093/ijnp/pyw018
17. Maust D, Cristancho M, Gray L, Rushing S, Tjoa C, Thase ME. Chapter 13 - psychiatric rating scales. In: Aminoff MJ, Boller F, Swaab DF, editors. Handbook of Clinical Neurology. Vol. 106. Elsevier; 2012:227–237.
18. Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62. doi:10.2147/PROM
19. Curtis VA, Katsafouros K, Moller HJ, Medori R, Sacchetti E. Long-acting risperidone improves negative symptoms in stable psychotic patients. J Psychopharmacol. 2008;22(3):254–261. doi:10.1177/0269881107082119
20. Turkoz I, Bossie CA, Dirks B, Canuso CM. Direct and indirect effects of paliperidone extended-release tablets on negative symptoms of schizophrenia. Neuropsychiatr Dis Treat. 2008;4(5):949–958. doi:10.2147/ndt.s3668
21. Janssen B, Gaebel W, Haerter M, Komaharadi F, Lindel B, Weinmann S. Evaluation of factors influencing medication compliance in inpatient treatment of psychotic disorders. Psychopharmacology (Berl). 2006;187(2):229–236. doi:10.1007/s00213-006-0413-4
22. Brasso C, Bellino S, Bozzatello P, Montemagni C, Rocca P. Role of 3-monthly long-acting injectable paliperidone in the maintenance of schizophrenia. Neuropsychiatr Dis Treat. 2017;13:2767–2779. doi:10.2147/NDT
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.