Back to Journals » Advances in Medical Education and Practice » Volume 13
Implementation of Learning Communities at Khalifa University College of Medicine and Health Sciences, Abu Dhabi, United Arab Emirates
Authors Hernandez Jr R , Lou J, Al-Omari B , Aloum L, Kanj S, Ismaiel S, Rock J
Received 1 February 2022
Accepted for publication 16 May 2022
Published 28 May 2022 Volume 2022:13 Pages 577—583
DOI https://doi.org/10.2147/AMEP.S360731
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Robert Hernandez Jr,1,2 Jennie Lou,1,3 Basem Al-Omari,1,3 Lujain Aloum,1,4 Saly Kanj,1 Sawsan Ismaiel,1 John Rock5
1Department of Academic Affairs, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates; 2Department of Medicine, Kirk Kerkorian School of Medicine, University of Nevada Las Vegas, Las Vegas, NV, USA; 3Department of Epidemiology and Population Health, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates; 4Department of Pharmacology, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates; 5Dean’s Office, College of Medicine and Health Sciences, Khalifa University, Abu Dhabi, United Arab Emirates
Correspondence: Robert Hernandez Jr, Department of Medicine, Kirk Kerkorian School of Medicine, University of Nevada Las Vegas, 2040 W. Charleston Blvd., 4th Floor, Las Vegas, NV, 89102, USA, Tel +1 702-895-2662, Email [email protected]
Abstract: Learning community programs have been widely implemented in higher education institutions, including many accredited medical schools in North America. Learning communities have been shown to create a sense of belonging, enhance teaching and learning, and promote an inclusive educational environment that reinforces collaboration, professionalism, and wellbeing. Based on their demonstrated success, a learning community program was included in the development of Khalifa University College of Medicine and Health Sciences (KU CMHS), the first medical school in the capital city of Abu Dhabi and the first to offer a postbaccalaureate, Doctor of Medicine (MD) degree in the United Arab Emirates (UAE). Named the Falcon Learning Communities (FLCs), the program adopted the core values of the Learning Communities Institute and integrated them into curricular, co-curricular, and extra-curricular programming. This paper presents an overview on the development of the FLC program, its implication for both students and faculty, preliminary feedback from teachers and learners, and considerations for future work.
Keywords: undergraduate medical education, teaching, learning, strategies
History of Learning Communities
The origins of modern learning communities can be traced back to the early 1920s.1 Alexander Meiklejohn, a philosopher and educational reformer, pioneered a model of education that fostered closer relationships between teachers and learners using the concepts of a unified curriculum and a cohesive and cooperative learning community.2 John Dewey, a philosopher and American intellectual, supported learning that was active, student centered, and involved shared inquiry.1 By 1984, The National Institute for Education called for institutions of higher learning to create, “learning communities organized around specific intellectual themes or tasks”.1 Since then, the learning community model has taken hold in many institutions of higher education, including many accredited medical schools in the United States.
Although they have been widely implemented, there is no universal definition for learning communities. In a report for the Association for the Study of Higher Education - Educational Resources Information Center (ASHE-ERIC), Lenning and Ebers defined them as intentionally developed groups that promote and maximize learning.3 Learning communities also vary widely in structure and function. Gabelnick et al noted that learning communities, “purposefully restructure the curriculum to link together courses or coursework, so that students find greater coherence in what they are learning as well as increased intellectual interaction with faculty and fellow students”.1 West and Williams identified four defining characteristics of learning communities: access, relationships, vision, and function.4
In 1971, the University of Missouri - Kansas City School of Medicine became the first US medical school to incorporate learning communities into its MD program. According to a survey conducted by the Liaison Committee for Medical Education (LCME), more than 100 North American medical schools have implemented learning communities.5 A 2015 survey of LCME-accredited medical schools found that learning communities provide a large variety of services and support, including professional development, mentoring, advising, counseling, social and wellness activities, community service, and research.5 The survey also found that Learning communities have been shown to create a sense of belonging, enhance teaching and learning, and promote a positive learning environment that reinforces professionalism, humanism, and wellbeing. They also enable personal and professional success and positively impact learners, teachers, staff, and community.
Several authors of this paper have been involved in the development and/or management of learning communities at different LCME-accredited medical schools in the United States. While the communities varied in form and function, all helped achieve the important institutional goal of organizing teachers and learners into groups that promoted and enhanced learning. For that reason, implementation of learning communities was felt to be a critical goal for the development of a new American-style medical school in the United Arab Emirates.
Khalifa University College of Medicine and Health Sciences
Khalifa University College of Medicine and Health Sciences (KU CMHS) is the first medical school developed in the city of Abu Dhabi and the first four-year, post-baccalaureate Doctor of Medicine (MD) Program in the United Arab Emirates (UAE). The program is fashioned after medical degree programs in the United States and Canada that are accredited by the Liaison Committee for Medical Education (LCME). Recruitment and admission of students to the MD Program began during academic year 2018–19, and the first entering class matriculated in August 2019. The program achieved full accreditation from the Commission of Academic Accreditation (CAA) in January 2021. The CAA is a recognized accrediting agency by both the World Federation for Medical Education (WFME) and The Foundation for Advancement of International Medical Education and Research (FAIMER).
The mission of the CMHS is to enhance the healthcare ecosystem of Abu Dhabi and the UAE through outstanding education, research, healthcare, and service to the community. To achieve its aims, the college recruits a diverse group of Emiratis, UAE nationals, and international students with the potential to contribute to the productivity and competitiveness of the national healthcare workforce. The MD program leverages its position in Khalifa University of Science and Technology, a research-intensive institution, to seamlessly integrate technology into personalized preventative medical practice.
Doctor of Medicine Curriculum
The MD curriculum, depicted in Table 1, provides an innovative and challenging curriculum taught by the best clinical and research faculty in the UAE. The curriculum is designed to provide content of sufficient breadth and depth to prepare its graduates for entry into any specialty and for the subsequent contemporary practice of medicine. Students are required to take the UMSLE Steps 1 and 2 CK, as the program aspires to graduate physicians capable of pursuing graduate and fellowship training in North American and then returning to practice in the UAE.
 |
Table 1 Khalifa University College of Medicine and Health Sciences Curriculum Map |
The curriculum fully integrates basic and clinical science instruction into four periods of study. Period 1, Foundations of Medicine, covers foundational topics in molecular and cellular biology; human genetics; human anatomy, histology, and embryology; physiology and immunology; pathology; microbiology and infectious disease; and pharmacology and therapeutics. Period 2, Organ Systems, focuses on the in-depth study of human biology, disease, illness, and injury organized by the major organ-systems; specifically, the cardiovascular, respiratory, hematopoietic, lymphoreticular, endocrine, reproductive, musculoskeletal, integumentary, gastrointestinal, renal, nervous, and behavioral systems. Clinical correlations tie the biomedical sciences to medical practice. Period 3 begins the intensive clinical training phase and consists of eight (8) core clerkships: Surgery, Internal Medicine, Neurology, Medical Imaging, Family Medicine, Obstetrics and Gynecology, Pediatrics, and Psychiatry. One day each week, students participate in formal lectures, case-based small group sessions and/or simulation training as part of the Core Concepts in Medicine course. Period 4 builds on clerkship experiences and prepares students to enter their chosen field of specialization after graduation. All students must complete rotations in Emergency Medicine, Geriatrics, and Advanced Medicine and Sub-Internship experiences in a specific discipline.
Five themes or strands are interwoven throughout the four periods of study. The strands align with core competencies of the Accreditation Council for Graduate Medical Education (ACGME). They are the Biomedical Science strand; the Clinical Medicine strand; the Medicine and Society strand; the Physicianship strand; and the Research, Technology, and Innovation strand. Biomedical Science aligns with the core competency of medical knowledge. Clinical Medicine aligns with the competencies of patient care, and interpersonal and communication skills. Medicine and Society aligns with the core competency of systems-based practice. Physicianship aligns with the core competencies of professionalism, and practice-based learning and improvement. Research, Technology, and Innovation focuses on the development of knowledge and skills necessary to identify and address the complex problems one faces in the healthcare environment.
The 4-year course of study leading to the MD degree employs a variety of teaching and learning methodologies. There is a strong focus on student-centered active learning experiences (eg, problem-based learning, case-based learning), independent student-directed learning activities, flipped classroom, simulation training, and real-world clinical experiences. These methodologies are designed to help students gain the competencies expected of all physicians. A variety of assessment strategies are used to evaluate student progress, including National Board of Medical Examiners (NBME) subject examinations, NBME comprehensive basic and clinical science examinations, objective structured clinical examinations, and the United States Medical Licensing Examinations Steps 1 and 2 CK. The duration of the MD program is 153 weeks.
Falcon Learning Communities
The Falcon Learning Communities (FLCs) are an educational and social structure designed to support learners and teachers through a variety of special programs and services that are fully integrated with the M.D. curriculum. The FLCs promote six core values which are adapted from the Learning Communities Institute, a group that values and supports the active presence of learning communities based in health professions schools in the United States, Mexico, and Canada. The six core values are: relationships, professionalism, scholarship, wellness, professional development, and inclusiveness.
In addition to promoting these values, the FLCs aim to instill pride in the community and culture of the UAE. The communities are named after the falcon, the UAE’s national bird and a potent symbol of strength and courage to Emiratis. There are four learning communities. In recognition of the rich cultural and medical heritage of the Arab world, each community is named after a famous Arab or Muslim physician or scientist; Al-Zahrawi, Ibn Zuhr, Ibn Rushd and Ibn Al-Nafis.
Abū al-Qāsim Khalaf ibn al-‘Abbās al-Zahrāwī al-Ansari (936–1013), otherwise known as Al-Zahrawi or Abulcasis, was an Arab Muslim physician, surgeon, and chemist who lived in Al-Andalus (Islamic Iberia). He is considered to be the greatest surgeon of the Middle Ages and has been described as the father of surgery. He authored Kitab al-Tasrif, a 30-volume encyclopedia of medical practice, which took him 50 years to complete and which was used around the world for several centuries.
Ala-al-din abu Al-Hassan Ali ibn Abi-Hazm al-Qarshi al-Dimashqi (1213–1288), otherwise known as Ibn al-Nafis, was an Arab Muslim physician from Damascus who was the first to describe the pulmonary circulation of the blood and predicted the existence of capillary blood vessels. He also described coronary and capillary circulations. For this he is sometimes referred to as “the father of circulatory physiology.” He wrote more than 110 important medical texts, including an extensive medical encyclopedia, Al-Shamil fi al-Tibb (the Comprehensive Book of Medicine), an 80-volume medical encyclopedia, one of the largest ever written by one person.
Abū l-Walīd Muḥammad Ibn ʾAḥmad Ibn Rušd (1126–1198), otherwise known as Ibn Rushd or Averroes, was a Muslim Andalusian philosopher who wrote about many subjects, including philosophy, theology, astronomy, jurisprudence, and medicine. He is considered one of the greatest thinkers and scientists of history. His greatest medical work was Kitab al-Kulliyyat (General Principles of Medicine) which described anatomy, illness, nutrition, and preventive medicine. This became a medical textbook that was used for centuries throughout Europe.
Abū-Marwān “Abd al-Malik ibn Abī al-”Alā’ Ibn Zuhr (1093–1162), otherwise known as Ibn Zuhr or Avenzoar, was a Muslim Andalusian physician, surgeon, and poet who was best known for his emphasis on a more rational, empiric basis of medicine and a formal method of education of surgeons. He was a pioneer in the development of the surgical procedures of tracheostomy and cataract surgery and is considered as one of the greatest clinicians of the western caliphate.
Each of the four communities has a faculty academic advisor, basic science faculty advisors, clinical skills preceptors, research advisors, BALSAM Preceptors, and a learning community coordinator. The program is overseen by the assistant dean for Falcon Learning Communities who reports to the associate dean for academic affairs/chief academic officer. Each community has its own multipurpose room with ample space for educational and social activities. The four learning community rooms are located on the 2nd floor of the medical school building, close to the administrative offices where the faculty advisors reside. The layout of a typical learning community room is depicted in Figure 1.
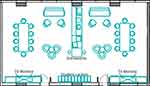 |
Figure 1 Layout of typical learning community space. |
At matriculation, students are assigned to one of the four learning communities. They remain in that community for the duration of their matriculation. As they move forward in the program, students take on greater organizational and leadership roles within their community. In this manner, upper-level students can serve as teachers and mentors to those who come behind.
The signature programs of the FLCs align to core components of the MD curriculum and are delivered through a variety of curricular, co-curricular, and extra-curricular activities. The signature programs are service learning, peer-assisted learning, professional development, and innovation and entrepreneurship.
The service-learning program aligns with the Medicine and Society strand and the core competency of systems-based practice. Integral to Medicine and Society is BALSAM or Barnamij L-Ta’leem Sehat al-Mujtama (برنامج لتعليم صحة المجتمع - بَلسمْ), a community-based, household-focused, longitudinal service-learning program that incorporates attention to the social determinants of health (SDoHs) thru its education, health care, and research missions. BALSAM integrates social sciences, clinical experience, interprofessional teamwork, and attention to the SDoHs to prepare socially accountable and culturally sensitive physicians, while partnering with a network of community agencies to improve the health of households and communities.
BALSAM participation is required, starting from year two of the MD program. It is executed in collaboration with the Ambulatory Healthcare Services (AHS) of the Abu Dhabi Health Services Company (SEHA), the main health care provider in Abu Dhabi. Students accompany an AHS team during routine home visits in the local community. Prior to the visits, students attend a huddle at the AHS clinic to discuss the patients that they will be visiting. During each visit, students get the opportunity to practice clinical skills and be involved in patient care under the direct supervision of the AHS physician. Students are asked to consider the social determinants of health in relation to each patient’s case and discuss them in a reflective assignment. This assignment is linked to one of the assessments of the Medicine and Society strand.
The peer-assisted learning program, named Falcon PALs, aligns with the Clinical Medicine strand and the core competencies of patient care, medical knowledge, and interpersonal and communications skills. Over the first two years, students take Clinical Skills I and II. As students acquire and demonstrate competencies in clinical skills, they are given opportunities to participate in peer-assisted learning. Student teachers go through a certification process. Once certified, they participate in clinical skills training and offer tutoring and practice sessions. This prepares learners to take on the teaching roles they will be expected to assume during residency training and beyond.
The professional development program aligns with the Physicianship strand and the core competencies of professionalism and practice-based learning and improvement. The program is designed to advocate for professionalism by defining and role modeling desirable behaviors while identifying and addressing inappropriate and disruptive behaviors. The program includes a system for members of the community to report exemplary professional behavior or unprofessional behavior. Exemplary behaviors are recognized and noted in the student’s record. Depending on their severity or repetitiveness, unprofessional behavior can be addressed in a formative manner by the FLC advisors or be referred to the student progress committee for evaluation and action.
The innovation and entrepreneurship program aligns with the Research, Technology, and Innovation (RTI) strand. The MD curriculum attempts to inculcate in students an entrepreneurial mindset, or a way of thinking that enables them to identify and address challenges in a manner that is self-directed, active, creative, and engaged. Students are required to complete a scholarly project as a condition for graduation. The FLCs provide a forum through which students can identify challenges and receive appropriate support to develop strategies that address them.
In addition to meeting the four critical functions described above, the FLCs provide additional services to the MD program. The administrative coordinators, who hold master’s degrees in various disciplines, participate in curriculum development and delivery. They also serve as proctors for NBME subject examinations and objective structured clinical evaluations. Further, they participate in planning and managing major events such as freshman orientation, match, and graduation.
Student Experience
Students are matched to one of the four learning communities at the beginning of their first year and remain in the same community for the remainder of their matriculation in the MD program. FLC assignments are based on several criteria, including prior academic performance, primary language, gender, nationality, and age. The goal is to create communities of individuals who bring diverse academic and life experiences to the group.
The FLCs play an important role in onboarding students, introducing them to the culture of the CMHS, and preparing them for the rigors of MD training. One popular activity, Falcon Day, occurs during freshman orientation. It introduces students to their learning community colleagues, advisors and coordinators through a series of friendly competitions that require teamwork and sportsmanship. The winning community receives the Falcon Award, a gold-colored statue that resides in the learning community for the academic year.
Early in the first semester, students meet with their academic advisor to discuss their academic and professional goals for the year. During the year, students are encouraged to meet with their advisor if they wish to seek guidance or support. They have the option to meet with their basic science advisor if they wish to obtain tutoring. The student progress committee may mandate for students to meet with their academic advisor if they experience any difficulty. At the end of the year, students again meet with their advisor to review their academic performance and overall progress.
The FLC clinical preceptors participate in clinical skills training sessions with their students. In addition to teaching communication and examination skills, the preceptors evaluate student performance during objective structured clinical examinations and provide both formative and summative feedback. As previously noted, students work with their clinical preceptors and the FLC coordinators to organize peer-assisted learning (PAL) training sessions. These additional co-curricular sessions promote the acquisition of core knowledge and skills while also giving students the opportunity to practice teaching skills.
The Falcon Learning Communities also support student health and wellness through a series of year-round activities that begin during orientation. Students are not only the beneficiaries of wellness programming, but also work closely with the medical education administration to develop co-curricular and extra-curricular activities that support student physical, mental, social, spiritual, financial, and academic wellness.
FLC advisors and coordinators support the research curriculum by teaching in the Research, Technology, and Innovation strand. FLC research advisors are available to meet with and assist students interested in pursuing extracurricular research opportunities. This has motivated students to participate in research activities, and to generate high-impact publications. Within the first two years of establishing the FLCs, 12 medical students, working with faculty research advisors, published research papers in Q1 and Q2 Scopus and PubMed indexed journals.
The FLCs also play an important role in introducing students to the Abu Dhabi community, its history, and its culture. Co-curricular and extracurricular activities and events held throughout the year include lectures, seminars, and service events. For example, seminars have been delivered to teach Arabic language and the Emirati dialect to non-Arabic speaking medical students. The seminars help students communicate effectively in hospital, clinic and community healthcare settings, and help overcome communication barriers with patients and families during BALSAM visits. Several community-oriented campaigns (eg, waste recycling and blood donation,) have helped broaden students’ perspectives beyond the classroom and have engaged them in various environmental and socio-economic efforts.
Lastly, the FLCs offer a variety of wellness and social events that help students decompress while promoting healthy lifestyles. During lockdowns caused by the COVID-19 pandemic, virtual activities were held to support students’ physical and mental wellbeing. Students who had to quarantine or who participated in distance learning due to travel restrictions were able to maintain social relationships by participating in FLC virtual activities. On campus, the FLCs have held many types of activities, such as meditation and yoga sessions, to promote mindfulness and balance.
Outcomes
Thus far, both subjective and objective measures indicate that the FLC program is proving to be effective at supporting the school’s mission. Routine focus groups and surveys demonstrate high satisfaction among teachers and learners with FLC-supported activities. The academic performance of students, supported by FLC academic advising, has also been strong as demonstrated by median scores a standard deviation above the international average on the National Board of Medical Examiners International Foundations of Medicine Basic Science examination. The impact of FLCs on student-life has also been very positive. For example, during pandemic lockdowns, the FLCs played a vital role in maintaining health and wellness as reported in student testimonials. “Social isolation was very stressful for me and being able to connect with people, talk and play games kept me going!” “I loved the weekly challenges – I thought it was very generous to give out prizes, and I loved the games. It was nice to see and speak to colleagues and classmates and get through this period together”. Plans are to conduct more through and comprehensive surveys when all four classes have students in each community, and when the inaugural class of 2019 graduates from the MD program in 2023.
Future Directions
Presently, the primary focus of the Falcon Learning Communities is to prepare for four full classes of students. The fourth class will enter in July 2022. At that time, the FLCs will be able to fully realize the intended organizational and leadership structure of the program. Senior students will participate in strategic planning and help implement an apprenticeship model of modern medical education. Relationships between teachers and learners will be supplemented by the further development of peer-assisted learning and peer mentorship. Given the importance of mastering interactions with patients, a future consideration is to establish a faculty-student-patient continuity model by collecting systematic feedback from patients and relaying it to students in a constructive manner. Furthermore, coordinating routine multi-institutional evaluations of FLC performance will help identify areas for improvement. Finally, the FLCs aim to create and sustain an impactful student Alumni chapter within the CMHS to ensure classmates and students have a platform to establish research collaborations and gain access to continuing education and career opportunities.
Disclosure
The authors report no financial/non-financial interests or conflicts of interest in this work.
References
1. Gabelnick F, MacGregor J, Matthews RS, Smith BL. Learning community foundations. N Directions Teach Learning. 1990;41:5–18.
2. Nelson AR. Education and Democracy: The Meaning of Alexander Meiklejohn, 1872–1964.
3. Lenning OT, Ebbers LH. The powerful potential of learning communities: improving education for the future. ASHE-ERIC Higher Educ Rep. 1999;26(6):22.
4. Williams GS, West RE. I don’t think that word means what you think it means: a proposed framework for defining learning communities. Educ Tech Res Dev. 2017;65:1569–1582. doi:10.1007/s11423-017-9535-0
5. Shochet R, Fleming A, Wagner J, et al. Defining learning communities in undergraduate medical education: a national study. J Med Educ Curric Dev. 2019;6:2382120519827911. doi:10.1177/2382120519827911
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
