Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Impact of Thrombolysis Time Metrics When Participating in National Stroke Center Construction Project
Authors Cheng W, Mofatteh M , Baizabal-Carvallo JF, Lu S, Su P, Chen Y , Li L, Qin L, Zuo X, Lan Y, Huang Y, Yu Z, Luo Z, Chen G
Received 26 July 2023
Accepted for publication 19 October 2023
Published 7 November 2023 Volume 2023:16 Pages 3333—3338
DOI https://doi.org/10.2147/JMDH.S432458
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Wanchun Cheng,1 Mohammad Mofatteh,2 José Fidel Baizabal-Carvallo,3,4 Shaohuan Lu,1 Ping Su,1 Yimin Chen,5,6 Luoming Li,1 Lizhi Qin,1 Xingmei Zuo,1 Yifeng Lan,7 Yue Huang,8 Zhihui Yu,9 Zirui Luo,10,* Gang Chen10,*
1Department of Neurology and National Stroke Center, The 5th People’s Hospital of Foshan City, Foshan, People’s Republic of China; 2School of Medicine, Dentistry and Biomedical Sciences, Queen’s University Belfast, Belfast, UK; 3Parkinson’s Disease Center and Movement Disorders Clinic, Department of Neurology, Baylor College of Medicine, Houston, Texas, USA; 4Department of Sciences and Engineering, University of Guanajuato, León, Mexico; 5Department of Neurology and Advanced National Stroke Center, Foshan Sanshui District People’s Hospital, Foshan, People’s Republic of China; 6Neuro International Collaboration (NIC), Foshan, People’s Republic of China; 7Department of Radiology, the 5th People’s Hospital of Foshan City, Foshan, People’s Republic of China; 8Department of Emergency, the 5th People’s Hospital of Foshan City, Foshan, People’s Republic of China; 9Department of Laboratory Medicine, the 5th People’s Hospital of Foshan City, Foshan, People’s Republic of China; 10Dean’s Office, the 5th People’s Hospital of Foshan City, Foshan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zirui Luo; Gang Chen, Dean’s Office, the 5th People’s Hospital of Foshan City, Foshan, Guangdong Province, 528211, People’s Republic of China, Email [email protected]; [email protected]
Purpose: Intravenous thrombolysis has emerged as an effective approach to improve the long-term survival and functional status of patients with ischemic stroke. The aim of this study was to assess the impact of a national stroke project on the door-to-needle-time (DNT).
Patients and Methods: The patients were divided into pre-construction and construction periods. Construction Measures were performed during the construction period. The DNT and onset-to-needle time (ONT) were compared in two period groups.
Results: After participating in the National Stroke Center Project and effective measurements, the thrombolysis treatment metrics were improved significantly. The DNT (IQR) was shortened from 65.0 (54.5,85.0) minutes in the Pre-Construction period to 40.0 (33.0,53.0) minutes in the Construction period (p < 0.001). Similarly, the ONT was reduced from 157.0 (IQR) (115.0,184.0) minutes to 116.0 (87.8,170.0) minutes (p = 0.035).
Conclusion: The DNT time and ONT time can be shortened by National Stroke Center Construction projects. More suitable hospitals should be encouraged to participate as the National Stroke Center.
Keywords: acute ischemic stroke, intravenous thrombolysis, door-to-needle time, onset-to-needle time
Introduction
Stroke accounts for the second most common cause of global death as well as the most common etiology contributing to increased mortality and the leading cause of disability-adjusted life-year in China.1 Intravenous thrombolysis is an effective approach to improve long-term survival and functional status for patients suffering from ischemic stroke.2
Previous studies have shown that early intravenous alteplase treatment was significantly associated with clinical improvement and efficiency of care outcomes for ischemic stroke patients.3–5 In treating stroke patients, every minute counts on stroke thrombolysis and the goal is to “Save a Minute, Save a Day”.6 It has also been delayed in thrombolysis time metrics that were associated with worse neurological outcomes.7 However, there are still some factors contributing to delaying intravenous thrombolytic therapy, including pre-hospital and in-hospital factors.8 Previous studies have demonstrated that multidisciplinary collaboration and workflow optimization can shorten the Door-to-Needle-Time (DNT) and stroke treatment time.9,10
In order to prevent and treat stroke effectively, the Ministry of Health China Stroke Prevention Project Committee (CSPPC) was established in April 2011 in China.11 The 5th People’s Hospital of Foshan City was a comprehensive hospital in Foshan City, Guangdong Province, China. It has more than 500 beds, accommodates more than 1 million outpatient visits and 18,000 admissions annually. It provides medical services for more than 300,000 inhabitants. Since 24/11/2020, the hospital began to apply as a National Stroke Center. The aim of this study was to assess the impact of Participating National Stroke Center Construction projects on door-to-needle time (DNT). We hypothesized that participation in the National Stroke Center Construction project can result in reduced DNT and improved patient outcomes.
Materials and Methods
We retrospectively analyzed the data of the stroke center. The 5th People’s Hospital of Foshan City began to apply as the China National Stroke Center on 11/24/2020. We included all thrombolysis patients between 2/27/2019 and 11/30/2021. The data were divided into two groups (Pre-construction period 2/27/2019 to 11/23/2020) and (Construction period 11/24/2020 to 11/30/2021), as shown in Table 1.
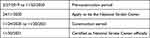 |
Table 1 Time Metrics of Participating in National Stroke Center Construction |
The data was derived from the China National Stroke Center system and Hospital’s electronic medical record system. The following data were collected: age, sex, risk factors of cerebrovascular disease, National Institute of Health Stroke Scale (NIHSS) admission, symptomatic intracranial hemorrhage (sICH), DNT, onset to needle time (ONT), onset to door time (ODT). Outcomes were evaluated by Modified Rankin Score (mRS) at 90 days.
The 5th People’s Hospital of Foshan City review board approved the study protocol. All patients were consented to do the thrombolysis. Written informed consent from the participants’ legal guardians/next of kin was not required to participate in this study per the national legislation and institutional requirements. The DNT and other factors were collected prospectively as China National Stroke Center projects’ requirements. All patient data were confidential, and all procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
A summary of measures for the National Stroke Center Construction is shown in Table 2.
 |
Table 2 A Summary of National Stroke Center Construction Measures |
In order to shorten the DNT of thrombolysis and improve stroke care, the hospital team spared no effort to find the causes of stroke care delays. The modified measures were conducted as shown in Table 2.
Statistical Analysis
BM SPSS version 27 (IBM-Armonk, NY) was performed to analyze the data. The normally distributed data are described as means with corresponding standard deviations (SD) and compared by the Student’s t-test. If the data were non-normally distributed continuously, it is compared by non-parametric Mann–Whitney U-test and reported as medians along with the interquartile range (IQR). P-values less than 0.05 were considered statistically significant.
Results
The patients were divided into Pre-Construction period and Construction period groups. As demonstrated in Table 3, there were 41 patients in the re-Construction period group and 47 in the Construction period groups. There was no statistical significance in age, sex, risk factors of cerebrovascular diseases, NIHSS Admission, and toast types between two groups.
 |
Table 3 Comparing the Baseline Information of Two Groups |
After participating in the National Stroke Center Project, effective measures were carried on. The thrombolysis treatment metrics were improved significantly as shown in Table 4.
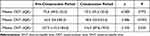 |
Table 4 Comparing the Time Metrics of Thrombolysis |
The DNT (IQR) was shortened from 65.0 (54.5,85.0) minutes in the Pre-Construction period to 40.0 (33.0,53.0) minutes in the Construction period (p < 0.001). Similarly, the ONT (IQR) was reduced from 157.0 (115.0,184.0) minutes to 116.0 (87.8,170.0) minutes (p = 0.035).
There are no significant differences in sICH, mRS discharge and mRS at 90 days as demonstrated in Table 5.
 |
Table 5 Comparing the Stroke Outcome of Two Period Groups |
Discussion
Our results revealed that the DNT in our center of thrombolysis could be shortened by 25 minutes from 65.0 minutes to 40.0 minutes. Similarly, ONT was shortened by 41 minutes from 157.0 minutes to 116.0. Compatible with other previous studies, the median DNT was reduced by participating in the National Stroke Center Programs.12 As time is the brain, every minute is precious for the thrombolysis of acute stroke patients.6 The delay factors of intravenous thrombolytic therapy include pre-hospital and in-hospital factors.8 Delaying factors were associated with stroke assessment, imaging time and thrombolysis administration.8 Atypical or mild symptoms, older, lower socioeconomic status, and living alone can contribute to longer onset to needle time.6 As it has been shown previously, treating patients by stroke thrombolysis is not only the neurology department’s responsibility but also requires multidisciplinary collaboration.9 Effective multiple Strategies can be conducted to shorten DNT in most centers to reach a median DNT of 30 minutes.12 As a previous study showed, through the China Stroke Center certification project, the annual rt-PA thrombolysis rates in South China increased from 1.4% to 7.2% from 2015 to 2020.11 Stroke thrombolysis should become more prevalent, and rt-PA was used more in stroke centers than that in non-stroke centers.11
Data from the China Stroke Center Data-Sharing Platform also showed that admission to stroke center hospitals was related to a lower risk of intracranial hemorrhage and mortality for acute ischemic stroke patients receiving thrombolytic therapy.13 Similarly, the New York Statewide Planning and Research Cooperative System also demonstrated that patients with acute ischemic stroke admitted to designated stroke center had lower mortality and higher frequency of use of intravenous thrombolysis.14
Endovascular therapy is effective for patients with comorbidities, including atrial fibrillation,15 and it can be used for predicting patient mortality.16,17 Based on these findings, we can suggest that the stroke center staff may provide more professional thrombolysis and stroke care. The DNT and ONT can be shortened by National Stroke Center Construction projects. More suitable hospitals should be encouraged to participate as part of the National Stroke Center.
The time from onset to reperfusion affects the favorable outcome and mortality in stroke patients, every effort should be taken to minimize that interval. For example, a previous study demonstrated that real-time feedback on mobile application use for emergency management reduced the DNT and improved the patient prognosis.18 In addition, another study in Norway used simulation and a revision of their protocol to provide training for the staff, which resulted in a shortened DNT.19 In our study, we demonstrated that DNT and ONT can be shortened by national projects by multidisciplinary health care and cooperation with resource allocation. Multidisciplinary health care and cooperation can be more practical and feasible to perform in some developing countries.
Our study has some limitations. This was a retrospective single-center study with a relatively moderate sample size of only 88 patients, which can bias the findings. Despite such limitations, our results can provide some insight from a stroke treatment perspective in a developing country to prompt other stroke treatment centers around the globe to adopt such measures. Future prospective large-scale studies are required to address these limitations, and to validate and expand these findings.
Conclusion
DNT and ONT can be shortened by National Stroke Center Construction projects. More suitable hospitals should be encouraged to participate as National Stroke Center.
Acknowledgments
We would like to thank all colleagues for data collection and stroke care for patients, all departments enrolled in the study, and patients for their contribution.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Burnier M, Fricker AF, Hayoz D, et al. Pharmacokinetic and pharmacodynamic effects of YM087, a combined V1/V2 vasopressin receptor antagonist in normal subjects. Eur J Clin Pharmacol. 1999;55:633–637. doi:10.1007/s002280050685
2. Muruet W, Rudd A, Wolfe CDA, Douiri A. Long-Term Survival After Intravenous Thrombolysis for Ischemic Stroke: a Propensity Score-Matched Cohort With up to 10-Year Follow-Up. Stroke. 2018;49(3):607–613. doi:10.1161/strokeaha.117.019889
3. Rajan SS, Decker-Palmer M, Wise J, Dao T, Salem C, Savitz SI. Beneficial effects of the 30-minute door-to-needle time standard for alteplase administration. Ann Clin Transl Neurol. 2021;8(8):1592–1600. doi:10.1002/acn3.51400
4. Nguyen TN, Fischer U. Treatment Effect of Intravenous Thrombolysis Bridging to Mechanical Thrombectomy on Vessel Occlusion Site. Stroke. 2022;53(1):17–19. doi:10.1161/strokeaha.121.037603
5. Masoud HE, de Havenon A, Castonguay AC, et al. 2022 Brief Practice Update on Intravenous Thrombolysis Before Thrombectomy in Patients With Large Vessel Occlusion Acute Ischemic Stroke: a Statement from Society of Vascular and Interventional Neurology Guidelines and Practice Standards (GAPS) Committee. Stroke. 2022;2(4):e000276. doi:10.1161/SVIN.121.000276
6. Meretoja A, Keshtkaran M, Saver JL, et al. Stroke thrombolysis: save a minute, save a day. Stroke. 2014;45(4):1053–1058. doi:10.1161/STROKEAHA.113.002910
7. Jillella DV, Nahab F, Nguyen TN, et al. Delays in thrombolysis during COVID-19 are associated with worse neurological outcomes: the Society of Vascular and Interventional Neurology Multicenter Collaboration. J Neurol. 2022;269(2):603–608. doi:10.1007/s00415-021-10734-z
8. Sharobeam A, Jones B, Walton-Sonda D, Lueck CJ. Factors delaying intravenous thrombolytic therapy in acute ischaemic stroke: a systematic review of the literature. J Neurol. 2021;268(8):2723–2734. doi:10.1007/s00415-020-09803-6
9. Chen Y, Nguyen TN, Wellington J, et al. Shortening Door-to-Needle Time by Multidisciplinary Collaboration and Workflow Optimization During the COVID-19 Pandemic. J Stroke Cerebrovasc Dis. 2022;31(1):106179. doi:10.1016/j.jstrokecerebrovasdis.2021.106179
10. Yang S, Yao W, Siegler JE, et al. Shortening door-to-puncture time and improving patient outcome with workflow optimization in patients with acute ischemic stroke associated with large vessel occlusion. BMC Emerg Med. 2022;22(1):136. doi:10.1186/s12873-022-00692-8
11. Chen Y, Li J, Dang C, et al. Impact of stroke center certification on rt-PA thrombolysis after acute ischemic stroke in South China from 2015 to 2020. Int J Stroke. 2022;17(5):559–565. doi:10.1177/17474930211031440
12. Chao BH, Yan F, Hua Y, et al. Stroke prevention and control system in China: CSPPC-Stroke Program. Int J Stroke. 2021;16(3):265–272. doi:10.1177/1747493020913557
13. Shen Y, Chao BH, Cao L, Tu WJ, Wang LD. Stroke Center Care and Outcome: results from the CSPPC Stroke Program. Transl Stroke Res. 2020;11(3):377–386. doi:10.1007/s12975-019-00727-6
14. Xian Y, Holloway RG, Chan PS, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011;305(4):373–380. doi:10.1001/jama.2011.22
15. Wu W, Pitton Rissardo J, Nguyen TN, et al. Effect of atrial fibrillation on outcomes in patients with anterior circulation occlusion stroke receiving endovascular therapy. Front Aging Neurosci. 2023;15:1160265. doi:10.3389/fnagi.2023.1160265
16. Chen Y, Diana F, Mofatteh M, et al. Functional and technical outcomes in acute ischemic stroke patients with hyperdense middle cerebral artery sign treated with endovascular thrombectomy. Front Neurol. 2023;14. doi:10.3389/fneur.2023.1150058
17. Chen Y, Zhou S, Yang S, et al. Developing and predicting of early mortality after endovascular thrombectomy in patients with acute ischemic stroke. Front Neurosci. 2022;16:1034472. doi:10.3389/fnins.2022.1034472
18. Reziya H, Sayifujiamali K, Han HJ, et al. Real-time feedback on mobile application use for emergency management affects the door-to-needle time and functional outcomes in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2023;32(4):107055. doi:10.1016/j.jstrokecerebrovasdis.2023.107055
19. Ajmi SC, Advani R, Fjetland L, et al. Reducing door-to-needle times in stroke thrombolysis to 13 min through protocol revision and simulation training: a quality improvement project in a Norwegian stroke centre. BMJ Qual Saf. 2019;28(11):939–948. doi:10.1136/bmjqs-2018-009117
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
