Back to Journals » International Journal of Women's Health » Volume 15
Impact of the COVID-19 Pandemic on Births, Vaginal Deliveries, Cesarian Sections, and Maternal Mortality in a Brazilian Metropolitan Area: A Time-Series Cohort Study
Authors Ferreira DP , Bolognani CV, Santana LA, Soares Fernandes SES, de Moraes MSF , Fernandes LAS , Pereira CDS , Ferreira GB , Göttems LBD, Amorim FF
Received 12 July 2023
Accepted for publication 23 October 2023
Published 4 November 2023 Volume 2023:15 Pages 1693—1703
DOI https://doi.org/10.2147/IJWH.S429122
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Dilson Palhares Ferreira,1,* Cláudia Vicari Bolognani,2,3,* Levy Aniceto Santana,2,* Sérgio Eduardo Soares Fernandes,2,3,* Matheus Serwy Fiuza de Moraes,3,* Luana Argollo Souza Fernandes,3,* Camila de Sousa Pereira,3,* Gabriela Billafan Ferreira,3,* Leila Bernarda Donato Göttems,2,3,* Fábio Ferreira Amorim1– 4,*
1Graduation Program in Health Sciences, University of Brasília (UnB), Brasília, Federal District, Brazil; 2Department of Research and Scientific Communication, Escola Superior de Ciências da Saúde (ESCS), Brasília, Federal District, Brazil; 3Medical School, Escola Superior de Ciências da Saúde (ESCS), Brasília, Federal District, Brazil; 4Graduation Program in Health Sciences of School Health Sciences, Escola Superior de Ciências da Saúde (ESCS), Brasília, Federal District, Brazil
*These authors contributed equally to this work
Correspondence: Fábio Ferreira Amorim; Dilson Palhares Ferreira, Coordenação de Pesquisa e Comunicação Científica - Escola Superior de Ciências da Saúde, SMHN Quadra 03, conjunto A, Bloco 1 - Edifício FEPECS, Brasília, Federal District, CEP 70701-907, Brazil, Email [email protected]; [email protected]
Purpose: The COVID-19 pandemic posed a worldwide challenge, leading to radical changes in healthcare. The primary objective of the study was to assess the impact of the COVID-19 pandemic on birth, vaginal delivery, and cesarian section (c-section) rates. The secondary objective was to compare the maternal mortality before and after the pandemic.
Patients and Methods: Time-series cohort study including data of all women admitted for childbirth (vaginal delivery or c-section) at the maternities in the Public Health System of Federal District, Brazil, between March 2018 and February 2022, using data extracted from the Hospital Information System of Brazilian Ministry of Health (SIH/DATASUS) on September 30, 2022. Causal impact analysis was used to evaluate the impact of COVID-19 on birth, vaginal delivery, and c-section using the CausalImpact R package, and a propensity score matching was used to evaluate the effect on maternal mortality rate using the Easy R (EZR) software.
Results: There were 150,617 births, and considering total births, the effect of the COVID-19 pandemic was not statistically significant (absolute effect per week: 5.5, 95% CI: − 24.0− 33.4). However, there was an increase in c-sections after COVID-19 (absolute effect per week: 18.1; 95% CI: 11.9− 23.9). After propensity score matching, the COVID-19 period was associated with increased maternal mortality (OR: 3.22, 95% CI: 1.53− 6.81). The e-value of the adjusted OR for the association between the post-COVID-19 period and maternal mortality was 5.89, with a 95% CI: 2.43, suggesting that unmeasured confounders were unlikely to explain the entirety of the effect.
Conclusion: Our study revealed a rise in c-sections and maternal mortality during the COVID-19 pandemic, possibly due to disruptions in maternal care. These findings highlight that implementing effective strategies to protect maternal health in times of crisis and improve outcomes for mothers and newborns is crucial.
Keywords: COVID-19, cesarean section, maternal health services, maternal mortality
Introduction
The COVID-19 pandemic posed a significant challenge for healthcare systems worldwide, rapidly infecting numerous individuals and causing substantial fatalities and persistent health issues before vaccines were available.1 The burden to manage COVID-19 led to notable changes in healthcare system provision, including the preventive suspension of elective surgeries, procedures, and outpatient appointments, along with redirecting healthcare services to manage COVID-19 cases.2,3 There is a consensus that the COVID-19 pandemic may have impacted population health conditions often not directly linked to the SARS-CoV-2 infection. Maternal health is of great interest in all conditions impacted by COVID-19 as it is a proxy indicator of the quality of a country’s healthcare services.4–7
As the COVID-19 pandemic continued to spread, there was a notable rise in cases of moderate to severe illness among pregnant women, leading to concerns about their susceptibility to infection and potential fatalities.4–6,8–11 Thus, beyond the fear of the possibility of vertical transmission, special attention was initially given to understanding the direct effects of COVID-19 on maternal health. Notably, the severity of infection during pregnancy was a primary area of concern, especially in women from high-risk groups, such as those with obesity, hypertension, diabetes, and immunosuppression conditions.1,6–11 In this aspect, a systematic review with meta-analysis including 42,754 infected pregnant patients showed a rapid increase in cesarian sections (c-sections); the mortality trend was not elucidated with a maternal mortality rate of 1.2% and a rise of preterm births.11
It is important to note that the impact of the pandemic on maternal health transcended the direct effects of individual infections. The indirect effects, such as the reduced access to and provision of maternal healthcare services and lower levels of their utilization due to fear of being infected, may lead to a significant impact on the quality of maternal care.5–12 Thus, apart from the direct effects of COVID-19 on maternal health, the interruption of maternal healthcare services provision during the pandemic, breaking the continuum of healthcare throughout antenatal, intrapartum, and postnatal stages, could adversely affect both mother and newborn health, including a rise in preterm births and maternal mortality.5–12
The adaptations made in antenatal and postnatal services, the modifications to provide maternity care can also influence intrapartum services. These modifications can involve changes to provide care for pregnant women during labor, including alterations in anesthesia practices and the approach to childbirth itself.5,8,12–16 Regarding the mode of birth, most studies have focused on assessing COVID-19-infected pregnant women.14,15 Furthermore, while the context of the COVID-19 pandemic may have led to an increase in pre-planned induced births and chosen c-sections compared to vaginal delivery, the evidence regarding the indirect impact of pandemic and lockdown measures on the mode of birth is inconsistent.5,8,9,16–18
Latin American countries were impacted harder by COVID-19 than observed in developed countries.7,19 Brazil was one of the most affected countries worldwide.7,20,21 After the first case of COVID-19 reported on February 26, 2020, in the city of São Paulo,22 COVID-19 initially spread to Brazil’s largest metropolitan areas in the Southeast. It quickly moved to other regions, starting in the North and Northeast, followed by the Midwest and South. In May 2020, the public healthcare system in Manaus, a city in the North with the least ICU beds, had already collapsed, foreshadowing the country’s severe pandemic from late 2020 to the end of 2021. The disease’s focal point shifted during the pandemic, resulting in three significant waves of infections and deaths from March 2020 to January 2022. By the end of 2022, Brazil had registered 36.3 million confirmed COVID-19 cases, constituting around 5% of global cases. It ranked second in deaths among countries, accounting for about 10% of worldwide COVID-related deaths.20,21 Factors contributing to the severe impact of COVID‐19 in Brazil involve inconsistent containment measures, delayed guidelines for COVID‐19 care, restricted health access, disparities among vulnerable populations, and the strain of the pandemic on an already strained and underfunded Brazilian public health system.22,23
In this scenario, the primary objective of this study is to assess the impact of the COVID-19 pandemic on birth, vaginal delivery, and c-section rates in a Brazilian metropolitan area. The secondary objective is to compare the maternal mortality before and after the pandemic.
Materials and Methods
Study Design
A time-series cohort study including all women admitted for childbirth (vaginal delivery or c-section) at the maternities in the Public Health System of Federal District (FD), Brazil, between March 2018 and February 2022. Data were obtained from the Hospital Information System in the Department of Informatics of the Brazilian Unified Health System (SIH/DATASUS), an audited nationwide database with information regarding every hospital admission performed in the healthcare services affiliated with the Brazilian public health system (SUS).24,25 The dataset was extracted from SIH/DATASUS on September 30, 2022.
Setting and Participants
The FD is a metropolitan area with 2,469,489 inhabitants that includes the city of Brasilia, the capital of Brazil, and has the highest Human Development Index (HDI) in Brazil. The first case of COVID-19 was reported on February 26, 2020, in the city of São Paulo.22 Soon after this case, COVID-19 spread to other Brazilian states, with the first COVID-19 case in the FD dated March 8, 2020. The state government established the first lockdown in the FD due to COVID-19 on March 18, 2020, when there were 36 confirmed cases and another 174 notifications to be evaluated. The lockdown measures included suspending non-essential activities and the closure of gyms, schools, and shopping centers, restricting people’s movement, and curbing the transmission of the virus. Thus, in this study, the pre-COVID-19 onset period was defined as between March 2018 and February 2020, and the post-COVID-19 onset period was between March 2020 and February 2022.
The public healthcare system of FD comprises 12 maternities in hospitals and one birth house. All information regarding admissions and procedures on these healthcare services needs to be provided in SIH/DATASUS to reimburse hospital-related procedures. Thus, the study included all women admitted for childbirth (vaginal delivery or c-section) at the hospital maternities and the birth house of the FD Public Health System between March 2018 and February 2022, informed in the SIH/DATASUS until September 30, 2022. No exclusion criteria were applied.
Data Collection
The SIH/DATASUS plays a pivotal role in processing and monitoring hospital admissions in the SUS and is responsible for managing hospital admission authorization forms, payments for hospital-related procedures and streamlining hospital oversight and audit functions, concurrently monitoring disbursements related to hospital admissions in Brazilian public healthcare services. Its database contains relevant parameterized information, including procedure code, hospital identification, and patient information, such as the city of residence, age, sex, admission and discharge date, and discharge status. Therefore, the SIH/DATASUS is widely used in epidemiological studies in Brazil.24,25
The variables collected from the SIH/DATASUS were maternal age, mode of birth (vaginal delivery or c-section), city of residence, maternal admission and discharge date, maternal length-of-stay (LOS), and discharge status (survivor or non-survivor).
Statistical Analysis
The distribution and normality of variables were checked using the Shapiro–Wilk test. Quantitative data are expressed as mean ± standard deviation (SD), median, and interquartile range (IQR25%–75%), and categorical variables are expressed as numbers and percentages.
Birth, Vaginal Delivery, and c-Section Rate Analysis
First, the total births, vaginal deliveries, and c-sections were calculated for each epidemiological week between March 2018 and February 2022. The trend of births, vaginal deliveries, and c-sections over the epidemiological weeks during the study period was initially evaluated using univariate linear regression analysis. The Cochran-Armitage test for trend in proportions was also performed to preliminarily compare the number of vaginal deliveries and c-sections between March 2018 and February 2019, March 2019 and February 2020, March 2020 and February 2021, and March 2021 and February 2022.
Then, the causal effects of COVID-19 onset on birth, vaginal delivery, and c-section rates were evaluated using causal impact analysis with the CausalImpact R package that applies a Bayesian structural time series model with predictor data sets to determine the likely trajectory of a trend line had a particular event not occurred (the COVID-19 pandemic) and then calculated the difference between that projected counterfactual trend line (if COVID-19 pandemic had not occurred) and the real data line (after the COVID-19 onset).19 As control variables in the model, the causal impact analysis of the COVID-19 pandemic on births was adjusted for the estimated population of the FD on each epidemiological week, and the causal impact analysis of the COVID-19 pandemic on c-sections was adjusted for the total births each epidemiological week.
The causal impact analysis extends the traditional interrupted time series (ITS) analysis by incorporating Bayesian structural time series models to adjust for seasonality and other factors. Thus, when an intervention or event occurs, the method estimates the causal effect by comparing the observed data to what would have been expected based on the model’s predictions. While the ITS analysis typically focuses on identifying the immediate impact of an intervention on a time series data set, causal impact analysis not only quantifies the intervention’s immediate effect but also provides a post-intervention counterfactual prediction, allowing for a more robust assessment of the causal effect. In this aspect, causal impact analysis accounts for various factors, including seasonality, by modeling the pre-intervention period using a Bayesian structural time series model. Thus, seasonal components, trends, and other time-varying covariates and patterns are captured in the model.26,27
Maternal Mortality Analysis
As the number of maternal deaths was too low during the study period, which poses challenges for conducting meaningful causal inference analysis for maternal mortality in maternity, impacting the analysis feasibility, reliability, and interpretability of causal inference analysis, we opted to use propensity score matching to evaluate the effect of the COVID-19 pandemic on maternal mortality.26,27
First, to evaluate the covariates considered for the propensity score matching, a univariate analysis was performed using Student’s t-test or Mann–Whitney test to evaluate quantitative variables associated with maternal mortality in maternity, as appropriate, and Pearson’s chi-square test (χ2) was used as necessary for categorical variables.
Thus, an enter method binary logistic regression analysis was used to evaluate independent factors associated with maternal mortality in maternity, including non-collinear variables associated with the outcome with a p-value < 0.05 in the univariate analysis and the confounding factors according to previous knowledge with a p-value < 0.20 in the univariate analysis. Non-collinearity was accepted when the tolerance was higher than 0.10 and the variance inflation factor (VIF) was lower than 10.0. The odds ratio (OR) expressed the results with their respective 95% confidence interval (95% CI).
Finally, a propensity score matching for maternal mortality in maternity applying a logit regression model adjusted to factors independently associated in the logistic regression analysis with maternal mortality in maternity was performed to assess the effect of COVID-19 on maternal mortality in maternity using the Easy R (EZR) software version 1.54 (Saitama Medical Center, Jichi Medical University, Japan) with a 1:1 pair-matching ratio without replacement on the logit of the propensity score applying a caliper of 0.2 widths. The OR and 95% CI of the COVID-19 effect on maternal mortality in maternity are calculated in the sample after matching and are shown as a forest plot.
For sensitivity analysis of the effect of the post-COVID-19 onset period on maternal mortality in maternity after propensity score matching, the e-value was used to measure the robustness of the association between COVID-19 and maternal mortality for unmeasured or unadjusted confounding, ie, a tool to evaluate the strength of the effected of another variable required to potentially overturn an observed effect estimate due to unmeasured or residual confounding. E-value was computed with an online e-value calculator (https://www.evalue-calculator.com/).28,29
Statistical analyses were performed using the IBM Statistical Package for the Social Sciences version 20.0 for Mac (SPSS 20.0 Mac, SPSS Inc., Chicago, Illinois, USA), Jamovi 2.3.24 (https://www.jamovi.org), and statistical software R version 4.2.3 (https://www.r-project.org/). Statistical significance was set at a two-sided p-value ≤ 0.05.
The study adhered to the principles outlined in the Declaration of Helsinki. Since DATASUS has no personal data, our study was exempt from review by the Brazilian National Research Ethics Committee (CONEP).
Results
Between March 2018 and February 2022, there were 150,617 births in the FD public health system, with 61,167 c-sections (40.6%). The mean maternal age was 26.8 ± 6.8 years (median: 26.0 years, IQR 25%–75%: 21.0–32.0 years), and the median maternity LOS was 3.0 days (IQR 25%–75%: 2.0–4.0). The maternal mortality rate was 0.0003% (40 out of 150,617 women). See Supplementary Table S1.
Supplementary Figure S1 shows the number of births, vaginal deliveries, and c-sections per epidemiological week from March 2018 to February 2022. During the study period, the number of vaginal and total births decreased (r = −0.552, 95% CI: −0.552−-0.361, p < 0.001; r = −0.718, 95% CI: −0.548−-0.419, p = 0.271, respectively), whereas the number of c-sections did not change significantly (r = 0.077, 95% CI: −0.021–0.075, p = 0.271).
Figure 1 shows a causal impact analysis of the COVID-19 pandemic on the total births in the FD public health system over the study period, adjusted for the FD population. After the onset of COVID-19 in Brazil in March 2020, there were 72,948 births, compared to 71,488 births expected if the COVID-19 pandemic had not occurred (95% CI: 68,818–74,531 births). After adjusting for the FD population over the study period, the effect of the COVID-19 pandemic on births was not statistically significant when considering the entire period after the COVID-19 onset as a whole, with an absolute effect per epidemiological week of 5.5 births (95% CI: −24.0–33.4 births) and a relative effect of 0.9% (95% CI: −3.3–5.5%).
Although the COVID-19 pandemic did not affect total births in the FD public health system, there was an increase in c-sections compared to vaginal deliveries after the COVID-19 outbreak in March 2020 (p < 0.001). See Figure 2.
Figure 3 shows a causal impact analysis of the COVID-19 pandemic on the total number of c-sections in the FD public health system over the study period, adjusted for the total births. After the onset of COVID-19 in Brazil in March 2020, there were 30,462 c-sections in the FD public health system, compared to 28,596 c-sections expected if the COVID-19 pandemic had not occurred (95% CI: 28,000–29,233 C-sections). The causal impact analysis of the COVID-19 pandemic on c-sections, adjusted for the total births over the study period, revealed a statistically significant effect when considering the entire period after the COVID-19 onset as a whole, with an absolute effect per epidemiological week of 18.1 c-sections (95% CI: 11.9–23.9 c-sections) and a relative effect of 6.6% (95% CI: 4.2–8.8%).
Supplementary Table S2 shows the univariate analysis of maternal age and maternity LOS among births in the FD public health system before and after COVID-19 onset. Maternal age was higher (p < 0001), and maternity LOS was lower (p < 0.001) after the COVID-19 onset.
Supplementary Table S3 shows the univariate analysis of variables associated with maternal mortality in maternity. The c-section (p < 0.002) and post-COVID-19 onset period (p < 0.001) were associated with increased maternal mortality in maternity.
Table 1 shows the multivariate analysis of variables associated with maternal mortality in maternity. The c-section (OR: 3.10, 95% CI: 1.51–6.34, p = 0.002) and post-COVID-19 onset period (OR: 2.62, 95% CI: 1.37–5.03, p = 0.04) were independently associated with increased maternal mortality in maternity.
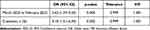 |
Table 1 Multivariate Analysis of Variables Associated with Maternal Mortality |
Figure 4 shows the effect of the post-COVID-19 onset period (March 2020 to February 2022) on maternal mortality in maternity after propensity score matching adjusted for c-section and age. COVID-19 was associated with increased maternal mortality in maternity (OR: 3.22, 95% CI: 1.53–6.81, p = 0.02).
 |
Figure 4 Effect of the post-COVID period (March 2020 to February 2020) on maternal mortality in maternity after propensity score-matching adjusted to c-section and age. |
For sensitive analysis of the effect of the post-COVID-19 onset period on maternal mortality in maternity after propensity score matching, the e-value of the adjusted OR for the association between the post-COVID-19 period and maternal mortality in maternity was 5.89, with a 95% CI of 2.43, suggesting that unmeasured confounders were unlikely to explain the entirety of the effect.
Discussion
Our study showed that the total births in the public maternities of FD was unaffected by the COVID-19 pandemic. However, there was an increase in c-sections compared to the counterfactual prediction if the COVID-19 pandemic had not occurred. Additionally, there was increased maternal mortality when comparing the pre-and post-COVID-19 periods. These findings may not only reflect the adaptations made in maternity units but also highlight the limitations in the provision and utilization of maternal healthcare services, which have had a detrimental impact on the continuity of maternal care.4–6
Although there was no alteration in the recommendations for the mode of birth during the pandemic, with vaginal delivery remaining the preferred approach and c-sections reserved for standard indications based on fetal and maternal factors, the observed increase in c-sections during this period can be attributed to various factors. The fear of contracting COVID-19 at healthcare facilities may have contributed to a hesitancy in timely referrals to emergency care units. These delayed referrals may have complicated the management of laboring women, particularly when facing obstetrical complications, thereby increasing the likelihood of resorting to a c-section. Moreover, some obstetricians may hesitate to expose themselves, their trainees, and midwives to pregnant patients whose PCR status is unknown. This cautionary approach may manifest as a preference for c-sections even when vaginal delivery would have been a more feasible choice. Furthermore, the threshold for opting for c-sections during the COVID-19 pandemic may have been lowered to minimize the duration of maternal hospitalization and mitigate the potential for cross-infection. Additionally, some pregnant women may have chosen to undergo a c-section out of fear of COVID-19 and due to restrictions on their partners’ access to maternity.16,30–32
Similar to our findings, a study conducted in Iran reported a significant increase in the overall c-section rate during the initial wave of the COVID-19 pandemic.33 Another Brazilian study showed increased c-sections in all gestational age groups and a higher risk of preterm babies during the COVID-19 pandemic.7 A study during the COVID-19 lockdown period in India observed a significantly higher c-section rate than the pre-lockdown period.34 Two studies in England, one study in Turkey, one study in Nepal, and one study in China also showed a rise in the overall c-section rate during the pandemic.17,35–38 However, it is worth noting that other studies have presented conflicting results compared to our study regarding the mode of birth. Some studies have shown no significant change,22,39–44 while others have even reported an increase in vaginal deliveries.5 A systematic review with meta-analysis published in 2021, including 11 studies, did not find a significant difference in the c-section rate during the COVID-19 pandemic.8
Interestingly, a study performed at a Brazilian tertiary hospital in São Paulo, Brazil, during the initial surge of the COVID-19 pandemic in 2020, observed a significant increase in the number of pregnant patients admitted to the hospital in the advanced stages of labor. This trend was particularly evident among pregnant women who had initially been advised to undergo elective c-sections due to abnormal fetal presentation or previous c-sections.45 It is plausible that this phenomenon was linked to the fear of exposure to COVID-19, prompting these women to commence labor at home.45–47 In contrast to the increase in c-sections observed in our study, this finding raises an intriguing question and highlights the importance of considering the unique characteristics of the population evaluated in each study. It is important to note that the study in question was conducted on maternity at a specialized university hospital that serves a larger population of women with high-risk pregnancies. Additionally, the city where the study took place confronts formidable obstacles to urban transportation, thereby impeding the timely referral of pregnant individuals to maternity services compared to the FD. This is further compounded by reduced public transportation options during the pandemic. Consequently, many pregnant women were admitted to the hospital in a more advanced phase of labor, ultimately resulting in vaginal deliveries.45 Indeed, a study in India observed a delay in seeking health care from pregnant women and a reduction in institutional births due to either inaccessibility, lack of transport, or fear of contracting infection.46
Our study identified an elevated incidence of maternal mortality in maternity during COVID-19. Notably, another Brazilian study analyzing national data on maternal mortality revealed a notable surplus of maternal deaths during the post-pandemic period following the emergence of COVID-19 in 2020, persisting even after considering the expected rise in mortality among women of reproductive age due to COVID-19,48 which was also observed in a time-series study in the Brazilian state of Bahia.49 These results align with two studies conducted in middle-income countries, India and Mexico, which also reported a significant surge in maternal deaths during the COVID-19 pandemic.34,50 Another study in India showed increased non-COVID-19 maternal mortalities during the COVID pandemic.51 Indeed, a systematic review with meta-analysis published in 2021 observed a significant increase in maternal death during the COVID-19 pandemic.8
Timely access to adequate maternity care is essential for women’s safety and quality of care, as the delay in receiving care is associated with adverse maternal outcomes.52 These findings indicate the presence of additional maternal deaths indirectly linked to COVID-19 can be attributed to the challenges encountered by healthcare systems in effectively managing the impact of the COVID-19 pandemic on the continuum of maternal care, including prenatal care, suitable childbirth, and postpartum care.8 These challenges encompass a range of factors, such as reduced attendance for routine prenatal care and change in maternity care service provision, resulting in limited access to maternal care services.39,42,46,53–56 Indeed, many pregnant women refrained from seeking healthcare services due to concerns about the risk of contracting COVID-19, government recommendations to stay at home, and limited availability of public transportation during periods of lockdown.46,57 Furthermore, a time-series study in Colombia showed increased maternal mortality, particularly pronounced in municipalities with the lowest wealth quintile. This finding shows the heightened vulnerability of women with lower income and disadvantaged living conditions, emphasizing the exacerbation of healthcare access inequities during the COVID-19 pandemic.58
Our study did not show difference in the number of births in the public maternities of FD comparing the pre- and post-COVID-19 pandemic period that was also observed in a study performed in Ethiopia.55 However, it is important to analyze this finding within the context of how the pandemic has impacted healthcare services in different locations. Some studies have reported a decrease in hospital births, particularly during periods of strict lockdown and in regions where the healthcare system was under significant strain due to high numbers of COVID-19 cases.32,34,35,41,42,46,51,56 In this aspect, the decline in births conducted in healthcare facilities may be attributed to a variety of factors, such as women may opt for home or at nearby healthcare facilities births due to factors such as limited accessibility, lack of transportation, and fear of infection in maternity.32,46,51,59
Our study has some limitations. Firstly, the lacked of information on the specific indications for c-sections, pregnancy complications, waiting time before being admitted and receiving care, and the complete demographic characteristics of the women, including their education and socio-economic status. Additionally, there was no data on the prevalence of COVID-19 among the study population, and our analysis was only limited to births in maternities. Furthermore, it is important to acknowledge that other factors not considered in our study could have influenced the group outcomes. While the absence of information on these variables is a limitation, the sensitivity analysis of the effect of the post-COVID-19 onset period on maternal mortality in maternity after propensity score matching using the e-value suggests that unmeasured confounders were unlikely to entirely explain the observed impact on maternal mortality to the point of modifying the observed results.28,29 Regarding the causal impact analysis, the impact of COVID-19 on births, vaginal deliveries, and c-sections was evaluated from the combination of three elements: a regression component that relates the outcome of the COVID-19 period to the outcomes on counterfactual prevision, a time-series component capturing temporal patterns in the data, and an error element considering any unpredicted variation. Despite its strengths, there are limitations to the use of the causal impact analysis. Specifically, the underlying time-series model usually involves numerous unknown parameters, necessitating substantial data to estimate these parameters, including the counterfactual prediction accurately. In our study, 150,617 births were included. Further, the performance of the causal impact can be impacted if the outcome of interest is subject to measurement errors. However, this does not apply to the outcomes evaluated in our study.26,27
Conclusion
Our study revealed the detrimental impact of the COVID-19 pandemic on maternal care, specifically an increase in maternal mortality and c-section rates following the onset of the pandemic. These findings highlight the indirect consequences of COVID-19 on the continuum of maternal care. It is crucial to implement effective strategies to mitigate the long-term impact of COVID-19 on maternal health and enhance the overall health outcomes for both mothers and newborns.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res. 2020;25(1):39. doi:10.1186/s40001-020-00439-w
2. Rodriguez-Llanes JM, Castro Delgado R, Pedersen MG, Meneghini M, Arcos González P. Surging critical care capacity for COVID-19: key now and in the future. Prog Disaster Sci. 2020;8:100136. doi:10.1016/j.pdisas.2020.100136
3. Stirparo G, Oradini-Alacreu A, Migliori M, et al. Public health impact of the COVID-19 pandemic on the emergency healthcare system. J Public Health. 2022;44(1):e149–e152. doi:10.1093/pubmed/fdab212
4. Takemoto MLS, Menezes MO, Andreucci CB, et al. Maternal mortality and COVID-19. J Matern Fetal Neonatal Med. 2022;35(12):2355–2361. doi:10.1080/14767058.2020.1786056
5. Esposito G, Rossi M, Favilli A, et al. Impact of the first and second lockdown for COVID-19 pandemic on preterm birth, low birth weight, stillbirth, mode of labor, and of delivery in Lombardy, Italy. J Pers Med. 2023;13(3):499. doi:10.3390/jpm13030499
6. Galle A, Kavira G, Semaan A, Malonga Kaj F, Benova L, Ntambue A. Utilisation of services along the continuum of maternal healthcare during the COVID-19 pandemic in Lubumbashi, DRC: findings from a cross-sectional household survey of women. BMJ Open. 2023;13(6):e069409. doi:10.1136/bmjopen-2022-069409
7. Charles CM, Souza Neto LA, Soares CF, et al. Preterm births prevalence during the COVID-19 pandemic in Brazil: results from the national database. Sci Rep. 2023;13(1):14580. doi:10.1038/s41598-023-37871-x
8. Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. 2021;9(6):e759–e772. doi:10.1016/S2214-109X(21)00079-6
9. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi:10.1016/S0140-6736(20)30360-3
10. Papapanou M, Papaioannou M, Petta A, et al. Maternal and neonatal characteristics and outcomes of COVID-19 in pregnancy: an overview of systematic reviews. Int J Environ Res Public Health. 2021;18(2):596. doi:10.3390/ijerph18020596
11. Marchand G, Patil AS, Masoud AT, et al. Systematic review and meta-analysis of COVID-19 maternal and neonatal clinical features and pregnancy outcomes up to June 3, 2021. AJOG Glob Rep. 2022;2(1):100049. doi:10.1016/j.xagr.2021.100049
12. Lucas DN, Bamber JH. Pandemics and maternal health: the indirect effects of COVID-19. Anaesthesia. 2021;76(Suppl S4):69–75. doi:10.1111/anae.15408
13. Jardine J, Relph S, Magee LA, et al. Maternity services in the UK during the coronavirus disease 2019 pandemic: a national survey of modifications to standard care. BJOG. 2021;128(5):880–889. doi:10.1111/1471-0528.16547
14. Debrabandere ML, Farabaugh DC, Giordano C. A review on mode of delivery during COVID-19 between December 2019 and April 2020. Am J Perinatol. 2021;38(4):332–341. doi:10.1055/s-0040-1721658
15. Di Toro F, Gjoka M, Di Lorenzo G, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(1):36–46. doi:10.1016/j.cmi.2020.10.007
16. Li M, Yin H, Jin Z, et al. Impact of Wuhan lockdown on the indications of cesarean delivery and newborn weights during the epidemic period of COVID-19. PLoS One. 2020;15(8):e0237420. doi:10.1371/journal.pone.0237420
17. Bhatia K, Columb M, Bewlay A, et al. The effect of COVID-19 on general anaesthesia rates for caesarean section. A cross-sectional analysis of six hospitals in the north-west of England. Anaesthesia. 2021;76(3):312–319. doi:10.1111/anae.15313
18. Bornstein E, Gulersen M, Husk G, et al. Early postpartum discharge during the COVID-19 pandemic. J Perinat Med. 2020;48(9):1008–1012. doi:10.1515/jpm-2020-0337
19. Lima EEC, Vilela EA, Peralta A, et al. Investigating regional excess mortality during 2020 COVID-19 pandemic in selected Latin American countries. Genus. 2021;77(1):30. doi:10.1186/s41118-021-00139-1
20. Worldometer. Coronavirus Cases [Internet]. Available from: https://www.worldometers.info/coronavirus/.
21. Sunahara AS, Pessa AAB, Perc M, Ribeiro HV. Complexity of the COVID-19 pandemic in Maringá. Sci Rep. 2023;13(1):12695. doi:10.1038/s41598-023-39815-x
22. Silva LLSD, Lima AFR, Polli DA, et al. Social distancing measures in the fight against COVID-19 in Brazil: description and epidemiological analysis by state. Cad Saude Publica. 2020;36(9):e00185020. PMID: 32965378. doi:10.1590/0102-311X00185020
23. Menezes MO, Takemoto MLS, Nakamura-Pereira M, et al. Risk factors for adverse outcomes among pregnant and postpartum women with acute respiratory distress syndrome due to COVID-19 in Brazil. Int J Gynaecol Obstet. 2020;151(3):415–423. doi:10.1002/ijgo.13407
24. Rocha TAH, Silva NCD, Amaral PVM, et al. Geolocation of hospitalizations registered on the Brazilian National Health System’s Hospital Information System: a solution based on the R Statistical Software. Epidemiol Serv Saude. 2018;27(4):e2017444. doi:10.5123/S1679-49742018000400016
25. Figueiredo FWDS, Almeida TCDC, Schoueri JHM, Luisi C, Adami F. Association between primary care coverage and breast cancer mortality in Brazil. PLoS One. 2018;13(8):e0200125. doi:10.1371/journal.pone.0200125
26. Brodersen KH, Gallusser F, Koehler J, Remy N, Steven L, Scott SL. Inferring causal impact using bayesian structural time-series models. Ann Appl Stat. 2015;9(1):274. doi:10.1214/14-AOAS788
27. Samartsidis P, Martin NN, De Gruttola V, et al. Evaluating the power of the causal impact method in observational studies of HCV treatment as prevention. Stat Commun Infect Dis. 2021;13(1):20200005. doi:10.1515/scid-2020-0005
28. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–274. doi:10.7326/M16-2607
29. Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Web site and R package for computing E-values. Epidemiology. 2018;29(5):e45–e47. doi:10.1097/EDE.0000000000000864
30. Arab W, Atallah D. Cesarean section rates in the COVID-19 era: false alarms and the safety of the mother and child. Eur J Midwifery. 2021;5:14. doi:10.18332/ejm/134998
31. Qi H, Luo X, Zheng Y, et al. Safe delivery for pregnancies affected by COVID-19. BJOG. 2020;127(8):927–929. doi:10.1111/1471-0528.16231
32. Khalil A, von Dadelszen P, Draycott T, Ugwumadu A, O’Brien P, Magee L. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324(7):705–706. doi:10.1001/jama.2020.12746
33. Gharacheh M, Kalan ME, Khalili N, Ranjbar F. An increase in cesarean section rate during the first wave of COVID-19 pandemic in Iran. BMC Public Health. 2023;23(1):936. doi:10.1186/s12889-023-15907-1
34. Kumari V, Mehta K, Choudhary R. COVID-19 outbreak and decreased hospitalisation of pregnant women in labour. Lancet Glob Health. 2020;8(9):e1116–e1117. doi:10.1016/S2214-109X(20)30319-3
35. Kc A, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8(10):e1273–e1281. doi:10.1016/S2214-109X(20)30345-4
36. Yalçin SS, Boran P, Tezel B, et al. Effects of the COVID-19 pandemic on perinatal outcomes: a retrospective cohort study from Turkey. BMC Pregnancy Childbirth. 2022;22(1):51. doi:10.1186/s12884-021-04349-5
37. Xue RH, Li J, Chen L, et al. Alternations of cesarean section rates in a non-infected population after the outbreak of COVID-19: a cross-sectional study. Psychol Health Med. 2022;27(9):1877–1883. doi:10.1080/13548506.2021.1893768
38. Gurol-Urganci I, Waite L, Webster K, et al. Obstetric interventions and pregnancy outcomes during the COVID-19 pandemic in England: a nationwide cohort study. PLoS Med. 2022;19(1):e1003884. doi:10.1371/journal.pmed.1003884
39. Gu XX, Chen K, Yu H, Liang GY, Chen H, Shen Y. How to prevent in-hospital COVID-19 infection and reassure women about the safety of pregnancy: experience from an obstetric center in China. J Int Med Res. 2020;48(7):300060520939337. doi:10.1177/0300060520939337
40. Greene NH, Kilpatrick SJ, Wong MS, Ozimek JA, Naqvi M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2(4):100234. doi:10.1016/j.ajogmf.2020.100234
41. Hui PW, Ma G, Seto MTY, Cheung KW. Effect of COVID-19 on delivery plans and postnatal depression scores of pregnant women. Hong Kong Med J. 2021;27(2):113–117. doi:10.12809/hkmj208774
42. Justman N, Shahak G, Gutzeit O, et al. Lockdown with a price: the impact of the COVID-19 pandemic on prenatal care and perinatal outcomes in a Tertiary Care Center. Isr Med Assoc J. 2020;22(9):533–537.
43. Long JE, Wanje G, Aliyan N, et al. Impact of the COVID-19 pandemic on obstetrical care at a tertiary care facility in Mombasa, Kenya: time-series analyses and staff perspectives. PLOS Glob Public Health. 2023;3(4):e0001829. doi:10.1371/journal.pgph.0001829
44. Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynaecol Obstet. 2020;150(2):184–188. doi:10.1002/ijgo.13249
45. Sun SY, Guazzelli CAF, de Morais LR, et al. Effect of delayed obstetric labor care during the COVID-19 pandemic on perinatal outcomes. Int J Gynaecol Obstet. 2020;151(2):287–289. doi:10.1002/ijgo.13357
46. Goyal M, Singh P, Singh K, Shekhar S, Agrawal N, Misra S. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2021;152(2):231–235. doi:10.1002/ijgo.13457
47. Corbett GA, Milne SJ, Hehir MP, Lindow SW, O’connell MP. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;249:96–97. doi:10.1016/j.ejogrb.2020.04.022
48. Guimarães RM, Reis LGC, Gomes MASM, Magluta C, de Freitas CM, Portela MC. Tracking excess of maternal deaths associated with COVID-19 in Brazil: a nationwide analysis. BMC Pregnancy Childbirth. 2023;23(1):22. doi:10.1186/s12884-022-05338-y
49. de Carvalho-Sauer RCO, Costa MDCN, Teixeira MG, et al. Impact of COVID-19 pandemic on time series of maternal mortality ratio in Bahia, Brazil: analysis of period 2011–2020. BMC Pregnancy Childbirth. 2021;21(1):423. doi:10.1186/s12884-021-03899-y
50. Lumbreras-Marquez MI, Campos-Zamora M, Seifert SM, et al. Excess maternal deaths associated with Coronavirus disease 2019 (COVID-19) in Mexico. Obstet Gynecol. 2020;136(6):1114–1116. doi:10.1097/AOG.0000000000004140
51. Chaurasia A, Gupta D, Shweta K, Srivastava Y. Impact of COVID-19 pandemic on non-COVID-19 maternal mortalities in a Tertiary Health Care Center of North India. J Obstet Gynaecol India. 2023;73(3):201–207. doi:10.1007/s13224-022-01734-8
52. Pacagnella RC, Cecatti JG, Parpinelli MA, et al. Delays in receiving obstetric care and poor maternal outcomes: results from a national multicentre cross-sectional study. BMC Pregnancy Childbirth. 2014;14:159. doi:10.1186/1471-2393-14-159
53. Khalil A, von Dadelszen P, Kalafat E, et al. Change in obstetric attendance and activities during the COVID-19 pandemic. Lancet Infect Dis. 2021;21(5):e115. doi:10.1016/S1473-3099(20)30779-9
54. Peahl AF, Powell A, Berlin H, et al. Patient and provider perspectives of a new prenatal care model introduced in response to the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. 2021;224(4):384.e1–384.e11. doi:10.1016/j.ajog.2020.10.008
55. Abdela SG, Berhanu AB, Ferede LM, van Griensven J. Essential Healthcare Services in the Face of COVID-19 prevention: experiences from a Referral Hospital in Ethiopia. Am J Trop Med Hyg. 2020;103(3):1198–1200. doi:10.4269/ajtmh.20-0464
56. Dell’Utri C, Manzoni E, Cipriani S, et al. Effects of SARS Cov-2 epidemic on the obstetrical and gynecological emergency service accesses. What happened and what shall we expect now? Eur J Obstet Gynecol Reprod Biol. 2020;254:64–68. doi:10.1016/j.ejogrb.2020.09.006
57. Biviá-Roig G, La Rosa VL, Gómez-Tébar M, et al. Analysis of the impact of the confinement resulting from COVID-19 on the lifestyle and psychological wellbeing of Spanish pregnant women: an Internet-Based Cross-Sectional Survey. Int J Environ Res Public Health. 2020;17(16):5933. doi:10.3390/ijerph17165933
58. Castañeda-Orjuela C, Hilarion Gaitan L, Diaz-Jimenez D, Cotes-Cantillo K, Garfield R. Maternal mortality in Colombia during the COVID-19 pandemic: time series and social inequities. BMJ Open. 2023;13(4):e064960. doi:10.1136/bmjopen-2022-064960
59. Verhoeven CJM, Boer J, Kok M, Nieuwenhuijze M, de Jonge A, Peters LL. More home births during the COVID-19 pandemic in the Netherlands. Birth. 2022;49(4):792–804. doi:10.1111/birt.12646
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



