Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Impact of the Accreditation Program of the Saudi Central Board for Accreditation of Healthcare Institutions on the Safety Dimension of the Institute of Medicine Quality
Authors Alsaedi A , Sukeri S, Yaccob NM, Almazroea A
Received 3 March 2023
Accepted for publication 21 April 2023
Published 28 April 2023 Volume 2023:16 Pages 1179—1190
DOI https://doi.org/10.2147/JMDH.S410925
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Abdulaziz Alsaedi,1 Surianti Sukeri,2 Najib Majdi Yaccob,3 Abdulhadi Almazroea4
1Medical Services, NGHA, Madinah, Saudi Arabia; 2Department of Community Medicine, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia; 3Unit of Biostatistics and Research Methodology, School of Medical Sciences, Universiti Sains Malaysia, Kubang Kerian, Kelantan, Malaysia; 4Medical College, Taibah University, Madinah, Saudi Arabia
Correspondence: Najib Majdi Yaccob, School of Medical Sciences, Health Campus, Universiti Sains Malaysia, Kubang Kerian, Kelantan, 16150, Malaysia, Tel +6097673000, Fax +6097673370, Email [email protected]
Background: Although hospital accreditation is recognized as a tool for improving healthcare, there are inconsistent results regarding its impact on healthcare quality. In Saudi Arabia, it is mandatory for all Ministry of Health (MOH) hospitals to be accredited by the Central Board for Accreditation of Healthcare Institutions (CBAHI).
Purpose: This study measured the impact of the CBAHI accreditation program on the Institute of Medicine’s (IOM) safety dimension in Madinah.
Methods: A cross-sectional study was conducted using retrospective data gathered from a review of hospital records over 60 months (ie, 12 months before, 36 during, and 12 post-accreditation). The data were analyzed using piecewise (segmented) regression analysis.
Results: The three indicators (ie: incident reports, medication errors, and nosocomial infection) were continuously improved compared to the data before accreditation, as a results of implementing the CBAHI accreditation program. Therefore, the CBAHI had a significantly positively impacts on MOH hospitals’ safety dimension.
Conclusion: Complying with the CBAHI standards can help reduce the rates of incident reports, medication errors, nosocomial infections, and post-admission mortality. This study provides insight for MOH hospitals and opportunities to expand the accreditation program to improve the quality of healthcare services.
Keywords: healthcare, hospital accreditation, quality of care, safety, Saudi Arabia
Introduction
Healthcare organizations are under pressure to improve the quality of services they provide.1 Avedis Donabedian defined the quality of care as
The kind of care that is expected to maximize an inclusive measure of patient welfare, after taking into account the balance of expected gains and losses that attend the process of care process in all its parts.2
The Institute of Medicine (IOM), is a US-based private and not-for-profit organization, aiming to improve the quality of healthcare.3 In 1999, the IOM released a disturbing report on healthcare safety.3 According to their findings, up to 98,000 people die annually due to preventable medical errors. This figure exceeds the number of deaths caused by car accidents, breast cancer, and AIDS collectively. Consequently, the issue of patient safety and quality of care has moved to the top of the healthcare reform agenda.4
The IOM has developed six goals to overcome these challenges and to improve the quality of care including: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity.5 The safety dimension refers to protecting patients from injuries resulting from care intended to improve their health status.6 Several clinical indicators were used to assess the safety dimension in healthcare. Some studies used the hospital infection rate, for instance, Janati et al.7 Mumford et al8 and Almasabi and Thomas.9 Others were found that measured the rate of medication errors, such as Devkaran and O’Farrell;10 and Abduljawad.11 While some studies looked at other incident reports as an indicator for the safety dimensions, such as Abduljawad,11 Janati et al.7
Consequently, healthcare decision-makers require a robust tool to improve healthcare quality in hospitals.12 Hospital accreditation is perceived as a tool for improving the quality of care.6,13,14 It is defined as
an external review process to assess how well a healthcare organization performs relative to pre-established standards covering the organization’s structure, process, and outcome.15
However, the literature shows inconsistent findings regarding the effects of accreditation on the safety dimension. A South Korea-based mixed-methods study revealed a positive correlation between the Joint Commission International’s implementation and patient safety measures.16 Another study found a highly positive effect of hospital accreditation on patient safety.17 Similarly, safety measures improved during the accreditation process.12 Moreover, hospitals with higher accreditation scores were found to have higher rates of staphylococcus aureus bacteremia.8
In contrast, a survey revealed that participation in hospital accreditation was not associated with improved ulcer performance measures.15 Similarly, the Saudi Central Board for Accreditation on Healthcare Institutions’ (CBAHI) quality of care was investigated, and revealed that the accreditation had improved the care procedure. However, no improvement was seen in hospital nosocomial infections.9 Similarly, both positive and negative effects were found on the quality of care regarding the measurement of pressure ulcers and the rate of nosocomial infection.7
The Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI) is a not-for-profit organization established in October 2005.18 It is the only legally recognized institution in Saudi Arabia that evaluates all governmental and private healthcare providers and awards accreditation certificates.19 The first set of its national standards was developed and disseminated in 2006.19 In 2012, the CBAHI published its second edition of hospital standards, which were published in cooperation with experts from the public and private sectors.20 Currently, the CBAHI provides accreditation for hospitals, primary healthcare centers, clinical laboratories, and ambulatory healthcare centers, while another twelve accreditation programs are being implemented.21
After the troubling IOM report released, the International Society for Quality in Health Care (ISQua) developed a set of principles based on the six IOM quality dimensions.22 All national or international accrediting bodies who want to gain a certificate from ISQua must adhere to these standards. The CBAHI agency has already complied with these standards and received ISQua accreditation.23 Thus, the IOM quality dimensions, safety, and the CBAHI standards are intimately related.
A literature review found only two studies on the CBAHI accreditation program.6,24 However, neither of them examined the impact of the accreditation program on IOM’s safety dimension. Moreover, neither considered changes in the safety dimension during the accreditation journey. Previous findings were deemed inconsistent by the review because of the limited studies assessing the impact of the CBAHI on the healthcare quality.
Moreover, none of the studies used a piecewise (segmented) regression analysis to enhance the understanding of the effects of the CBAHI accreditation program on quality dimensions during the accreditation lifecycle (ie, pre-, during, and post-accreditation). Furthermore, some previous studies found no noticeable effects on healthcare accreditation programs, while others revealed significantly positive results. Hence, a research gap exists as the role of healthcare accreditation programs in improving care quality remains inconclusive.25 Therefore, our study aimed to measure the effects of the Saudi CBAHI accreditation program on IOM’s safety dimension at Ministry of Health (MOH) hospitals in Madinah.
Materials and Methods
This study used a cross-sectional design based on retrospective data collected from a review of hospital records. We included all CBAHI-accredited MOH hospitals in Madinah operating during the study period. Furthermore, we excluded CBAHI-accredited MOH hospitals not possessing sufficiently recorded pre-, during, and post-accreditation data. Only five hospitals met the criteria; therefore, no sample size calculation was performed because all the study population (ie, five hospitals) were selected. Background information on the five hospitals is provided in Table 1.
 |
Table 1 Background Information on the Five CBAHI-Accredited Hospitals in Madinah |
Data Source
Secondary data on monthly clinical indicators were obtained from the Hospital Quality Management Department, Infection and Prevention Control, and the Department of Statistics at every hospital. The monthly data on clinical indicators were received for one-year pre-accreditation, three years during the preparation for accreditation, and one-year post-accreditation.
Research Tool
The data for the IOM safety dimension were gathered using secondary data proforma, which included the following measures: rates of incident reports, medication errors, and nosocomial infections. The incident rate refers to any event occurring to patients or staff inside the hospital. It was calculated by the sum of events, adverse and sentinel events, or near misses reported to each hospital’s quality management department. Medication errors are healthcare providers’ errors in ordering, transcribing, dispensing, administering, or monitoring drugs. It was measured by the number of reported medication errors each month. The rate of nosocomial infections refers to infections found in patients that were not present at the time of admission to the hospital. An infection discovered 48 h after admission is usually considered a nosocomial infection.
Data on monthly hospital clinical indicators were collected and analyzed to achieve the study objectives. Previous studies have highly recommended using clinical indicators to assess the effects of healthcare accreditation programs on the quality of care.26
Data Collection
The data collection was conducted over six months, from July to September 2019. The data were collected per the following steps:
- We met the department heads or representatives to explain the study objectives and the data required to ensure a smooth data collection process.
- All data were gathered over 60 months: 12 months pre-accreditation, 36 months during preparation for accreditation, and 12 months post-accreditation. Each hospital started accreditation on different dates (Table 2). Data were obtained through emails or manually using hardcopy proforma.
- The collected data were thoroughly checked to ensure that no details were missing.
- Any form of missing data was promptly returned to the concerned department, which was asked to provide the complete data.
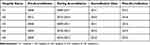 |
Table 2 Data Collected According to the Year of the Pre-, During, or Post-Accreditation Periods of All Five Hospitals Included in the Study |
Data Analysis
A piecewise regression analysis was performed using STATA version 25, (SatatCorp LLC, Texas, USA) which was downloaded from the official website, https://www.stata.com. The analysis involved partitioning an ordinary least-square linear regression analysis. The univariate normality of all variables was assessed using statistical and graphical methods. The skewness, kurtosis, Shapiro–Francia test, and Shapiro–Wilk test were applied to evaluate whether the distribution of the variables deviated statistically from the normal distribution.
Regarding skewness and kurtosis, p-values were obtained to test the hypothesis that the skewness and kurtosis levels were significantly different from those of normal distribution at the 5% significance level. Skewness and kurtosis p-values < 0.05 indicated that the skewness and kurtosis levels of the variables deviated significantly from the normal distribution. Similarly, regarding the results of the Shapiro–Francia and the Shapiro–Wilk tests, p-values < 0.05 indicated that the variable distribution deviated significantly from the normal distribution, and the assumption of univariate normality was violated.
We used two graphical methods: a histogram with an overlaid normal curve and a quartile-quartile (Q-Q) plot. The distribution was approximately normal if the overlaid normal curve on the histogram resembled a bell-shaped curve. The points on the Q-Q plot fell in a straight line close to the hypothetical regular distribution line.
We have already run regression analysis for all periods (pre-during-post), and compare the coefficients. In addition, the trend of incident reports, medication errors, and nosocomial infection during pre-, during-, and post-accreditation were analyzed using segmented regression analysis. The results are presented as the regression coefficient (slope) accompanied by the 95% confidence intervals (95% CI) and significance (p-value) for the three time periods (pre, during, and post-accreditation).
Similarly, the differences between the two period’s coefficients are evaluated using piecewise regression analysis. The regression coefficient’s changes are presented as changes in slope accompanied by the 95% CI and the significance of the changes (p-value).
Results
The largest hospital was “hospital 2”, with a capacity of 500 beds; it was also the last to be accredited among the five hospitals.
Changes in the Safety Dimension
Changes in the safety dimension were observed based on three indicators: the rates of incident reports, medication errors, and nosocomial infections, and the results are described below.
Incident Reports
The mean (SD) of the incident reports was 25.9 (4.6) during the pre-accreditation period. The mean was higher during the accreditation period, at 32.0 (8.2), and even higher in the post-accreditation period, at 38.0 (6.1), than the pre-accreditation period. Table 3 presents the descriptive statistics.
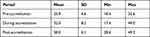 |
Table 3 Descriptive Statistics for the Mean of the Incident Reports at the Pre-, During, and Post-Accreditation Periods |
The trend and slope of the fitted line during the pre-accreditation period indicated an increasing trend of reported incidents by 0.2 per month. The slope decreased slightly, but not significantly, from the pre- to during the accreditation periods (Table 4 and Figure 1). Therefore, the slope indicating incidents reported during the accreditation period was slightly lower than those in the pre-accreditation period. The trend of reported incidents during the accreditation period increased by 0.15 per month. Changes of 0.01 in the slope were observed in the during and post-accreditation periods. However, the changes in slopes were not statistically significant. In the post-accreditation period, reported incidents increased by 0.17 per month.
 |
Table 4 Trends and Changes in the Mean Incident Reports Pre, During, and Post-Accreditation |
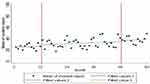 |
Figure 1 Changes in the mean of the incident reports pre, during, and post-accreditation. |
Medication Errors
The mean (SD) of medication errors was 201.9 (12.8) during the pre-accreditation period. The mean was lower during the accreditation period, at 189.6 (70.6), and even lower in the post-accreditation period, at 93.4 (11.8), than the pre-accreditation period. Table 5 presents the descriptive statistics.
 |
Table 5 Descriptive Statistics for the Mean of Medication Errors at the Pre-, During, and Post-Accreditation Periods |
The trend and slope of the fitted line for the mean of medication errors during the pre-accreditation period indicated a trend toward a reduction in medication errors by 0.19 per month before accreditation (Table 6 and Figure 2). The slope was reduced significantly by 5.77 units from the pre- to during accreditation periods. Therefore, the slope of medication errors during the accreditation period was markedly lower than that in the pre-accreditation period. The trend in medication errors during the accreditation period was reduced by 5.96 per month. A significant increase in the slope of 7.95 was observed in the during and post-accreditation periods. In the post-accreditation period, medication errors increased by 1.99 per month.
 |
Table 6 Trends and Changes in the Medication Errors Pre, During, and Post-Accreditation |
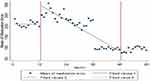 |
Figure 2 Changes in the mean of medication errors before, during, and after accreditation. |
Nosocomial Infection
The mean (SD) of nosocomial infections was 8.3 (1.7) during the pre-accreditation period. The mean was slightly lower during the accreditation period, at 8.0 (2.1), but higher in the post-accreditation period, at 8.7 (1.4), than the pre-accreditation period. Table 7 presents the descriptive statistics.
 |
Table 7 Descriptive Statistics for the Mean of Nosocomial Infections at the Pre-, During, and Post-Accreditation Periods |
The trend and slope of the fitted line for the mean of nosocomial infection in the pre-accreditation period indicated an increasing trend of 0.21 per month (Table 8 and Figure 3). The slope was reduced non-significantly by 0.24 units from pre- to during the accreditation periods. Therefore, the slope of nosocomial infections within the accreditation period was lower than that of the pre-accreditation period. The trend in nosocomial infection within the accreditation period was reduced by 0.03 per month. A further reduction of 0.09 in the slope was observed from the during accreditation period to the post-accreditation period. In the post-accreditation period, the trend in nosocomial infection decreased by 0.13 per month.
 |
Table 8 Trends and Changes in the Nosocomial Infection Pre, During, and Post-Accreditation |
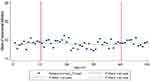 |
Figure 3 Changes in the mean of nosocomial infections before, during, and after accreditation. |
Discussion
The study’s results indicated promising improvements in the outcomes of IOM’s safety dimension in MOH hospitals in Madinah, probably attributable to the implementation of the CBAHI accreditation program and the collaboration between the accreditation teams in the hospitals. The results indicated an increase in the average number of reported incidents during the post-accreditation period.
Although this increase was not statistically significant, implementing the CBAHI accreditation standards is beneficial in ensuring increased compliance with safety control measures in MOH hospitals in Madinah. This finding is consistent with a previous study on the impact of accreditation on patient safety measures in Hail, Saudi Arabia, which found that hospital accreditation enhanced the incident reporting culture.17 This finding also aligns with another study exploring the awareness of the incident reporting system in Jordanian hospitals.27 The study showed a significant difference in the rate of reported incidents in accredited hospitals compared with non-accredited ones.
The CBAHI accreditation program helped improve the quality of care and patient safety by encouraging hospital staff to remain committed to the safety standards previously established by the authorities. The CBAHI requires hospitals to adhere to the highest levels of safety in their operations, preventing medical errors and minimizing recurrence rates. Per the CBAHI safety standards, hospitals must report incidents immediately. Furthermore, the incident reports must be documented transparently and referenced and reviewed when necessary because they may offer valuable lessons learned from mistakes.27
The term “incident” refers to an event that could have or has resulted in unnecessary harm to a patient (eg, medical errors, violations, patient abuse, and unsafe acts).28 Incident reports data are valuable in identifying potential risk areas to patients and taking action to achieve a sustainable reduction in risks and maintain patient safety.29 Incident reports provide responsible individual with information to avoid any potential risk. However, an increase in incident reporting should not be interpreted as deteriorating patient safety but rather as an increased awareness of safety issues among healthcare professionals.
Incident reports also identify and mitigate risks efficiently and improve employee performance through training programs. Additionally, they are an excellent opportunity to educate hospital staff about potential threats causing various medical errors, whether these errors are biological, physiological, or psychological.
Thus, the incident reporting system has become a safety improvement strategy widely used in healthcare.30 It helps identify high safety risks, develop mitigation interventions, and assess whether interventions reduce harm.31 Hence, incident reports are fundamental for maintaining hospital patient safety. Additionally, improving patient safety and reducing hospital patient injuries may reduce costs.
This study also showed that arithmetic averages indicated a decreased rate of medication errors from the pre- to the post-accreditation periods. Although the decline was not statistically significant, implementing CBAHI accreditation standards in Madinah’s MOH hospitals have increased compliance with systematic safety control. It may have led to the prevention and effective management of medication errors that caused patients’ morbidity and mortality.32
The CBAHI accreditation encourages research on medication errors to develop appropriate solutions to enhance patient safety in healthcare organizations and reduce medication errors. Al-Sughayir studied the impact of hospital accreditation on administering medication in psychiatric units in a teaching hospital in Saudi Arabia.33 He showed that adherence to accreditation standards contributed positively to medication administration. This improvement was related to effective clinical practice guidelines, a multidisciplinary management approach, the participation of clinical pharmacists’, and nursing support. Another study on patient safety indicators in a teaching hospital in Saudi Arabia revealed that medication management improved post-accreditation compared with pre-accreditation.34 Moreover, Devkaran and O’Farrell monitored 23 quality and patient safety indicators during the accreditation cycle in a multispecialty hospital in Abu Dhabi, UAE.10 They found the compliance of accreditation standards to increase during the accreditation period. Similarly, our study’s results indicated that implementing accreditation enhances staff compliance with safety standards.
Accreditation ensures that the administration is responsible for developing a safety culture and a robust error-reporting system in the workplace. It also instils a “no blame” culture in the workplace, which is essential to encourage hospital staff to report accidental medication errors and contribute to introducing preventive policies and practices that reduce these errors as much as possible. Adopting accreditation standards also reduces medication errors by fostering technical strategies, including distinguishing high-risk medications, separating some medicines, and assigning competent nurses to administer medications,35 thereby reducing medication errors and improving patient safety.
Finally, our results showed a decreasing trend in the nosocomial infection rate in Madinah’s MOH hospitals during the post-accreditation period. The CBAHI accreditation may have contributed to reducing nosocomial infections through preventive procedures that reduced the spread of infection. Accreditation fosters a safe environment for patients and hospital staff by ensuring compliance with infection prevention and control manuals.
Our results are similar to those of a study on the effects of accreditation on quality indicators at King Abdulaziz University in Saudi Arabia,34 which showed that implementing accreditation led to a significant reduction in the rate of nosocomial infections. Another study on the CBAHI’s impact on the quality measures in a tertiary hospital in Saudi Arabia supported our results that implementing accreditation positively influenced the patient safety indicator, including the rate of nosocomial infections.20 Contradicting our results, a study measuring the impact of accreditation on patient safety-related indicators at a teaching hospital in Iran did not reveal a positive impact of accreditation on the rate of nosocomial infections.7
Healthcare providers may unintentionally become disease vectors and spread new infections among unsuspecting patients.36 Hence, not complying with infection control guidelines, especially by nurses, transits nosocomial infections.37 However, the CBAHI accreditation standards encourage adopting simple preventive strategies such as regular handwashing, wearing personal protective equipment, sterilizing stethoscopes, using hand sanitizers, and displaying reminders and posters throughout the hospital.
Moreover, a 20% increase in hand hygiene reduces the nosocomial infection rate by 40%.38 Mandatory staff educational activities were conducted to increase awareness of the importance of reducing risk factors involving nosocomial infections. Infection control guidelines and manuals on preventing hospital infection and maintaining environmental hygiene have also been developed and are readily available for reference in all departments.
Accreditation standards clearly state that nosocomial infections should be prevented because they increase negative health outcomes, the length of hospital stays, and healthcare-related costs. Thus, the staff must adhere to the sterilization and disinfection guidelines recommended in the accreditation process. The hospital staff must be enthusiastic and prepared to meet and exceed healthcare standards, which significantly reduce infection and reflect positively on the hospital’s quality and safety of medical care.17
Strengths
The study used piecewise (segmented) regression analysis to precisely measure the CBAHI’s impact on the IOM dimensions. Accordingly, we bridged the research gap on the effect of accreditation on the quality of care through the IOM dimensions, specifically in the Saudi context. The selection of five major hospitals, a large study sample, and a high response rate helped strengthen the study’s findings through the representativeness of sample. Furthermore, the results will inform MOH policymakers and the CBAHI regarding the areas of improvement, improving the quality of care by implementing the CBAHI accreditation standards.
Limitations
The current study was limited to MOH hospitals. Therefore, the findings cannot be generalized to hospitals in other governmental organizations or the private sector.
Recommendations
We present the following recommendations for the MOH, the Saudi CBAHI, and future researchers.
The Saudi MOH
For the Saudi MOH to effectively implement the CBAHI standards, the hospitals’ financial and non-financial support should be linked to their compliance with it. It will encourage organizations to focus on efficiency and effectiveness. Establishing an annual national award for the best performing MOH hospitals is also recommended. It can encourage employees to compete by raising the bar. Moreover, a platform should be developed for automatically retrieving and publicly reporting the performance of MOH hospitals. This measure spreads transparency and organizations will respond favorably.
The CBAHI
To increase the impact of the CBAHI accreditation on IOM’s quality dimensions, especially safety, the agency must develop new indicators that directly measure quality instead of proxy indicators. Finally, we strongly suggest a special online reporting platform for publicly reporting hospitals’ clinical indicators and accreditation status.
Future Researchers
Our study has paved the way for hospital accreditation in Saudi Arabia, including opportunities for future research. This study examined the effects of CBAHI accreditation on three IOM quality dimensions. We suggest the following recommendations for future researchers:
- Investigating the effects of CBAHI accreditation on other IOM quality dimensions, such as efficiency, effectiveness, timeliness, equity, and patient-centeredness would determine its overall effect on the quality of care.
- Further studies should be conducted to expand the strategy of sustaining the improvements from the accreditation programs. This might help in effectively utilizing resources invested in the CBAHI or other accreditation programs.
- The current study should be replicated in other governmental and private hospitals to derive a broad view of the effects of accreditation on the quality of care. By comparing MOH hospitals with other hospitals, a future study may identify potential positively influencing factors impacting the CBAHI accreditation on the quality of care.
Conclusions
Based on our results, the CBAHI accreditation positively affected safety. Significant reductions were observed in the rates of incident reports, medication errors, nosocomial infections, and post-admission mortality. Our results provide insights for MOH hospitals and an opportunity to extend the CBAHI accreditation program to improve healthcare service quality.
Abbreviations
IOM, Institute of Medicine; CBAHI, Central Board for Accreditation on Healthcare Institutions; MOH, Ministry of Health; Q-Q plot, Quartile-quartile plot; H1, Hospital 1; H2, Hospital 2; H3, Hospital 3; H4, Hospital 4; H5, Hospital 5.
Ethical Approval and Informed Consent
Ethical approval for this study was granted by both the Human Research Ethics Committee of Universiti Sains Malaysia (reference number: USM\JEPeM\18080384, date: February 21, 2019) and the Ethical Review Committee (IRB) of the General Directorate of Health Affairs, Madinah, Saudi Arabia (reference number: H-03-M-084, date: March 18, 2019). Written consent was obtained from all participants.
Acknowledgments
We extend our gratitude to all the hospitals and their employees for their valuable participation, which made this study possible.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Corrêa JÉ, Turrioni JB, De Paiva AP, et al. The influence of accreditation on the sustainability of organizations with the Brazilian accreditation methodology. J Healthc Eng. 2018;2018:5–9. doi:10.1155/2018/1393585
2. Blumenthal D, De Melo PC. Quality of health care. Acta Med Port. 2000;13(5–6):303–307. doi:10.1787/52793ed8-en
3. IOM. To Err is Human: Building a Safer Health System. National Academies Press; 1999.
4. Brubakk K, Vist GE, Bukholm G, et al. A systematic review of hospital accreditation: the challenges of measuring complex intervention effects. BMC Health Serv Res. 2015;15(1). doi:10.1186/s12913-015-0933-x
5. IOM. Crossing the Quality Chasm. National Academies Press; 2001.
6. Almasabi M, Thomas S. The impact of Saudi hospital accreditation on quality of care: a mixed methods study. Int J Health Plann Manage. 2016;32(4):e261–e278. doi:10.1002/hpm.2373
7. Janati A, Sadegh J, Toofan F, Algalandis KN, Ebrahimoghli R. Hospital accreditation: what is its effect on quality and safety indicators? Experience of an Iranian Teaching Hospital. Bali Med J. 2016;5(2):303–307. doi:10.15562/bmj.v5i2.241
8. Mumford V, Reeve R, Greenfield D, Forde K, Westbrook J, Braithwaite J. Is accreditation linked to hospital infection rates? A 4-year, data linkage study of Staphylococcus aureus rates and accreditation scores in 77 Australian acute hospitals. Int J Qual Health Care. 2015:1–7. DOI:10.1093/intqhc/mzv078
9. Almasabi M, Thomas S. The impact of Saudi hospital accreditation on quality of care: a mixed methods study. Int J Health Plann Manage. 2017;32:261–278. doi:10.1002/hpm.2373
10. Devkaran S, O’Farrell PN. The impact of hospital accreditation on clinical documentation compliance: a life cycle explanation using interrupted time series analysis. BMJ Open. 2014;4:8. doi:10.1136/bmjopen-2014-005240
11. Abduljawad A. The impact of accreditation on the quality of hospitals int eh gulf cooperation council contries; 2013.
12. Devkaran S, Farrell PNO, Ellahham S, Arcangel R. Impact of repeated hospital accreditation surveys on quality and reliability, an 8-year interrupted time series analysis. BMJ Open. 2019;9:1–13. doi:10.1136/bmjopen-2018-024514
13. Chung KP, Yu TH. Are quality improvement methods a fashion for hospitals in Taiwan? Int J Qual Health Care. 2012;24(4):371–379. doi:10.1093/intqhc/mzs021
14. Jaararipooyan E, Agrizzi D, Akbari-haghighi F. Healthcare accreditation systems: further perspectives on performance measures. Int J Qual Health Care. 2011;23(6):645–656. doi:10.1093/intqhc/mzr063
15. Bogh SB, Falstie-Jensen AM, Bartels P, Hollnagel E, Johnsen SP. Accreditation and improvement in process quality of care: a nationwide study. Int J Qual Health Care. 2015;27(5):336–343. doi:10.1093/intqhc/mzv053
16. Despotou G, Her J, Arvanitis TN. Nurses’ perceptions of joint commission international accreditation on patient safety in tertiary care in South Korea. J Nurs Regul. 2020;10(4):30–36. doi:10.1016/S2155-8256(20)30011-9
17. Alshammari M, Alhabib S, Alshubrami D, Alrasidi M. Impact of Hospital‘Accreditation on Patient Safety in Hail City, Saudi Arabia: nurses‘Perspective. IOSR J Nurs Health Sci. 2015;4(1):51–55. doi:10.9790/1959-04115155
18. CBAHI. National hospital standards; 2016:12.
19. CBAHI. Saudi central board for accreditation of healthcare institutions. CBAHI; 2018. Available from: https://portal.cbahi.gov.sa/english/about-us/cbahi-at-a-glance.
20. Shaikh MZ, Al-Omari A, Ahmed A. The impact of CBAHI accreditation on critical care unit outcome quality measures: a case study. Int J Health Sci Res. 2018;8(7):7. doi:10.13140/RG.2.2.24226.12485
21. CBAHI. CBAHI Corporate Profile. The Suadi Central Board for Accreditation of Healthcare Institutions; 2017.
22. Fortune T, O’Connor E, Donaldson B. Guidance on designing healthcare external evaluation programmes including accreditation. Int Soc Qual Health Care. 2015;2015:1–84.
23. ISQua. Current awards – iSQua; 2022. Available from: https://ieea.ch/accreditation.html.
24. Seada AM. impact of hospital accreditation on quality of care as perceived by nursing staff in King Khaled Hospital in Najran at Kingdom of Saudi Arabia. J Am Sci. 2012;8(7):308–315. doi:10.1017/CBO9781107415324.004
25. Greenfield D, Pawsey M, Braithwaite J. The role and impact of accreditation on the healthcare revolution. Revista acreditação. 2011;1(2):134–150.
26. El-Jardali F, Jamal D, Dimasi H, Ammar W, Tchaghchaghian V. The impact of hospital accreditation on quality of care: perception of Lebanese nurses. Int J Qual Health Care. 2008;20(5):363–371. doi:10.1093/intqhc/mzn023
27. Abualrub RF, Al-Akour NA, Alatari NH. Perceptions of reporting practices and barriers to reporting incidents among registered nurses and physicians in accredited and nonaccredited Jordanian hospitals. J Clin Nurs. 2015;24(19–20):2973–2982. doi:10.1111/jocn.12934
28. Runciman W, Hibbert P, Thomson R, Van Der Schaaf T, Sherman H, Lewalle P. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care. 2009;21(1):18–26. doi:10.1093/intqhc/mzn057
29. World Health Organization. Patient Safety Incident Reporting and Learning Systems. World Health Organization; 2020.
30. Macrae C. The problem with incident reporting. BMJ Qual Saf. 2016;25(2):71–75. doi:10.1136/bmjqs-2015-004732
31. Pham JC, Girard T, Pronovost PJ. What to do with healthcare Incident Reporting Systems. J Public Health Res. 2013;2(3):27. doi:10.4081/jphr.2013.e27
32. Nguyen MNR, Mosel C, Grzeskowiak LE. Interventions to reduce medication errors in neonatal care: a systematic review. Ther Adv Drug Saf. 2018;9(2):123–155. doi:10.1177/2042098617748868
33. Alsughayir MA. Does accreditation improves pro re nata benzodiazepines administration.pdf. Int J Mental Health Sys. 2017;11(16):1–5.
34. Al Awa B, Jacquery A, Almazrooa A, et al. Comparison of patient safety and quality of care indicators between pre and post accreditation periods in King Abdulaziz University hospital.pdf. Res J Med Sci. 2011;5(1):61–66. doi:10.3923/rjmsci.2011.61.66
35. Salar A, Kiani F, Rezaee N. Preventing the medication errors in hospitals: a qualitative study. Int J Afr Nurs Sci. 2020;13:100235. doi:10.1016/j.ijans.2020.100235
36. Khan HA, Ahmad A, Mehboob R. Nosocomial infections and their control strategies. Asian Pac J Trop Biomed. 2015;5(7):509–514. doi:10.1016/j.apjtb.2015.05.001
37. Noaman AY, Al-Abdullah N, Jamjoom A, Ragab AHM, Nadeem F, Ali AG. knowledge based e-health surveillance system for predicting hospital acquired infections. Proce Int Compu Software Appl Conf. 2018;2:345–351. doi:10.1109/COMPSAC.2018.10255
38. AlKuwaiti A, Subbarayalu AV. Reducing hospital-acquired infection rate using the Six Sigma DMAIC approach. Saudi J Med Med Sci. 2017;5(3):260. doi:10.4103/sjmms.sjmms_98_16
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
