Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Impact of Serum Cystatin C Level on Long-Term Cognitive Impairment After Acute Ischemic Stroke and Transient Ischemic Attack
Authors Zuo L, Dong Y, Pan Y, Yan H , Meng X, Li H, Zhao X , Wang Y, Wang Y, Liao X
Received 16 March 2023
Accepted for publication 8 June 2023
Published 5 July 2023 Volume 2023:19 Pages 1543—1554
DOI https://doi.org/10.2147/NDT.S412825
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Taro Kishi
Lijun Zuo,1 Yanhong Dong,2 Yuesong Pan,3 Hongyi Yan,3 Xia Meng,3 Hao Li,3 Xingquan Zhao,1 Yilong Wang,1 Yongjun Wang,1 Xiaoling Liao1
1Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Alice Lee Centre for Nursing Studies, Yong Loo Lin School of Medicine, National University of Singapore, Clinical Research Centre, Singapore, 117597, Singapore; 3National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Xiaoling Liao, Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, No. 119, South Fourth Ring West Road, Fengtai District, Beijing, 100070, People’s Republic of China, Tel +86-010-59978350, Fax +86-010-59973383, Email [email protected]
Objective: Cognitive impairment after stroke/transient ischemic attack (TIA) has a high prevalence. Cystatin C (CysC) has been found as a novel biomarker of neurodegenerative diseases, such as dementia and Alzheimer’s disease. We aimed to explore the possible correlations of serum CysC level with cognitive impairment in patients who had mild ischemic stroke and TIA after 1 year.
Methods: We measured serum CysC level in 1025 participants with a minor ischemic stroke/TIA from enrolled from the Impairment of Cognition and Sleep (ICONS) study of the China National Stroke Registry-3 (CNSR-3). They were divided into four groups according to quartiles of baseline CysC levels. Patients’ cognitive functions were assessed by Montreal Cognitive Assessment (MoCA)-Beijing at day 14 and at 1 year. Multiple logistic regression models were performed to evaluate the relationship between CysC and post-stroke cognitive impairment (PSCI) at 1-year follow-up.
Results: Cognitive impairment was defined as MoCA-Beijing ≤ 22. Most patients were in 60s (61.52± 10.97 years old) with a median (interquartile range) National Institute of Health Stroke Scale(NIHSS) score of 3.00 (4.00) and greater than primary school level of education, and 743 participants (72.49%) were male. Among the 1025 participants, 331 participants (32.29%) patients suffered PSCI at 1-year follow-up. A U-shaped association was observed between CysC and 1-year PSCI [quartile (Q)1 vs Q3: adjusted odds ratio (aOR) 2.69, 95% CI 1.67– 4.34, p < 0.0001; Q2 vs Q3: aOR 1.63, 95% CI 1.03– 2.57, p = 0.0354; Q4 vs Q3: aOR 1.83, 95% CI 1.16– 2.87, p = 0.009]. Moreover, the U-shaped trends were also found between CysC level and the subscores of attention, recall, abstraction and language in MoCA.
Conclusion: CysC showed a U-shaped correlation with 1-year overall cognitive function. It is probable that measurement of the serum CysC level would aid in the early diagnosis of PSCI.
Keywords: mild stroke, post stroke cognitive impairment, cystatin C
Introduction
Long-term cognitive impairment is a common complication of acute ischemic stroke (AIS)/transient ischemic attack (TIA). Although neurological deficits may return to a certain extent (transient cognitive impairment [TCI]), cognitive recovery does not necessarily consistent with physical recovery. About 40% of patients had a TCI within 7 days after TIA compared to only 19% of those seen after 7 days.1 There are both transient and long-term cognitive impairment after TIA.2 This TCI (rather than the absolute cognitive level) predicted subsequent cognitive decline. Approximately 58.82% of patients experienced cognitive impairment after stroke in acute phase.3 It may affect the quality of life, and predict dependency4 and death.5
Cystatin C (CysC) is an endogenous protein inhibitor of cysteine protease. It plays a wide range of biological roles, ranging from regulating normal tissue processes such as cell proliferation and growth to modulating potentially pathogenic events, including infection,6 and neurodegenerative diseases such as dementia, Alzheimer’s disease (AD).7 CysC was reported as a predictive marker of cardiovascular diseases8 and AIS.9 CysC has been thought to be related to the clinical manifestations of cognitive impairment.10–12 There have been several studies demonstrating that CysC inhibited the aggregation of cerebral amyloid protein (Aβ) and potentially prevented cognitive impairment in AD.13 It indicated that low level of CysC combined with increased cysteines protease and amyloid protein aggregation,14 which has direct cytotoxic effects on brain tissue and leads to cognitive impairment.15 On the other hand, cohort studies evaluated the association between CysC and cognitive functions in older adults, indicating that higher CysC level was associated with worse cognitive function.16 One meta analysis showed that CysC level was associated with the risk of mild cognitive impairment (MCI) in the Asian population but not in the Caucasian population, and it could be considered as a predictor for the risk of cognitive impairment.17 Moreover, the increased CysC level predicted the high risk of PSCI at 3-month of follow-up.10,17 However, those studies only focused on short-term cognitive function and did not analyze the long-term cognition.
In this analysis of the Impairment of Cognition and Sleep quality (ICONS), we aimed to assess the association between CysC level and cognitive outcomes at 1 year among patients with AIS/TIA.
Methods
Participants
Patients in this study are from the ICONS subgroup of CNSR-III database. CNSR-III is a multicenter (201 hospitals) prospective registry. It consecutively recruited AIS or TIA in-hospital patients within 7 days after onset between August 15, 2015, and January 2018, with 1-year follow-up finished in March 2019.18 There are 2625 patients enrolled in ICONS, and finally, 1025 patients perform the MoCA-Beijing and CysC test at baseline (within two weeks of index cerebrovascular event) and at 1 year after AIS/TIA by trained research psychologists.
The inclusion criteria for patients in this study were: (i) aged over 18 years older; (ii) diagnosed with AIS or TIA in hospital within 7 days; Patients’ ischemic stroke/TIA are diagnosed according to World Health Organization criteria (acute onset of neurological deficit, persisting for >24 hours in case of stroke, or for <24 hours in case of TIA), and confirmed with brain CT or MRI; (iii) no history of severe cognitive impairment, schizophrenia or mental disease; (VI) the absence of any factors affecting cognitive tests, for instance, visual or hearing disorders, severe unilateral neglect, severe aphasia defined as National Institutes of Health Stroke Scale (NIHSS) item 9 > 2, or consciousness disorders.
Data collection for ICONS was approved by the ethics committee of all participating hospitals. Prior to data collection, all participants or their legal representatives signed written informed consents.
Procedure
Data Collection
Demographics (age, gender, smoking, drinking, body mass index and educational level), and evaluation of medical histories (stroke, hypertension, hypercholesterolemia, diabetes, coronary artery disease, atrial fibrillation, heart failure and epilepsy) were collected.
The 7-item Generalized Anxiety Disorder Scale (GAD) and Patient Health Questionnaire-9 (PHQ-9) were used to assess participants’ anxiety and depression status. In addition, a detailed physical examination was completed, and several parameters, including the modified Rankin Scale (mRS), Trial of ORG 10172 in Acute Stroke Treatment (TOAST) type, NIHSS score, and Glasgow Coma Scale. The blood samples were gathered within 24h of admission and transported through the cold chain to the central laboratory in Beijing Tiantan Hospital. All serum samples were kept frozen at −80◦C until ready for assay. The level of CysC was detected by the immunoturbidimetric method (Roche Cobas c501 analyzer with cystatin C assay); coefficient of variation (CV) was 2%.
Outcome Evaluation
The MoCA-Beijing was used to assess global cognition and detect PSCI. The MoCA-Beijing was developed with the following modifications as previous study showed.19 The primary outcome was PSCI at 1 year after AIS or TIA. Patients who have MoCA-Beijing ≤22 were regarded as cognitive impairment. This norms were on the basis of our previous results recruited 102 AIS or TIA patients at 2 weeks and evaluated by a formal neuropsychological test.3 The data showed that the optimal cutoff point for MoCA-Beijing in discriminating patients with or without cognitive impairment (NCI) was 22/23. The sensitivity was 85%, and the specificity was 88%.
Statistical Analysis
Normally distributed continuous variables were described as mean± SD and analyzed by two-tailed t-tests. Skewed data were described as median (interquartile range) and analyzed using nonparametric tests. Categorical variables were analyzed by chi-square test. Patients in this study were categorized into 4 groups by CysC quartiles. Multivariable logistic regression analysis was used to evaluate the association among CysC level and PSCI. The quartile 3 of the CysC was used as a reference value in the multivariate analysis. The 2 models were performed. Model 1 was adjusted for age, gender and educational level; Model 2 was additionally adjusted for smoking, hypertension, diabetes, coronary heart disease, history of stroke, atrial fibrillation, estimated glomerular filtration rate (eGFR), TOAST type, the scores of baseline NIHSS, MoCA and pre-mRS. P < 0.05 was considered statistically significant. All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC).
Results
Baseline Characteristics
There were 2625 patients enrolled in the ICONS study. We excluded 1600 patients missing CysC data on admission and MoCA results at the 1-year follow-up. Finally, 1025 patients were involved in the current analysis (Figure 1). Most of those patients were at their 60 years (61.52±10.97 years old), and 743 participants (72.49%) were male. The ranges of CysC for quartiles (Q1–Q4) were defined as follows: Q1 ≤ 0.84mg/l, 0.84mg/l < Q2 ≤ 0.95mg/l, 0.95mg/l < Q3 ≤ 1.09mg/l and Q4 ≥ 1.09 mg/l. The differences in demographics and clinical characteristics of patients among different CysC level groups are shown in Table 1. Significant differences in age, gender, smoking, previous history of stroke, diabetes, coronary heart disease, atrial fibrillation, TOAST classification, eGFR level, the scores of baseline NIHSS, MoCA and pre-mRS were observed among the groups with different CysC levels (Table 1). In cognitive domains, data showed dramatically difference in attention, recall, abstraction and language (Table 1).
 |
Table 1 Demographic, Clinical Characteristics and Outcomes of Patients with Different Cystatin C Ranges at 1 Year |
 |
Figure 1 Flowchart of patients participating in the study. |
Logistic Regression Analysis
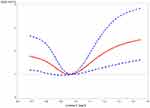
A total of 331 participants (32.29%) suffered from PSCI in 1-year follow-up (Table 2). The 1-year incidence of PSCI among the groups with different CysC levels (from low to high) was 25.98, 23.56, 17.22, and 33.23%, respectively (Table 2). After adjustment for conventional covariables (Model 1) and further adjustment for smoking, hypertension, diabetes, coronary heart disease, history of stroke, atrial fibrillation, eGFR, TOAST type, NIHSS score, pre-mRS score and MoCA score at baseline in model 2, patients in the first and last CysC quartiles (Q1 and Q4) had worse cognitive function (MoCA ≤ 22) compared with the third quartile [quartile (Q)1 vs Q3: adjusted odds ratio (aOR) 2.69, 95% CI 1.67–4.34, p < 0.0001; Q2 vs Q3: aOR 1.63, 95% CI 1.03–2.57, p = 0.0354; Q4 vs Q3: aOR 1.83, 95% CI 1.16–2.87, p = 0.009]. A U-shaped association was observed between CysC and 1-year incidence of cognitive impairment in all the included patients (Figure 2).
 |
Table 2 Logistic Regression Analysis of Cognitive Outcomes at 12 m in AIS Participants |
Subgroup Analysis
CysC level for 1-year incidence of cognitive impairment and ORs for cognitive impairment at 1-year by age, gender, etiology of stroke and educational level are shown in Table 3 and Figure 3. There was no heterogeneity in the effects of CysC level on the primary outcome between subgroups classified by age, gender, TOAST subtypes, and educational level. In cognitive domain analysis, data show there were U-shape trends among CysC level and scores of attention, recall, abstraction and language (Figure 4).
 |
Table 3 Subgroup Analysis of Association Between CysC and Cognitive Function**: <0.01,*: <0.05. |
 |
Figure 3 Subgroup analysis of association between CysC groups and 1-year PSCI in patients with AIS/ TIA. |
 |
Figure 4 The analysis of association between CysC level and different cognitive domains after 1-year in patients with AIS/ TIA. |
Discussion
In this prospective study, we explored the relationship between serum CysC level and long-term PSCI in patients with AIS/TIA. Data showed several great discoveries in this study. First, it demonstrated a U-shaped correlation between serum CysC level and long-term PSCI. Second, in cognitive sub-domains, the data showed that both low and high CysC levels were associated with attention, recall, abstraction and language.
The U-shaped correlation between CysC level and long-term cognitive impairment means low level of CysC has a deleterious association on cognition after AIS/TIA. At present, the relationship between serum CysC level and PSCI is not clear. A clinical study found that increased serum CysC level in patients with norm renal function was related to a lower risk of cognitive impairment at 3 months.20 CysC is a crucial endogenous protective factor against stroke and can be an independent predictor of ischemic stroke.21 Several studies have shown an association between CysC level and cognitive dysfunction.22,23 Previous studies showed that CysC binded Aβ and inhibited formation of Aβ fibrils and oligomers, suggesting that a decreased CysC level was linked to AD.22,23 CysC could also change amyloid protein precursor processing and protect against Aβ production in AD.24 More recently, multiple studies have shown an association between the CysC gene (CST3) and late-onset AD.25 AD patients showed significantly reduced CysC level in CSF than non-dementia controls.26 A clinical study found that increased serum CysC level in stroke patients was related to a lower risk of cognitive impairment at 3 months, suggesting that CysC was a protective factor for PSCI.20
On the other hand, some studies indicated that serum CysC was a risk factor for cognitive impairment.27–29 Furthermore, the serum CysC level was shown to be associated with long-term dementia risk in older patients.29 Serum CysC level was increased at acute phase after minor ischemic stroke, and higher serum CysC level at baseline might be an independent risk factor for PSCI.30 Another study suggested that high serum CysC level increased the risk of vascular dementia.10 High CysC level is an independent risk factor of cognitive impairment after lacunar infarction.28 Additional underlying mechanisms are suggested. CysC as a cysteine protease inhibitor is reported to be involved in the pathophysiological processes of atherosclerosis and plaque instability.31 Our previous study found that the CysC showed a U-shaped correlation with poor outcome after stroke, especially in small artery occlusion group.9 Similarly, other studies reported that high CysC level was found to be associated with unfavourable outcomes in AIS patients treated with intravenous alteplase32 and futile recanalization treatment.33 All these studies suggested high CysC level involved in the vascular pathophysiology. Increasing pieces of evidence revealed that serum CysC level was associated with periventricular hyperintensities.34 The serum CysC level in patients with acute stroke complicated with intracranial microhemorrhage was significantly higher than patients without microhemorrhage and proved that CysC was an independent risk factor for intracranial microhemorrhage.34,35 The pathologic changes under periventricular hyperintensities and microhemorrhage were finally leading to cognitive dysfunction.35 However, a few studies showed no significantly difference in CysC level between Caucasian patients with MCI and controls.36–38 Another study demonstrated significantly increased plasma CysC level in all cohorts of African American, Hispanic, and White amnestic MCI patients compared with controls. When corrected for ethnicity and disease status, plasma level of CysC was only significantly higher in Hispanic amnestic MCI female patients compared with the Hispanic age-matched control group.38 One meta analysis showed that CysC was associated with the risk of MCI in the Asian population but not in the Caucasian population.17 The relationship between CysC level and cognitive impairment might be related to ethnicity. This study is the first to find a nonlinear relationship between CysC level and 1-year PSCI after AIS/TIA, adding evidence of bilateral effects of CysC level on cognitive impairment. Previous study showed that elevated CysC level was closely related to the occurrence of PSCI in stroke patients at 3 months follow-ups.30 The differences may be explained by the different sample sizes, cognitive evaluation time and adjustment of confounders, and these studies explored the possibility of a linear relationship rather than a nonlinear relationship.
CysC level might be an independent risk factor for overall cognitive impairment.34 However, the impact of CysC on different cognitive domains remains unclear. In this study, we also found the U-shaped trend between CysC level and scores of attention, recall, abstraction and language. As previous study reported that the relationship between CysC level and periventricular hyperintensities and microhemorrhage, which was closely associated with frontal lobe dysfunction, particularly with attention, executive dysfunction.34 The microhemorrhage was closely related to cognitive dysfunction, such as executive function, memory and abstract thinking.35 It indicated that attention, recall, abstraction and language were the 4 major cognitive domains CysC had influence on, and finally leading to cognitive deficits. However, these aspects might need further study in the future.
There was no heterogeneity in the effects of CysC level on 1-year PSCI after AIS/TIA between subgroups classified by age, gender, TOAST subtypes, and educational level. Statistical interaction between CysC and age, gender, TOAST subtypes, and educational level did not show a significant difference. The underlying mechanism still needs further study.
Our study had some limitations. Firstly, only baseline CysC level was measured in this study. However, the CysC level is likely to fluctuate, so we were unable to examine the association of CysC changes with 1-year PSCI. We may add repeated measurement intervals and do some in-depth research about CysC fluctuations and cognitive impairment in the future. Secondly, we consecutively recruit patients with AIS or TIA from multiple subcentral hospitals, fewer patients with TIA were included in the study than patients with AIS, the patients are unevenly distributed. Thirdly, most of the patients recruited in this study had mild ischemic stroke or TIA, which might not represent all patients with AIS/TIA. Therefore, our findings may not be applicable to all stroke patients. Fourthly, we found a U-shape relationship between CysC level and overall cognition, as well as U-shape trends between CysC level and subdomains in MoCA, further work is needed to include detailed neuropsychological scales consisting of different cognitive domains to validate our research and to explore underlying mechanisms. Lastly, as study reported that more than half of the patients with a first-ever lacunar stroke and without cognitive impairment had minor neuropsychological alterations.39 It is the lacunar but not leukoaraiosis exerting an independent effect on cognitive function.40 The pathophysiology, prognosis and clinical features of lacunar strokes are different from all other acute cerebrovascular diseases.41 However, we did not evaluate the neuroimaging features in this study, such as lacunar, which might have an impact on PSCI. Further research should perform neuroimaging tests, and expanding the results on the relationship of serum CysC level and long-term cognitive impairment in ischemic lacunar versus non-lacunar stroke.
Conclusions
The results of this study indicated that both lower and higher CysC level were associated with 1-year PSCI. CysC level at baseline might be a biomarker for PSCI in patients with acute minor ischemic stroke. Further prospective studies are needed to verify our results and to elucidate the potential mechanisms.
Data Sharing Statement
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study involves human participants and was approved by the Ethics Committee of Beijing Tiantan Hospital and all participating hospitals (No. KY2015-001-01) in accordance with the Declaration of Helsinki. Prior to data collection, all participants or their legal representatives signed written informed consents.
Patient Consent for Publication
Parental/guardian consent obtained.
Acknowledgments
The authors would like to thank all participants for their involvement. This work was performed at Beijing Tiantan Hospital, Capital Medical University, Beijing, China. We also thank Professor Xingao Wang from Beijing Tiantan Hospital, Capital Medical University for his modification and review of the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work is supported by the National Key Research and Development Program of China (2017YFC1308404, 2020YFC2004800),Capital Medical University Cultivation Fund(PYZ22120) and Beijing Excellent Talents Training Program(2018000021469G237).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Pendlebury ST, Wadling S, Silver LE, Mehta Z, Rothwell PM. Transient cognitive impairment in tia and minor stroke. Stroke. 2011;42(11):3116–3121. doi:10.1161/STROKEAHA.111.621490
2. Ganesh A, Barber PA. The cognitive sequelae of transient ischemic attacks-recent insights and future directions. J Clin Med. 2022;11:53.
3. Zuo L, Dong Y, Zhu R, et al. Screening for cognitive impairment with the Montreal cognitive assessment in Chinese patients with acute mild stroke and transient ischaemic attack: a validation study. BMJ Open. 2016;6:e011310.
4. Nys GM, van Zandvoort MJ, de Kort PL, et al. The prognostic value of domain-specific cognitive abilities in acute first-ever stroke. Neurology. 2005;64:821–827.
5. Mijajlović MD, Pavlović A, Brainin M, et al. Post-stroke dementia - a comprehensive review. BMC Med. 2017;15:11.
6. van Kasteren SI, Berlin I, Colbert JD, Keane D, Ovaa H, Watts C. A multifunctional protease inhibitor to regulate endolysosomal function. ACS Chem Biol. 2011;6:1198–1204.
7. Wang R, Chen Z, Fu Y, et al. Plasma cystatin c and high-density lipoprotein are important biomarkers of Alzheimer’s disease and vascular dementia: a cross-sectional study. Front Aging Neurosci. 2017;9:26.
8. Keller T, Messow CM, Lubos E, et al. Cystatin c and cardiovascular mortality in patients with coronary artery disease and normal or mildly reduced kidney function: results from the atherogene study. Eur Heart J. 2009;30:314–320.
9. Ding Y, Liu L, Chen Z, et al. Serum cystatin c predicts stroke clinical outcomes at 1 year independent of renal function. Front Neurol. 2021;12:676872.
10. Zeng Q, Huang Z, Wei L, Fang J, Lin K. Correlations of serum cystatin c level and gene polymorphism with vascular cognitive impairment after acute cerebral infarction. Neurol Sci. 2019;40:1049–1054.
11. Hu WD, Chen J, Mao CJ, et al. Elevated cystatin c levels are associated with cognitive impairment and progression of Parkinson disease. Cogn Behav Neurol. 2016;29:144–149.
12. Sacre JW, Magliano DJ, Zimmet PZ, et al. Associations of chronic kidney disease markers with cognitive function: a 12-year follow-up study. J Alzheimers Dis. 2019;70:S19–s30.
13. Butler JM, Sharif U, Ali M, et al. A missense variant in cst3 exerts a recessive effect on susceptibility to age-related macular degeneration resembling its association with Alzheimer’s disease. Hum Genet. 2015;134:705–715.
14. Wu H, Du Q, Dai Q, Ge J, Cheng X. Cysteine protease cathepsins in atherosclerotic cardiovascular diseases. J Atheroscler Thromb. 2018;25:111–123.
15. Sundelöf J, Sundström J, Hansson O, et al. Cystatin c levels are positively correlated with both abeta42 and tau levels in cerebrospinal fluid in persons with Alzheimer’s disease, mild cognitive impairment, and healthy controls. J Alzheimers Dis. 2010;21:471–478.
16. Chen WW, Cheng X, Zhang X, et al. The expression features of serum cystatin c and homocysteine of Parkinson’s disease with mild cognitive dysfunction. Eur Rev Med Pharmacol Sci. 2015;19:2957–2963.
17. Nair P, Misra S, Nath M, et al. Cystatin c and risk of mild cognitive impairment: a systematic review and meta-analysis. Dement Geriatr Cogn Disord. 2020;49:471–482.
18. Wang Y, Jing J, Meng X, et al. The third China national stroke registry (cnsr-iii) for patients with acute ischaemic stroke or transient ischaemic attack: design, rationale and baseline patient characteristics. Stroke Vasc Neurol. 2019;4:158–164.
19. Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal cognitive assessment, moca: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53:695–699.
20. Guo DX, Zhu ZB, Zhong CK, et al. Serum cystatin c levels are negatively correlated with post-stroke cognitive dysfunction. Neural Regen Res. 2020;15:922–928.
21. Kim TJ, Kang MK, Jeong HG, et al. Cystatin c is a useful predictor of early neurological deterioration following ischaemic stroke in elderly patients with normal renal function. Eur Stroke J. 2017;2:23–30.
22. Tizon B, Ribe EM, Mi W, Troy CM, Levy E. Cystatin c protects neuronal cells from amyloid-beta-induced toxicity. J Alzheimers Dis. 2010;19:885–894.
23. Gauthier S, Kaur G, Mi W, Tizon B, Levy E. Protective mechanisms by cystatin c in neurodegenerative diseases. Front Biosci. 2011;3:541–554.
24. Wang XF, Liu DX, Liang Y, et al. Cystatin c shifts app processing from amyloid-β production towards non-amyloidgenic pathway in brain endothelial cells. PLoS One. 2016;11:e0161093.
25. Levy E, Jaskolski M, Grubb A. The role of cystatin c in cerebral amyloid angiopathy and stroke: cell biology and animal models. Brain Pathol. 2006;16:60–70.
26. Hansson SF, Andréasson U, Wall M, et al. Reduced levels of amyloid-beta-binding proteins in cerebrospinal fluid from Alzheimer’s disease patients. J Alzheimers Dis. 2009;16:389–397.
27. Kono S, Adachi H, Enomoto M, et al. Impact of cystatin c and microalbuminuria on cognitive impairment in the population of community-dwelling Japanese. Atherosclerosis. 2017;265:71–77.
28. Wanggong F, Xiang J, Yang S, Zhang W, Tuerganbieke R. Correlation of serum uric acid, cystatin c and high-sensitivity c-reactive protein with cognitive impairment in lacunar cerebral infarction. Am J Transl Res. 2021;13:6717–6723.
29. Slinin Y, Peters KW, Ishani A, et al. Cystatin c and cognitive impairment 10 years later in older women. J Gerontol a Biol Sci Med Sci. 2015;70:771–778.
30. Yan X, Chen H, Shang XL. Association between serum cystatin c level and post-stroke cognitive impairment in patients with acute mild ischemic stroke. Brain Behav. 2022;12:e2519.
31. Helmersson-Karlqvist J, Ärnlöv J, Carlsson AC, Härmä J, Larsson A. Increased urinary cystatin c indicated higher risk of cardiovascular death in a community cohort. Atherosclerosis. 2014;234:108–113.
32. Chang Z, Zou H, Xie Z, et al. Cystatin c is a potential predictor of unfavorable outcomes for cerebral ischemia with intravenous tissue plasminogen activator treatment: a multicenter prospective nested case-control study. Eur J Neurol. 2021;28:1265–1274.
33. Su M, Zhou Y, Chen Z, et al. Cystatin c predicts futile recanalization in patients with acute ischemic stroke after endovascular treatment. J Neurol. 2022;269:966–972.
34. Zhang S, Luo Y, Dong Z, et al. Impact of periventricular hyperintensities and cystatin c on different cognitive domains in the population of non-demented elderly Chinese. J Clin Neurosci. 2019;68:201–210.
35. Yang J, Lyu Y, Ma Y, Chen Y. Relationship between cerebral microbleeds location and cognitive impairment in patients with ischemic cerebrovascular disease. Neuroreport. 2018;29:1209–1213.
36. Casado Naranjo I, Portilla Cuenca JC, Duque de san juan B, et al. Association of vascular factors and amnestic mild cognitive impairment: a comprehensive approach. J Alzheimers Dis. 2015;44:695–704.
37. Rajagopalan P, Refsum H, Hua X, et al. Mapping creatinine- and cystatin c-related white matter brain deficits in the elderly. Neurobiol Aging. 2013;34:1221–1230.
38. Grewal R, Haghighi M, Huang S, et al. Identifying biomarkers of dementia prevalent among amnestic mild cognitively impaired ethnic female patients. Alzheimers Res Ther. 2016;8:43.
39. Blanco-Rojas L, Arboix A, Canovas D, Grau-Olivares M, Oliva Morera JC, Parra O. Cognitive profile in patients with a first-ever lacunar infarct with and without silent lacunes: a comparative study. BMC Neurol. 2013;13:203.
40. Arboix A. Lacunar infarct and cognitive decline. Expert Rev Neurother. 2011;11:1251–1254.
41. Rudilosso S, Rodríguez-Vázquez A, Urra X, Arboix A. The potential impact of neuroimaging and translational research on the clinical management of lacunar stroke. Int J Mol Sci. 2022;23.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.