Back to Journals » International Journal of General Medicine » Volume 16
Impact of Promising Biomarkers on Severity and Outcome of Acute Pulmonary Embolism
Authors Sagcan G, Dogan Z, Uzun H , Cuhadaroglu C, Okumus G, Arseven O
Received 25 April 2023
Accepted for publication 28 July 2023
Published 2 August 2023 Volume 2023:16 Pages 3301—3309
DOI https://doi.org/10.2147/IJGM.S416541
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Gulseren Sagcan,1 Zeki Dogan,2 Hafize Uzun,3 Caglar Cuhadaroglu,1 Gulfer Okumus,4 Orhan Arseven4
1Department of Chest Diseases, Faculty of Medicine, Acıbadem University, İstanbul, Turkey; 2Department of Cardiology, Faculty of Medicine, Istanbul Atlas University, Istanbul, Turkey; 3Department of Medical Biochemistry, Faculty of Medicine, Istanbul Atlas University, Istanbul, Turkey; 4Department of Chest Diseases, Faculty of Medicine, Istanbul University, İstanbul, Turkey
Correspondence: Gulseren Sagcan, Department of Chest Diseases, Faculty of Medicine, Acıbadem University, İstanbul, Turkey, Tel +902166495751 ; +905323637953, Fax +902166495373, Email [email protected]
Background: Acute pulmonary embolism (APE) is a common clinical condition. Its severity ranges from asymptomatic radiological findings to fatal obstructive shock. The potential circulating biomarkers have been studied to predict APE outcomes. This study aimed to explore their predictive power on prognosis in APE.
Material and Method: It was a prospective observational study between March 2008 and April 2010. All consecutive patients diagnosed with APE were categorized as massive/high-risk, submassive/moderate-risk, and non-massive/low-risk. Cardiac troponin T (cTnT), myoglobin, N-terminal pro-brain natriuretic peptide (NT-proBNP), heart-type fatty acid-binding protein (H-FABP), growth differentiation factor-15 (GDF-15), and D-dimer levels were measured.
Results: Of these patients, 14 (29.8%), 16 (34.0%), and 17 (36.2%) patients were categorized as low-risk, moderate-risk, and high risk-patients, respectively. There was no significant difference between the patient groups categorized based on the risk stratification in terms of demographic and clinical characteristics. The cTnT, myoglobin, HFABP, and D-dimer levels have also not differed significantly between the groups. There was a significant difference between the groups in respect of NT-proBNP and GDF-15 levels (p=0.009 and p=0.037, respectively). Nine (19.1%) patients had died by the 3rd-month follow-up. Adverse events were seen in 26 (55.3%) patients. GDF-15 had the highest area under the curve (AUC) value for predicting any adverse event (cut-off value=9.3 ng/mL, AUC=0.796, CI (confidence interval) 95%: 0.653– 0.899). NT-ProBNP was determined as the best predictor for mortality (cut-off value=229.2 pg/mL, AUC=0.889, CI 95%: 0.756– 0.964).
Conclusion: Higher levels of NT-proBNP and GDF-15 were found to be associated with more severe APE, worse outcomes, and mortality.
Keywords: pulmonary embolism, biomarkers, adverse clinical outcome, natriuretic peptides, growth differentiation factor-15
Introduction
Acute pulmonary embolism (APE) is a common clinical condition. Its severity ranges from asymptomatic radiological findings to fatal obstructive shock.1 It has significant morbidity and mortality depending on its severity.2 The disease is clinically categorized into three main classes considering the patients’ hemodynamic status and the presence of right ventricular enlargement or strain: massive/high-risk, submassive-intermediate-risk, and low-risk APE.2 It is generally accepted that the risk stratification of APE is an essential step to treat the disease reasonably.3
Several cardiac biomarkers have been studied in predicting the morbidity and mortality of APE (I). These markers, including cardiac troponin T (cTnT), myoglobin, N-terminal pro-brain natriuretic peptide (NT-proBNP), heart-type fatty acid-binding protein (H-FABP), and growth differentiation factor-15 (GDF-15), have been regarded as helpful in predicting the clinical adverse events associated with APE. D-dimer is a cornerstone test in the diagnostic assessment of several conditions, like venous thromboembolism (VTE) or aortic syndromes, for both of which the risk of misdiagnosis and the possibility of overtesting is high.4 The higher levels of these biomarkers are considered to indicate cardiac dysfunction, and thus more aggressive treatment management is recommended.5 Nevertheless, significant discordances have been reported about the changes that occurred in the levels of these biomarkers.6–9 Moreover, a more sensitive and specific marker to determine the intermediate- and high-risk patients and predict the prognosis is needed in order to improve clinical outcomes.3
This study aimed to evaluate the prognostic impact of the novel biomarkers in patients with high-, intermediate-, and low-risk APE and explore the predictive power of these markers regarding the morbidity and mortality of APE.
Materials and Methods
Research Design
This prospective observational study included patients diagnosed with APE in the Emergency Department of Istanbul University, Faculty of Medicine between March 2008 and April 2010. The study was approved by the Istanbul University, Faculty of Medicine, Clinical Research Ethics Committee (approval number: 2947). The study was conducted in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent of the patients who volunteered for the study was obtained prior to the study.
Patient Group
All consecutive patients with suspicious clinical symptoms (acute onset dyspnea, chest pain, tachycardia, and tachypnea with the need for oxygen supplementation) associated with APE admitted to the emergency department were prospectively evaluated. The diagnosis of APE was confirmed by computed tomography (CT), ventilation/perfusion scintigraphy, or pulmonary angiography. The exclusion criteria were determined as follows: coexisting diseases (coronary artery disease, congestive heart failure, and chronic renal failure), cardiopulmonary resuscitation, stroke, cancer, pregnancy and extensive muscular injury.
Variables
Patients’ demographic and clinical data were collected. The risk factors for APE were determined. Echocardiography was performed on all patients to stratify the severity of APE. The echocardiographic parameters related to APE include pulmonary arterial pressure, right ventricular motion, and left ventricular ejection fraction (LVEF). Tricuspid annular plane systolic excursion (TAPSE) and right ventricular (RV) fractional area change (FAC) were measured according to guideline recommendations.10 The development of complications and mortality were evaluated during both in-hospital and follow-up periods (up to 90-day). Cardiopulmonary resuscitation, hemodynamic instability (systolic blood pressure <90 mmHg or a drop in systolic blood pressure by >40 mmHg for >15 min with signs of end-organ hypoperfusion), inotrope use, recurrent or diffuse / peripheral APE, development of lower limb thrombosis, the use of mechanical ventilation within one month of admission, newly developed chest pain and dyspnea, and bleeding episode due to anticoagulant use were regarded as the adverse events.9 APE-related death was considered in the development of death secondary to irreversible right ventricular failure or recurrence of APE.10 All-cause mortality was also investigated. Accordingly, the causes of the mortalities were determined by the primary researcher as cardiac disease, APE, malignancy, respiratory disease, infection/sepsis, cerebrovascular disease, dementia, vascular disease, and other causes.
Severity of APE
The patients were grouped as massive/high-risk, submassive/moderate-risk, and non-massive/low-risk groups based on the criteria defined previously in the literature.2,5,11,12 Accordingly, APE patients with shock or persistent hypotension with hemodynamic instability (ie, systolic blood pressure <90 mmHg or a drop of ≥40 mmHg for >15 min) were regarded as massive/high-risk patients; APE patients with right ventricular dysfunction (end-diastolic diameter of the right ventricle on the parasternal view>30mm and a systolic pulmonary artery pressure >30 mmHg) with or without increased troponin levels were regarded as submassive/moderate-risk patients; and APE patients with normal right ventricular function and normal troponin levels were regarded as non-massive/low-risk patients.13
Biomarkers
Venous blood samples were collected before the initiation of treatment for APE. After immediate centrifugation, serum samples were centrifuged and stored at −80 °C till the laboratory analysis for cTnT, D-dimer (Hyphen Biomed, D-Dimer, Catalog Number: RK023A), NT-proBNP (Biomedica Slovakia, NT-proBNP, Catalog Number: SK1204), myoglobin (Diagnostic Automation Inc, myoglobin, Catalog Number: SK-1667Z), H-FABP (Biocheck Inc, H-FABP, Catalog Number: BC-1123), and GDF-15/MIC-1 (Biovendor Research and Diagnostic Products, Human GDF-15/MIC-1 ELISA, Catalog Number: RD191135200R).
Follow-Up
All patients included in the study were followed up for 3-months through regular follow-up examinations conducted in the outpatient clinics and phone interviews if respiratory or lower limb symptoms were present.
Statistical Analysis
The primary outcome was the development of short-term (in-hospital or 30-day) or long-term (90-day) adverse events or death. Post-hoc power analysis was performed for the study, and the power of the study was found to be 85% at α = 0.05, for the biomarkers. Descriptive statistics were expressed as mean ± standard deviation values and as median values along with minimum-maximum in the case of continuous variables depending on whether they conform to the normal distribution or not. The Kruskal–Wallis test was used to compare more than two independent groups involving numerical variables, which were determined not to conform to normal distribution. The differences between the groups were evaluated using the Tukey or Dunn’s tests in case of homogeneous data based on whether they conform to the normal distribution. The Mann–Whitney U-test was used in the case of variables that were determined not to conform to normal distribution. Pearson’s Chi-Squared test and Fisher’s Exact test were used in order to compare the differences between categorical variables in 2×2 tables. Additionally, the Wilcoxon Signed-Rank test was used to evaluate the differences between the admission and 90th-day measurements in the case of variables that were determined not to conform to normal distribution. The receiver operating characteristic (ROC) analysis was used to determine the biomarkers’ cut-off values that can be used to predict mortality. The significance level (p-value) was set at 0.05.
Results
Hypertension, which was detected in 20 patients, was the most frequent (42.6%) comorbidity observed in the study group. Immobilization was detected as the most common (68.1%) predisposing factor for APE development.
Of the patients included in the study group, 14 (29.8%), 16 (34.0%), and 17 (36.2%) patients were categorized as low-risk, moderate-risk, and high risk-patients, respectively. No significant difference was found between the groups in terms of demographic and clinical characteristics (p>0.05) (Table 1).
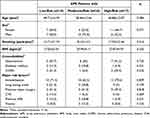 |
Table 1 Demographic and Clinical Characteristics of the Study Groups |
The systolic and diastolic blood pressure values of the patients with high-risk APE were significantly lower than those of moderate- and low-risk patients (p<0.001 in both cases) (Table 2).
 |
Table 2 The Distribution of the Clinical Parameters in the Study Groups |
The comparison of the patients as per the laboratory, CT, and echocardiography findings is shown in Table 3. The patients with high-risk APE had significantly lower serum albumin levels than those of moderate- and low-risk patients (p=0.031). There was no significant difference between the groups in terms of cTnT, myoglobin, HFABP, and D-dimer levels (Table 3). On the other hand, there was a significant difference between the groups in NT-proBNP and GDF-15 levels (p=0.009 and p=0.037, respectively). NT-proBNP levels of high-risk patients were significantly higher than those of moderate-risk and low-risk patients (p=0.012 and p=0.001, respectively). The extension of the thromboembolic lesions showed a similar distribution pattern in the lungs between the groups. The pulmonary artery pressure values measured at admission and 3rd-month follow-up were significantly higher in the high-risk APE patients (p<0.001 in both cases). The interventricular septal deviation and paradoxical movements were significantly more frequent in the high-risk patients (p<0.001). As shown, patients with high-risk APE had significantly lower TAPSE and RV FAC values (p<0.001). As shown, patients with high-risk APE had significantly lower TAPSE and RV FAC, and a higher number of patients with RV/LV ratio ≥1 (p<0.001).
 |
Table 3 Comparison of the Patients with Different Severity Grades According to the Laboratory, Computed Tomography and Echocardiography Findings |
There were nine (19.1%) mortalities in the study group by the 3rd-month follow-up: one in the low-risk, one in the moderate-risk, and seven in the high-risk APE group. APE was the cause of mortality in five of these mortalities. The other causes of mortality were postoperative complications in one patient who underwent colorectal surgery, and malignancies (breast, lung, and hematological system) in the remaining three patients. There was a significant difference between the high-risk and low-risk groups in the serum GDF-15 levels (p=0.013). The comparison of the biomarkers in patients who survived and were exitus revealed significant differences (Table 4). The H-FABP, D-dimer, and GDF-15 levels were significantly higher in patients who were exitus (p=0.023, p=0.008, and p=0.047, respectively).
 |
Table 4 The Comparison of the Cardiac Biomarkers in Patients Who Survived and Non-Survived Patients |
The results of the ROC analyses on the biomarkers’ predicting power of the development of adverse events and mortality are shown in Table 5 and Table 6. GDF-15 had the highest AUC value for predicting any adverse event (cut-off value= 9.3, AUC=0.796, CI 95%: 0.653–0.899) (Table 5). Additionally, the ROC analysis revealed that NT-ProBNP was the best predictor in predicting the all-cause mortality (AUC=0.889, CI 95%: 0.756–0.964), with a negative predictive value of 100% at >229.2 pg/mL (Table 6).
 |
Table 5 The Receiver Operating Curve Analysis of the Cardiac Biomarkers in Predicting the Development of Morbidity |
 |
Table 6 The Receiver Operating Curve Analysis of the Cardiac Biomarkers in Predicting the Development of All-Cause Mortality |
Discussion
The findings of this study revealed that higher levels of NT-proBNP and GDF-15 were significantly associated with high-risk APE. GDF-15 and NT-proPNP levels were found to have high predictive powers in predicting the development of adverse events and mortality, respectively, in patients with APE.
The serum levels of the natriuretic peptides indicate increased ventricular load in acute and chronic thromboembolic events.11,13,14 In parallel, it was speculated that there is a possible association between the right ventricular dysfunction secondary to APE and the increased levels of the natriuretic peptides.5,15 Jenab et al15 and Vuilleumier et al16 found that the increased levels of NT-proBNP and APE-related short- and long-term adverse outcomes and mortality were significantly associated. Nevertheless, they did not find any significant relation between other markers, including GDF-15, H-FABP, tenascin-C, and D-dimer, and the prognosis of APE. Bi et al13 reported that higher BNP, TnI, and D-dimer levels were positively correlated with the severity of APE and APE-related mortality. Andresen et al5 found that NT-proBNP decreased significantly following the successful treatment of APE using an invasive treatment method. This finding may suggest a negative correlation between NT-proBNp levels and revascularization success. Vuilleumier et al6 showed the negative predictive power of NT-proBNPon identifying low-risk patients with non-massive APE. In comparison, in this study, NT-proBNP was found to be the most potent independent predictive factor for hospitalization during the three-month follow-up period compared to other biomarkers, including cardiac troponins, H-FABP, myoglobin, and D-dimer. Additionally, increased NT-proBNP levels were found to be associated with high-risk APE, predicting the mortality in APE patients. Although the exact pathophysiological mechanisms for the increase in the natriuretic peptide levels and the associations thereof with the ventricular dysfunction remain obscure, the findings of this study and the respective findings reported in the literature suggest that NT-proBNP can be used as a marker for the severity of APE.6,13
GDF-15 has been identified as a molecule that reflects pressure overload or myocardial ischemia.15,17,18 Increased levels of GDF-15 in patients with APE might be related to underlying conditions like heart failure, renal insufficiency, or malignancy. In parallel, patients with such conditions were excluded from this study in order to assess the predicting power of GDF-15.15 A significant relation was found between higher GDF-15 levels and the development of adverse events in the positive direction, contrary to some of the findings reported in the literature.15 Similarly, Lankeit et al17 reported that GDF-15 is a promising marker for the risk stratification of APE. GDF-15 was the only independent predictor for a complicated APE course compared with other biomarkers such as cardiac troponins and NT-proBNP. Duran et al18 demonstrated the superiority of GDF-15 than NT-proBNP in predicting early death in normotensive APE patients. Although the sensitivity rates of GDF-15, cTnT, and NT-proBNP were found to be similar in predicting severe adverse events, GDF-15 may be a promising predictor for the early prediction of hemodynamic destabilization and bleeding complications in APE.18 In summary, it would be better to interpret the GDF-15 levels together with NT-proPNP levels in the risk stratification of APE patients.
Cardiac troponins are well-known biomarkers for cardiac injury. Several authors demonstrated the relationship between higher levels of cTnT and the severity of APE.10,11 Bi et al13 suggested that higher troponin levels may be attributed to the impairment of the right ventricular myocardial injury in APE patients. The interval between the onset of the symptoms and the peak levels of cardiac troponins seems to be the key indicating the respective levels in these patients.17 In parallel, several authors did not find the elevation of cardiac troponins as remarkable in APE patients, which is compatible with the findings of this study.3
H-BABF is significantly associated with the severity of APE.3,11,12,15 In Liu’s meta-analysis, higher H-FABP levels were reported to be associated with at least a 10-fold increased risk of adverse events in patients with APE.19 Due to the close association between H-FABP and cardiac injury, higher levels of this biomarker are likely in APE patients with cardiac dysfunction. Qian et al3 demonstrated the superiority of H-FABP as a predictor over cardiac troponins in APE patients. Similar results have been reported by other researchers.12
In comparison, no such relation was detected in this study, probably due to the severity of the right ventricular dysfunction. Similar findings have also been reported by several other authors.15 These controversial results might be attributed to the low number of primary outcomes or different inclusion and exclusion criteria outlined in other studies.
It has been suggested that the elevated levels of biomarkers such as troponins, myoglobin, and H-FABP in association with cardiomyocytes damage could provide more significant prognostic information in patients with APE.3,20,21 Nonetheless, it is evident that the impact of APE on the cardiac system should be given due consideration in this suggestion. In this study, NT-proBNP was found to be the most potent predictor of unfavorable outcomes in APE compared to troponins, myoglobin, and H-FABP, in line with the literature data.6,20 This finding may be regarded as evidence for the presence of right ventricular dysfunction in the study group.
Seropian et al9 studied the impact of high cardiac troponin levels together with low NT-proBNP levels (high troponin discordance) on the outcomes of APE patients. They reported that high troponin discordance was significantly associated with the worse outcomes in these patients. The use of different cut-off values for these biomarkers might be the reason for such contradictory results. Taking the different predictive powers of biomarkers into consideration, Liu et al7 recommended using a joint test, which included a number of abnormal biomarkers, for a better prediction of the long-term risk of APE recurrence and all-cause mortality. Rapid progression of the disease leading to variations in the levels of the biomarkers may also be the reason for such controversial outcomes.
The prospective design of this study was one of its major strengths. Nevertheless, there were also some limitations to this study. First, it was carried out as a single-center study with a relatively small sample. Secondly, the dynamic and quantitative tests of the biomarkers studied within the scope of this study to evaluate the time curve of the changes during an APE attack were not conducted. Due to these biomarkers’ short half-lives and circadian rhythm, serial measurements might be more effective in monitoring such associations.18,22
In conclusion, the higher levels of NT-proBNP and GDF-15 were found to be associated with more severe APE, worse outcomes, and mortality. Thus, these biomarkers can be used as indicators for predicting morbidity and mortality in relation to. Further large-scale studies are needed to clarify the potential roles of these biomarkers before they are considered for use in the risk stratification system for APE.
Data Sharing Statement
The data supporting the revelations of this study can be retrieved from the corresponding author upon reasonable request.
Informed Consent Statement
This prospective observational study included patients diagnosed with APE in the Emergency Department of Istanbul University, Faculty of Medicine between March 2008 and April 2010. The study was approved by the Istanbul University, Faculty of Medicine, Clinical Research ethics committee (approval number:2947). The study was conducted in accordance with the principles outlined in the Declaration of Helsinki. Written informed consent of the patients who volunteered for the study was obtained prior to the study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Disclosure
The authors have no relevant financial or non-financial interests to disclose for this work.
References
1. Blondon M, Jimenez D, Robert‐Ebadi H, et al. Comparative clinical prognosis of massive and non‐massive pulmonary embolism: a registry‐based cohort study. J Thromb Haemost. 2021;19:408–416. doi:10.1111/jth.15146
2. Gupta R, Ammari Z, Dasa O, et al. Long-term mortality after massive, submassive, and low-risk pulmonary embolism. Vasc Med. 2020;25:141–149. doi:10.1177/1358863X19886374
3. Qian H-Y, Huang J, Yang Y-J, et al. Heart-type fatty acid binding protein in the assessment of acute pulmonary embolism. Am J Med Sci. 2016;352:557–562. doi:10.1016/j.amjms.2016.08.018
4. Innocenti F, Lazzari C, Ricci F, Paolucci E, Agishev I, Pini R. D-dimer tests in the emergency department: current insights. Open Access Emerg Med. 2021;13:465–479. doi:10.2147/OAEM.S238696
5. Andresen M, González A, Mercado M, et al. Natriuretic peptide type-B can be a marker of reperfusion in patients with pulmonary thromboembolism subjected to invasive treatment. Int J Cardiovasc Imaging. 2012;28:659–666. doi:10.1007/s10554-011-9857-7
6. Vuilleumier N, Le Gal G, Verschuren F, et al. Cardiac biomarkers for risk stratification in non-massive pulmonary embolism: a multicenter prospective study. J Thromb Haemost. 2009;7:391–398. doi:10.1111/j.1538-7836.2008.03260.x
7. Liu X, Zheng L, Han J, et al. Joint analysis of D-dimer, N-terminal pro b-type natriuretic peptide, and cardiac troponin I on predicting acute pulmonary embolism relapse and mortality. Sci Rep. 2021;11:14909. doi:10.1038/s41598-021-94346-7
8. Duffett L, Castellucci LA, Forgie MA. Pulmonary embolism: update on management and controversies. BMJ. 2020;370:m2177. doi:10.1136/bmj.m2177
9. Seropian IM, Chiabrando JG, Damonte JI, et al. Prognosis of patients with acute pulmonary embolism and discordant right ventricle strain serum biomarkers. Int J Cardiol. 2021;340:88–93. doi:10.1016/j.ijcard.2021.08.032
10. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39.e14. doi:10.1016/j.echo.2014.10.003
11. Dursunoglu N, Dursunoglu D, Yildiz AI, Rota S. Evaluation of cardiac biomarkers and right ventricular dysfunction in patients with acute pulmonary embolism. Anadolu Kardiyol Dergisi/The Anatol J Cardiol. 2014. doi:10.5152/akd.2014.5828
12. Kaczyñska A, Pelsers MMAL, Bochowicz A, et al. Plasma heart-type fatty acid binding protein is superior to troponin and myoglobin for rapid risk stratification in acute pulmonary embolism. Clin Chim Acta. 2006;371:117–123. doi:10.1016/j.cca.2006.02.032
13. Bi W, Liang S, He Z, et al. The Prognostic Value of the Serum Levels of Brain Natriuretic Peptide, Troponin I, and D-Dimer, in Addition to the Neutrophil-to-Lymphocyte Ratio, for the Disease Evaluation of Patients with Acute Pulmonary Embolism. Int J Gen Med. 2021;14:303–308. doi:10.2147/IJGM.S288975
14. Naito A, Tanabe N, Jujo T, et al. Pentraxin3 in Chronic Thromboembolic Pulmonary Hypertension: a New Biomarker for Screening from Remitted Pulmonary Thromboembolism. PLoS One. 2014;9:e113086. doi:10.1371/journal.pone.0113086
15. Jenab Y, Pourjafari M, Sotoudeh M, et al. Comparing the effect of cardiac biomarkers on the outcome of normotensive patients with acute pulmonary embolism. Monaldi Arch Chest Dis. 2017;87. doi:10.4081/monaldi.2017.767
16. Vuilleumier N, Righini M, Perrier A, et al. Correlation between cardiac biomarkers and right ventricular enlargement on chest CT in non massive pulmonary embolism. Thromb Res. 2008;121:617–624. doi:10.1016/j.thromres.2007.07.003
17. Lankeit M, Kempf T, Dellas C, et al. Growth Differentiation Factor-15 for Prognostic Assessment of Patients with Acute Pulmonary Embolism. Am J Respir Crit Care Med. 2008;177:1018–1025. doi:10.1164/rccm.200712-1786OC
18. Duran L, Kayhan S, Guzel A, et al. The Prognostic Values of GDF-15 in Comparison with NT-proBNP in Patients with Normotensive Acute Pulmonary Embolism. Clin Lab. 2014;60. doi:10.7754/Clin.Lab.2013.130827
19. Liu M, Yuan X, Qiu X, et al. Prognostic Role of Heart-type Fatty Acid Binding Protein in Pulmonary Embolism: a Meta-analysis. Thromb Res. 2015;135:20–25. doi:10.1016/j.thromres.2014.10.007
20. Pruszczyk P, Bochowicz A, Kostrubiec M, et al. Myoglobin stratifies short-term risk in acute major pulmonary embolism. Clin Chim Acta. 2003;338:53–56. doi:10.1016/j.cccn.2003.07.017
21. Bonfanti L, Cervellin G, Calamai S, et al. Diagnostic significance of combining d-dimer with high-sensitivity cardiac troponin I for improving the diagnosis of venous thromboembolism in the emergency department. Acta Biomed. 2021;92. doi:10.23750/abm.v92i5.9752
22. Skowrońska M, Skrzyńska M, Machowski M, et al. Usefulness of GDF-15 concentrations in plasma in prognosing serious adverse events and bleeding in acute pulmonary embolism: a prospective observational study. Polish Arch Intern Med. 2020. doi:10.20452/pamw.15515
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
