Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Impact of Antidepressants on Cardiac Events and All-Cause Mortality in Parkinson’s Disease: A National Data-Linkage Study
Authors Orayj K
Received 18 June 2021
Accepted for publication 27 July 2021
Published 30 July 2021 Volume 2021:17 Pages 2499—2510
DOI https://doi.org/10.2147/NDT.S325521
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Khalid Orayj
Clinical Pharmacy Department, School of Pharmacy, King Khalid University, Abha, Saudi Arabia
Correspondence: Khalid Orayj
Clinical Pharmacy Department, School of Pharmacy, King Khalid University, Abha, 62529, Saudi Arabia
Tel +966 505442013
Email [email protected]
Purpose: This study investigated the 1-year risk of ischemic heart disease (IHD), all cardiovascular events, and all-cause mortality among newly diagnosed Parkinson’s disease (PD) patients who used antidepressants compared to those who did not.
Patients and Methods: Patients with PD aged 40 years or older were identified using data from 2000 through 2016 held within the Welsh Secure Anonymized Information Linkage (SAIL) databank. Antidepressant users were propensity-score matched 1:1 with non-users, adjusting for patients’ demographics, socioeconomic status, and multiple comorbidities. Cox proportional hazard regression analyses were performed to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for the association between the antidepressants and the study outcomes. The follow-up period was 1 year after the initial prescription of antidepressants.
Results: The study group comprised a total of 3364 participants, with numbers split equally between the antidepressant-user and non-user groups, based on the propensity score-matching process. Overall, the propensity score-adjusted model showed that antidepressant usage in PD patients was not significantly associated with the risk of IHD (HR = 1.05; 95% CI 0.63– 1.75) or all cardiovascular events (HR = 1.01; 95% CI 0.71– 1.45) compared to non-users. The propensity score-adjusted model also showed that the use of any antidepressant, regardless of its category, was not statistically significantly associated with all-cause mortality (HR = 0.81; 95% CI 0.65– 1.02). However, this association reached statistical significance in the multivariate adjusted model (HR = 0.67; 95% CI 0.54– 0.84).
Conclusion: There was no evidence that antidepressant use was associated with an increased risk of IHD or all cardiovascular events in newly diagnosed PD patients who suffered from depression. Furthermore, antidepressant use might reduce the mortality rate in PD patients during the first year after initiation.
Keywords: antidepressants, cardiovascular events, depression, ischemic heart disease, Parkinson’s disease
Introduction
Depression is a highly prevalent disease and a serious global health concern. According to the World Health Organization (WHO), it currently affects 322 million people worldwide.1,2 The most widely available treatments for symptoms are tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs).2 Despite having comparable efficacies, SSRIs have superseded TCAs due to their more benign overall safety profiles.2 Although numerous studies have demonstrated the efficacy of antidepressants in treating this condition,3,4 there have been inconsistent findings regarding their cardiovascular safety.
TCAs are linked to systematic inflammation that might increase cardiovascular risk5 and, especially, ischemic heart disease (IHD).6,7 By contrast, SSRIs can have cardioprotective effects due to their thrombolytic activity;8 however, they also exhibit antiplatelet activity and can constrict arterial vessels, which may increase the risk of other cardiac events such as stroke.9 Cardiac events, particularly IHD, are not linked only to the use of antidepressants; it has been established that depression itself is a significant risk factor for IHD and other cardiac events.10 Additionally, comorbidities that coexist with depression and antidepressant use, such as Parkinson’s disease (PD), might increase the cardiovascular risk.11
It is estimated that the prevalence of depression among PD patients can reach 35%, and antidepressants are commonly used to treat it.12 The reported prevalence of antidepressant use among PD patients ranges from 1.9% to 43.2%.13–22 This variation might be explained by differences in the time period under study. For example, studies conducted in the early 1990s have tended to report a lower prevalence of antidepressant use, such as 13.19% in Norway in 1992 (20) and 1.9% in US nursing homes from 1992 to 1996.19 By contrast, more recent studies have tended to report a greater prevalence of antidepressant use, such as 23% in Denmark in 200715 and 29.8% in the USA in 2014.23 This increase in the use of antidepressants in recent years is attributed to the increased recognition of depression in PD patients.24
Cardiac events, particularly IHD, are more prevalent in PD patients compared to non-PD controls.25–27 Drugs that are commonly used in PD patients and carry a risk of cardiac effects, such as dopamine agonists28,29 and antipsychotics,30,31 can have an impact on this phenomenon. Although antidepressants have been associated with IHD and other cardiac events in the general population,6,7 the correlation remains unclear in PD patients. Additionally, there is conflicting evidence in the literature of an association between antidepressant use and a higher risk of mortality in the general population and in patients with various diseases. While some studies have suggested that the use of antidepressants can reduce the mortality rate,32,33 others have not found such an effect.34 This inconsistency in results has also been observed in PD patients, with some studies reporting an increased risk of mortality in antidepressant users versus non-users,35 and other studies reporting the opposite.36 Variation in the association between antidepressant use and mortality risk might be due to the level of adherence to the medications, associated comorbidities and polypharmacy, or the extent of PD progression.37 To our knowledge, no previous studies have examined such associations in newly diagnosed PD patients using a large-scale data-linkage databank in which the role of disease progression has been minimized and comorbidities and polypharmacy have been controlled for.
Thus, the primary objective of this study was to assess the 1-year risk of IHD among antidepressant users compared with non-users in newly diagnosed PD patients. The risk of all cardiovascular events and all-cause mortality were also assessed as a secondary objective of the study.
Patients and Methods
Design and Data Source
This retrospective cohort study used data from the Welsh Secure Anonymized Information Linkage (SAIL) databank from 2000 to 2016. SAIL is a data-linkage system that covers 80% of Welsh general practice (GP) surgeries and is linked to other Welsh databases that contain additional patient-related data;32 these include demographic, hospitalization, and mortality data stored in the Welsh Demographic Service database, Patient Episode Database, and Annual District Death Extract (ADDE), respectively.38 Social deprivation status data were available from SAIL and measured using the Welsh Index of Multiple Deprivation (WIMD) scale.38 The Patient Episode Database was utilized to determine patients’ comorbidities and first cardiovascular hospitalization episode. Cardiovascular and all-cause mortality data were obtained using the ADDE. All data used in this study were anonymized and the protocol was approved by the Information Governance Review Panel (IGRP; reference number 0507).
Study Population and Definitions
The study population included all individuals older than 40 years who had a first definitive PD diagnosis Read code in SAIL and started taking PD medication between 2000 and 2016 (Appendix 1). Patients who were diagnosed with PD within 6 months of the SAIL registration date and/or had been prescribed antipsychotics in the year preceding diagnosis were excluded from the study.39
The index date was defined as the day of the first prescription of antidepressant medication in newly diagnosed PD patients. Patients were followed up for 1 year after the index date until the occurrence of an outcome of interest classified as model 1 (first IHD event), model 2 (first cardiovascular event such as arrhythmia, heart failure, IHD, stroke, or cardiovascular death), or model 3 (all-cause mortality). Survival times were measured in days. For all models, patients were censored if they transferred out from SAIL, if the study period ended without the occurrence of an outcome of interest, if antidepressant users changed or ceased the medications, or if the time between two consecutive prescriptions for the same antidepressant exceeded 30 days. Patients in model 1 were also censored if death or any cardiac hospitalization other than IHD (that is, arrhythmia, stroke, or heart failure) occurred. Patients in model 2 were also censored if non-cardiac death occurred.
The covariates extracted at the time of PD diagnosis from SAIL included age, gender, health-board location, WIMD deprivation status, previous comorbidities, and previous consumption of medications that might cause cardiovascular side effects. Appendix 2 details the covariate definitions.
Statistical Methods
Descriptive statistics (means and percentages) were used to examine demographics and other patient covariates.
Propensity Score Calculation and Matching
All confounding covariates with a p-value ≤0.20 for the Wald test in the bivariate logistic regression were used to calculate the propensity score estimates,34 which described the probability of receiving antidepressants on the index date. Data from antidepressant users and non-users were then subjected to propensity score-matching analysis using a 1:1 ratio with the nearest neighbor method without replacement. The caliper size was set at 0.2-times the standard deviation (SD) of the logit of the propensity scores.34
Time to Event Survival Analysis
Cox proportional hazards regression was used to examine the hazard ratio (HR) of IHD (model 1), cardiac events (model 2), and all-cause mortality (model 3) for propensity score-matching samples. The covariates included in the model were those with a p-value ≤0.20 according to single Cox regression.
To explore as many statistical associations as possible, two Cox regression approaches were utilized in this study. The first was multivariate Cox regression, in which all candidate covariates were incorporated in the regression model.
The second was propensity score adjusted Cox regression, in which a new propensity score estimate was calculated for every model, which represented the probability of developing the outcome of interest. Consequently, the calculated propensity score was added to the Cox regression model as a covariate, instead of the aforementioned covariates.40 Additionally, the main explanatory variable, which was the use of antidepressants, was added to all models. To maintain the linearity assumption of the propensity scores, they were divided into five groups as follows: 0–0.2, 0.21–0.4, 0.41–0.6, 0.61–0.8, and 0.81–1. The Schoenfeld test was utilized to verify the assumption of proportional hazards; the results confirmed that this assumption was met in all three models. Kaplan–Meier graphs were used to express the probability of IHD, cardiac events, and all-cause mortality from the index date until the event or exclusion date. All statistical analyses were conducted using SPSS version 25. A p-value <0.05 was considered statistically significant.
Results
Patient Characteristics
Between January 1, 2000 and December 31, 2016 there were 13,293 PD patients in the SAIL databank. After applying the exclusion criteria, 9142 patients remained (Figure 1). Propensity score matching analysis identified 3364 patients, 1682 (50%) of whom were treated with antidepressants and 1682 (50%) of whom were untreated (Figure 1). The main characteristics of the antidepressant user and non-user groups are shown in Table 1. Overall, the mean age of the participants was 75.9 years (SD=7.5), the most common age group was 61–80 years (1845 cases, 54.8%), and there were more males (2034 cases, 60.4%) than females. Most participants were prescribed levodopa as the first-line PD medication (2876 cases, 85.4%) followed by dopamine agonists (306 cases, 9.1%), and then monoamine oxidase-B (MAO-B) inhibitors (182 cases, 5.4%). Among the antidepressant users included in the matched cohort, 57.5% received SSRIs, whereas 26.5% received TCAs, and the remaining 16% received other antidepressants (Table 1). Citalopram (SSRI drug) compromised almost third of all antidepressants prescribed (33.7%), followed by amitriptyline (TCA drug) (14.9%) and fluoxetine (SSRI) (10.6%) (Table 2). In the antidepressant-users group and over one year after the first antidepressants prescription, 31 IHD cases (n=31), 58 cardiovascular events (3.4%), and 136 death (8.1%) occurred (Table 1).
 |
Table 1 Patients Demographics |
 |
Table 2 Number of Antidepressants in Antidepressant Users Cohort |
 |
Figure 1 Cases selection and exclusion process. |
Hospitalization Due to IHD
Appendix 3 illustrates the detailed outcomes of univariate and multivariate Cox regression analyses in all three models examined. The propensity score-adjusted model and the relevant HR in antidepressant users are shown in Table 3. Overall, the propensity score-adjusted model showed that taking antidepressants in PD patients had no significant association with the risk of IHD compared to non-users (HR = 1.05, 95% confidence interval [CI] 0.63–1.75). No significant interactions were reported between any of the different antidepressant categories or individual drugs and IHD (Table 3).
 |
Table 3 Results of Multivariate and Propensity Scores Adjusted Cox Regression Models That Examining the Relationship Between Antidepressants and the Study Outcomes |
Hospitalization Due to All Cardiovascular Events
The propensity score-adjusted model suggested that there was no significant difference between patients who used antidepressants and non-users in terms of developing cardiovascular events, specifically arrhythmia, heart failure, IHD, stroke, or cardiovascular death (HR = 1.01, 95% CI 0.71–1.45) (Table 3). Non-significant associations with all cardiovascular events were also reported among different antidepressant categories and individual drugs (Table 3).
All-Cause Mortality
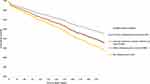
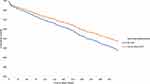
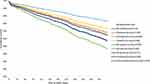
The propensity score-adjusted model showed that the use of any antidepressant, regardless of its category, had no statistically significant association with all-cause mortality (HR = 0.81; 95% CI 0.65–1.02) (Table 3 and Figure 2). This association reached statistical significance in the multivariate adjusted model (HR = 0.67, 95% CI 0.54–0.84). Multivariate analysis of the TCA- and SSRI-user groups showed reduced mortality in the latter (HR = 0.7, 95% CI 0.54–0.91), and to a lesser extent in the former (HR= 0.84; 95% CI 0.48–0.98) (Table 3). Both TCAs and SSRIs showed no significant associations in the propensity score-adjusted model (Table 3 and Figure 3). Among the individual antidepressants, mirtazapine had the lowest HR (0.43, 95% CI 0.21–0.87) in the all-cause mortality multivariate adjusted model, followed by citalopram (HR=0.65, 95% CI 0.47–0.91) (Table 3). The propensity score model, however, revealed no significant association between any of the individual antidepressants and all-cause mortality (Table 3 and Figure 4).
Discussion
There is growing evidence that individuals with PD are more likely to develop cardiovascular diseases, particularly IHD.25 Several factors increase the risk of developing IHD in PD patients, including hereditary inclination, heavy smoking, and diabetes mellitus.25 Furthermore, because PD is more common among the elderly, patients are likely to have higher cardiovascular morbidity profiles and an increased prevalence of polypharmacy.41 On average, a PD patient will be prescribed five different drugs, and this number rises with increasing age and as motor and non-motor symptoms worsen.42 Certain medications that are commonly used in PD patients, such as non-steroidal anti-inflammatory drugs (NSAIDs)43 and antipsychotics,44 are associated with an increased risk of cardiovascular events. Other medications, such as antidepressants, may also increase the risk of cardiovascular events, particularly IHD,45 although they have yet to be evaluated in PD patients.
This study analyzed data collected from almost 80% of the Welsh population over a period of 17 years. Among antidepressant users, citalopram (SSRI) constituted almost a third of prescribed antidepressants, which is in line with guidelines that recommend use of an SSRI as a first-line therapy to treat depression in PD patients.3 While there is evidence of its efficacy to treat depression,3 which could explain why it was the second most common antidepressant prescribed in this cohort (14.9%), amitriptyline (TCA) is not highly recommended in PD patients due its anticholinergic side effects.3 Although the current study only included antidepressants prescribed to PD patients after a diagnosis of depression, it is still possible that the relatively high prescribing rate of amitriptyline in this study might be explained by the fact that amitriptyline can be used to treat conditions other than depression, such as migraine and tension headaches.24
No significant association was found between antidepressant use and IHD and other cardiovascular event risks during the first year after PD diagnosis in patients taking these medications compared with non-users. Similar findings were observed for the associations of each antidepressant category and individual antidepressants with IHD and other cardiovascular event risks. Previous studies have reported inconsistent findings in this regard. Some have suggested that SSRIs may increase the risk of IHD while TCAs and other types of antidepressant do not carry such a risk.46,47 In contrast, others have found that TCAs are associated with cardiovascular risk (including IHD), while SSRIs appear to be safer in this regard.6,48 Moreover, a meta-analysis of 16 observational studies found that neither SSRIs nor TCAs increased the risk of IHD and other cardiac events.49 These inconsistent results might be due to differences in the inclusion and exclusion criteria have been applied in each study. The current study did not find any such association in PD patients during a short follow-up period of 1 year. The current study examined the immediate cardiovascular risk of antidepressants in patients who were diagnosed with depression after their PD diagnosis compared to those who were free from depression. This might have introduced an indication bias, since depression itself is a risk factor that could contribute to IHD; however, this possibility was minimized by restricting the follow-up period to 1 year, minimizing the effect of depression on IHD and other cardiovascular risks.50 In diseases like PD, in which the cardiovascular risks are high51 and the progressive and complex nature of the disorders exacerbate them over time,52 it is difficult for long-term follow-up studies to attribute IHD risks to either depression or antidepressant use, even when applying sophisticated statistical analysis that are intended to control for all possible confounders.53 Mitigating the effect of PD progression by shortening the follow-up period may therefore be the most appropriate approach to test the direct effect of antidepressants on IHD risk, although this approach has its drawbacks as it cannot test the risk in the long term.
Previous reports suggested that TCAs can cause weight gain54 and exacerbate cardiotoxic effects, such as postural hypotension and QT interval prolongation,55,56 by blocking the norepinephrine and serotonin reuptake at nerve terminals and blocking sodium channels.57 By contrast, SSRIs were reported to have both cardioprotective and cardiotoxic properties. SSRIs inhibit serotonin reuptake in presynaptic terminals, which could lead to increased heart rate and constriction of the coronary arteries;58 however, they can also have cardioprotective properties by inhibiting platelet aggregation, reducing inflammation, and improving endothelial function.8 These pharmacological effects of both TCAs and SSRIs did not appear to have a direct clinical impact on newly diagnosed PD patients who used antidepressants in the short term, according to the current study. However, this did not preclude cardiac risk in the long term.
The multivariate adjusted model in this study suggested that the general use of antidepressants significantly decreased all-cause mortality risk in PD patients. This reduction in mortality risk was observed across different antidepressant categories (that is, TCAs, SSRIs, and other antidepressants), as well as in two individual antidepressants (that is, citalopram and mirtazapine) in the multivariate adjusted model. Although the propensity score-adjusted model did not reach statistical significance; the results of the multivariate model highlight the possible role of antidepressants in reducing the mortality rate in PD patients. Previous studies have reported a reduction in mortality rate among antidepressant users compared to non-users in patients with dementia,33 cardiovascular disease,59 and some other disorders.60,61 In PD patients, only two previous studies examined the association between antidepressants and mortality rate, and they reported contradictory results: Frandsen et al found that the general use of antidepressants was associated with an increased mortality rate,35 whereas Shoval et al found the opposite.36 This divergence could be attributed to the confounding factors that affected both studies. For example, Frandsen et al did not account for any comorbidities that the PD patients may have suffered from, which could have resulted in inaccurate estimates.35 The results of the current study were similar to those of Shoval et al.36 An additional finding of the current work was that among the individual antidepressants, only citalopram and mirtazapine were associated with a significant reduction in the multivariate adjusted model. It is unlikely that mirtazapine has pharmacological proprieties that lead to a reduction in mortality rate; in fact, previous studies reported that it could increase the mortality rate due its association with cardiovascular mortality and weight gain in the general population.62,63 However, no studies so far have examined the association of mirtazapine with mortality rate in PD patients, and this requires further investigation.
There are several possible interpretations of the reduction in mortality rate associated with antidepressant use in newly diagnosed PD patients in this study. For instance, PD patients who use antidepressants might have regular contact with movement disorder specialists or PD nurses, resulting in better outcomes for depression and other comorbidities.64 Moreover, the control group in the current study included PD patients who might have been suffering from undiagnosed depression without treatment, which in itself is a cause of mortality.65 Indeed, underrecognized depression in newly diagnosed PD patients has been reported as a critical problem in the literature.66 Caution should therefore be taken when attributing the reduction in mortality rate observed in the current study only to the use of antidepressants.
This was the first study to explore the relationship between antidepressant use and cardiovascular events, particularly IHD, in newly diagnosed PD patients. It benefitted from having a large sample size and utilizing a comprehensive population database. Furthermore, the propensity score-matching model used in the analysis boosted the statistical significance of the study findings.67
The current study had some limitations. Medical record codes were utilized to identify patients with PD and other diagnoses, without validation from neurologists or movement-disorder specialists. Also, the results might have been skewed by indication bias. For example, the patients who used antidepressants may have had more severe PD, resulting in a greater mortality rate. Therefore, causality could not be concluded. However, action was taken to minimize this bias by restricting the analysis to newly diagnosed PD patients. The short follow-up period could be a limitation; however, it could also be seen as a necessity when pursuing the goal of analyzing the immediate risks of antidepressants. Further research to assess the long-term effects of antidepressants while controlling for the confounding effects of PD neurodegenerative progression is needed.
Conclusions
Although antidepressants play an important role in treating patients with PD, their use has been associated with certain risks in the general population.10,68 This study revealed no association between antidepressant use and either IHD or all cardiovascular events in newly diagnosed PD patients. Additionally, the multivariate model suggested that the use of antidepressants reduced the mortality rate at 1 year of follow up. These findings highlighted that TCAs, SSRIs, and other antidepressants might be safe for use in the treatment of depression in patients with PD. There is a need for further research with larger sample sizes and longer follow-up periods. In the meantime, the advantages of antidepressants for treating patients with PD must continue to be balanced against the safety concerns.
Abbreviations
CI, confidence interval; GP, general practice; HR, hazard ratio; IGRP, Information Governance Review Panel; IHD, ischemic heart disease; MAO-B, monoamine oxidase-B; NSAID, non-steroidal anti-inflammatory drug; PD, Parkinson’s disease; SAIL, Secure Anonymized Information Linkage; SD, standard deviation; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; WHO, World Health Organization; WIMD, Welsh Index of Multiple Deprivation.
Acknowledgments
I acknowledge the help provided by the SAIL team in all stages of the study.
Funding
The study was supported by King Khalid University, Abha, Saudi Arabia.
Disclosure
The author reports no conflicts of interest in this work.
References
1. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: World Health Organization; 2017.
2. Thom R, Silbersweig DA, Boland RJ. Major depressive disorder in medical illness: a review of assessment, prevalence, and treatment options. Psychosom Med. 2019;81(3):246–255. doi:10.1097/PSY.0000000000000678
3. Mills KA, Greene MC, Dezube R, Goodson C, Karmarkar T, Pontone GM. Efficacy and tolerability of antidepressants in Parkinson’s disease: a systematic review and network meta‐analysis. Int J Geriatr Psychiatry. 2018;33(4):642–651. doi:10.1002/gps.4834
4. Moncrieff J, Kirsch I. Efficacy of antidepressants in adults. BMJ. 2005;331(7509):155–157. doi:10.1136/bmj.331.7509.155
5. Thanacoody HR, Thomas SH. Tricyclic antidepressant poisoning. Toxicol Rev. 2005;24(3):205–214. doi:10.2165/00139709-200524030-00013
6. Cohen HW, Gibson G, Alderman MH. Excess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agents. Am J Med. 2000;108(1):2–8. doi:10.1016/S0002-9343(99)00301-0
7. Maslej MM, Bolker BM, Russell MJ, et al. The mortality and myocardial effects of antidepressants are moderated by preexisting cardiovascular disease: a meta-analysis. Psychother Psychosom. 2017;86(5):268–282. doi:10.1159/000477940
8. Andrade C, Kumar CB, Surya S. Cardiovascular mechanisms of SSRI drugs and their benefits and risks in ischemic heart disease and heart failure. Int Clin Psychopharmacol. 2013;28(3):145–155. doi:10.1097/YIC.0b013e32835d735d
9. Shin D, Oh YH, Eom CS, Park SM. Use of selective serotonin reuptake inhibitors and risk of stroke: a systematic review and meta-analysis. J Neurol. 2014;261(4):686–695. doi:10.1007/s00415-014-7251-9
10. Nezafati MH, Vojdanparast M, Nezafati P. Antidepressants and cardiovascular adverse events: a narrative review. ARYA Atheroscler. 2015;11(5):295–304.
11. Park JH, Kim DH, Park YG, et al. Association of Parkinson disease with risk of cardiovascular disease and all-cause mortality: a nationwide, population-based cohort study. Circulation. 2020;141(14):1205–1207. doi:10.1161/CIRCULATIONAHA.119.044948
12. Schapira AHV, Chaudhuri KR, Jenner P. Non-motor features of Parkinson disease. Nat Rev Neurosci. 2017;18(7):435–450.
13. Qureshi SU, Amspoker AB, Calleo JS, Kunik ME, Marsh L. Anxiety disorders, physical illnesses, and health care utilization in older male veterans with Parkinson disease and comorbid depression. J Geriatr Psychiatry Neurol. 2012;25(4):233–239. doi:10.1177/0891988712466458
14. Althaus A, Becker OA, Spottke A, et al. Frequency and treatment of depressive symptoms in a Parkinson’s disease registry. Parkinsonism Relat Disord. 2008;14(8):626–632. doi:10.1016/j.parkreldis.2008.01.016
15. Brandt-Christensen M, Garcia Lopez A, Morkeberg Nilsson F, Kragh Andersen P, Vedel Kessing L. Parkinson’s disease and antidepressant drug treatment: a case-register study. Parkinsonism Relat Disord. 2007;13(7):406–410. doi:10.1016/j.parkreldis.2007.01.006
16. Weintraub D, Moberg PJ, Duda JE, Katz IR, Stern MB. Recognition and treatment of depression in Parkinson’s disease. J Geriatr Psychiatry Neurol. 2003;16(3):178–183. doi:10.1177/0891988703256053
17. Vanacore N, Bianchi C, Da Cas R, Rossi M. Use of antiparkinsonian drugs in the Umbria Region. Neurol Sci. 2003;24(3):221–222. doi:10.1007/s10072-003-0140-0
18. Gony M, Lapeyre-Mestre M, Montastruc JL; French Network of Regional Pharmacovigilance C. Risk of serious extrapyramidal symptoms in patients with Parkinson’s disease receiving antidepressant drugs: a pharmacoepidemiologic study comparing serotonin reuptake inhibitors and other antidepressant drugs. Clin Neuropharmacol. 2003;26(3):142–145.
19. Lapane KL, Fernandez HH, Friedman JH. Prevalence, clinical characteristics, and pharmacologic treatment of Parkinson’s disease in residents in long-term care facilities. Pharmacotherapy. 1999;19(11I):1321–1327. doi:10.1592/phco.19.16.1321.30877
20. Aarsland D, Larsen JP, Cummins JL, Laake K. Prevalence and clinical correlates of psychotic symptoms in Parkinson disease: a community-based study. Arch Neurol. 1999;56(5):595–601. doi:10.1001/archneur.56.5.595
21. Trewin VF, Lawrence CJ, Abdulla AJ, Pearce VR, Veitch GB, Roach M. Differences in drug prescribing patterns in elderly parkinsonian patients identified at hospital admission. Pharm World Sci. 1997;19(6):275–278. doi:10.1023/A:1008669826178
22. Richard IH, Kurlan R. A survey of antidepressant drug use in Parkinson’s disease. Parkinson Study Group. Neurology. 1997;49(4):1168–1170.
23. Early NK, Peckham AM, Fairman KA, Sclar DA. Prevalence of depression and receipt of antidepressant pharmacotherapy among patients with Parkinson’s disease: a national assessment of US office-based physician visits. J Parkinsonism Restless Legs Syndrome. 2017;7:79–84. doi:10.2147/JPRLS.S147203
24. Bega D, Wu SS, Pei Q, Schmidt PN, Simuni T. Recognition and treatment of depressive symptoms in Parkinson’s disease: the NPF dataset. J Parkinsons Dis. 2014;4(4):639–643. doi:10.3233/JPD-140382
25. Scorza FA, Fiorini AC, Scorza CA, Finsterer J. Cardiac abnormalities in Parkinson’s disease and Parkinsonism. J Clin Neurosci. 2018;53:1–5. doi:10.1016/j.jocn.2018.04.031
26. McLean G, Hindle JV, Guthrie B, Mercer SW. Co-morbidity and polypharmacy in Parkinson’s disease: insights from a large Scottish primary care database. BMC Neurol. 2017;17(1):126. doi:10.1186/s12883-017-0904-4
27. Yang YW, Hsieh TF, Li CI, et al. Increased risk of Parkinson disease with diabetes mellitus in a population-based study. Medicine (Baltimore). 2017;96(3):e5921. doi:10.1097/MD.0000000000005921
28. Schade R, Andersohn F, Suissa S, Haverkamp W, Garbe E. Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med. 2007;356(1):29–38. doi:10.1056/NEJMoa062222
29. Crispo JAG, Willis AW, Thibault DP, et al. Associations between cardiovascular events and nonergot dopamine agonists in Parkinson’s disease. Movement Disord Clin Practice. 2016;3(3):257–267. doi:10.1002/mdc3.12286
30. Waring WS. Clinical use of antidepressant therapy and associated cardiovascular risk. Drug, Healthc Patient Saf. 2012;4:93. doi:10.2147/DHPS.S28804
31. Rotella F, Cassioli E, Calderani E, et al. Long-term metabolic and cardiovascular effects of antipsychotic drugs. A meta-analysis of randomized controlled trials. Eur Neuropsychopharmacol. 2020;32:56–65.
32. Tiihonen J, Suokas JT, Suvisaari JM, Haukka J, Korhonen P. Polypharmacy with antipsychotics, antidepressants, or benzodiazepines and mortality in schizophrenia. Arch Gen Psychiatry. 2012;69(5):476–483. doi:10.1001/archgenpsychiatry.2011.1532
33. Enache D, Fereshtehnejad SM, Kareholt I, et al. Antidepressants and mortality risk in a dementia cohort: data from SveDem, the Swedish Dementia Registry. Acta Psychiatr Scand. 2016;134(5):430–440. doi:10.1111/acps.12630
34. Veien KT, Videbaek L, Schou M, et al. High mortality among heart failure patients treated with antidepressants. Int J Cardiol. 2011;146(1):64–67. doi:10.1016/j.ijcard.2010.01.006
35. Frandsen R, Baandrup L, Kjellberg J, Ibsen R, Jennum P. Increased all-cause mortality with psychotropic medication in Parkinson’s disease and controls: a national register-based study. Parkinsonism Relat Disord. 2014;20(11):1124–1128. doi:10.1016/j.parkreldis.2014.07.012
36. Shoval G, Stubbs B, Balicer RD, et al. Low adherence to antidepressants is associated with increased mortality in Parkinson disease patients. Parkinsonism Relat Disord. 2017;43:92–96. doi:10.1016/j.parkreldis.2017.07.032
37. Frisina PG, Tenenbaum HR, Borod JC, Foldi NS. The effects of antidepressants in Parkinson’s disease: a meta-analysis. Int J Neurosci. 2008;118(5):667–682. doi:10.1080/00207450701239418
38. Jones KH, Ford DV, Lyons RA. The SAIL Databank: 10 Years of Spearheading Data Privacy and Research Utility. Sail Publications, Swansea University; 2017.
39. Rochon PA, Stukel TA, Sykora K, et al. Atypical antipsychotics and parkinsonism. Arch Intern Med. 2005;165(16):1882–1888. doi:10.1001/archinte.165.16.1882
40. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–718. doi:10.1093/aje/kwk052
41. Vrettos I, Voukelatou P, Katsoras A, Theotoka D, Kalliakmanis A. Diseases linked to polypharmacy in elderly patients. Curr Gerontol Geriatr Res. 2017;2017:4276047.
42. Csoti I, Herbst H, Urban P, Woitalla D, Wullner U. Polypharmacy in Parkinson’s disease: risks and benefits with little evidence. J Neural Transm (Vienna). 2019;126(7):871–878. doi:10.1007/s00702-019-02026-8
43. McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011;8(9):e1001098. doi:10.1371/journal.pmed.1001098
44. Lin ST, Chen CC, Tsang HY, et al. Association between antipsychotic use and risk of acute myocardial infarction: a nationwide case-crossover study. Circulation. 2014;130(3):235–243. doi:10.1161/CIRCULATIONAHA.114.008779
45. Hamer M, Batty GD, Seldenrijk A, Kivimaki M. Antidepressant medication use and future risk of cardiovascular disease: the Scottish Health Survey. Eur Heart J. 2011;32(4):437–442. doi:10.1093/eurheartj/ehq438
46. Coupland CA, Dhiman P, Barton G, et al. A study of the safety and harms of antidepressant drugs for older people: a cohort study using a large primary care database. Health Technol Assess. 2011;15(28):
47. Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–856. doi:10.1001/archgenpsychiatry.2009.81
48. Lapane KL, Zierler S, Lasater TM, Barbour MM, Carleton R, Hume AL. Is the use of psychotropic drugs associated with increased risk of ischemic heart disease? Epidemiology. 1995;6(4):376–381. doi:10.1097/00001648-199507000-00008
49. Oh SW, Kim J, Myung SK, Hwang SS, Yoon DH. Antidepressant use and risk of coronary heart disease: meta-analysis of observational studies. Br J Clin Pharmacol. 2014;78(4):727–737. doi:10.1111/bcp.12383
50. Anda R, Williamson D, Jones D, et al. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of U.S adults. Epidemiology. 1993;4(4):285–294. doi:10.1097/00001648-199307000-00003
51. Alves M, Caldeira D, Ferro JM, Ferreira JJ. Does Parkinson’s disease increase the risk of cardiovascular events? A systematic review and meta-analysis. Eur J Neurol. 2020;27(2):288–296. doi:10.1111/ene.14076
52. Potashkin J, Huang X, Becker C, Chen H, Foltynie T, Marras C. Understanding the links between cardiovascular disease and Parkinson’s disease. Mov Disord. 2020;35(1):55–74. doi:10.1002/mds.27836
53. Joseph K, Mehrabadi A, Lisonkova S. Confounding by indication and related concepts. Curr Epidemiol Rep. 2014;1(1):1–8. doi:10.1007/s40471-013-0004-y
54. Kivimaki M, Hamer M, Batty GD, et al. Antidepressant medication use, weight gain, and risk of type 2 diabetes: a population-based study. Diabetes Care. 2010;33(12):2611–2616. doi:10.2337/dc10-1187
55. Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010;67(11):1067–1074. doi:10.1016/j.biopsych.2009.12.012
56. Licht CM, de Geus EJ, Seldenrijk A, et al. Depression is associated with decreased blood pressure, but antidepressant use increases the risk for hypertension. Hypertension. 2009;53(4):631–638. doi:10.1161/HYPERTENSIONAHA.108.126698
57. Whyte IM, Dawson AH, Buckley NA. Relative toxicity of venlafaxine and selective serotonin reuptake inhibitors in overdose compared to tricyclic antidepressants. QJM. 2003;96(5):369–374. doi:10.1093/qjmed/hcg062
58. Vikenes K, Farstad M, Nordrehaug JE. Serotonin is associated with coronary artery disease and cardiac events. Circulation. 1999;100(5):483–489. doi:10.1161/01.CIR.100.5.483
59. Biffi A, Scotti L, Rea F, et al. Adherence to antidepressants and mortality in elderly patients with cardiovascular disease. Clin Drug Investig. 2018;38(7):593–602. doi:10.1007/s40261-018-0642-4
60. Avrahamy H, Shoval G, Hoshen M, et al. Association between adherence to SSRI treatment and mortality among individuals with metabolic syndrome components. Pharmacopsychiatry. 2021. doi:10.1055/a-1425-7246
61. Shoval G, Balicer RD, Feldman B, et al. Adherence to antidepressant medications is associated with reduced premature mortality in patients with cancer: a nationwide cohort study. Depress Anxiety. 2019;36(10):921–929. doi:10.1002/da.22938
62. Howland RH. Mortality risk of mirtazapine: guilt by association? JAMA Psychiatry. 2014;71(5):585–586. doi:10.1001/jamapsychiatry.2013.4582
63. Khan A, Faucett J, Morrison S, Brown WA. Comparative mortality risk in adult patients with schizophrenia, depression, bipolar disorder, anxiety disorders, and attention-deficit/hyperactivity disorder participating in psychopharmacology clinical trials. JAMA Psychiatry. 2013;70(10):1091–1099. doi:10.1001/jamapsychiatry.2013.149
64. Jarman B, Hurwitz B, Cook A, Bajekal M, Lee A. Effects of community based nurses specialising in Parkinson’s disease on health outcome and costs: randomised controlled trial. BMJ. 2002;324(7345):1072–1075. doi:10.1136/bmj.324.7345.1072
65. Hughes TA, Ross HF, Mindham RH, Spokes EG. Mortality in Parkinson’s disease and its association with dementia and depression. Acta Neurol Scand. 2004;110(2):118–123. doi:10.1111/j.1600-0404.2004.00292.x
66. Rihmer Z, Gonda X, Dome P. Depression in Parkinson’s disease. Ideggyogy Sz. 2014;67(7–8):229–236.
67. Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi:10.1080/00273171.2011.568786
68. Sprenger F, Poewe W. Management of motor and non-motor symptoms in Parkinson’s disease. CNS Drugs. 2013;27(4):259–272. doi:10.1007/s40263-013-0053-2
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.