Back to Journals » OncoTargets and Therapy » Volume 16
Immunotherapy Combined with Chemotherapy in Relapse Metaplastic Breast Cancer
Authors Chen L, Meng Z, Zhou Z, Li X, Zhao L, Jia Z, Chen J, Tian Y, Meng Q, Liu Y
Received 17 August 2023
Accepted for publication 26 October 2023
Published 30 October 2023 Volume 2023:16 Pages 885—890
DOI https://doi.org/10.2147/OTT.S435958
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Arseniy Yuzhalin
Ling Chen,1,* Zhe Meng,2,* Zhiguo Zhou,1,* Xiaomin Li,2 Liyan Zhao,2 Zhaohui Jia,2 Jingli Chen,3 Ye Tian,3 Qingju Meng,2 Yibing Liu1
1The Fourth Hospital of Hebei Medical University, Shijiazhuang, Hebei Province, 050011, People’s Republic of China; 2The First Affiliated Hospital of Xingtai Medical College, Xingtai, Hebei Province, 054000, People’s Republic of China; 3Hebei Medical University, Shijiangzhuang, Hebei Province, 050011, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yibing Liu, Department of Medical Oncology, The Fourth Hospital of Hebei Medical University, 12 JianKang Road, Shijiazhuang, Hebei Province, 050011, People’s Republic of China, Tel +86-13831173220, Email [email protected] Qingju Meng, Department of Orthopedics, The First Affiliated Hospital of Xingtai Medical College, 376 Shun de Road, Qiaodong District, Xingtai, Hebei Province, People’s Republic of China, Tel +86-13780444436, Email [email protected]
Abstract: Metaplastic breast cancer (MBC) is a rare disease, and there was rarely reported the treatment after recurrence and metastasis. Here, we report the treatment of an adult patient who suffered from MBC with lung, lymph nodes and left pleura metastasis after radical surgery. The next-generation sequencing result demonstrated that it had tumor mutational burden (TMB) of 12.0 Muts/Mb and microsatellite stability. The patient received sintilimab, an immune checkpoint inhibitor, plus chemotherapy and achieved partial response (PR). This is a report of a good outcome of metastatic MBC achieving 24 months of progression-free survival (PFS) and 39 months of overall survival (OS) with a combination therapy of immune checkpoint inhibitor and chemotherapy. Immuno-chemotherapy may have antitumor activity for relapse MBC. TMB may serve as a potential predictor associated with PD-1 inhibitors in MBC and help clinicians make an optimum treatment strategy.
Keywords: metaplastic breast cancer, tumor mutational burden, immunotherapy, chemotherapy, progression-free survival, overall survival
Background
Metaplastic breast cancer (MBC) is a rare histological subtype of breast cancer, accounting for 0.2%~0.5% of all breast cancer cases. The pathological type of MBC is unique, and glandular components can be partially or completely replaced by non-glandular components.1,2 It was first reported in 1948 by Halpert B and Young MO.3 “Metaplastic breast cancer” was replaced by “metaplastic breast cancer with mesenchymal differentiation (MBC)” in the 2012 World Health Organization (WHO) classification of the breast.4 Because of its rarity, only a few small sample size retrospective analyses or case reports of MBC have been reported in the past.5–17 These limited studies showed that MBC is always an aggressive, poorly differentiated, hormone receptor-negative tumor, with a worse prognosis than other pathological subtypes.5,7,8 Despite the poor prognosis of MBC, evidence for the effective management remains limited. Currently, MBC is mainly based on multidisciplinary treatment, including surgery, chemotherapy, radiotherapy, endocrine therapy and targeted therapy. However, the benefit of systemic therapy agents remains unclear.18 Till now, accurate information concerning immunotherapy in metastatic MBC is unavailable.
Case Presentation
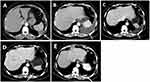
An adult patient presented to the Breast Surgery with complaints of a left breast tumor in October 2018. Ultrasonic scans revealed a lesion in the left mammary gland and left axillary lymph node. The patient underwent modified radical mastectomy (MRM) in Aug 2018. Postoperative pathology suggested that the mass size was 2.8*1.9cm, differentiation level II. There was no vascular tumor emboli or nerve involvement, but the underlying lymph node had metastasis (1/17). Immunohistochemistry showed ER(-), PR(-), HER-2(0), P53(+++), ki-67(30%), P120(+), CK56(gland+), SMA(-), Desmin(-), Vimentin(++), S-100(-), EMA(gland+), CK(gland+), CD68(+). The patient was diagnosed with MBC, stage IIB (pT2N1M0). Eight cycles of postoperative adjuvant therapy were administrated between Aug 2018 and Jan 2019, including four cycles of Cyclophosphamide (500mg/m2) plus Epirubicin (100mg/m2), at 14-day intervals, and four cycles of Docetaxel (100mg/m2), at 21-day intervals. However, in a follow-up in December 2019, Computed Tomography (CT) and Positron Emission Tomography (PET)-CT revealed lung and left pleura metastasis (Figures 1A and 2). Lung operative biopsy suggested metaplastic breast cancer. Immunohistochemistry showed ER(-), PR(-), CR(-), HER-2(0), ki-67(25–50%), CK20(-), Vimentin(++), S-100(+), GATA-3(+), TTF-1 (-), mamma(+), AE1/AE3 (-), Syn (-). Next-generation sequencing (NGS) of peripheral blood samples detected four driver mutations (KDM6A, DNMT3A, JAK3, TP53). Tumor mutation burden (TMB) was 12 Muts/Mb, which indicated possible sensitivity to immune checkpoint inhibitors (ICIs). After signing informed consent, the patient was administrated sintilimab (200mg) and gemcitabine (1000mg/m2, day 1 and day 8) plus carboplatin (AUC = 5) as first-line therapy. Unfortunately, the patient developed disease progression with newly pleural effusion in February 2020 after two cycles of treatment (Figure 1B). Then, the regimen was changed to sintilimab (200mg, Q3W), and paclitaxel-albumin (260mg/m2, Q3W) plus doxorubicin hydrochloride liposome (20mg/m2, Q3W), started from March 2020 (Figure 3). Soon, the left pleural effusion was effectively controlled and PR (Figures 1C and 3) was obtained within six-cycles therapy (Figures 1D and 3). The patient received sintilimab and paclitaxel-albumin as maintenance therapy and showed progression in March 2022 (Figures 1E and 3). Then, the regimen was changed to sintilimab (200mg, Q3W), and anrotinib (8mg, QD) plus Pirarubicin Hydrochloride (30mg/m2, Q3W), started from March 2022. The tumor was controlled and SD was obtained with six cycles therapy (Figure 3). The patient received sintilimab and anlotinib as maintenance therapy and showed progression in January 2023 (Figure 3). Unfortunately, the patient died on June 2023 (Figure 3). The serum tumor marker level is remained normal throughout the palliative treatment period. Treatment-related adverse events were rash and neutropenia which were grade II according to CTCAE 5.0.
 |
Figure 2 Positron emission tomography (PET)-CT revealed lung and left pleura metastasis. |
 |
Figure 3 The timeline from diagnosis of metaplastic breast cancer to different stages of therapeutic regime and evaluation. |
The investigators have obtained informed consent for participation, publish information and images from the patient described in this case report.
Discussion
MBC is a rare malignant tumor in clinical practice, and the treatment usually follows the NCCN or CSCO guidelines for invasive breast cancer, but the curative effect is not satisfied.19 Most patients cannot benefit from anti-human epidermal growth factor receptor-2 (HER2) treatment, because MBC is mostly triple negative.20 However, the molecular heterogeneity of MBC is strong, and its molecular expression is unique.18,21,22 Positive expressions of phosphatidylinositol 3-kinase (PI3K), mammalian target of rapamycin (mTOR), TP53, and epidermal growth factor receptor (EGFR) in certain cases can be observed.21 Patients with variations in the PI3K/AKT/mTOR pathway can receive targeted treatment with everolimus.23 In addition, in addition to being more sensitive to platinum drugs, MBC patients with breast cancer susceptibility protein 1 (BRCA1/BRAC2) gene mutations can also receive PARP inhibitors.24 Previous studies showed that the proportion of programmed death ligand 1 (PD-L1) expression in MBC is relatively high, providing a theoretical basis for the use of immune checkpoint inhibitors (ICIs).25
Herein, we report the treatment of an adult patient who suffered from relapse MBC with a moderate burden of TMB (12Muts/Mb) and microsatellite stability (MSS). After the failure of chemotherapy, the patient received sintilimab, an immune checkpoint inhibitor, plus chemotherapy and achieved partial relief (PR) according to RECIST1.1 in the subsequent 24 months with a manageable toxicity. Over the past decade, immunotherapy, especially immune checkpoint inhibitors targeting cytotoxic T-lymphocyte-associated protein 4 (CTLA-4), programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1), has shown significant survival benefits in various cancers. However, this success has little been reported in metaplastic breast cancers because of its rarity.
As an emerging biomarker, the predictive value of TMB has been confirmed in various cancers. Moderate and high TMB generally imply less genomic stability, which usually considered to further enhance immunogenicity and promote neoantigen production. Samstein et al analyzed the association between somatic TMB and response to immune checkpoint inhibitors in various cancer types. The results showed that the moderate TMB was associated with better objective response and prolonged survival in patients receiving ICIs.26 Currently, based on the results of 10 refractory solid tumor cohorts, pembrolizumab has been approved by the FDA in June 2020 for the treatment of solid tumors with high tissue TMB (tTMB), which was defined as ≥10 Mut/Mb. However, when tissue sample was inadequate for the advanced patients, cell-free DNA (cfDNA) provides an alternative sample for TMB assessment. Blood TMB from plasma cfDNA has been proved as a potential predictor of clinical benefit in NSCLC patients treated with PD-1 or PD-L1 inhibitors.27 Besides, Shi et al demonstrated the feasibility of ctDNA for predicting and monitoring the response to sintilimab in relapsed or refractory classical Hodgkin lymphoma.28
Conclusion
This case reports a patient with advanced MBC with long-term clinical benefits obtained after combined use of immunotherapy and chemotherapy. It would be a good addition to clinical practice providing new strategies and directions for the diagnosis and treatment of this rare disease. TMB may serve as a potential predictor associated with PD-1 inhibitors in MBC and help clinicians make an optimum treatment strategy. However, in future clinical work, we still need to confirm the efficacy and safety of immune checkpoint inhibitors on MBC through prospective clinical trials to improve the survival outcomes of such patients.
Data Sharing Statement
The raw data may be found in the Fourth Hospital of Hebei Medical University.
Ethics Approval and Consent to Participate
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Patient Consent for Publication
Patient has consented images for publication.
Acknowledgments
The authors thank the patient and students who participated in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for this study.
Disclosure
The authors report no competing interests in this work.
References
1. Rosai J. Special techniques in surgical pathology. In: John RG, Jesse KM, Laura WL, Jeffrey LM, editors. Rosai and Ackerman’s Surgical Pathology.
2. Lebeau A, Denkert C. Updated WHO classification of tumors of the breast: the most important changes. Pathologe. 2021;42(3):270–280. doi:10.1007/s00292-021-00934-9
3. Halpert B, Young MO. Carcinosarcoma of the mammary gland. Surgery. 1948;23:289–292.
4. Reis-Filho JSLS, Gobbi H, Sneige N. Metaplastic carcinoma. In: Lakhani S, Ellis I, Schnitt S, editors. World Health Organization Classification of Tumours of the Breast.
5. Wargotz ES, Norris HJ. Metaplastic carcinomas of the breast. III. Carcinosarcoma. Cancer. 1989;64:1490–1499. doi:10.1002/1097-0142(19891001)64:7<1490::AID-CNCR2820640722>3.0.CO;2-L
6. Tse GM, Tan PH, Putti TC, et al. Metaplastic carcinoma of the breast: a clinicopathological review. J Clin Pathol. 2006;59:1079–1083. doi:10.1136/jcp.2005.030536
7. Hennessy BT, Giordano S, Broglio K, et al. Biphasic metaplastic sarcomatoid carcinoma of the breast. Ann Oncol. 2006;17:605–613. doi:10.1093/annonc/mdl006
8. Tseng WH, Martinez SR. Metaplastic breast cancer: to radiate or not to radiate. Ann Surg Oncol. 2011;18:94–103. doi:10.1245/s10434-010-1198-6
9. Yang YF, Liu J, Fang ZY, et al. Clinical features and prognosis of 25 cases of breast carcinosarcoma. Zhonghua Zhong Liu Za Zhi. 2012;34(34):620–623. doi:10.3760/cma.j.issn.0253-3766.2012.08.014
10. Yakan S, Sarı E, Erkan N, et al. Breast carcinosarcomas. J Breast Health. 2014;10(3):161–165. doi:10.5152/tjbh.2014.2197
11. Kennedy WR, Gabani P, Acharya S, et al. Clinical outcomes and patterns of care in the treatment of carcinosarcoma of the breast. Cancer Med. 2019;8(4):1379–1388. doi:10.1002/cam4.1942
12. Ilhan E, Vardar E, Ozkok G, et al. A rare tumour of the breast: carcinosarcoma. J Clin Med Res. 2010;2:96–98. doi:10.4021/jocmr2010.03.275w
13. Tian W, Xu D. Diagnosis and management of multiple carcinosarcoma of the breast in a young Chinese patient. Breast Care. 2012;7(2):147–149. doi:10.1159/000337772
14. Kang Y, Kang S, Li Q, et al. Mixed epithelial and mesenchymal metaplastic carcinoma (carcinosarcoma) of the breast: a case report. Eur J Med Res. 2014;19(1):14. doi:10.1186/2047-783X-19-14
15. Mele M, Jensen LL, Vahl P, et al. Breast carcinosarcoma: clinical and pathological features. Breast Dis. 2015;35(3):211–215. doi:10.3233/BD-150402
16. Ghilli M, Mariniello DM, Fanelli G, et al. Carcinosarcoma of the breast: an aggressive subtype of metaplastic cancer. Report of a rare case in a Young BRCA-1 mutated woman. Clin Breast Canc. 2017;2017:17.
17. Muslim S, Prasad G, Alam I, et al. Carcinosarcoma of breast mimicking breast abscess. Indian J Surg Oncol. 2018;9:398–401. doi:10.1007/s13193-018-0777-z
18. Thomas HR, Hu B, Boyraz B, et al. Metaplastic breast cancer: a review. Crit Rev Oncol Hematol. 2023;182:103924. doi:10.1016/j.critrevonc.2023.103924
19. Gradishar WJ, Anderson BO, Balassanian R, et al. Breast cancer, version 4.2017, clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(3):310–320. doi:10.6004/jnccn.2018.0012
20. Schroeder MC, Rastogi P, Geyer CE, et al. Early and locally advanced metaplastic breast cancer: presentation and survival by receptor status in surveillance, epidemiology, and end results (SEER) 2010–2014. Oncologist. 2018;23(4):481–488. doi:10.1634/theoncologist.2017-0398
21. González-Martínez S, Pérez-Mies B, Carretero-Barrio I, et al. Molecular features of metaplastic breast carcinoma: an infrequent subtype of triple negative breast carcinoma. Cancers. 2020;12(7):1832. doi:10.3390/cancers12071832
22. Thomas A, Douglas E, Reis-Filho JS, et al. Metaplastic breast cancer: current understanding and future directions. Clin Breast Cancer;2023;2023:8209. doi:10.1016/j.clbc.2023.04.004
23. Basho RK, Yam C, Gilcrease M, et al. Comparative effectiveness of an mTOR-based systemic therapy regimen in advanced, metaplastic and non metaplastic triple-negative breast cancer. Oncologist. 2018;23(11):1300–1309. doi:10.1634/theoncologist.2017-0498
24. Tung NM, Robson ME, Ventz S, et al. TBCRC 048: Phase II study of olaparib for metastatic breast cancer and mutations in homologous recombination-related genes. J Clin Oncol. 2020;38(36):4274–4282. doi:10.1200/JCO.20.02151
25. Tray N, Taff J, Singh B, et al. Metaplastic breast cancers: genomic profiling, mutational burden and tumor-infiltrating lymphocytes. Breast. 2019;44:29–32. doi:10.1016/j.breast.2018.12.010
26. Samstein RM, Lee CH, Shoushtari AN, et al. Tumor mutational load predicts survival after immunotherapy across multiple cancer types. Nat Genet. 2019;51(2):202–206. doi:10.1038/s41588-018-0312-8
27. Wang Z, Duan J, Cai S, et al. Assessment of blood tumor mutational burden as a potential biomarker for immunotherapy in patients with non-small cell lung cancer with use of a next-generation sequencing cancer gene panel. JAMA Oncol. 2019;5(5):696–702. doi:10.1001/jamaoncol.2018.7098
28. Shi Y, Su H, Song Y, et al. Circulating tumor DNA predicts response in Chinese patients with relapsed or refractory classical Hodgkin lymphoma treated with sintilimab. EBioMedicine. 2020;54:102731. doi:10.1016/j.ebiom.2020.102731
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.