Back to Journals » Drug Design, Development and Therapy » Volume 18
Immunosuppression with Generics in Liver and Kidney Transplantation: A Real-World Evidence Study
Authors Finocchietti M, Marino ML, Rosa AC, Bellini A , Masiero L , Cardillo M, Massari M , Spila Alegiani S , Pierobon S , Ferroni E , Zanforlini M, Leoni O, Ledda S, Garau D, Davoli M, Addis A , Belleudi V
Received 7 September 2023
Accepted for publication 22 December 2023
Published 12 January 2024 Volume 2024:18 Pages 53—69
DOI https://doi.org/10.2147/DDDT.S431121
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Anastasios Lymperopoulos
Marco Finocchietti,1,* Maria Lucia Marino,1,* Alessandro C Rosa,1 Arianna Bellini,1 Lucia Masiero,2 Massimo Cardillo,2 Marco Massari,3 Stefania Spila Alegiani,3 Silvia Pierobon,4 Eliana Ferroni,4 Martina Zanforlini,5 Olivia Leoni,6 Stefano Ledda,7 Donatella Garau,7 Marina Davoli,1 Antonio Addis,1 Valeria Belleudi1 On behalf of CESIT Study Group
1Department of Epidemiology, Lazio Regional Health Service-ASL Roma 1, Rome, Italy; 2Italian National Transplant Center, Istituto Superiore di Sanità, Rome, Italy; 3National Center for Drug Research and Evaluation, Istituto Superiore Di Sanità, Rome, Italy; 4Azienda Zero, Veneto Region, Padua, Italy; 5The innovation and procurement regional company, A.R.I.A. S.p.A.-Lombardy Region, Milan, Italy; 6Regional Epidemiological Observatory, Lombardy Region, Milan, Italy; 7General Directorate for Health, Sardinia Region, Cagliari, Italy
*These authors contributed equally to this work
Correspondence: Valeria Belleudi, Department of Epidemiology, ASL Roma 1, Lazio Region, Via Cristoforo Colombo, 112, Roma, 00147, Italy, Tel +39.06.99722133, Fax +39.06.99722111, Email [email protected]
Purpose: This study evaluates the use, benefit-risk profile, and economic impact of generic immunosuppressants (tacrolimus-TAC, cyclosporine-CsA, and mycophenolate-MYC) in kidney and liver transplant recipients compared to brand-name drugs.
Patients and Methods: A retrospective multicentre observational study, involving four Italian regions, was conducted based on the national transplant Information system and regional healthcare claims data. The analysis focused on incident patients who received kidney and liver transplants between 2013 and 2019 and evaluated the use of generic of CsA, TAC, and MYC during the 30-day period following discharge. For each type of transplant and immunosuppressive agent, the benefit-risk profile of generic vs branded drugs in a two-year window was estimated by multivariate Cox models (HR; 95% CI). Furthermore, the potential cost savings per person associated with one year of treatment using generics were calculated.
Results: The utilization of generic drugs showed a significant increase; over the study years, the proportion of users among kidney recipients ranged from 14.2% to 40.5% for TAC, from 36.9% to 56.7% for MYC, and from 18.2% to 94.7% for CsA. A great variability in generic uptake for region was found. A comparable risk-benefit profile between generic and branded formulations was shown for all immunosuppressors considered. Choosing generic immunosuppressants during maintenance could result in yearly savings of around 2000 euros per person for each therapy ingredient.
Conclusion: The study shows an increasing proportion of patients using generic immunosuppressive drugs over time suggesting a growing acceptance of generics within the transplant community and reveals comparable risk-benefit profiles between the generic and branded formulations of TAC, CsA, and MYC. A significant variability in the use of generics immunosuppressive agents was found both at the regional level and among transplant centers and future research should delve into regional prescribing variations.
Keywords: transplant, maintenance therapy, tacrolimus, cyclosporine, mycophenolate, uptake generics, risk-benefit profile, sustainability
Introduction
Patients who have undergone organ transplantation require lifelong immunosuppressive therapy. As known, there is high variability in the managing of immunosuppressive regimens, even among different clinical centres.1 The complexity of treatment is further complicated by the use of multiple drugs, prescribed to prevent rejection, which often consists of around 10 different compounds.2 Additionally, the availability of generic drugs as substitutes for branded immunosuppressives has sparked discussions in the scientific community and regulatory authorities at national and international level regarding their safety and efficacy when switching or substituting between generic and branded drugs in transplant patients.3–5 This is particularly important for immunosuppressive drugs such as cyclosporine (CsA) and tacrolimus (TAC), which are considered narrow therapeutic index drugs (NTIDs). Generic substitution for NTIDs, as well as for other drugs in this category, requires caution due to the potential clinical consequences resulting from slight variations in dosage that may lead to under- or over-exposure to the drugs.3 However, since the cost of drugs accounts for 15–25% of the total cost in the first year of kidney transplantation, and considering that transplanted patients require lifelong immunosuppressive therapy, switching from branded drugs to generic formulations can significantly reduce treatment costs.3 Since the availability of generic formulations for CsA, TAC and mycophenolate mofetil (MYC), the controversy surrounding the use of generics in transplanted patients has stimulated clinical research to provide evidence on the interchangeability between generic and branded formulations. An important meta-analysis was conducted on CsA, TAC, and MYC, comparing branded formulations versus generics in different solid organ transplantations.6 The results indicated that data demonstrating the bioequivalence of generic immunosuppressants are limited. Although generic formulations do not fully meet the bioequivalence criteria established by the US and European regulatory agencies, they showed no significant differences in acute rejection compared to originator drugs.6
The concept of bioequivalence is crucial for generic medication approval. Two drugs with the same active substance are considered bioequivalent if their bioavailability, in terms of rate and extent, after administration in the same molar dose falls within predefined limits. This ensures comparable in vivo performance, indicating similarity in safety and efficacy.3 Key pharmacokinetic parameters, such as AUC (area under the concentration-time curve) and Cmax (maximum plasma concentration), determine bioequivalence. The 90% confidence interval for the ratio of the test and reference products should be contained within the acceptance interval of 80–125%. Specifically, the entire 90% confidence interval of these key parameters must lie within 80% and 125% of the value for perfect bioequivalence.
However, the European Medicines Agency (EMA) modified the bioequivalence standards for narrow therapeutic index (NTI) drugs and required more stringent criteria for generic approval suggesting that the concentration for AUC needs to fall between 90 and 111%.3,7 Further, bioequivalence tests in healthy volunteers may not accurately reflect conditions in transplant recipients, especially with multiple doses over an extended period.8
Recent systematic reviews and retrospective studies comparing originator and equivalent formulations of TAC have shown no differences in terms of the incidence of acute rejection, graft failure and adverse events.9,10 A 2020 meta-analysis9 found no difference in biopsy-proven acute rejection (BPAR) between generic and branded TAC immunosuppression but regarding bioequivalence, the authors reported that studies on de novo use did not fulfill EMA requirements. In contrast, Gantar and colleagues reported bioequivalence studies comparing a generic formulation of once-daily tacrolimus 5 mg prolonged-release with the reference product. The results revealed strikingly similar concentration–time profiles, and the bioequivalence studies, conducted under both single-dose fasting and single-dose fed conditions, met the criteria set by the EMA and Health Canada. Additionally, under multiple-dose fasting conditions for once-daily tacrolimus, the EMA criteria were also satisfied.11 In 2015, Robertsen et al focused their research on the use of generic tacrolimus in the elderly. The prospective, single-center, randomized, crossover trial evaluated the pharmacokinetic parameters of generic tacrolimus in renal transplant recipients over 60 years of age. The results indicated that both the area under the curve (AUC) and maximum concentration of generic TAC were higher and did not meet bioequivalence standards. This suggests that caution is necessary when using generic formulations of TAC in the elderly population due to the higher drug exposure potentially increasing the risk of adverse events.12
In Italy, the Italian Medicine Agency (AIFA) and the Italian Society of Organ Transplantation (SITO) have released guidelines regarding the appropriate substitution of branded immunosuppressors with generics.4,5,13 These guidelines recommend: avoiding generic drugs that do not meet the guidelines set by the European Medicines Agency (EMA); conducting any switch between the original and generic formulations under close clinical monitoring, managed by medical specialists experienced in immunosuppressive therapy; avoiding frequent changes in generic formulations, as well as the simultaneous use of multiple generics of the same drug in the same patient; using generic drugs in “de novo” patients rather than patients already on treatment, with the option for the prescriber to continue with the original drug if deemed appropriate; ensuring that patients are properly informed about the reasons for using the generic equivalent, the associated risks and benefits, and instructing them to identify the specific product they are using and to inform the specialist physician in case of a change in formulation. The European Society for Organ Transplantation (ESOT) expresses similar recommendations.3 Therefore, the analysis conducted by Rottembourg and colleagues in 2019 on the clinical aspects (efficacy, safety, and bioequivalence) of generic immunosuppressive drugs in comparison to their branded counterparts among solid organ transplant recipients. The study also considered the position statements of various scientific societies on the use of generic immunosuppressive drugs, affirming a consistent recommendation for generic immunosuppression. However, a universal consensus regarding the acceptance criteria for the bioequivalence of generic drugs is lacking.7
Recently, AIFA has funded an observational multicenter study based on healthcare claim data to compare the risk-benefit profile of different immunosuppressive therapeutic regimens, including generics and originators, in the post-transplant maintenance phase (the CESIT project).14
This study, a component of the broader project, focuses on evaluating the use of generic immunosuppressants in patients undergoing kidney and liver transplantation. Specifically, the objectives of this study were threefold: 1) to describe the utilization of generic immunosuppressants in transplant patients, including switching between version; 2) to analyze the effectiveness and safety of generic versus brand-name drugs for TAC, CsA and MYC; and 3) to provide an economic evaluation of treatment with brand-name and generic formulations.
Materials and Methods
This study is a retrospective multicenter observational cohort investigation conducted across four regions in Italy (Lombardy, Veneto, Lazio, Sardinia) and includes a total population of over 20 million individuals. The included regions account for approximately 45% of transplants nationwide.
The study utilizes data obtained from regional healthcare claims and the national transplant information system.
The Italian National Health Service (NHS) is a system composed of structures and services aimed at ensuring universal access to healthcare for all citizens on an equal basis. It provides coverage for a wide range of essential pharmaceuticals and diagnostic services, either fully or partially through a system of cost-sharing for patients known as “ticket.” The NHS promotes efficient and effective management through local health authorities to ensure consistent delivery of services throughout the country. In Italy, healthcare administrative data have a high level of coverage due to national laws mandating data collection on a regional level to track healthcare service utilization and monitor the uniformity of service delivery across the country.
Specifically, for this study, analytical datasets were established for each region, focusing on incident patients who underwent kidney and liver transplantation between 2013 and 2019. These datasets were created according to a common data model that incorporated data from the hospital information system, pharmaceutical dispensation records, mortality information system, and co-payment exemption registry. Most of these data sources have been extensively utilized to study various facets of healthcare, such as drug utilization, safety, comparative effectiveness, cost, and cost-effectiveness, demonstrating both a high level of coverage and good quality.15
To facilitate the analysis, a distributed analysis tool called “TheShinISS” was utilized.16 This tool allows elaborating and processing health archives at local level, performing data quality control, matching/sampling, record-linkage, and finally creating the anonymized dataset for the centralized data analyses.17,18
To link nationwide data on demographic and clinical characteristics of both donors and recipients (such as human leukocyte antigen type, blood group, body mass index, clinical indications to transplant, incidence of rejection) a semi-deterministic matching approach was utilized.
In particular, we implemented a step-by-step deterministic record linkage procedure using pseudonymous variables, such as sex, organ type, year and month of birth, year and month of transplant, and the transplant hospital. Multiple keys, concatenating combinations of these variables, were created. At each step, subjects with duplicated keys were excluded before conducting the linkage procedure, which involves an exact match of the key. Further details regarding this matching procedure can be found elsewhere in the literature.14
For both kidney and liver transplantation, the study examined the use of CsA, TAC, and MYC in the 30-day period after discharge (index period). Patients were classified as either generic or originator users based on the type of drug (originator/generic) dispensed in the index period. If patients were using a combination of immunosuppressive drugs, they were counted more than once.
For each type of transplantation and active ingredient, patients who received generic formulations were compared to originator users. This comparison considered factors such as the patient’s region of residence, characteristics of the donor and recipient, transplant information, length of hospital stay for transplantation, year of discharge, clinical history including other medical conditions and concomitant medications.
The proportion of patients receiving generic formulations was calculated overall and by year, separately for each type of transplantation and each immunosuppressive agent. Additionally, a detailed analysis was conducted at the regional level and within the hospital center.
Furthermore, for all patients who survived for one year, the proportion of those who switched from originator to generic and vice versa was calculated. The same analysis was replicated considering a two-years timeframe.
In order to estimate the risk-benefit profile of generics, we restricted our cohorts to December 31st, 2017. Each patient was followed up from 30 days after hospital discharge until the occurrence of the study event, death, a maximum of 2 years, or the end of the study, whichever came first. The outcomes considered were transplant rejection/graft failure and mortality for effectiveness analysis, and incidence of severe infections, diabetes, and statin use for safety analysis. For each outcome, only patients who were at risk of developing the outcome for the first time were considered.
The effectiveness and safety of generic versus originator drugs for each type of transplant and each immunosuppressive agent were estimated using multivariate Cox models (HR; 95% CI). The models were adjusted for variables found to be strongly related to exposure and outcomes (ie, recipient age and sex, indication for transplant and region). For each active ingredient, a sensitivity analysis was conducted to account for potential variations in immunosuppressive regimens among the comparison groups. In this analysis the immunosuppressive therapies used in combination with the exposure were included in the models as possible confounders.
Finally, to estimate the saving of one year of immunosuppressive therapy with generics compared to branded, we considered the national average price per DDD (defined daily dose) for each active ingredient estimated by AIFA19 and based on of this value we calculated the cost of one year of therapy and the associate saving.
All analyses were performed using SAS Statistical Software version 9.4 (SAS Institute Inc., Cary, NC) and R version 4.1.3.
Results
In the study period, several generics for CsA, TAC and MYC were available (Table 1).
 |
Table 1 Branded and Generic Version of Tacrolimus, Cyclosporine and Mycophenolate |
Between January 1st, 2013, and November 30th, 2019, a total of 3106 kidney and 1759 liver recipients who met the study eligibility criteria were identified (Figure 1). In the kidney recipient cohort, there were 2354 users of TAC, 627 users of CsA, and 2143 users of MYC. For liver recipients, the numbers were 1518 for TAC, 223 for CsA, and 662 for MYC. Among TAC users, the proportion of patients receiving generic medications was comparable between kidney and liver transplant recipients, with 35.0% in the kidney cohort and 34.6% in the liver cohort. Kidney recipients compared to liver recipients had higher use of generic CsA (47.8% vs 21.8%) and slightly lower use of generic MYC (45.9% vs 50.3%).
 |
Figure 1 Study eligibility criteria by kidney and liver transplantation. |
Time Trends in the Use of Generic Immunosuppressant
As shown in Figure 2, the proportion of patients using generic immunosuppressive medications increased over time. Specifically, for TAC, it reached its peak in 2017 with 47.5% for kidney and 56.6% for liver, slightly decreasing in the following two years. The peak usage of generic CsA was observed in 2018 for kidney recipients (95.1%) and in 2017 for liver recipients (92.9%). As for MYC, the highest proportion of generic users in both transplant cohorts was observed in 2019 (56.7% for kidney and 69.1% for liver).
 |
Figure 2 Generic and branded users of TAC, CsA and MYC by year in kidney and liver transplantation. |
Characteristics of Branded and Generic Users
When comparing transplant characteristics between branded and generic users, a higher proportion of patients treated with generic drugs was observed in Lombardy for both cohorts and all immunosuppressive agents considered (Table 2). Generic TAC therapy was more frequent prescribed to younger kidney recipients (43.1% in patients aged<50 years), Additionally, a higher proportion of CsA generic use was observed for patients with hepatocellular carcinoma (HCC).
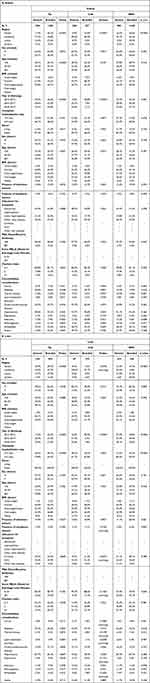 |
Table 2 Transplant, Recipient and Donor Characteristics According to Generic/Branded Version by Active Ingredient in Kidney and Liver Transplantation |
The greater utilization of generics by transplant patients in Lombardy was also evident when examining the proportion of use at regional level by year (Table 3). Furthermore, a high variability was found in the proportion of generic immunosuppressive drugs dispensed to patients by transplant hospital for both cohorts (Figure 3A–C).
 |
Table 3 Proportion of Patients Treated with Generic Version for TAC, CsA and MYC Over Time by Region in Kidney and Liver Transplantation |
 |
Figure 3 (A-C) Hospital variability in patients treated with generic drugs by active ingredient in kidney and liver transplantation. |
Switching from a Generic to Branded and Vice Versa
Figure 4 displays the proportion of patients changing drug versions during the first year of treatment. In both cohorts and for all active agents considered, a higher proportion of patients switched from generic to branded drugs compared to vice versa. The difference between these two percentages (% switching from generic to branded and % switching from branded to generic) was particularly evident for TAC users in both cohorts (Δ=34.7–6.5 =28.2% for kidney and Δ=43.7–11.4=32.3% for liver). A part of this switch is explained by the change in formulation from immediate (IM) to prolonged release (PR) (53.8% for kidney and 55.1% for liver), no generic is available for the latter formulation indeed. However, also for CsA we observed a higher proportion of switch from generic to branded respect vice versa, in particular in the liver recipients (32.6% vs 2.3%). The difference between these two types of switches was relatively smaller in the remaining comparisons, ranging from 5% in MYC users in the liver cohort to 7.8% in MYC users in the kidney cohort. This tendency to switch more frequently from generics to branded immunosuppressor than vice versa remained consistent when we considered sensitivity analysis over a 2-year time frame (Figure 5), except for MYC users in the liver cohort, where the switching rates were similar: 23.1% from generic to branded and 21.7% from branded to generic.
 |
Figure 4 Proportion of patients changing drug version within one year from starting therapy by active ingredient in kidney and liver transplantation. |
 |
Figure 5 Proportion of patients changing drug version within two years from starting therapy by active in kidney and liver transplantation. |
Effectiveness and Safety of Generic versus Branded Drugs
No statistically significant difference in the risk of lack of effectiveness and safety between generics and originators was found for TAC, CsA and MYC in kidney transplant patients (Figure 6), specifically the adjusted HR for mortality was equal to 1.53 (95% CI 0.86–2.70), 1.24 (95% CI 0.50–3.03) and 1.15 (95% CI 0.66–2.00), respectively. In the liver transplantation, the lower numerosity in terms of patients and outcomes reduced the statistical power of the study; in particular, it was not possible to compare generic versus branded in CSA users (the number of CsA generic users was 47) and to estimate the risk of rejection between generic and branded in MYC users (9 individuals had the outcome). For all other comparisons, no statistically significant difference was found, although a protective role of generics in TAC seems to emerge in term of mortality (0.55 95% CI 0.29–1.04) and rejection (0.70 95% CI 0.30–1.62), and a potential mortality risk seems related to generic MYC (1.88 95% CI 0.91–3.92).
 |
Figure 6 Risk-benefit profile of generic versus branded by active ingredient in kidney and liver transplantation. |
Similar results were obtained when including immunosuppressive therapies used in combination with the exposure in the adjustment models (Table 4). The table in the supplementary materials shows the therapeutic combinations prescribed in the 30 days post-transplant (index therapy) in the cohort of kidney and liver recipients (Table S1).
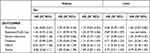 |
Table 4 Sensitivity Analysis Adjusting for Immunosuppressive Therapies Used in Combination with the Exposure |
Economic Evaluation
Taking into consideration the national average price per DDD as shown in Figure 7, we calculated the following savings associated with one year of treatment: €1995 for TAC, €1858 for CsA, and €2358 for MYC. These savings can exceed €4000 in the case of dual therapy involving calcineurin inhibitors and MYC.
 |
Figure 7 Saving of one year of immunosuppressive therapy with generics compared to branded. |
Discussion
The findings of this retrospective study provide valuable insights into the trends in the utilization of generic and branded immunosuppressive drugs among kidney and liver transplant recipients in Italy. The analysis revealed a significant shift towards the utilization of generic medications over the study period, suggesting a positive impact of national recommendations on the use of generics within a vulnerable population like transplant patients. The exploration of clinical outcomes or adverse events associated with the use of generic and branded immunosuppressants suggesting a similar risk-benefit profile for TAC, CsA and MYC. As already shown in USA20 generic products have the potential to reduce costs for the healthcare system; our findings showed that opting for generic immunosuppressant during the maintenance phase would lead to estimated economic savings amounting to approximately 2000 euro in one year for person, which then becomes 4000 in the case of dual therapy of generic immunosuppressants such as calcineurin inhibitors plus MYC. This is interesting considering that the report published in 2022 on the use of drugs in Italy21 showed immunosuppressants as one of the most expensive categories of medication together with oncological drugs. On the other hand, it should be taken into account that the cost savings derived by generic use may be associated with additional expenses related to increased monitoring or clinical visits,22 for these reasons it appears important also from an economic point of view to produce evidence on the efficacy and safety profile of generic medication that enables practitioners to use it safely.
One notable observation was the comparable proportion of patients receiving generic TAC in both kidney and liver cohorts, indicating a widespread acceptance and adoption of generic TAC. On the other hand, there were variations in the usage of generic CsA and MYC between the kidney and liver cohorts. The kidney cohort showed a higher proportion of generic CsA users, while the liver cohort exhibited slightly higher usage of generic MYC. However, the increasing proportion of patients using generic immunosuppressive drugs over time suggests a growing acceptance of generics within the transplant community.
A noteworthy finding is the regional variation in the utilization of generic immunosuppressants, particularly in Lombardy. The higher proportion of patients treated with generic drugs in Lombardy, across all immunosuppressive agents and both cohorts, suggests regional factors such as healthcare policies or local preferences, even at hospital level, influencing prescribing practices.
The analysis also identified demographic and clinical factors associated with the use of generic medications. Generic TAC therapy was more commonly prescribed to younger kidney recipients, potentially due to cost considerations and the desire to enhance long-term adherence. In contrast, generic CsA and MYC were predominantly observed in older liver recipients, possibly reflecting a more cautious approach in this patient population. Another possible explanation for these associations could be due to the central role of the hospital in defining the therapy. Indeed, the observed differences in transplant characteristics between generic and branded users could reflect the different case mix of patients per hospital and different immunosuppressive strategies in terms of active agents, version and formulations per hospital.
The observed patterns of switching between generic and branded drugs within the first year of treatment indicate a higher rate of switching from generic to branded medications compared to vice versa. This phenomenon was particularly pronounced in TAC users in both cohorts and can be partially explained with a switching of formulation from TAC IR to PR, it is plausible that the switch to once-daily administration of TAC may improve patient compliance; it may also reflect some practitioners’ hesitancy in using generic TAC given that TAC is a narrow therapeutic index medication, whereas MYC is not; this is confirmed by the relatively smaller difference in switching rates observed for MYC users.23,24 The narrow therapeutic index status may imply severe risk of adverse clinical consequences in case of subtherapeutic or toxic drug concentrations25,26 and require particular attention until therapeutic equivalency is confirmed in clinical practice. The switch from generic to branded drugs can be also related to other factors, such as: - minor and unreported adverse reaction; - A dubious attitude from both patients and physicians regarding generic drugs, or - switch due to a different choice in the purchase of the drug by the health facility as a result of competitive bidding, or due to problems of shortages and unavailability.
The analysis of generic versus branded immunosuppressants’ efficacy and safety profiles aligns with previous studies, affirming a consistent risk-benefit equivalence between generic and branded formulations among users of CsA27–31 and TAC.7,32–35 These results suggest that clinicians may consider generic formulations as viable alternatives to their branded counterparts without compromising patient outcomes. Further, for liver transplantation a potential protective role of TAC generics compared branded was detected for mortality and rejection, even if the risks were not statistical significantly, this finding is in line with the review of Kahn and colleagues9 that suggests lower biopsy‐proven acute rejection risk with generic TAC for de novo use in liver setting. However, as suggested by authors some risk of bias could affect the estimate. The potential difference between generic and branded shown for MYC users in liver recipients was not statistical significantly and do not find consensus in literature.36 It is probable that the low numerosity of events as well as the presence of residual confounding may have played a role in the estimate validity. Further, the narrow therapeutic index of TAC and the aforementioned reluctance among physicians may introduce a bias favoring the prescription of generic TAC in individuals perceived as having a lower risk of experiencing side effects or deemed more likely to tolerate variations in drug response.
Strengths and Limitations
The primary strength of this study lies in the accessibility of data regarding four regions, which collectively represent Northern, Central, and Southern Italy. Additionally, the study benefits from a robust sample size achieved across the diverse groups, enhancing the statistical power and reliability of the findings.
However, it is important to consider some limitations of this study. Firstly, being a retrospective analysis, it is subject to inherent biases and limitations associated with such designs. However, real-world data provided by observational studies have been extensively utilized to study various aspects of healthcare, including drug utilization, safety, comparative effectiveness, cost, and cost-effectiveness. Despite the inherent limitations of observational studies not being randomized controlled trials, they still offer valuable insights and evidence from real-world scenarios.
Secondly, even though the safety-effectiveness analysis revealed no significant differences between branded and generic drugs, the use of administrative data leaves room for the existence of unobserved clinical factors; our data only allow us to observe severe therapy-related effects that have required the use of healthcare services, yet there may be additional side-effects that do not manifest in hospitalization/medication use or emergency-room visits, thus eluding our observation.
Finally, the study focused on a specific context and timeframe, and the generalizability of the findings to other country as well as other time periods should be examined. However, our analysis includes four major Italian regions, which collectively account for more than 45% of transplantation activities. These regions provide a significant representation of the transplantation landscape in Italy. As previously mentioned, our study marks an initial endeavor to examine the utilization of generic drugs in Italy, revealing a pronounced interregional variability. These findings can represent an opportunity to engage policymakers and prescribers in a dialogue regarding this variability, serving as a starting point for exploring its underlying motivations.
Conclusion
This study sheds light on the trends in the utilization of generic and branded immunosuppressive drugs in kidney and liver transplant recipients in Italy and demonstrates that the two options of TAC, CsA and MYC exhibit comparable risk-benefit profiles. The increasing use of generic medications over time highlights the importance of cost-effectiveness and accessibility in transplantation care; also, our findings provide clinicians with valuable insights to guide evidence-based decision-making in immunosuppressive therapy. While the economic advantages of generic immunosuppressants are evident, clinicians should balance this with a commitment to optimizing the overall well-being and long-term outcomes of transplant recipients. In this context, the results on the comparison between branded and generic drugs in real-world setting can empower healthcare providers to make informed decisions when tailoring immunosuppressive therapy to individual patients.
Future research should explore factors driving regional disparities in prescribing practices and examine in depth the specific patient subpopulations that may benefit more from one therapeutic option over the other for contributing to the evolution of guidelines that promote a comprehensive and patient-centered approach in transplant medicine.
Ethical Approval
This retrospective study protocol was notified, prior to commencement of your study, to the Ethical Committee of the Local Health Authority “ASL Roma 1”, the reference ethical committee for the project’s coordinating center (Department of Epidemiology of Lazio), according to the current national law. All organs were donated voluntarily with the written informed consent, these donations were conducted in accordance with the Declaration of Istanbul. All study procedures complied with the ethical standards (EU GDPR).
Acknowledgments
This study was conducted in the context of the multiregional active pharmacovigilance CESIT project, funded by the Italian Medicines Agency.
VB conceived the project. CESIT study group contributed to data acquisition. MF and ACR participated in analysis and prepared figures. VB, MF and MLM wrote the manuscript with input from all authors. All authors have made a substantial, direct and intellectual contribution to the work, and approved the final manuscript.
Funding
This study was funded by the Italian Medicines Agency in the context of the multiregional pharmacovigilance project (AIFA 2012–2014: Comparative Effectiveness and Safety of Immunosuppressive Drugs in Transplant patients—CESIT project). Grant code: J85I2000009005 (CUP). The authors of this manuscript have no conflicts of interest to disclose, MZ was employed by ARIA, S.p.A.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Marino ML, Rosa AC, Finocchietti M, et al. Temporal and spatial variability of immunosuppressive therapies in transplant patients: an observational study in Italy. Front Transplant. 2023;1:1060621. doi:10.3389/frtra.2022.1060621
2. Tönshoff B. Immunosuppressive therapy post-transplantation in children: what the clinician needs to know. Expert Rev Clin Immunol. 2020;16(2):139–154. doi:10.1080/1744666X.2020.1714437
3. Van Gelder T. ESOT Advisory Committee on Generic Substitution. European Society for Organ Transplantation Advisory Committee recommendations on generic substitution of immunosuppressive drugs. Transpl Int. 2011;24(12):1135–1141. doi:10.1111/j.1432-2277.2011.01378.x
4. AIFA. Determinazione AIFA; 2016. Available from: http://www.agenziafarmaco.gov.it/sites/default/files/Determinazione_AIFA_n._5-2016.pdf.
5. AIFA. Precisazioni AIFA su Tacrolimus; 2011. Available from: http://www.agenziafarmaco.gov.it/sites/default/files/precisazioni_aifa_su_tacrolimu.pdf.
6. Molnar AO, Fergusson D, Tsampalieros AK, et al. Generic immunosuppression in solid organ transplantation: systematic review and meta-analysis. BMJ. 2015;350:h3163.
7. Rottembourg J. Generic Immunosuppression in Transplantation: a Controversial Analysis. J Med Toxicol Clin Forensic Med. 2019;5(1):1.
8. Cattaneo D, Perico N, Remuzzi G, et al. Generic cyclosporine formulations: more open questions than answers. Transpl Int. 2005;18(4):371–378. doi:10.1111/j.1432-2277.2005.00078.x
9. Kahn J, Pregartner G, Schemmer P. Immunosuppression with generic tacrolimus in liver and kidney transplantation-systematic review and meta-analysis on biopsy-proven acute rejection and bioequivalence. Transpl Int. 2020;33(4):356–372. doi:10.1111/tri.13581
10. Son SY, Jang HR, Lee JE, et al. Comparison of the long-term efficacy and safety of generic Tacrobell with original tacrolimus (Prograf) in kidney transplant recipients. Drug Des Devel Ther. 2017;11:203–210. doi:10.2147/DDDT.S118154
11. Gantar K, Škerget K, Mochkin I, Bajc A. Meeting Regulatory Requirements for Drugs with a Narrow Therapeutic Index: bioequivalence Studies of Generic Once-Daily Tacrolimus. Drug Healthc Patient Saf. 2020;12:151–160. doi:10.2147/DHPS.S256455
12. Robertsen I, Åsberg A, Ingerø AO, et al. Use of generic tacrolimus in elderly renal transplant recipients: precaution is needed. Transplantation. 2015;99(3):528–532. doi:10.1097/TP.0000000000000384
13. SITO. Considerazioni sull’uso degli immunosoppressori equivalenti dopo trapianto d’organo solido; 2022. Available from: https://www.societaitalianatrapiantidiorgano.com/wpcontent/uploads/2015/04/ConsiderazioniSITO_farmaci_immunosoppressori_equivalenti.pdf.
14. Belleudi V, Rosa AC, Finocchietti M, et al. An Italian multicentre distributed data research network to study the use, effectiveness, and safety of immunosuppressive drugs in transplant patients: framework and perspectives of the CESIT project. Front Pharmacol. 2022;13:959267. doi:10.3389/fphar.2022.959267
15. Trifirò G, Gini R, Barone-Adesi F, et al. The role of European healthcare databases for post-marketing drug effectiveness, safety and value evaluation: where does Italy stand? Drug Saf. 2019;42(3):347–363. doi:10.1007/s40264-018-0732-5
16. Massari M, Spila Alegiani S, Da Cas R, et al. TheShinISS: un applicativo open-source per la conduzione di analisi distribuite in studi di farmacoepidemiologia di tipo multi-database. Boll Epidemiol Naz. 2020;1(2):39–45.
17. Trifirò G, Isgrò V, Ingrasciotta Y, et al. Large-Scale Postmarketing Surveillance of Biological Drugs for Immune-Mediated Inflammatory Diseases Through an Italian Distributed Multi-Database Healthcare Network: the VALORE Project. BioDrugs. 2021;35(6):749–764. doi:10.1007/s40259-021-00498-3
18. Spila Alegiani S, Morciano C, Menniti-Ippolito F, et al. Postmarketing observational study on the safety of 2021/2022 and 2022/2023 influenza vaccination campaigns in Italy: theShinISS-Vax|Flu study protocol. BMJ Open. 2023;13(8):e069858. doi:10.1136/bmjopen-2022-069858
19. Italian Medicines Agency - AIFA. Monitoring of patent-expired non-biologic medicines. Available from: https://www.aifa.gov.it/en/monitoraggio-farmaci-non-biologici-A-brevetto-scaduto.
20. Helmuth ME, Liu Q, Turenne MN, et al. Secular Trends in the Cost of Immunosuppressants after Solid Organ Transplantation in the United States. Clin J Am Soc Nephrol. 2019;14(3):421–430. doi:10.2215/CJN.10590918
21. The Medicines Utilisation Monitoring Centre. National Report on Medicines Use in Italy. Rome: Italian Medicines Agency; 2022.
22. Harrison JJ, Schiff JR, Coursol CJ, et al. Generic immunosuppression in solid organ transplantation: a Canadian perspective. Transplantation. 2012;93(7):657–665. doi:10.1097/TP.0b013e3182445e9d
23. El Hajj S, Kim M, Phillips K, Gabardi S. Generic immunosuppression in transplantation: current evidence and controversial issues. Expert Rev Clin Immunol. 2015;11(5):659–672. doi:10.1586/1744666X.2015.1026895
24. Liu Q, Smith AR, Park JM, et al. The adoption of generic immunosuppressant medications in kidney, liver, and heart transplantation among recipients in Colorado or nationally with Medicare part D. Am J Transplant. 2018;18(7):1764–1773. doi:10.1111/ajt.14722
25. Lee RA, Gabardi S. Current trends in immunosuppressive therapies for renal transplant recipients. Am J Health Syst Pharm. 2012;69(22):1961–1975. doi:10.2146/ajhp110624
26. Taube D, Jones G, O’Beirne J, et al. Generic tacrolimus in solid organ transplantation. Clin Transplant. 2014;28(5):623–632. doi:10.1111/ctr.12336
27. Kahn D, Muller E, Pascoe M. Safe conversion to cicloral, a generic cylosporine, in both stable and de novo renal transplant recipients. Saudi J Kidney Dis Transpl. 2010;21(3):426–432.
28. Diarra DA, Riegersperger M, Säemann MD, et al. Maintenance immunosuppressive therapy and generic cyclosporine A use in adult renal transplantation: a single center analysis. Kidney Int Suppl. 2010;115:S8–11. doi:10.1038/ki.2009.505
29. Tarek BO, Nadia BF, Anis K, et al. Assessment of bioequivalence of a generic cyclosporine (Equoral) by a prospective randomized controlled trial on allogeneic stem cell transplant recipients. Transplant Proc. 2010;42(9):3735–3738. doi:10.1016/j.transproceed.2010.06.019
30. Niemczyk M, Paczek L. Generic formulation of cyclosporine A, Equoral®, in de novo kidney transplant recipients: five-year follow-up. Ann Transplant. 2011;16(2):59–62. doi:10.12659/AOT.881866
31. Durlik M, Paczek L, Rutkowski B, et al. The efficacy and safety of ciclosporin (Equoral®) capsules after renal transplantation: a multicentre, open-label, Phase IV clinical trial. Ann Transplant. 2010;15(3):51–59.
32. Spence MM, Nguyen LM, Hui RL, Chan J. Evaluation of clinical and safety outcomes associated with conversion from brand-name to generic tacrolimus in transplant recipients enrolled in an integrated health care system. Pharmacotherapy. 2012;32(11):981–987. doi:10.1002/phar.1130
33. Ensor CR, Trofe-Clark J, Gabardi S, et al. Generic maintenance immunosuppression in solid organ transplant recipients. Pharmacotherapy. 2011;31(11):1111–1129. doi:10.1592/phco.31.11.1111
34. McDevitt-Potter LM, Sadaka B, Tichy EM, Rogers CC, Gabardi S. A multicenter experience with generic tacrolimus conversion. Transplantation. 2011;92(6):653–657. doi:10.1097/TP.0b013e31822a79ad
35. Momper JD, Ridenour TA, Schonder KS, et al. The impact of conversion from prograf to generic tacrolimus in liver and kidney transplant recipients with stable graft function. Am J Transplant. 2011;11(9):1861. doi:10.1111/j.1600-6143.2011.03615.x
36. Kim JM, Kwon CH, Yun IJ, et al. A multicenter experience with generic mycophenolate mofetil conversion in stable liver transplant recipients. Ann Surg Treat Res. 2014;86(4):192–198. doi:10.4174/astr.2014.86.4.192
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
