Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
Imidafenacin, An Orally Active Muscarinic Receptor Antagonist, Improves Pulmonary Function In Patients With Chronic Obstructive Pulmonary Disease: A Multicenter, Randomized, Double-Blind, Placebo-Controlled 3×3 Crossover Phase II Trial
Authors Machida K , Kawayama T, Kinoshita M, Ichinose M, Tsuda T , Takata S, Koto H , Yoshida M , Ashihara Y, Kawashima M, Suna H, Inoue H
Received 12 July 2019
Accepted for publication 5 September 2019
Published 19 September 2019 Volume 2019:14 Pages 2175—2184
DOI https://doi.org/10.2147/COPD.S223002
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Kentaro Machida,1,* Tomotaka Kawayama,2,* Masaharu Kinoshita,3,* Masakazu Ichinose,4 Tohru Tsuda,5 Shohei Takata,6 Hiroshi Koto,7 Makoto Yoshida,8 Yoshinori Ashihara,9 Masaru Kawashima,10 Hideaki Suna,10 Hiromasa Inoue1
1Department of Pulmonary Medicine, Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima 890-8520, Japan; 2Division of Respirology, Neurology, and Rheumatology, Department of Medicine, Kurume University School of Medicine, Kurume 830-0011, Japan; 3Nagata Hospital, Yanagawa 832-0059, Japan; 4Department of Respiratory Medicine, Tohoku University, Graduate School of Medicine, Sendai 980-8574, Japan; 5Kirigaoka Tsuda Hospital, Kitakyushu 802-0052 Japan; 6Division of Respiratory Medicine, National Hospital Organization Fukuoka-Higashi Medical Center, Koga 811-3195, Japan; 7Division of Respiratory Medicine, Kyushu Central Hospital of the Mutual Aid Association of Public School Teachers, Fukuoka 815-8588, Japan; 8Division of Respiratory Medicine, National Hospital Organization Fukuoka Hospital, Fukuoka 811-1394, Japan; 9Division of Respiratory Medicine, Oita Nakamura Hospital, Oita 870-0022, Japan; 10ONO Pharmaceutical Co. Ltd., Osaka 541-8564, Japan
*These authors contributed equally to this work
Correspondence: Hiromasa Inoue
Department of Pulmonary Medicine, Graduate School of Medical and Dental Sciences, Kagoshima University, 8-35-1 Sakuragaoka, Kagoshima 890-8520, Japan
Tel +81 99 275 6481
Fax +81 99 275 6482
Email [email protected]
Background: Although long-acting muscarinic receptor antagonists are central to the management of chronic obstructive pulmonary disease (COPD), inhaled medicines may have technical difficulty in some patients and adherence barriers.
Methods: A multicenter, randomized, double-blind, placebo-controlled 3×3 crossover Phase II trial was performed to evaluate the efficacy and safety of oral administration of the antimuscarinic agent imidafenacin in patients with COPD. Twenty-seven male COPD patients with % forced expiratory volume in 1 s (FEV1) ≥30% and <80% predicted were randomized to single oral dose of imidafenacin 0.1 mg, imidafenacin 0.2 mg, or placebo.
Results: Maximum change in FEV1 with both doses of imidafenacin significantly improved from baseline to 24 hrs after administration when compared with a placebo. Area under the curve in FEV1 during 24 hrs after administration with 0.2 mg, but not 0.1 mg dose, was significantly improved when compared with a placebo, and the improvement was significantly based on dose-dependent manners. Plasma imidafenacin level was positively correlated with change in FEV1. All subjects with both doses of imidafenacin completed without moderate nor severe adverse events.
Conclusion: A single oral dose of imidafenacin 0.1 mg or imidafenacin 0.2 mg may contribute to the improvement of pulmonary function with excellent safety and tolerability in patients with COPD.
Trial registration: JapicCTI-121760 (Japan Pharmaceutical Information Center – Clinical Trials Information [JapicCTI]; http://www.clinicaltrials.jp/user/cteSearch_e.jsp).
Keywords: anti-cholinergic, bronchodilator, imidafenacin, lung function, COPD
Introduction
Long-acting bronchodilators play a central role in the management for patients with chronic obstructive pulmonary disease (COPD), which is characterized by persistent airflow limitation.1 Long-acting muscarinic 3 (M3) receptor antagonists (LAMAs) and β2-agonists (LABA) are well known to improve lung function, quality of life (QOL), exercise tolerance, and attenuate frequency and severity of exacerbations and mortality in stable patients with COPD.2–7 To maximize the bronchodilation via direct effects and minimalize the systemic effects, every medicine of LAMAs is inhalant for management of chronic respiratory diseases.8–11 However, some patients, especially elderly, with COPD have difficulty in mastering inhalation techniques.12,13
Oral bronchodilators may potentially be more convenient, particularly for less compliant patients and those who have difficulty using inhaled medicines. Imidafenacin, 4-(2-methyl-1-H-imidazol-1-yl)-2,2-diphenyl butanamide, is one of the LAMAs with high affinity for the M3 and M1 muscarinic receptor subtypes and low affinity for the M2 subtype.14 The M3 subtype is expressed on airway smooth muscle and mediates bronchoconstriction. In contrast, prejunctional M2 receptors are expressed in nerves innervating the heart and lungs and inhibit the release of acetylcholine, and inhibition of the M2 subtype potentially increases the risk of bronchoconstriction and tachycardia. Therefore, we hypothesized that imidafenacin may have fewer side effects, allowing higher exposure and a favorable therapeutic margin. Doses of 0.1 mg–0.2 mg of oral imidafenacin already have established safety and tolerability in patients with overactive bladder worldwide including Japan.15,16
Preclinical studies demonstrated that oral administration of imidafenacin inhibited methacholine-induced bronchial constriction in a dose-dependent manner in guinea pigs (Figure S1). To verify a hypothesis based on the preclinical results that imidafenacin can improve pulmonary function, we conducted a multicenter, randomized, double-blind, placebo-controlled crossover Phase II trial with a 3×3 design, wherein the efficacy and safety of oral imidafenacin were examined in patients with COPD.
Methods
Study Design
To assess the efficacy and tolerability of two single doses of oral imidafenacin (0.1 mg and 0.2 mg) in patients with COPD, a multicenter, randomized, placebo-controlled, double-blind, three-treatment tertiary stage, crossover study was intended. The primary endpoint was the maximum change in forced expiratory volume in 1 s (FEV1) from baseline at various times during 24 hrs after administration of oral imidafenacin 0.1 mg or 0.2 mg. The secondary endpoint was the area under the curve (AUC) of FEV1 from baseline to 24 hrs after administration (AUC24h). The forced vital capacity (FVC), peak expiratory flow (PEF), maximal mid-expiratory flow (MMF), maximal expiratory flow at 50% (50) and 25% (25) vital capacity, and 50/25 were assessed as the exploratory endpoints.
The study was conducted in accordance with the principles of the Amended Declaration of Helsinki (2008) and the Guideline for Good Clinical Practice, and was approved by the Ethics Committee of each institution. After providing written informed consents, screening, and a 4-week run-in period, eligible patients were randomized to three separated 1-day treatment periods (Figure 1). Laboratory tests, vital signs, and a 12-lead electrocardiogram (ECG) were assessed at the screening visit. The treatments comprised a single dose of oral imidafenacin 0.1 mg, imidafenacin 0.2 mg, or placebo. All doses were administered in the morning between 08:00 and 10:00. Each treatment period was separated by a 7–28-day washout period.
Subjects
Japanese male or female patients aged ≥40 years with stable COPD stages II and III (an FEV1/FVC ratio <0.70 and 30% ≤ %FEV1 ˂80% predicted at post-bronchodilator: 2 puffs of salbutamol) according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) reports modified in 20101 and who had a smoking history of ≥10 pack-years were enrolled in the trial. Patients with a history of asthma, lung cancer, bronchiectasis, diffuse panbronchiolitis, sinobronchial syndrome, interstitial pneumonia, tuberculosis, and active malignancies were excluded. Patients with surgery of lungs, pregnant, nursing, and contraindications for imidafenacin were also excluded. Patients with long-term oxygen therapy (≥15 hrs/day) were also excluded.
Medication Restrictions
A list of contraindicating medicines and periods of non-recognition prior to pulmonary function tests at each visit are shown below; inhaled short-acting β2-agonists and muscarinic receptor antagonists for 8 hrs and 12 hrs, respectively, twice-daily and once-daily inhaled LABAs for 24 and 48 hrs, respectively, oral or transdermal β2-agonists for 24 hrs, LAMAs, injected or oral muscarinic receptor antagonists, and cholinergic agonists for 7 days, and twice-daily and once-daily theophylline for 24 and 48 hrs, respectively. Contraindication medicines were prohibited until the last administration of the study medications. Systemic corticosteroids, anti-allergic or histaminic agents, and injective methylxanthines were not accepted for COPD-related exacerbations through the trial.
Efficacy Assessments
Spirometry was performed in accordance with previous recommendations.17,18 The best value of three tests was employed. Assessments were conducted at the beginning of each period, and at 1, 2, 3, 4, 8, 12, and 24 hrs after administration of oral imidafenacin (Figure 1).
Pharmacokinetics
Within 15 mins before or after the pulmonary function tests, 5 mL of heparinized blood samples were collected before medication, and 1, 2, 3, 4, 8, 12, and 24 hrs after administration at each visit (Figure 1). The plasma concentration of imidafenacin was determined from blood samples by liquid chromatography–tandem mass spectrometry. A non-compartment analysis was used to determine the maximum plasma concentration of the analyte (Cmax), time to reach Cmax (Tmax), AUC24h, AUC from time 0 to infinity (AUCinf), elimination half-life (T1/2), and apparent clearance (CL/F).
Safety Assessments
Adverse events (AEs) were documented from screening visit to 28 days after the last study medications (period 3). However, the AEs related to imidafenacin or AEs which may be attributed to imidafenacin were recognized as side effects.
Statistical Analysis
Four patient populations were defined: all randomized patients (RND); safety analysis set (SAF); full analysis set (FAS); and per protocol set (PPS). The SAF comprised all patients who received at least one dose of study medication. The FAS included all randomized patients who received doses of the study medication and had at least one post-medication measurement. The PPS consisted of the subset of FAS patients who completed all doses of the study medication, who complied with the medication restrictions and who had all data of the maximum FEV1 change from baseline during 24 hrs after administration. The primary analysis population for efficacy was the PPS. As supportive analyses, the primary efficacy analyses were performed based on the FAS. The least-square mean values of peak FEV1 were compared between the groups by analysis of covariance (ANCOVA), which included the primary endpoint as the response variable, baseline FEV1 data at each test period as covariates, test drug effects, group effects, and period effects as factors, and subjects as random effects. Descriptive statistics were also calculated. The values for the secondary endpoint, AUC24h of FEV1, were compared between the groups by ANCOVA. Additional secondary endpoints of the maximum change rates and maximum changes of FVC, PEF, MMF, 50, 25, and 50/25 were evaluated by the same ANCOVA as that for the primary endpoint. The sample size of 26 (planned) was calculated using a paired t-test, to achieve at two-sided significance level of 5%, and power of 90% prior to the study, assuming a mean peak FEV1 and a standard deviation of between imidafenacin and placebo as 150.0 mL and 200.0 mL, respectively, based on study of tiotropium,19 referring to a previous preliminary study of imidafenacin20 using a crossover design, two-sided significance level of 5%, and power of 80%. For the safety analysis population, the incidence, severity, and time-course of AEs or side effects were collected by the Medical Dictionary for Regulatory Activities (MedDRA) system organ class as well as the preferred term in each treatment group of the SAF. Pharmacokinetic parameters such as Cmax, Tmax, AUC24h, AUCinf, T1/2, and CL/F were determined by a non-compartment analysis. An exposure/response analysis was also carried out using the FEV1 data.
Results
Patient Characteristics
A total of 27 patients were randomized to the treatment groups (Figure 2). The baseline characteristics of the patients are summarized in Table 1. All patients were males with a mean age of 69.9 ± 5.9 years old and a mean duration of COPD for 30.3 ± 28.3 months. The mean %FEV1 predicted and a ratio of FEV1/FVC after bronchodilators were 53.4% and 46.8%, respectively.
 |
Table 1 Baseline Characteristics Of Patients |
 |
Figure 2 Analyses for the enrolled subjects. |
Efficacy Assessment
The primary analysis population for efficacy was the PPS. The results for efficacy in the FAS were similar to those in the PPS. The FEV1 values at baseline did not differ among the groups for each treatment, and no group effect, period effect, or order effect were observed. Thus, it was judged that the crossover test was unbiased.
As shown in Table 2A, imidafenacin 0.1 mg and 0.2 mg produced a greater increase in the maximum change of FEV1 from baseline during 24 hrs after administration, compared with placebo, with differences of 0.06 and 0.09 L, respectively. Both differences were statistically significant (P=0.0286 and P=0.0017, respectively). Regarding the secondary endpoint, AUC24h of FEV1, the differences between imidafenacin 0.1 mg and placebo and between imidafenacin 0.2 mg and placebo were 0.91 L·h (P=0.0729) and 1.25 L·h (P=0.0175), respectively (Table 2B). For the exploratory endpoints, both the imidafenacin 0.1 mg and 0.2 mg groups showed significantly higher maximum change rates of FEV1 than the placebo group; 4.94% (P=0.0128) and 7.52% (P=0.0003), respectively (data not shown).
 |
Table 2 Changes In FEV1 After Oral Imidafenacin When Compared With Placebo |
Imidafenacin 0.1 mg and 0.2 mg resulted in significant improvement in FEV1 from 1 hr up to 4 hrs and from 1 hr up to 12 hrs compared with placebo, respectively (Figure 3, full data in Table S1). In addition, the differences in the change in FEV1 between imidafenacin 0.2 mg and placebo at 2 hrs and 3 hrs were 0.128 L (P<0.0001) and 0.115 L (P=0.0001), respectively (Figure 3). Regarding the maximum change and maximum change rate of FVC from baseline during 24 hrs after administration, imidafenacin 0.2 mg [0.15 L (P=0.0060) and 5.54% (P=0.0076)], but not 0.1 mg [0.08 L (P=0.1120) and 2.67% (P=0.1750)], showed significant increase compared with placebo. For the maximum change and maximum change rate of PEF (Table S2A), MMF (Table S2B), 50 (Table S2C), 25 (Table S2D), and 50/25 (Table S2E), the effects of both doses of imidafenacin did not differ from placebo.
Pharmacokinetics
The pharmacokinetic parameters after a single oral administration of imidafenacin 0.1 mg and 0.2 mg were analyzed by a non-compartment model, and are summarized in Figure 4. The plasma concentrations [mean ± SD, pg/mL at Tmax (Min – Max)] for imidafenacin 0.1 mg (FAS, n = 26) and 0.2 mg (n = 27) followed similar time-courses, reaching Cmax [582 ± 136 at 1.96 (0.93–3.83) hrs and 1250 ± 406 at 1.97 (0.92–4.00) hrs, respectively] after administration, and having mean (SD) of T1/2 and CL/P of 5.2 (0.97) and 26.7 (10.9) L/hr for imidafenacin 0.1 mg, and 5.3 (0.95) hrs and 25.9 (9.8) L/hr, respectively. The mean (SD) of AUC24h [3910 (1160) with imidafenacin 0.1 mg and 8270 (2690) with imidafenacin 0.2 mg] and AUCinf [4180 (1230) with imidafenacin 0.1 mg and 8680 (2880) with imidafenacin 0.2 mg] increased in roughly dose-dependent manners.
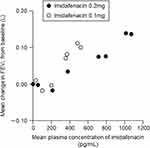
To evaluate the relationship between exposure and efficacy, the plasma imidafenacin concentrations were plotted against the change in FEV1 from baseline during 24 hrs after administration. The plasma imidafenacin level was positively correlated with the change in FEV1 during the 24-hrs period after imidafenacin administration (Figure 5).
Safety Assessments
All 27 subjects received the test drugs and were the targets of the safety analysis. However, one subject revoked consent after finishing Period 2, and did not receive imidafenacin at Period 3. Thus, the safety analysis populations were 27 subjects for placebo and imidafenacin 0.2 mg, and 26 subjects for imidafenacin 0.1 mg. The incidences of AEs were 11.1% in the imidafenacin 0.2 mg group and 7.7% in the imidafenacin 0.1 mg group, although there were no AEs in placebo group (Table 3). All AEs were mild, but not moderate nor severe. The imidafenacin 0.2 mg group had dry mouth (3.7%), muscle stiffness (3.7%), insomnia (3.7%), and skin exfoliation (3.7%), whereas the imidafenacin 0.1 mg group had thirst (3.8%) and T-wave inversion (3.8%) by ECG as AEs. No meaningful clinical changes in blood pressure or heart rate measured up to 24 hrs after administration were noted in all groups (data not shown). There were also no clinically relevant changes in routine laboratory tests from the run-in period to the study completion.
 |
Table 3 Summary of Adverse Events |
Discussion
This study assessed the efficacy and safety of oral administration of imidafenacin in the treatment of COPD. The results showed that imidafenacin 0.1 mg and 0.2 mg were effective for the primary endpoint (maximum change in FEV1 from baseline during 24 hrs after administration), and that imidafenacin 0.2 mg, but not 0.1 mg, was effective for the secondary endpoint (AUC24h of FEV1). However, the imidafenacin 0.1 mg increased the parameters to almost the levels of statistical significance, when compared with a placebo.
The pharmacokinetic profiles of imidafenacin 0.1 mg and 0.2 mg showed almost identical Tmax, T1/2, and CL/F values with dose-dependent Cmax and AUC values in patients with COPD. The profiles of kinetics were generally the same as previous observations in healthy subjects.19 The previous study reported that the minimum change was 0.10 L in trough FEV1 and has been recommended as the minimum clinically important difference in patients with COPD.21 Actually, inhaled long-acting bronchodilators such as tiotropium and glycopyrronium bromide improve FEV1 to exceed 0.10 L over 12 hrs in patients with COPD. Regarding oral imidafenacin 0.2 mg, the changes in FEV1 were significantly higher than those for placebo from 1 hr up to 12 hrs, especially the changes at 2 hrs and 3 hrs of 0.128 L (P<0.0001) and 0.115 L (P=0.0001), respectively.
The treatment with imidafenacin 0.1 mg and 0.2 mg was well tolerated, as all subjects completed the trial without moderate or severe AEs including dysuria or glaucoma attacks in our study. Transient dry mouth and thirst and T-wave inversion by ECG might be related with imidafenacin as anticholinergic effects. All AEs (Table 3) were mild and also already known previously.15,22,23 Neither clinically meaningful changes in vital signs nor clinically relevant changes occurred for both doses of imidafenacin in laboratory tests. Imidafenacin is predominantly metabolized by cytochrome P450 3A4 and uridine 5ʹ-diphospho-glucuronosyltransferase 1A4 in liver.24 The prevalence of COPD increases with age. Although the oral clearance of imidafenacin is decreased with advancing age, it has been reported that the effect of age on oral clearance was limited.25 Previous studies supported our results that oral imidafenacin showed better tolerances and was safer than other anticholinergics in patients with overactive bladder disorder.14–16
Regarding the balance of pharmacological benefits and risks on chronic airway diseases between oral and inhaled administration, oral administration may have more effects on central to peripheral airway as benefits, but may exert more influences systemically as risks. Both doses of oral imidafenacin did not improve peripheral airway function, indicated in parameters of MMF, 25, 50, and 50/25 (Table S2A–E). Our results showed that treatment with oral imidafenacin had benefits with the improvement of FEV1 safety in patients with COPD who had difficulty mastering inhalation techniques.13 Oral imidafenacin was less effective in improving lung function than approval inhaled LAMAs, such as tiotropium, glycopyrronium, or umeclidinium. However, many studies have demonstrated that oral medications improve patient satisfaction and adherence compared with inhaled drugs.26–28 Oral administration may contribute to pharmacological adherences significantly.
Our study demonstrated the efficacy and safety of a single dose of oral imidafenacin. Comparisons of efficacy between once-daily and twice-daily LAMAs are limited in the management for patients with COPD.29,30 Using a network meta-analysis of randomized controlled trials, the twice-daily dosing had the efficacy of similar improvement in the lung function, health-related quality of life, and dyspnea when compared with once-daily dosing of LAMAs.29,30 However, the twice-daily dosing may have more benefits than once-daily doing 12 hrs to 24 hrs after initial administration.31 Aclidinium, twice-daily dosing, provided more bronchodilation during the nighttime, improvement of early-morning and nighttime symptoms, and early-morning limitation of activity than tiotropium, a once-daily dosing of LAMAs, in patients with moderate to severe COPD.32 Imidafenacin should be administrated twice-daily clinically as like the treatment of patients with overactive bladder.
Our study has some limitations. First, imidafenacin showed no improvement of peripheral airway function. The sample size might be too small to find evidence since we calculated the sample size based on the estimated difference of FEV1, primary endpoint, between imidafenacin and placebo. Second, the study was conducted only with the oral single administration. Thus, the efficacy of twice-daily dosing of oral imidafenacin is still unclear. Further studies are needed to evaluate the effects, tolerances, and safety of long-term usage. Third, the efficacy and safety of long-term imidafenacin therapy is still unknown in patients with COPD. Further studies are necessary to address these limitations.
Conclusion
In conclusion, the present study showed the potential usefulness and tolerability of oral imidafenacin for improving the pulmonary function of patients with COPD.
Abbreviations
AEs, adverse events; ANCOVA, analysis of covariance; AUC, area under the curve; AUC24h, AUC from baseline to 24 hrs; AUCinf, AUC from time 0 to infinity; CL/F, clearance; Cmax, maximum plasma concentration of analyte; COPD, chronic obstructive pulmonary disease; ECG, electrocardiogram; FAS, full analysis set; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease; MedDRA, Medical Dictionary for Regulatory Activities; MMF, mid-maximum flow; PEF, peak expiratory flow; PPS, per protocol set; RND, randomized patients; SAF, safety analysis set; SD, standard deviation; T1/2, elimination half-life; Tmax, time to reach Cmax; V25, 25% vital capacity; V50, 50% vital capacity.
Ethics Approval And Consent To Participate
The study was approved by the Ethics Committee of each of the participating institutions and all subjects gave written informed consent.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
Funding for this study was provided by Ono Pharmaceutical Co., Ltd., Osaka, Japan. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We would like to thank the investigators, health care providers, research staff, and patients who participated in this study. A complete list of the investigators is provided in the Supplementary Appendix.
Author Contributions
Dr. Machida, Dr. Kawayama, Dr. Kinoshita, Dr. Tsuda, Dr. Takata, Dr. Koto, Dr. Yoshida, Dr. Ashihara, and Dr. Inoue were investigators for this study. Dr. Ichinose was the medical advisor for this study. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr. Kinoshita received honoraria from GlaxoSmithKline K.K., Daiichi Sankyo Co. Ltd., Novartis Pharma K.K., Takeda Pharmaceutical Co. Ltd., and Astellas Pharma Inc. Dr. Tsuda received honoraria from Novartis Pharma K.K., Pfizer Japan Inc., and Nippon Boehringer Ingelheim Co. Ltd. Mr. Kawashima and Dr. Suna are full-time employees of Ono Pharmaceutical Co. Ltd., Japan. Dr. Inoue received research grants from Asahi Kasei Corporation, Astellas Pharma Inc., Nippon Boehringer Ingelheim Co. Ltd., Chugai Pharmaceutical Co. Ltd., Sumitomo Dainippon Pharma Co. Ltd., Eisai Co. Ltd., MSD K.K., Nippon Kayaku Co. Ltd., Shionogi & Co. Ltd., Taisho Toyama Pharmaceutical Co. Ltd., and Teijin Pharma Ltd.; gave lectures and acted on advisory committees for Asahi Kasei Corporation, Astellas Pharma Inc., AstraZeneca K.K., Nippon Boehringer Ingelheim Co. Ltd., Chugai Pharmaceutical Co. Ltd., Eisai Co. Ltd., GlaxoSmithKline K.K., Eli Lilly Japan K.K., Kyorin Pharmaceutical Co. Ltd., MSD K.K., Meiji Seika Pharma Co. Ltd., Novartis Pharma K.K., Otsuka Pharmaceutical Co. Ltd., Pfizer Japan Inc., Shionogi & Co. Ltd., Taisho Pharmaceutical Co. Ltd., and Teijin Pharma Ltd. The authors report no other conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of COPD [updated 2019]. Available from: https://goldcopd.org/gold-reports/.
2. Wu J, Sin DD. Improved patient outcome with smoking cessation: when is it too late? Int J Chron Obstruct Pulmon Dis. 2011;6:259–267. doi:10.2147/COPD.S10771
3. Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. JAMA. 1994;272(19):1497–1505. doi:10.1001/jama.1994.03520190043033
4. Nrdini S, Camiciottoli G, Locicero S, et al. COPD: maximization of bronchodilation. Multidiscip Respir Med. 2014;9(1):50. doi:10.1186/2049-6958-9-50
5. Babu KS, Morjaria JB. Emerging therapeutic strategies in COPD. Drug Discov Today. 2015;20(3):371–379. doi:10.1016/j.drudis.2014.11.003
6. Ross CL, Hansel TT. New drug therapies for COPD. Clin Chest Med. 2014;35(1):219–239. doi:10.1016/j.ccm.2013.10.003
7. Barnes PJ. New anti-inflammatory targets for chronic obstructive pulmonary disease. Nat Rev Drug Discov. 2013;12(7):543–559. doi:10.1038/nrd4025
8. Aagha K, Palot A, Sofalvi T, et al. Long-acting muscarinic receptor antagonists for the treatment of chronic airway diseases. Ther Adv Chronic Dis. 2014;5(2):85–98. doi:10.1177/2040622313518227
9. Prakash A, Babu KS, Morjaria JB. Novel anti-cholinergics in COPD. Drug Discov Today. 2013;18(21–22):1117–1126. doi:10.1016/j.drudis.2013.07.005
10. Disse B, Speck GA, Rominger KL, et al. Tiotropium (Spiriva): mechanistical considerations and clinical profile in obstructive lung disease. Life Sci. 1999;64(6–7):457–464. doi:10.1016/s0024-3205(98)00588-8
11. Cazzola M, Page CP, Calzetta L, et al. Pharmacology and therapeutics of bronchodilators. Pharmacol Rev. 2012;64(3):450–504. doi:10.1124/pr.111.004580
12. Lavorini F. Inhaled drug delivery in the hands of the patient. J Aerosol Med Pulm Drug Deliv. 2014;27(6):414–418. doi:10.1089/jamp.2014.1132
13. Aydemir Y. Assessment of the factors affecting the failure to use inhaler devices before and after training. Respir Med. 2015;109(4):451–458. doi:10.1016/j.rmed.2015.02.011
14. Kobayashi F, Yageta Y, Segawa M, et al. Effects of imidafenacin (KRP-197/ONO-8025), a new anti-cholinergic agent, on muscarinic acetylcholine receptors. Arzneimittelforschung. 2007;57(2):92–100. doi:10.1055/s-0031-1296589
15. Masumori N. Long-term safety, efficacy, and tolerability of imidafenacin in the treatment of overactive bladder: a review of the Japanese literature. Patient Prefer Adherence. 2013;7:111–120. doi:10.2147/PPA.S28160
16. Leone Roberti Maggiore U, Scala C, Venturini PL, et al. Imidafenacin for the treatment of overactive bladder. Expert Opin Pharmacother. 2013;14(10):1383–1397. doi:10.1517/14656566.2013.796930
17. Miller MR, Hankinson J, Brusasco V, et al.; ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805.
18. The Japanese Respiratory Society. Guideline of respiratory function tests – spirometry, flow-volume curve, diffusion capacity of the lung. Nihon Kokyuki Gakkai Zasshi. 2004;Suppl:1–56 [article in Japanese].
19. Ohno T, Nakade S, Nakayama K, et al. Absolute bioavailability of imidafenacin after oral administration to healthy subjects. Br J Clin Pharmacol. 2008;65(2):197–202. doi:10.1111/j.1365-2125.2007.02999.x
20. Machida K, Sadamura Y, Mizuno K, Higashimoto I, Inoue H. Bronchodilator efficacy of single administration of oral anticholinergic agent in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185:A2919.
21. Donohue JF. Minimal clinically important differences in COPD lung function. COPD. 2005;2(1):111–124. doi:10.1081/COPD-200053377
22. Zaitsu M, Mikami K, Ishida N, et al. Comparative evaluation of the safety and efficacy of long-term use of imidafenacin and solifenacin in patients with overactive bladder: a prospective, open, randomized, parallel-group trial (the LIST study). Adv Urol. 2011;2011:854697. doi:10.1155/2011/854697
23. Homma Y, Yamaguchi T, Yamaguchi O. A randomized, double-blind, placebo-controlled phase II dose-finding study of the novel anti-muscarinic agent imidafenacin in Japanese patients with overactive bladder. Int J Urol. 2008;15(9):809–815. doi:10.1111/j.1442-2042.2008.02104.x
24. Kanayama N, Kanari C, Masuda Y, et al. Drug–drug interactions in the metabolism of imidafenacin: role of the human cytochrome P450 enzymes and UDP-glucuronic acid transferases, and potential of imidafenacin to inhibit human cytochrome P450 enzymes. Xenobiotica. 2007;37(2):139–154. doi:10.1080/00498250601140072
25. Ohno T, Nakade S, Nakayama K, et al. Population pharmacokinetic analysis of a novel muscarinic receptor antagonist, imidafenacin, in healthy volunteers and overactive bladder patients. Drug Metab Pharmacokinet. 2008;23(6):456–463.
26. Volovitz B, Dueñas-Meza E, Chielewska-Szewczyk DA, et al. Comparison of oral montelukast and inhaled cromolyn with respect to preference, satisfaction, and adherence: a multicenter, randomized, open-label, crossover study in children with mild to moderate persistent asthma. Curr Ther Res. 2000;61(7):490–506. doi:10.1016/S0011-393X(00)80032-6
27. Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. doi:10.1136/thx.2007.086041
28. Imamura Y, Kawayama T, Kinoshita T, et al. Poor pharmacological adherence to inhaled medicines compared with oral medicines in Japanese patients with asthma and chronic obstructive pulmonary disease. Allergol Int. 2017;66(3):482–484. doi:10.1016/j.alit.2016.10.008
29. Ismaila AS, Huisman EL, Punekar YS, et al. Comparative efficacy of long-acting muscarinic antagonist monotherapies in COPD: a systematic review and network meta-analysis. Int J Chron Obstruct Pulmon Dis. 2015;10:2495–2517. doi:10.2147/COPD.S92412
30. Karabis A, Lindner L, Mocarski M, et al. Comparative efficacy of aclidinium versus glycopyrronium and tiotropium, as maintenance treatment of moderate to severe COPD patients: a systematic review and network meta-analysis. Int J Chron Obstruct Pulmon Dis. 2013;8:405–423. doi:10.2147/COPD.S48967
31. Fuhr R, Magnussen H, Sarem K, et al. Efficacy of aclidinium bromide 400 μg twice daily compared with placebo and tiotropium in patients with moderate to severe COPD. Chest. 2012;141(3):745–752. doi:10.1378/chest.11-0406
32. Beier J, Mroz R, Kirsten A-M, Chuecos F, Gil EG. Improvement in 24 hr bronchodilation and symptom control with aclidinium bromide versus tiotropium and placebo in symptomatic patients with COPD: post hoc analysis of a Phase IIIb study. Int J Chron Obstruct Pulmon Dis. 2017;12:1731–1740. doi:10.2147/COPD.S121723
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.