Back to Journals » Clinical Epidemiology » Volume 15
Identifying Non-Steroidal Anti-Inflammatory Drug (NSAID) Users Among People with Osteoarthritis Through Administrative and Clinician-Reported Data – A Validation Study of 116,162 Patients
Authors Dell'Isola A , Kiadaliri A , Hellberg C , Turkiewicz A, Englund M
Received 16 December 2022
Accepted for publication 19 April 2023
Published 16 June 2023 Volume 2023:15 Pages 743—752
DOI https://doi.org/10.2147/CLEP.S401726
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Andrea Dell’Isola, Ali Kiadaliri, Clara Hellberg, Aleksandra Turkiewicz, Martin Englund
Clinical Epidemiology Unit, Department of Clinical Sciences Lund, Orthopedics, Lund University, Lund, Sweden
Correspondence: Andrea Dell’Isola, Email [email protected]
Purpose: (i) To report the prevalence of participants to a first-line intervention for OA in Sweden using over-the-counter (OTC) and/or prescribed NSAIDs; (ii) To estimate the accuracy of dispensed prescriptions of NSAIDs recorded in a Swedish health-care register to capture the use of NSAID considering clinician-report as reference standard.
Methods: Register-based study. We used data from OA individuals who participated in the Swedish first-line intervention recorded in the Swedish Osteoarthritis Register (SOAR). SOAR includes clinician-reported use of NSAIDs in the three months preceding the intervention. We used the Prescribed Drug Register to retrieve data on NSAID prescriptions dispensed in the same period. We estimated the prevalence of OTC users (individuals with clinicians-reported use of NSAID but no prescription dispensed), prescription users (individuals with clinicians-reported use of NSAID and a prescription dispensed) and non-users (neither of the previous). We calculated sensitivity, specificity, positive predictive value, and negative predictive value of dispensed prescriptions of NSAIDs vs clinician-report.
Results: We included 116,162 individuals (mean age [Standard Deviation]: 66 [9.6] years, 79% women, 77% knee OA). Overall, 24.7% (95% Confidence Intervals [CI] 24.5%; 25.0%) used OTC NSAIDs only, 18.2% (18.0%; 18.5%) used prescribed NSAIDs, 6.6% (6– 4%; 6.7%) reported not using NSAIDs while having an NSAID prescription dispensed. Of the 49,913 individuals with clinician-reported use of NSAIDs, 21,190 had a prescription dispensed (sensitivity: 42.5% [95% CI 42.0%, 42.9%]; positive predictive value: 73.5% [73.0%, 74.0%]). Of the 66,249 individuals reporting not using NSAIDs, 58,617 did not have a prescription dispensed (specificity: 88.5% [88.2%, 88.7%]; negative predictive value: 67.1% [66.8%, 67.4%]).
Conclusion: Overall, 24.7% of participants in a first-line intervention for OA used OTC NSAIDs only while 18.2% used prescribed NSAIDs. Dispensed prescriptions of NSAIDs have high specificity but low sensitivity and can correctly identify about 70% of both the non-users and users in this population.
Keywords: osteoarthritis, NSAID, register, validation
Introduction
Osteoarthritis (OA) affects more than 500 million people worldwide causing pain and disability.1 In the last 30 years, the prevalence of OA has increased by nearly 50%, a trend that is expected to continue.2 Without disease-modifying treatments, oral Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) are the most used pharmaceutical for OA pain control and are at least conditionally recommended by clinical practice guidelines as second-line treatments for OA.3,4 Still, NSAIDs are often preferred to first-line treatments – exercise, weight loss, and self-management – and are with opioids the most used treatment for OA in the US.5
NSAIDs are considered safe at low doses and for brief treatment periods. Nevertheless, their use is associated with a significant health burden due to frequent adverse events.6 Electronic medical records are important to study trends, side effects, and burden on society over long periods, which would otherwise be impossible in randomized controlled trials. However, many NSAIDs can be purchased over the counter (OTC) and are seldom recorded in health-care registers. A report from the 2011 five European countries (5EU) National Health and Wellness Survey (NHWS) suggested that 64% of people with OA report using NSAIDs, of which 17% use OTC-only and 9% use both.7 Other reports using insurance records showed a similar prevalence of prescribed and OTC NSAIDs among analgesic users in France.8 These results suggest that using prescribed NSAIDs may underestimate the proportion of real NSAID users, leading to the underestimation of the costs and burdens of these pharmaceuticals.
The aims of this study are: (i) to report the prevalence of participants to a first-line intervention for OA in Sweden using OTC and/or prescribed NSAIDs; (ii) to estimate the accuracy of dispensed prescriptions of NSAIDs recorded in a Swedish health-care register to capture the use of NSAID considering clinician-report as reference standard.
Methods
National Data Sources
We conducted a study using data from two National Swedish registers. The Swedish Osteoarthritis Register (SOAR) contains data from persons with knee or hip OA, who have participated in a face-to-face first-line treatment offered in more than 500 different physical therapist units all over Sweden.9 The Prescribed Drug Register contains information on all drugs prescribed and then dispensed at one of the pharmacies in the country, with data available from July 2005 and provided data on the dispensation of prescribed NSAIDs. The data from the different registers are linked through the personal unique identification number assigned to all residents in Sweden by the Swedish Tax Agency. The study was approved by the Lund University Ethics Committee (Dnr 2011e432 with amendments Dnr 2014_276, and Dnr 2018_233). We reported the study according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.10 Data management and analysis was performed in accordance with the General Data Protection Regulation (GDPR).
Study Population
All participants to the first-line intervention for OA recorded in SOAR have an OA diagnosis─which includes hip, knee, hand and shoulder OA─according to the recommendations from the Swedish National Board of Health and Welfare.9,11 The first-line intervention includes education (mandatory) and exercise (voluntary). The intervention has been described previously.12–14 Patients cannot take part in the intervention and are not registered in SOAR if: (i) there are reasons other than OA for joint problems (eg, sequel hip fractures, chronic widespread pain, inflammatory joint diseases, or cancer); (ii) they received a total joint replacement within the past 12 months or other surgery of the knee or hip joint within the past 3 months, and (iii) they are unable to read or understand Swedish.
Inclusion and Exclusion Criteria
We included all the people recorded in the BOA register who underwent the baseline visit of the intervention between January 1st 2008 and December 31st 2019. If a person had several baseline visits (eg, due to undergoing the program multiple times), we selected the first one. Persons with missing values for clinician-reported NSAID use were also excluded.
NSAIDs Regulations in Sweden
Sweden has publicly funded healthcare with a high-cost protection scheme where there is a ceiling for out-of-pocket payments for health-care visits and medications. This means that after reaching this ceiling threshold within a period of 12 months any additional care is free of charge.15 Treatments for OA ─ including surgery, prescribed analgesics, and physiotherapy ─ are included in this scheme. For drug dispensation, the ceiling threshold for a patient’s co-payments over 12 months (starting from the first purchase) is SEK 2400 (at the date of data extraction, equivalent to≈ EUR 220) after which any dispensation within 12 months is free of charge. Certain pharmaceuticals are also available OTC. Although each dispensing of OTC analgesics is confined to maximum pack sizes (eg, 12 g of Ibuprophen), there are no restrictions on the number of packages sold per person per day.16 Direct-to-consumer advertisement is allowed for OTC drugs if it provides a current, factual and balanced presentation that promotes the appropriate use of the drug.16
Clinician-Reported Use of NSAIDs
During the baseline visit, the patient is asked by the physiotherapist to list the drugs used in the last three months to manage the joint symptoms (has the patient taken drugs for the joint in the last three months? [yes/no]). The physiotherapist then first marks if the person has used drugs, and which specific drug was used choosing between paracetamol, NSAIDs or acetylsalicylic acid, glucosamine, hyaluronic acid injections, cortisone injection, natural remedies, other based on the information from the patient (ie, it is the physiotherapist that allocates the reported drugs to the above categories).
NSAIDs Dispensation
We used ATC codes to identify dispensed prescriptions of NSAIDs from the Prescribed Drug Register according to the list provided in Supplementary File 1, which has been used to identify NSAIDs use in Swedish register studies.17 Despite acetylsalicylic acid is not an NSAID, it was included in the list to reflect the grouping of NSAIDs used in the BOA register. All the drugs recorded in the Prescribed Drug Register have been prescribed and then dispensed.
Analysis
For aim (i), we used the clinician-reported NSAID use (yes or no) in the last 90 days before the visit and the NSAID-dispensed prescription during the same time interval to define NSAID-use status. People with clinician-reported NSAID use and without any dispensed prescription were classified as OTC users only. People with clinician-reported NSAID use and a dispensed prescription were considered using prescribed NSAIDs (this category includes users of prescribed NSAIDs only or of prescribed NSAIDs in combination with OTC NSAIDs). People with neither clinician-reported use nor dispensed prescription were regarded as non-users. We used the Stata command “proportions” to compute logit-transformed CIs for the NSAID use status. For aim (ii), we used clinician-reported NSAID use as the reference standard, to test the ability of registry records of dispensed prescriptions to identify people using NSAIDs. We used the Stata command “diagt” to calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of dispensed NSAIDs with 95% exact binomial confidence intervals.18 We reported the percentage of individuals correctly classified (number of individuals with the same status in both NSAID variables/total sample) to provide a single metric of the observed agreement between the analyzed variables and facilitate comparison with previous studies. Considering that using prescribed NSAIDs may depend on the baseline pain, age, and year of enrollment in the OA intervention, we repeated the analysis stratified by pain (measured with a 0–10 NRS scale; mild 0–3, moderate 4–6, severe 7–10), age (<60, 60–69, 70–79, 80+) and calendar year (2008 to 2019). To increase comparability between strata, we standardized by sex, and age (5-year strata) the analyses stratified by pain; by sex and pain (mild, moderate, severe) the analysis stratified by age while we standardized for age, sex and pain the analysis by year. Standardizations were based on the distribution of sex, age, and pain in the entire sample. Finally, people may have reported using NSAIDs that were prescribed and dispensed >90 days before the visit. As a further sensitivity analysis, we extended the time for the dispensation date to 120 days prior to the baseline visit.
Results
A total of 123,642 individuals were recorded in SOAR. After excluding duplicate cases (n = 555), 116,162 participants (mean age [Standard Deviation (SD)]: 66 [9.6] years, 79% women, 77% with knee OA) without missing data on the clinician-reported NSAID use for OA were included in the study (Figure 1, Table 1). When looking at the NSAID use in the whole sample, 24.7% (24.5%; 25.0%) of the individuals were classified as OTC users only, 18.2% (18.0%; 18.5%) as users of dispensed NSAID prescriptions, and 6.6% (6.4%; 6.7%) as non-users with a dispensed NSAID prescription (Figure 2, Supplementary File 2). When considering clinician-reported NSAID use as reference to identify users and non-users, dispensed NSAID could correctly classify 69% of the sample. Among the 49,913 individuals reporting using NSAIDs for their OA, 21,190 had a dispensed prescription (sensitivity 42.5%; 95% CI 42.0%; 42.9%) (Table 2). Overall, the probability of being an NSAID user for those with a prescription for NSAIDs (PPV) was 73.5% (73.0%; 74.0%). Among the 66,249 individuals reporting no use of NSAIDs, 58,617 had no prescription (specificity 88.5%; 95% CIs 88.2%; 88.7%). Overall, the probability of being a non-user for those without a prescription (NPV) was 67.1% (66.8%; 67.4%).
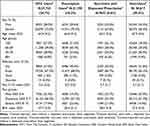 |
Table 1 Demographics and Sample Characteristics by NSAID User Category |
 |
Table 2 Prevalence of Reported NSAID Use and Psychometric Values of Dispensed NSAIDs in the 90 Days Preceding a First-Line Intervention to Identify People Reporting Use of NSAIDs |
 |
Figure 1 Study flowchart. |
 |
Figure 2 Prevalence of NSAID use in the whole sample and in age and pain categories. Confidence intervals of the estimate can be found in the Supplementary File 2. |
The secondary analyses showed that the prevalence of OTC NSAID use was stable across pain strata, while the prevalence of prescription users was lowest among those with mild pain and higher among those with severe pain (Figure 2, Supplementary File 2). Sensitivity and specificity also varied in the different pain strata. Sensitivity was lowest among people with mild pain and highest in people with severe pain. Specificity showed the opposite trend, but differences were smaller and values were relatively high in all groups (Supplementary File 3). The analyses by age strata showed that the prevalence of both OTC and prescribed NSAID use was highest in the youngest age stratum and decreased with increasing age (Figure 2, Supplementary File 2). The same trend was observed for the sensitivity, while specificity showed an opposite trend decreasing with increasing age. The analysis by year of participation in the OA intervention showed that the prevalence of OTC use was stable over time while the prevalence of prescription users decreased over the years (Figure 3, Supplementary File 4). Finally, NSAID dispensation within 120 days before enrollment (instead of 90) could correctly classify as user or non-user 66% of the sample. Sensitivity, specificity, as well as PPVs and NPVs were similar to the ones obtained from the main analysis (Supplementary File 3).
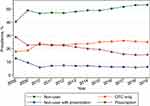 |
Figure 3 Prevalence of NSAID-user categories by calendar year. Confidence intervals of the estimate can be found in the Supplementary File 4. |
Discussion
We investigated the use of NSAIDs in a large cohort of more than 100,000 individuals with hip or knee OA participating in a first-line intervention. We found that 43% of the individuals reported using NSAIDs while 25% had a dispensed prescription. Thus, we classified 25% of the total sample as OTC-only users and 18% as prescription users. Overall, dispensed prescriptions of NSAIDs have poor sensitivity and high specificity to identify NSAID users for OA. Nevertheless, PPVs and NPVs suggest that roughly 30% of the individual may be misclassified when using health records of dispensed NSAIDs prescription to identify NSAID users for OA.
NSAIDs are a largely used class of pharmaceuticals among people with OA. The prevalence of reported use of NSAIDs in our cohort is in line with previous studies. Among OA patients referred to an outpatient rehabilitation center for OA in the Netherlands, 30% reported using NSAIDs, while in a large cohort of participants to a similar first-line intervention in Denmark, the prevalence of NSAID use was 37%.19,20 For what concerns NSAIDs prescription, the prevalence in our cohort (25%) was similar to what was reported in study analyzing a general population of OA patients (n = 1,760) sampled from France, Germany, Italy, Spain and the UK, where nearly 28% self-reported to use NSAIDs under prescription.7
In a study from Denmark, the authors reported a 75% of agreement between reported use of NSAIDs to a physiotherapist and NSAID dispensation from a national register (ie, both variables were yes or both no).21 In our study, the observed agreement between the reported use of NSAIDs and dispensed NSAIDs is 69%. For what concerns the psychometric values of prescribed NSAIDs to identify people reporting to use NSAIDs for OA, we observed an overall high specificity of around 90% in both the full-sample and analyzed subgroups. Sensitivity, on the other hand, was low varying between 42% in the full sample to 25% among individuals >80 years. These results suggest that the Swedish Prescribed Medication register may be adequate to identify individuals who use NSAIDs for OA with few false positives. However, sensitivity and specificity focus on the adequacy of a test (in this case the health record of dispensed NSAIDs) and should be interpreted carefully when deciding on individual people or population samples.22 When selecting a study population for an epidemiological study, the PPV and NPV may be more adequate metrics to consider. In our case, these metrics suggest a probability of around 30% to classify incorrectly a user (PPV) or a non-user (NPV) when using health records of NSAID dispensation to identify NSAID users. Whether these values are acceptable will largely depend on the research questions and scope of the study.22 However, the prevalence of the studied condition (use of NSAIDs in our case) should also be considered as it influences these metrics. In the analysis by age strata, we observed a change of ≈11% in PPV (decrease) and NPV (increase) between the age group <60 years (prevalence of NSAIDs users 58%) and >80 years (prevalence of NSAIDs users 25%).
The use of OTC NSAIDs is normally not recorded in drug use registers and is seldom investigated in people with OA. Kingsbury et al reported that, in a sample of subjects from the Osteoarthritis Initiative (OAI) progression cohort, 26% of the subjects used OTC medications, which included also other pharmaceuticals than NSAIDs.23 Moreover, only 8.7% of the study sample reported pain NRS scores greater than two units (on a 0–10 scale) in the month before the visit, a rather mild symptomatology for an OA population. All in all, comparison with other cohorts requires care as NSAID use (prescribed or OTC) can be strongly influenced by the characteristics of the population, the NSAIDs analyzed and national regulations, the impact of which is hard to evaluate.
In our sample, we observed that a large share of the OA population undergoing an education and exercise intervention uses OTC NSAIDs. OTC NSAIDs appear to be more common among younger OA patients with 29% of those aged <60 years using OTC medication compared to 16% of those >80 years. This could be expected considering that NSAIDs are not recommended in persons more than 75 years old or frail.3,24 Nevertheless, the proportion of people >80 years using OTC NSAIDs is almost double that of those with an NSAID prescription. These figures may suggest that people not receiving a prescription due to potential contraindications may resort to self-care. Analyses by calendar year showed a stable prevalence of OTC users over time while highlighting a decrease in the prevalence of prescription users of around 7% from 2009 to 2019. This trend can be the result of the growing attention around the safety of NSAIDs for the treatment of chronic painful conditions such as OA or could result from more patients entering the intervention at an earlier stage of the disease.25
Nearly 7% of the sample (7632 individuals) reported not using NSAIDs for the OA joint despite having a prescription dispensed in the previous three months, this figure was consistent in all the analyzed subgroups. A possible explanation may lie in the intermittent nature of OA pain and in clinical recommendations discouraging prolonged use of NSAIDs.3,26 In this scenario, prescribers may instruct patients to take out the prescription and use the drug in case of pain bouts. Another possible explanation is that the NSAIDs were prescribed for other complaints than OA. In this scenario, the patients may have reported no use of NSAIDs for OA despite having a dispensed prescription.
This study has some important strengths, but also limitations that need to be acknowledged. We used a large cohort of more than 120,000 patients participating in a first-line intervention for OA provided nationwide in Swedish primary care. Results from this study are therefore expected to mirror the use of NSAIDs among patients seeking treatment for OA. The use of NSAID and the type of compound used were reported by the patient which implies that recall bias may be present and difficult to assess. Nevertheless, this information was collected during an interview with a physiotherapist which may reduce the risk of compounds being misclassified. Moreover, our sensitivity analysis showed that increasing by 30 days the time for a dispensed prescription did not increase the proportion of users correctly classified. For what concerns the drug prescriptions, we used electronic records based on prescriptions dispensed at any pharmacy in Sweden, which means that medications prescribed but not dispensed were not included. This is a strength for our research questions that concern the use of medications, but it limits the applicability of our results to studies on prescription patterns. Further, the question assessing the use of NSAIDs was specific for medication to relieve OA symptoms in the treated joint (knee and/or hip) while some of the dispensed NSAIDs may have been prescribed for other disorders (eg, low back pain or other local pain/inflammation such as tendonitis, shoulder pain, etc.). Nevertheless, the population included in this study was seeking care for hip or knee OA which increases the likelihood that the observed dispensations are linked to the joint problem. Finally, this study relies on data from Sweden. Given the large variations in the patterns of NSAIDs prescription and use across countries as well as across different subgroups of the same population (eg, age and pain severity), the generalizability of the results to countries with different health-care systems needs caution.
Conclusions
NSAIDs are commonly used by people with OA. In our sample, we could attribute 25% of the NSAID use to medications purchased OTC. Moreover, the share of OTC users appears to vary based on the age of the individuals. Overall, health records of dispensed prescriptions of NSAIDs could correctly classify 69% of the sample and showed high specificity but low sensitivity to identify NSAID users for OA. This suggests that prescribed NSAIDs may be adequate for selecting samples of NSAID users, but less adequate when trying to quantify the total number of users in a population.
Data Sharing Statement
The data used in this study can be obtained directly from the relevant agencies (https://www.vgregion.se; https://www.socialstyrelsen.se).
Acknowledgment
This study was also presented at the Osteoarthritis Research Society International (OARSI) conference as an abstract presentation with interim findings. The poster’s abstract was published in Osteoarthritis and Cartilage, Volume 31, S235 - S236; DOI: https://doi.org/10.1016/j.joca.2023.01.232. We would also like to acknowledge the SOAR, and the National Board of Health and Welfare, Sweden, for accessing their databases. The interpretation and conclusions contained in this study are those of the authors alone. We would also like to thank all the participants to the intervention recorded in SOAR for agreeing for their data to be used for research purposes.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was funded by the Swedish Research Council, Greta and Johan Kock Foundations, The Swedish Rheumatism Association, Österlund Foundation, Governmental Funding of Clinical Research within National Health Service (ALF) and the Faculty of Medicine, Lund University, Sweden.
Disclosure
This study had no financial competing interests. Dr Ali Kiadaliri reports personal fees from Joint Academy, outside the submitted work. Professor Martin Englund reports grants from Swedish Research Council, Governmental Funding of Clinical Research within National Health Service (ALF), The Swedish Rheumatism Association, Österlund Foundation, and Gustav V’s 80-year Birthday Foundation, during the conduct of the study. The authors declare that they have no other conflicts of interest.
References
1. Long H, Liu Q, Yin H, et al. Prevalence trends of site-specific osteoarthritis from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Arthritis Rheumatol. 2022;74(7):1172–1183. doi:10.1002/art.42089
2. Hunter DJ, March L, Chew M. Osteoarthritis in 2020 and beyond: a lancet commission. Lancet. 2020;396(10264):1711–1712. doi:10.1016/s0140-6736(20)32230-3
3. Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–1589. doi:10.1016/j.joca.2019.06.011
4. Katz JN, Arant KR, Loeser RF. Diagnosis and treatment of hip and knee osteoarthritis: a review. JAMA. 2021;325(6):568–578. doi:10.1001/jama.2020.22171
5. Gore M, Tai KS, Sadosky A, Leslie D, Stacey BR. Use and costs of prescription medications and alternative treatments in patients with osteoarthritis and chronic low back pain in community-based settings. Pain Pract. 2012;12(7):550–560. doi:10.1111/j.1533-2500.2012.00532.x
6. Adams RJ, Appleton SL, Gill TK, Taylor AW, Wilson DH, Hill CL. Cause for concern in the use of non-steroidal anti-inflammatory medications in the community-a population-based study. BMC Fam Pract. 2011;12(1):70. doi:10.1186/1471-2296-12-70
7. Kingsbury SR, Gross HJ, Isherwood G, Conaghan PG. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatology. 2014;53(5):937–947. doi:10.1093/rheumatology/ket463
8. Duong M, Salvo F, Pariente A, et al. Usage patterns of ‘over-the-counter’ vs. prescription-strength nonsteroidal anti-inflammatory drugs in France. Br J Clin Pharmacol. 2014;77(5):887–895. doi:10.1111/bcp.12239
9. Jonsson T, Eek F, Dell’Isola A, Dahlberg LE, Ekvall Hansson E. The better management of patients with osteoarthritis program: outcomes after evidence-based education and exercise delivered nationwide in Sweden. PLoS One. 2019;14(9):e0222657. doi:10.1371/journal.pone.0222657
10. von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–808. doi:10.1136/bmj.39335.541782.AD
11. The National Board of Health and Welfare. Nationella riktlinjer för rörelseorganens sjukdomar 2012 [Elektroniska resurser]: Osteoporos, artros, inflammatorisk ryggsjukdom och ankyloserande spondylit, psoriasisartrit och reumatoid artrit: Stöd för styrning och ledning [National guidelines for musculoskeletal diseases 2012 [Electronic resources]: Osteoporosis, osteoarthritis, inflammatory back disease and ankylosing spondylitis, psoriatic arthritis and rheumatoid arthritis: Support for governance and management]. Socialstyrelsen; 2012.
12. Dell’Isola A, Turkiewicz A, Jönsson T, Rolfson O, Dahlberg L, Englund M. The role of pain and walking difficulties in shaping willingness to undergo joint surgery for osteoarthritis: data from the Swedish BOA register. Osteoarthr Cartil Open. 2021;3(2):100157. doi:10.1016/j.ocarto.2021.100157
13. Dell’Isola A, Jonsson T, Ranstam J, Dahlberg LE, Ekvall Hansson E. Education, home exercise, and supervised exercise for people with hip and knee osteoarthritis as part of a nationwide implementation program: data from the better management of patients with osteoarthritis registry. Arthritis Care Res. 2020;72(2):201–207. doi:10.1002/acr.24033
14. Dell’Isola A, Jonsson T, Nero H, Eek F, Dahlberg L. Factors associated with the outcome of a first-line intervention for patients with hip or knee osteoarthritis or both: data from the BOA register. Phys Ther. 2020;100(10):1771–1781. doi:10.1093/ptj/pzaa113
15. World Health Organization, Regional Office for E, European Observatory on Health S, Policies; et al. Health systems in transition: Sweden. Health Syst Transit. 2005;7(4):1.
16. Hakonsen H, Wangberg M, Alani D, Hedenrud T. Generic versus brand-name over-the-counter analgesics: knowledge and attitudes among Swedish pharmacy customers. J Pharm Policy Pract. 2020;13(1):60. doi:10.1186/s40545-020-00269-5
17. Dell’Isola A, Turkiewicz A, Zhang W, et al. Does osteoarthritis modify the association between NSAID use and risk of comorbidities and adverse events? Osteoarthr Cartil Open. 2022;4(2):100253. doi:10.1016/j.ocarto.2022.100253
18. Seed P. DIAGT: stata module to report summary statistics for diagnostic tests compared to true disease status; 2010.
19. Knoop J, van Tunen J, van der Esch M, et al. Analgesic use in patients with knee and/or hip osteoarthritis referred to an outpatient center: a cross-sectional study within the Amsterdam osteoarthritis cohort. Rheumatol Int. 2017;37(10):1747–1755. doi:10.1007/s00296-017-3785-3
20. Roos EM, Gronne DT, Skou ST, et al. Immediate outcomes following the GLA:D(R) program in Denmark, Canada and Australia. A longitudinal analysis including 28,370 patients with symptomatic knee or Hip osteoarthritis. Osteoarthritis Cartilage. 2021;29(4):502–506. doi:10.1016/j.joca.2020.12.024
21. Selcuk H, Roos EM, Gronne DT, Ernst MT, Skou ST. Agreement between self-reported information and administrative data on comorbidities, imaging and treatment in Denmark - a validation study of 38,745 patients with knee or hip osteoarthritis. Clin Epidemiol. 2021;13:779–790. doi:10.2147/CLEP.S309364
22. Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. perspective. Front Public Health. 2017;2017:5. doi:10.3389/fpubh.2017.00307
23. Kingsbury SR, Hensor EM, Walsh CA, Hochberg MC, Conaghan PG. How do people with knee osteoarthritis use osteoarthritis pain medications and does this change over time? Data from the osteoarthritis initiative. Arthritis Res Ther. 2013;15(5):R106. doi:10.1186/ar4286
24. Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage. 2010;18(4):476–499. doi:10.1016/j.joca.2010.01.013
25. Warner TD, Mitchell JA. COX-2 selectivity alone does not define the cardiovascular risks associated with non-steroidal anti-inflammatory drugs. Lancet. 2008;371(9608):270–273. doi:10.1016/s0140-6736(08)60137-3
26. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthritis Cartilage. 2013;21(9):1145–1153. doi:10.1016/j.joca.2013.03.018
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
