Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Identification of Bonding Difficulties in the Peripartum Period Using the Mother-to-Infant Bonding Scale-Japanese Version and Its Tentative Cutoff Points
Authors Hashijiri K , Watanabe Y , Fukui N, Motegi T, Ogawa M, Egawa J, Enomoto T , Someya T
Received 30 August 2021
Accepted for publication 9 November 2021
Published 20 November 2021 Volume 2021:17 Pages 3407—3413
DOI https://doi.org/10.2147/NDT.S336819
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Taro Kishi
Koyo Hashijiri,1 Yuichiro Watanabe,1 Naoki Fukui,1 Takaharu Motegi,1 Maki Ogawa,1 Jun Egawa,1 Takayuki Enomoto,2 Toshiyuki Someya1
1Department of Psychiatry, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan; 2Department of Obstetrics and Gynecology, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan
Correspondence: Yuichiro Watanabe Email [email protected]
Purpose: Identification of pregnant women with bonding difficulties is important to provide early intervention. However, few studies have examined the utility of self-report questionnaires that assess mother–infant bonding as screening tools for bonding difficulties. This longitudinal study aimed to identify pregnant women with bonding difficulties using the Japanese version of the Mother-to-Infant Bonding Scale (MIBS-J) and to estimate its optimal cutoff points in the peripartum period.
Patients and Methods: A total of 1301 pregnant women completed the MIBS-J and Hospital Anxiety and Depression Scale (HADS) at three time points: first trimester (T1; approximately 12– 15 weeks gestation), third trimester (T2; approximately 30– 34 weeks gestation), and postpartum (T3; approximately 4 weeks postpartum). A two-step cluster analysis was conducted to classify pregnant women based on their MIBS-J subscale scores at the three time points. Based on the cluster analysis results, receiver operating characteristic curve analysis was performed to estimate the optimal cutoff scores for the MIBS-J total score at each time point.
Results: The two-step cluster analysis produced two clusters: Cluster 1 (n = 824) and Cluster 2 (n = 477). Both the MIBS-J and HADS scores were significantly higher in Cluster 2 than in Cluster 1 at all time points. The MIBS-J tentative cutoff points were 3/4, 3/4, and 2/3 at T1, T2, and T3, respectively.
Conclusion: We identified two distinct groups across the perinatal period: pregnant women with bonding difficulties and pregnant women with normal bonding. Our findings suggest the usefulness of the MIBS-J as a screening tool to identify bonding difficulties during pregnancy.
Keywords: bonding difficulties, cluster analysis, HADS, MIBS-J, ROC analysis
Introduction
Bonding disorder is characterized by lack of affection and negative feelings of parents for their children.1 Brockington et al2 have defined bonding disorder as mild disorder (a delay in, or loss of, maternal emotional response), infant-focused anxiety, pathological anger, and rejection. Systematic reviews have indicated that maternal depression is negatively associated with bonding.3,4 In addition, bonding difficulties may predict neonatal emotional abuse.5 Therefore, it is important to identify mothers with bonding difficulties to improve maternal mental health and prevent child maltreatment.
Several observer-rated measures and self-report questionnaires have been developed to assess parent–infant bonding during the antenatal and postnatal periods.6 However, there are no established diagnostic criteria for bonding disorder. Therefore, it is difficult to demonstrate the utility of self-report questionnaires as screening tools for bonding disorder using observer-rated measures as gold standards.
The Mother-to-Infant Bonding Scale (MIBS) is a self-report questionnaire that evaluates the feelings of mothers toward their infants.7 The MIBS is an eight-item questionnaire that was adapted from the Mother-to-Infant Bonding Questionnaire (MIBQ).8 The original MIBQ was a 9-item questionnaire that was later revised to comprise 10 items. The Japanese version of the MIBS (MIBS-J)9 is a 10-item questionnaire based on the modified MIBQ. Although these scales have been widely used, few studies have examined their utility as screening tools for bonding difficulties. In a French study, 78 mothers completed the MIBS 48 hours after delivery and were interviewed 24 hours later.10 The semi-structured interview identified 10 mothers with bonding difficulties, and receiver operating characteristic (ROC) curve analysis found an optimal cutoff point for the MIBS total score of 1/2.10 A study of 723 Japanese mothers identified two clusters (normal and pathological maternal bonding) using a two-step cluster analysis based on the MIBS-J subscale scores at 5 days and 1 month after childbirth.11 In addition, a ROC analysis identified tentative optimal cutoff points for the MIBS-J total score of 3/4 and 4/5 at 5 days and 1 month after childbirth, respectively.11 Although the MIBS-J cutoff score of 4/5 was at 1 month after childbirth, some studies have used this cutoff score at different time points, reporting a prevalence of bonding difficulties of 8.6% at 4 months postpartum12 and 9.8–13.8% at 1 year after childbirth.13 Further studies are needed to determine the optimal cutoff score for the MIBS-J at each time point.
The identification of bonding difficulties during pregnancy is important to provide early interventions for mothers. One systematic review reported evidence for an association between prenatal and postnatal bonding quality.4 Recently, we also confirmed that bonding during pregnancy predicts postpartum bonding using MIBS-J data for 1301 Japanese pregnant women.14
Using these data, we aimed in this study to identify pregnant women with bonding difficulties and to estimate the optimal cutoff score for the MIBS-J. First, we performed a two-step cluster analysis to classify 1301 pregnant women according to the MIBS-J subscale scores at three time points: the first and third trimesters and 1 month postpartum. Subsequently, we estimated the optimal cutoff points for the MIBS-J total score at each time point.
Materials and Methods
Ethics Statement
Study procedures were carried out in accordance with the principles of the Declaration of Helsinki and were approved by the ethics committee of Niigata University (approval number: 2016–0019) and the ethics committees of the participating obstetric institutions. All participants provided written informed consent.
Participants
This study was part of the Perinatal Mental Health Research Project.14–18 In this study, we conducted a large-scale questionnaire survey in cooperation with the Department of Obstetrics and Gynecology, the Niigata University Medical and Dental Hospital, and 33 associated obstetric institutions in Niigata Prefecture, Japan, between March 2017 and March 2021. We recruited pregnant women, as previously described.14–18 In brief, we included pregnant Japanese women aged 18 years or older and excluded those with serious physical complications, serious pregnancy complications, or severe psychiatric disorders (eg, severe schizophrenia or severe depression).
Participants self-completed the MIBS-J and the Hospital Anxiety and Depression Scale (HADS) at three time points: the first trimester (T1; approximately 12–15 weeks gestation), the third trimester (T2; approximately 30–34 weeks gestation), and postpartum (T3; 4 weeks after childbirth). These participants were the same as in our previous study, which showed that perceived negative parenting before adolescence has direct effects and indirect effects (via anxiety and depression) on maternal–infant bonding in the perinatal period.14
Measurements
The MIBS-J consists of 10 items scored on a 4-point Likert scale (0–3; Supplementary Table 1).9 The total score ranges from 0 to 30; higher scores indicate poorer bonding. The MIBS-J has been validated in a previous study.9 Our previous study showed that the MIBS-J has a two-factor structure, “anger and rejection” (items 3, 5, and 9) and “lack of affection” (items 1, 4, 6, 8, and 10), and weak measurement invariance across the peripartum period.18 Therefore, we used these two MIBS-J subscale scores in a cluster analysis.
The HADS is a self-report questionnaire designed to assess anxiety and depression in non-psychiatric clinic settings.19 The HADS consists of 14 items scored on a 4-point Likert scale (0–3). The total score ranges from 0 to 42; higher scores indicate more severe anxiety and depressive symptoms. Because the HADS does not include physical symptoms such as nausea or anorexia, it can be used to accurately assess anxiety and depression in pregnant women experiencing hyperemesis gravidarum. In this study, we used the Japanese version of the HADS,20 which has been validated in a previous study.21
Statistical Analysis
First, we performed a two-step cluster analysis using the two MIBS-J subscale scores18 at three time points to classify the pregnant women. We compared the clusters on mean age and mean MIBS-J and HADS total scores at each time point using t-tests. We divided parity into two categories (primiparas and multiparas) and compared the ratio of these categories between clusters using the chi-square test.
Second, we carried out ROC analysis based on the two clusters identified in the two-step cluster analysis. A ROC curve was drawn based on the MIBS-J total score at each time point, and the area under the curve (AUC) was measured to evaluate the performance of the MIBS-J. We then estimated the optimal MIBS-J total score cutoff point at each time point using the maximum value of the Youden index22 (ie the sum of the sensitivity and specificity minus one).
We conducted statistical analyses using the Statistical Package for the Social Sciences (SPSS) version 25 (IBM Japan, Tokyo, Japan). The level of significance was set at p < 0.0063 following Bonferroni correction for eight statistical tests.
Results
The study participants were 1301 pregnant women (552 primiparas and 749 multiparas, mean age 31.5 [standard deviation 4.7] years). The two-step cluster analysis produced two clusters: Cluster 1 (n = 824) and Cluster 2 (n = 477; Table 1). The MIBS-J scores were significantly higher in Cluster 2 than in Cluster 1 at T1 (2.5 [2.1] vs 6.3 [3.2]), T2 (1.8 [1.6] vs 5.2 [2.7]), and T3 (1.0 [1.2] vs 3.8 [3.1]). The HADS scores were also significantly higher in Cluster 2 than in Cluster 1 at T1 (11.4 [5.4] vs 14.3 [5.9]), T2 (10.2 [5.3] vs 13.5 [5.9]), and T3 (9.8 [5.7] vs 13.9 [6.7]). There was no significant difference in age (31.7 [4.9] years vs 32.3 [4.5] years) and the ratio of primiparas (40.1% vs 45.2%) between the two clusters after the Bonferroni correction.
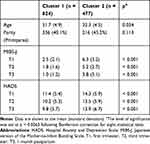 |
Table 1 Characteristics of the Two Clusters |
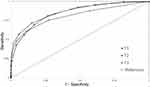
The AUCs of the ROC curve for the MIBS-J score at T1, T2, and T3 were 0.849, 0.862, and 0.810, respectively (Figure 1). The cutoff points of the MIBS-J for the maximum Youden index were 3/4 with 81.3% sensitivity and 73.3% specificity at T1 (Supplementary Table 2), 3/4 with 71.7% sensitivity and 84.8% specificity at T2 (Supplementary Table 3), and 2/3 with 61.2% sensitivity and 88.7% specificity at T3 (Supplementary Table 4).
Of 608 pregnant women who were positive according to the cutoff point at T1, 380 were positive at T2 and 216 of these were positive at T3 (Table 2). Of 693 pregnant women who were negative at T1, 606 were negative at T2, and 524 of these were negative at T3.
 |
Table 2 Number of Participants in Clusters 1 and 2 Who Were Positive or Negative According to the MIBS-J Cutoff Points |
Discussion
The two-step cluster analysis based on the MIBS-J subscale scores divided the 1301 pregnant Japanese women into two clusters. Clusters 1 and 2 were regarded as normal bonding and bonding difficulties, respectively. Pregnant women with bonding difficulties exhibited more severe anxiety and depressive symptoms than those with normal bonding. These results are in line with those of a previous study.11 Two clusters (normal and pathological maternal bonding) were identified based on the MIBS-J subscale scores of 723 Japanese mothers, and postpartum depressive symptoms were more severe in the pathological maternal bonding cluster than in the normal bonding cluster.11 Taken together, these findings suggest the existence of a group of pregnant women with bonding difficulties across the peripartum period distinctive from pregnant women with normal bonding.
In the present study, 477 of 1301 (36.7%) pregnant women were classified into the bonding difficulties cluster. The ROC analysis demonstrated MIBS-J cutoff values of 3/4 in the first trimester, 3/4 in the third trimester, and 2/3 at 1 month postpartum. In a previous study, 104 of 723 (14.4%) mothers were identified as part of a pathological maternal bonding cluster, and the cutoff values were 3/4 and 4/5 at 5 days and 1 month postpartum, respectively.11 There are several possible explanations for the inconsistency in findings between these two studies. First, our study population may be more representative than the previous study population of the general population of pregnant Japanese women. We recruited participants from 34 obstetric institutions in Niigata Prefecture, whereas the previous study was conducted in one general hospital and four antenatal clinics in Okayama Prefecture.11 The mean MIBS-J total score at 1 month postpartum was higher in the previous study (2.8 [2.5]) than in our study (2.0 [2.5]). In the previous study, 148 of 723 women (20.5%) were positive according to the cutoff point of 4/5 at 1 month postpartum.11 If we used the same cutoff point, 176 of 1301 women (13.5%) would be positive. Second, we used MIBS-J data from three time points during the antenatal and postnatal periods for the cluster analysis, whereas Matsunaga et al11 used data from two time points after childbirth. In general, bonding improves over time in the peripartum period.23,24 Indeed, the MIBS-J total score gradually decreased from T1 (3.9 [3.1]) to T3 (2.0 [2.5]) in the present study. Third, the two studies used different MIBS-J subscale items. We used scores from two subscales, “anger and rejection” (items 3, 5, and 9) and “lack of affection” (items 1, 4, 6, 8, and 10), for the cluster analysis, because our previous study provided evidence for the MIBS-J factor structure and weak measurement invariance.18 In contrast, Matsunaga et al11 used scores from items 2, 3, 5, and 7 for “anger and rejection” and scores from items 1, 6, 8, and 10 for “lack of affection”.9 Therefore, further studies are needed to draw definitive conclusions about the optimal cutoff score for the MIBS-J.
The MIBS-J is widely used in Japan,9,11–18 and the Japanese Society of Psychiatry and Neurology and the Japanese Society of Obstetrics and Gynecology25 recommend that the MIBS-J is administered to pregnant women during antenatal and postnatal checkups. Matsunaga et al11 proposed that midwives follow mothers with MIBS-J scores of 4 or more at discharge from a gynecological ward until community health centers provide home visiting services. Bonding during pregnancy predicts postpartum bonding.4,14 Therefore, it is important to identify mothers with bonding difficulties during pregnancy to provide early intervention for them. In Japan, antenatal checkups are routinely conducted once every 4 weeks from 0 to 23 weeks gestation, once every 2 weeks from 24 to 35 weeks gestation, and once every week from 36 weeks gestation to childbirth. Women with bonding difficulties need to be identified during pregnancy to enable early intervention. In the present study, the sensitivity (61.2–81.3%) and specificity (73.3–88.7%) of the MIBS-J gradually decreased and increased, respectively, from T1 to T3. Of 608 pregnant women who were positive at T1, 388 (63.8%) had bonding difficulties. Women who were positive at T1 should be carefully followed up through antenatal checkups. If feasible, promotional interviews26 conducted by trained midwives should be provided for them. Of 380 pregnant women who were positive at both T1 and T2, 306 (80.5%) had bonding difficulties. The AUCs of the MIBS-J at T1 (0.849) and T2 (0.862) were higher than the AUC at T3 (0.810). These findings suggest that the MIBS-J may be a useful screening tool for bonding difficulties during pregnancy. Pregnant women who are positive at both T1 and T2 should be referred to and further evaluated by mental health professionals. A recent review has highlighted the potential effectiveness of some interventions for postpartum bonding in mothers at risk (eg, mothers with postpartum depression).27 However, methodological heterogeneity among studies makes it difficult to determine which interventions should be used in clinical practice. Further studies are needed to implement effective interventions for mothers with bonding difficulties. Most midwives and mental health professionals in Japan have not received sufficient training to address bonding difficulties; therefore, it is important to train these medical personnel to provide adequate interventions for mothers with bonding difficulties.
Our study has some limitations that should be considered. First, we assessed bonding using a self-report questionnaire (the MIBS-J). Therefore, we cannot objectively determine the prevalence of bonding disorder. However, there are no established diagnostic criteria for bonding disorder. Matsunaga et al11 reported that the pathological maternal bonding cluster had higher psychological abuse subscale scores on the Parent-Child Conflict Tactics Scale than the normal maternal bonding cluster. Data on abusive or neglectful behaviors of pregnant women were not available in the present study, and thus the obtained cutoff points are tentative. Second, the MIBS was originally developed to evaluate postpartum bonding.7,9 Although our previous study provided evidence for the two-factor structure and weak measurement invariance of the MIBS-J across the peripartum period,18 further studies are needed to confirm the reliability and validity of the MIBS-J in both the antenatal and postnatal periods, to assess bonding over time.
Conclusion
The cluster analysis identified a group of pregnant women with bonding difficulties across the peripartum period distinctive from pregnant women with normal bonding. The ROC analysis estimated MIBS-J tentative cutoff points of 3/4 at the first trimester, 3/4 at the third trimester, and 2/3 at 1 month postpartum. These findings suggest the usefulness of the MIBS-J as a screening tool for bonding difficulties during pregnancy.
Abbreviations
AUC, area under the curve; HADS, Hospital Anxiety and Depression Scale; MIBQ, Mother-to-Infant Bonding Questionnaire; MIBS, Mother-to-Infant Bonding Scale; ROC, receiver operating characteristic.
Acknowledgments
We are grateful to Professor Koji Nishijima, Dr. Koichi Takakuwa, Dr. Masayuki Yamaguchi, Dr. Kazufumi Haino, Dr. Takuro Sugai, Dr. Ryusuke Tsuboya, Ms. Rie Araki, and Ms. Setsuko Mitome for their cooperation in the initial stages of this study. The authors greatly appreciate the involvement of all participants and staff of the participating obstetric institutions: Kameda Daiichi Hospital, Niitsu Obstetrics and Gynecology Clinic, Tomita Obstetrics and Gynecology Clinic, Honda Ladies Clinic, Agano City Hospital, Chihara Clinic, Sekizuka Clinic, Hirohashi Obstetrics and Gynecology Clinic, Niigata Saiseikai Sanjo Hospital, Saiseikai Niigata Hospital, Itoigawa Sogo Hospital, Niigata Prefectural Tokamachi Hospital, Takeyama Hospital, Watanabe Kinen Clinic, Kashiwazaki General Hospital and Medical Center, Kido Hospital, Tachikawa Medical Center, Saintpaulia Women’s Clinic, Nagaoka Chuo General Hospital, Arakawa Ladies Clinic, Ueda Ladies Clinic, Uonuma Kikan Hospital, Murakami General Hospital, Sado General Hospital, Tokunaga Ladies Clinic, Nagaoka Red Cross Hospital, Niigata Prefectural Shibata Hospital, Ladies Clinic Ishiguro, Angel Mother Clinic, Joetsu General Hospital, Niigata City General Hospital, Ojiya General Hospital, Watanabe Clinic, and Niigata University Medical and Dental Hospital. We thank Diane Williams, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
This work was supported by Grants-in-Aid for Scientific Research (20K23129 to KH and 19K08040 to NF) from the Japan Society for the Promotion of Science, by a grant from the Niigata Medical Association (to TM), and by a grant from the Medical Association of Niigata City (to MO).
Disclosure
Toshiyuki Someya reports grants and personal fees from Astellas Pharma Inc., Eli Lilly Japan K.K., Janssen Pharmaceutical K.K., Mitsubishi Tanabe Pharma Co., Mochida Pharmaceutical Co., Ltd., MSD K.K., Novartis Pharma K.K., Otsuka Pharmaceutical Co., Ltd., Shionogi Co., Ltd., and Sumitomo Dainippon Pharma Co., Ltd. outside the submitted work. The authors report no other potential conflicts of interest in this work.
References
1. Brockington I. Emotional rejection of the infant: status of the concept. Psychopathology. 2016;49(4):247–260. doi:10.1159/0004483342
2. Brockington IF, Aucamp HM, Fraser C. Severe disorders of the mother-infant relationship: definitions and frequency. Arch Womens Ment Health. 2006;9(5):243–251. doi:10.1007/s00737-006-0133-0
3. McNamara J, Townsend ML, Herbert JS. A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PLoS One. 2019;14(7):e0220032. doi:10.1371/journal.pone.0220032
4. Tichelman E, Westerneng M, Witteveen AB, et al. Correlates of prenatal and postnatal mother-to-infant bonding quality: a systematic review. PLoS One. 2019;14(9):1–15. doi:10.1371/journal.pone.0222998
5. Ohashi Y, Sakanashi K, Tanaka T, et al. Mother-to-infant bonding disorder, but not depression, 5 days after delivery is a risk factor for neonate emotional abuse: a study in Japanese mothers of 1-month olds. Open Fam Stud J. 2017;8(1):27–36. doi:10.2174/1874922401608010027
6. Wittkowski A, Vatter S, Muhinyi A, et al. Measuring bonding or attachment in the parent-infant-relationship: a systematic review of parent-report assessment measures, their psychometric properties and clinical utility. Clin Psychol Rev. 2020;82:101906. doi:10.1016/j.cpr.2020.101906
7. Taylor A, Atkins R, Kumar R, et al. A new mother-to-infant bonding scale: links with early maternal mood. Arch Womens Ment Health. 2005;8(1):45–51. doi:10.1007/s00737-005-0074-z
8. Kumar RC. “Anybody’s child”: severe disorders of mother-to-infant bonding. Br J Psychiatry. 1997;171:175–181. doi:10.1192/bjp.171.2.175
9. Yoshida K, Yamashita H, Conroy S, et al. A Japanese version of mother-to-infant bonding scale: factor structure, longitudinal changes and links with maternal mood during the early postnatal period in Japanese mothers. Arch Womens Ment Health. 2012;15(5):343–352. doi:10.1007/s00737-012-0291-1
10. Bienfait M, Maury M, Haquet A, et al. Pertinence of the self-report mother-to-infant bonding scale in the neonatal unit of a maternity ward. Early Hum Dev. 2011;87(4):281–287. doi:10.1016/j.earlhumdev.2011.01.031
11. Matsunaga A, Takauma F, Tada K, et al. Discrete category of mother-to-infant bonding disorder and its identification by the mother-to-infant bonding scale: a study in Japanese mothers of a 1-month-old. Early Hum Dev. 2017;111:1–5. doi:10.1016/j.earlhumdev.2017.04.008
12. Sampei M, Fujiwara T. Association of infertility treatment with perception of infant crying, bonding impairment and abusive behavior towards one’s infant: a propensity-score matched analysis. Int J Environ Res Public Health. 2020;17(17):6099. doi:10.3390/ijerph17176099
13. Tsuchiya S, Tsuchiya M, Momma H, et al. Association of cleft lip and palate on mother-to-infant bonding: a cross-sectional study in the Japan Environment and Children’s Study (JECS). BMC Pediatr. 2019;19(1):505. doi:10.1186/s12887-019-1877-9
14. Fukui N, Motegi T, Watanabe Y, et al. Perceived parenting before adolescence and parity have direct and indirect effects via depression and anxiety on maternal-infant bonding in the perinatal period. Psychiatry Clin Neurosci. 2021;75(10):312–317. doi:10.1111/pcn.13289
15. Fukui N, Motegi T, Watanabe Y, et al. Exclusive breastfeeding is not associated with maternal-infant bonding in early postpartum, considering depression, anxiety, and parity. Nutrients. 2021;13(4):1184. doi:10.3390/nu13041184
16. Ogawa M, Watanabe Y, Motegi T, et al. Factor structure and measurement invariance of the hospital anxiety and depression scale across the peripartum period among pregnant Japanese women. Neuropsychiatr Dis Treat. 2021;17:221–227. doi:10.2147/NDT.S294918
17. Motegi T, Watanabe Y, Fukui N, et al. Depression, anxiety and primiparity are negatively associated with mother–infant bonding in Japanese mothers. Neuropsychiatr Dis Treat. 2020;16:3117–3122. doi:10.2147/NDT.S287036
18. Motegi T, Fukui N, Hashijiri K, et al. Identifying the factor structure of the mother-to-infant bonding scale for post-partum women and examining its consistency during pregnancy. Psychiatry Clin Neurosci. 2019;73(10):661–662. doi:10.1111/pcn.12920
19. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
20. Kitamura T. Hospital anxiety and depression scale. Arch Psychiatr Diagn Clin Eval. 1993;4:371–372.
21. Kugaya A, Akechi T, Okuyama T, et al. Screening for psychological distress in Japanese cancer patients. Jpn J Clin Oncol. 1998;28(5):333–338. doi:10.1093/jjco/28.5.333
22. Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3(1):32–35. doi:10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3
23. Ohara M, Okada T, Kubota C, et al. Validation and factor analysis of mother-infant bonding questionnaire in pregnant and postpartum women in Japan. BMC Psychiatry. 2016;16:212. doi:10.1186/s12888-016-0933-3
24. Rossen L, Hutchinson D, Wilson J, et al. Maternal bonding through pregnancy and postnatal: findings from an Australian longitudinal study. Am J Perinatol. 2017;34(8):808–817. doi:10.1055/s-0037-1599052
25. Clinical guide for women with mental health problems during perinatal period. Details v1.1 [homepage on the Internet]. The Japanese Society of Psychiatry and Neurology and the Japanese Society of Obstetrics and Gynecology. Available from: https://www.jspn.or.jp/uploads/uploads/files/activity/Clinical_guide_for_women_with_mental_health_problems_during_perinatal_period_details_ver1.1.pdf.
26. Puura K, Davis H, Papadopoulou K, et al. The European early promotion project: a new primary health care service to promote children’s mental health. Infant Ment Health J. 2002;23(6):606–624. doi:10.1002/IMHJ.10039
27. Mascheroni E, Ionio C. The efficacy of interventions aimed at improving post-partum bonding: a review of interventions addressing parent-infant bonding in healthy and at risk populations. J Neonatal Nurs. 2019;25(2):61–68. doi:10.1016/j.jnn.2018.09.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.