Back to Journals » Infection and Drug Resistance » Volume 16
Identification of Bacterial Uropathogen and Antimicrobial Resistance Patterns Among Patients with Diabetic and Hypertension Attending Dilla University General Hospital, Dilla, Ethiopia
Authors Diriba K , Awulachew E, Bizuneh B
Received 9 May 2023
Accepted for publication 11 July 2023
Published 17 July 2023 Volume 2023:16 Pages 4621—4633
DOI https://doi.org/10.2147/IDR.S417033
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Kuma Diriba,1 Ephrem Awulachew,1 Bereket Bizuneh2
1Department of Medical Laboratory Sciences, Health Science and Medical CollegeDilla University, Dilla, Ethiopia; 2School of Medicine, Health Science and Medical College, Dilla University, Dilla, Ethiopia
Correspondence: Kuma Diriba, Tel +251913384550, Email [email protected]; [email protected]
Background: Having a urinary tract infection (UTI) is a serious health issue which is caused by microbial colonization and proliferation in the urinary system. Patients with diabetes and blood pressure are more vulnerable to bacterial urinary tract infections because their host defense is compromised and their urine has a high glucose content. A proper and quick investigation of uropathogen and their antibiogram is key to patient treatment and infection control.
Objective: Aimed to assess the identification of bacterial uropathogen and antimicrobial resistance patterns among diabetic and hypertension patients attending DUGH, Ethiopia.
Methods: A Facility-based cross-sectional study was conducted from February to December 2022 among 158 diabetic and hypertensive patients using a clean catch mid-stream urine sample. Pretested structured questionnaires were used to collect data from study participants. Urine samples were taken and cultured on Blood agar, MacConkey agar and CLED Agar for the identification of uropathogen. An antimicrobial susceptibility test was done according to CLSI. Binary and multiple logistic regression were used to assess the association. A P-value less than 0.05 was considered statistically significant.
Results: The overall prevalence of bacterial uropathogenic among diabetes mellitus and hypertension patients was 15.2%. E. coli (29.2%), coagulase negative Staphylococci (CoNS) (20.8%), K. pneumoniae 3 (12.5%) and S. aureus 2 (12.5%) were the leading isolated uropathogens. In our study, illiterates (AOR =8.1, 95% CI: (5.1– 12.4)), participants with high blood glucose levels (AOR=1.81, 95% CI: (1.01– 2.21)) and comorbid patients (AOR = 4.2, 95% CI: (4.1– 17.2)) were significantly associated with UTI. Both gram-negative and gram-positive isolated bacteria showed higher resistance to most of the commonly used antibiotics. Multidrug resistance was reported in 62.5% of the total isolates.
Conclusion: This study revealed a high prevalence of bacterial isolate and multidrug resistance. Therefore, continuous monitoring of microbiological and antimicrobial surveillance of UTI among DM patients is crucial for appropriate treatment and infection control.
Keywords: urinary tract infection, diabetes mellitus, hypertensive, uropathogens, prevalence, antimicrobial susceptibility pattern
Introduction
UTI is caused by microbial colonization and proliferation in the urinary system (UT).1,2 It may occur either because of the pathogenicity of the organism or the susceptibility of the host as bacteria transmit from the intestine to the urethra and start to grow to cause infection. UT is normally resistant to microbial development and colonization, which may be a result of a number of physiological mechanisms.3–5 Additionally, innate immunity, some antibody, protective secretion from mucous and prostate, barrier development, and over contents of urea protect microbial colonization and proliferation in the urinary system which causes UTI.4 Nevertheless, anatomical and physiological abnormalities that prevent urine from flowing normally6 and other factors that pass host immunity and resulted in UTI.7
As many research reports indicated, UT is the most frequent area for bacterial infection in humans.8 When microorganisms get a chance, UT can be affected by microbes, which develop virulence factors that allow them to overwhelm urinary epithelial cells. UTIs are caused by different microorganisms. Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis are the leading etiologic agent of UTIs which accounts for 75% of the isolates. Other Enterobacteriaceae species, enterococcus species and staphylococcus species also cause UTI. Antimicrobial resistance is becoming an important public health problem in patients with UTIs. The problem is challenging in low-income countries because of the high prevalence of infection, irrational uses of antibiotics and poor infection prevention practices.9,10
Globally, non-communicable illnesses are becoming a world threat as they cause high morbidity and mortality.11,12 Diabetes mellitus and hypertension are the most common non-communicable, organ or system disorder that persist for a long time. Numerous studies from throughout the world show that individuals with diabetes and hypertension are more likely to get urinary tract infections and that these infections are more severe and have dangerous consequences13–17 which may be due to host immune system abnormalities and a large concentration of glucose in the urine of those patients.3,18,19 These include granulocyte dysfunction and improved microbial adherence to the uroepithelial cells.20,21 Large glucose contents in urine promote bacterial growth and colonization in the UT22 and results in complications of renal function and lead to renal failure in these patients.23
Currently, the high prevalence of diabetes and hypertension throughout the world has become a major risk factor for UTI and is becoming a major economic burden on healthcare.17 Additionally, misuse of antibiotics for the treatment of UTIs contributes to the emergence of antibiotic-resistant uropathogens.24 There are no guidelines that separate treatment options among patients suffering from UTI who were with and without those NCDs.25 Moreover, the inappropriate use of antibiotics often results in the increased resistance of UT pathogens to the most commonly used antimicrobial drugs.26 Information about the etiologies of UTI and antimicrobial resistance among patients with diabetes and blood pressure is limited in the study area. Therefore, this study was undertaken to analyze the prevalence of bacterial etiologic agents, antimicrobial susceptibility patterns, and risk factors among patients with diabetes and hypertension in Dilla University Referral Hospital.
Methods
Study Design and Study Area
Facility-based cross-sectional study was applied between January 2022 and December 2022 by using Laboratory-based experimental tests for the isolation of etiologic agents and testing antimicrobial resistance patterns. The study was done in Gedeo Zone which is situated in Southern region of Ethiopia on patients with diabetics and hypertension. It is located at 365 kilometers from Addis Ababa (the capital city of the country). It is located in the Kola agro-ecological zone, 1400 kilometers above sea level, with an average annual temperature of 22 to 29 degree Celsius. According to the central statistical agency of Ethiopia’s 2007 census, Dilla had a total population of 61114 people, of which 31,329 were males and 29,785 were Females.
Study Population and Sampling Technique
The study population were patients with diabetic mellitus and hypertension cases visiting Dilla University General Hospital. All patients with confirmed diabetes mellitus and hypertension cases and those who signed informed consent were included in this study while patients without diabetic mellitus and hypertension cases and those patients with diabetics and hypertension cases who have been taking antibacterial drugs for the last two weeks were excluded from this study. Ethical approval was obtained from the institutional review board of Dilla University Medical and Health Science College with Unique protocol number duirb/012/22-01.
The sample size was calculated based on a single sample size estimation using the prevalence of 10.5% indicated in the study done in Ethiopia,27 with an expected margin of error taken at 5% and a confidence interval of 95% and 10% contingency for the non-respondent. The calculated sample size was 158. From a total of 502 diabetic and hypertension patients registered in the study area, 158 samples were drawn using a systematic random sampling technique.
Collection, Management, and Transportation of Specimens
Patients with diabetics and blood pressure were advised on how to collect the sample, a fresh midstream urine sample (5–10 mL) was collected in a sterile urine cup. Each specimen checked for its quality. Inappropriate samples contaminated with other materials like stool and soil were rejected. The urine sample was transported to Dill University Referral Hospital Microbiology Laboratory for organism identification and further analysis.
Isolation and Identification of Bacterial Uropathogen
Urine samples collected from patients were inoculated on Cysteine Lactose Electrolyte Deficient agar, MacConkey, and Blood agar plates (Oxoid, Ltd., Hampshire, England) using a sterile calibrated wire loop measuring 1 microliter. The inoculated plates were incubated aerobically for 24 hours at 35–37°C, and the results were classified as significant or non–significant. Significant bacteriuria was defined as culture plates containing 105 colony-forming units (CFU)/mL of a single bacterial species. Bacterial identification was done presumptively based on the appearance of bacteria on culture media, microscopic examination, and the gram-reaction. Gram-negative bacteria were further identified using indole production, citrate utilization, H2S formation, gas formation, urea hydrolysis, lysine decarboxylation, lactose fermentation, and motility. The mannitol fermentation test, catalase, and coagulase tests were utilized to identify gram-positive bacteria.
Antibiotic Susceptibility Testing (AST)
AST was performed for each identified bacterium using the standard Kirby-Bauer disk diffusion method on Muller Hinton agar (MHA) (Biomark Laboratories India) based on CLSI guidelines.28 The suspension was made by taking 3–5 colonies out of pure culture with an inoculation loop and was emulsified in nutrient broth and mixed gently. Until the suspension’s turbidity was corrected to 0.5 McFarland standards, it was incubated at 37°C. The organisms were evenly distributed across the surface of the MHA. The following drugs and concentrations were used to determine the antibiogram of the strains: Fourteen antibiotic disks were used and impregnated on the surface of the plate from the top antibiotics used in the study area. The drugs for disc diffusion testing were in the following concentrations: nitrofurantoin (30 μg), ciprofloxacin (15 μg), doxycycline (30μg), ampicillin (10μg), vancomycin (30μg), Trymethoprim-sulfamethoxazole (1.25/1.75 μg), gentamycin (10μg), penicillin (10 units), meropenem (10μg), ceftazidime (30μg), ceftriaxone (30μg) and amoxicillin-clavulanate (30μg). The antimicrobial selection was based on the recommendation of CLSI guidelines. The predefined antimicrobial disks were put on the MHA plate’s surface and incubated at 37°C for 18–24 hours and the clear region around the disc was measured to the nearest millimeter using a graduated caliper in millimeters, and the isolates were categorized as sensitive, intermediate, and resistant according to CLSI, 2016.29
Data Processing and Analysis
The laboratory request form was used to acquire demographic information and patient history. Data were entered and analyzed using Epi-Data 3.1 and the statistical package for social science version 23.0 software. Descriptive analysis such as frequency and mean was used. A P-value less than 0.05 was taken as statistically significant.
Result
Socio Demography of the Study Participants
A total of 158 diabetic and hypertension patients diagnosed with urinary tract infections were included in this study. Most of the study subjects were male 93 (58.9%), while female accounted 65 (41.1%) with male-to-female ratio of 1.43:1. The age of study participants ranged from 18 to 83 years with a mean age of 46.0+13.7 years. A 81.2% of study subjects were from urban areas. Most of the study participants have learned college and above. In the current study, more than half of the study participants were married (Table 1).
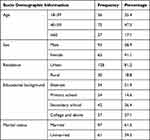 |
Table 1 Percentage of Socio-Demographic Data of Diabetic and Hypertensive Patients Diagnosed for UTIs in DUGH, South Ethiopia, 2022 |
Clinical Feature of the Study Participants
Among 158 study participants, 89 (56.4%) study participants were without symptoms of urinary tract infection while patients with urinary tract infection symptom accounted 69 (43.6%). The majority of participants were type II DM 132 (82.7%). Prior history of urinary tract infection and catheterization were found in 51 (32.3%) and 3 (1.8%) of study participants, respectively. Around 49 (30.1%) of the study participants were comorbid patients. Cardiovascular disease, rheumatoid arthritis, cancer, asthma and pyelonephritis are some of the comorbid diseases seen in study participants (Table 2).
 |
Table 2 Frequency of Clinical Feature of Diabetic Patients Diagnosed for UTIs in DUGH, South Ethiopia |
Prevalence of Bacterial Uropathogens
In the current study, the overall prevalence of uropathogens among DM and hypertension study participants was 24 (15.2%). From the total 24 uropathogens isolated, the female and male study participants accounted 16 (66.7%) and 8 (5.1%), respectively. From the total 24 uropathogens isolated, gram-negative and positive bacteria accounted 15 (62.5%) and 9 (37.5%) respectively. The isolated bacterial species were categorized into nine groups. E. coli 7 (29.2%) was found to be the leading bacterial isolates among gram-negative followed by K. pneumoniae 3 (12.5%) and Enterobacter species 2 (8.3%), while Coagulase negative staphylococcus (CoNS) 5 (20.8%) was the leading isolates followed by S. aureus 2 (12.5%) and Enterococcus species from gram-positive (4.2%) (Table 3).
 |
Table 3 Prevalence of Bacterial Isolates Among Different Age and Sex Groups in DURH, South Ethiopia, 2022 |
Antimicrobial Resistance Pattern Among Gram Negative and Positive Uropathogens
Gram-negative bacterial isolates which categorized into six groups were assessed for antimicrobial resistance patterns. Among the E. coli isolates, higher susceptibility was reported to nitrofurantoin, ceftriaxone, and meropenem each accounts 6 (85.7%) followed by ceftazidime and gentamicin each accounts for 5 (71.4%). It was highly resistant to ampicillin (100%) and doxycycline (85.7%). Likewise, a higher susceptibility to nitrofurantoin and meropenem each accounts 2 (66.7%) was reported to K. pneumoniae while it was highly resistant to ampicillin, ciprofloxacin, ceftazidime and doxycycline (100%). Enterobacter species, K. oxytoca, P. mirabilis and Citrobacter species showed high susceptibility to nitrofurantoin and ciprofloxacin (100%), but it was highly resistant to ampicillin (100%). Among gram-positive bacterial isolates, CoNS showed high susceptibility to vancomycin and nitrofurantoin ranging from 80% to 100% while it was high resistance to ampicillin (100%). On the other hand, among S. aureus isolated, high resistance was reported in ampicillin, Penicillin, Amoxicillin-clavulanic acid and ceftazidime ranged from 60% to 100%, but it was highly susceptible to vancomycin and nitrofurantoin ranging from 80% to 100%. Enterococcus species were highly resistant to ceftazidime and penicillin (100%), while it was highly susceptible to ciprofloxacin, nitrofurantoin, and ciprofloxacin (100%) (Table 4).
 |
Table 4 Antimicrobial Susceptibility Patterns of Gram Positive and Gram Negative Bacterial Isolate from Urine Sample at Dilla University Referral Hospital, from January 2022 to December 2022 |
Multidrug Resistance (MDR) Patterns of the Isolates
From the total 24 bacterial isolates, MDR (bacteria that are resistance to at least one in three or more categories of antibiotics) was reported in 16 (66.7%). Out of 15 gram-negative bacteria, 11 (73.3%) were MDR while 4 (44.4%) were MDR among 9 gram-negative bacteria. In this study, K. pneumoniae 3 (100%) followed by E. coli 4 (57.1%) and Enterobacter species 1 (50%) were reported as gram-negative bacteria with higher level of MDR, while S. aureus 2 (66.7%) followed by CoNS 2 (40%) were gram-positive bacteria with higher level of MDR (Table 5).
 |
Table 5 MDR Pattern of Gram Positive and Gram Negative Bacterial Isolate from Urine Sample at Dilla University Referral Hospital, from January 2022 to December 2022 |
Associated Risk Factors of Urinary Tract Infection
In our study, risk factors for urinary tract infections were assessed among twelve variables using bivariate analysis. In multivariate analysis, individuals who had no educational background (AOR =8.1, 95% CI: (5.1–12.4), p = 0.001), study subjects with high blood glucose level (AOR=1.81, 95% CI: (1.01–2.21), p = 0.01) and study subjects with additional disease (AOR = 4.2, 95% CI: (4.1–17.2), p = 0.001) were significantly associated with urinary tract infection (Table 6).
 |
Table 6 Bivariate and Multivariate Logistic Regression Analysis of Factors Associated with UTI Among Diabetic Patients (n=158) Attending in DUGH, Southern Ethiopia, 2022 |
Discussion
In the current study, the overall prevalence of uropathogens among DM and hypertension patients was 15.2%. It is in line with prior studies done in Harar30 (15.4%), Addis Ababa26 (14.9%), Gondar10 (17.8%), Metu, Ethiopia31 (16.7%) and Nekemte, Ethiopia32 (16.5%). However, our findings were disparately higher than studies done in London33 (5.7%), Iran34 (8.06%), Hawassa35 (13.8%), Romania36 (12.0%) and Debre Tabor14 (10.9%). However, this study was lower than studies done in Nepal19 (54.76%), Kuwait37 (35%), India38 (49.15%), and Uganda39 (22.0%). The variations might be explained by variation in location, lifestyle, personal hygiene practice, difference in sample size, study period variation and health education practices.
In our study, gram-negative uropathogens were commonly identified which account for around 62.5%. It includes E. coli, Klebsiella species, Enterobacter species, Proteus species, and Citrobacter species.31,40 Different studies conducted in Ethiopia and different parts of the world10,30,41–43 reported as they were the leading causative agents of UTI. In the current investigation, E. coli and Klebsiella pneumoniae were the two most prevalent bacterial isolates. This is in line with studies conducted in different areas of the world.19,30,32,35,41,42 The predominance of E. coli might be due to the existence of the bacteria as normal flora in fecal, which can easily rise through genitalia and results in UTI.35 E. coli has a number of virulent factors that assist the bacteria to easily colonize and invade the urinary epithelium and mediate the attachment of the bacteria to uroepithelial cells that contribute to UTI.44
In the present study, gram-positive staphylococcus species like CoNSs and S. aureus, and Enterococcus species, which play a lesser role in resulting UTI were also identified.45 Coagulase-negative staphylococcus and S aureus were the leading bacterial isolate with prevalence of 20.8% and 12.5%, respectively, followed by Enterococcus species (4.2%). Our finding was comparable with previous studies done in different parts of the country.26,35,37,46
In the current study, a large number of gram-negative enteric pathogens were extremely resistant to ampicillin and amoxicillin-clavulanic acid. Likewise, similar findings were reported high bacterial resistance to the medication in different parts of the country.26,32,35 Overuse/underuse or misuse of the drug, easy availability and cheap price of antibiotics, lack of current guidelines on the selection of medications, and a lack of diagnostic laboratory services for susceptibility tests are some of the factors that contribute to this. On the other hand, nitrofurantoin, meropenem, ceftriaxone and ceftazidime showed higher rates of sensitivity. This increased antibiotic resistance including multidrug resistance gram-negative bacterial isolates may be due to the habit of empirical use of drugs and lack of antimicrobial susceptibility testing. This leads to the onset of chronic renal disorder.47
Higher penicillin (56%), ceftazidime (75.6%), and ampicillin (100%) resistance was observed in gram-positive bacteria. This can be due to the accessibility and indiscriminate use of widely prescribed medications, which could result in a rise in resistance. On the other hand, greater than 80% of the examined gram-positive isolates exhibited nitrofurantoin, trymethoprim-sulfamethoxazole and vancomycin sensitivity. Likewise, similar studies reported the same finding in different parts of the country.26,35,40 According to our findings, trymethoprim-sulfamethoxazole, vancomycin, and nitrofurantoin are the most effective drugs for the empiric therapy of UTI, especially in study subjects with diabetic patients in the study area.
In our study, multiple drug resistance was reported in 16 (66.7%) bacterial isolates. This is comparable with the study conducted in Debre Tabor14 (56.7%), Gondar10 (59.8%) and Addis Ababa48 (71.7%). However, prior studies done in Harar30 (92.5%) and Hawassa35 (93.9%) reported higher prevalence of MDR. The discrepancy may result from differences in the time of study the kind and generation of antibiotics we used for susceptibility testing or differences in type and quantity of antibiotics used to define bacterial isolate as MDR or not or any combination of these factors. Multiple antibiotic resistant bacteria are increasing at high rate from time to time. Numerous factors have been identified as major contributors to the emergence of multidrug resistant strains, including the indiscriminate and prolonged use of a wide variety of antibiotics, a lack of infection control, an increase in the frequency and speed of travel, a lack of antibiotic susceptibility testing site, and the absence of updated guidelines on the selection of drugs.
In our study, most of the independent variables like age, sex, residence, educational status, marital status, previous UTL, history of catheterization, medication for diabetes, and hypertension had no significant association with identified uropathogens bacteria (P>0.05). This is comparable with studies conducted in different parts of the country.27,35,49 The current study showed that high blood glucose was positively correlated with urinary tract infections. Likewise, similar findings were reported in previous study conducted in Gondar.10 In contrast to our finding, studies conducted in Nigeria reported that there are no associations between urinary tract infection and blood glucose level.50 This may be due to the possibility that a single blood glucose reading does not accurately reflect glycemic management, which facilitates diabetic people to be more susceptible to UTIs. The increased prevalence of uropathogens in individuals with high blood sugar levels may be primarily attributable to a defective bladder’s inadequate contraction, which results in static urine pools and, in combination with glycosuria, produces an ideal habitat for bacterial growth.
In our study, illiterate study participants and patients with additional diseases had a significant association with uropathogens (higher odds of getting urinary tract infections compared with other study participants). This is the same as other studies conducted elsewhere which reported illiteracy as a risk factor for urinary tract infections. This might be due to a lower level of knowledge on how to protect their health, particularly their personal hygiene, and protect themselves from bacterial infection and the immune suppression of HIV in infected patients and also the effects of hypertension with kidney disease.32,51–54
Conclusion
The prevalence rate of bacterial isolates among uropathogens was high with predominance of isolates of E. coli, CoNS, and K. pneumoniae. Both gram-negative and positive were highly resistant to the commonly used antimicrobial agents. Moreover, high multidrug resistances were identified in both gram-negative and positive bacterial isolates. We identified a significant association between comorbid patients, illiterate patients, and patients with higher blood glucose levels and the presence of UTI among diabetic patients. For diabetes mellitus patients, health information should be disseminated regarding UTI, glycemic management, and drug usage habits. Patients with additional diseases and diabetics with blood glucose levels below 126 mg/dL should have their urinary tracts screened for infections. The therapy of urinary tract infections in diabetes mellitus patients should be supported by AST and urine culture test results. Additional research employing molecular techniques, such as genotypic characterization in ESBL-producing bacteria infecting diabetic patients’ urinary tracts in a larger sample size.
Data Sharing Statement
The corresponding author will provide the data set upon reasonable request, which was used for the analysis in the current work. All data relevant to the study are included in the article.
Ethical and Consent Statements
The Dilla University Health Research Ethics Review Committee authorized a protocol for patient recruitment and participation in the study that adhered to the Declaration of Helsinki and had the unique number duirb/012/2022-01. Each participant in the study received information about its purpose during the data collection process. Before beginning the data collection, each patient provided written consent. The clinical samples were gathered only for this study purpose. In order for patients to receive therapy based on the isolates’ drug susceptibility data, samples with positive culture results were shared with doctors. The Dilla University Medical and Health Science College’s Ethical Review Committee granted approval for the study. During the interview procedure, strict confidentiality was upheld, and anonymity was upheld during data processing and report writing. Participants in the study who had high levels of uropathogens were directed to their local medical center for the necessary therapies.
Acknowledgments
The Dilla University Research and Dissemination Office provided funds for this work, and the authors would like to thank the university for providing this opportunity for researchers to submit ideas for problem-solving projects and scientific inquiries. I thank all study participants for their cooperation during sample collection, as well as the employees of the laboratory department.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Dilla University Research and Dissemination Office.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Vasudevan R. Urinary tract infection: an overview of the infection and the associated risk factors. J Microbiol Exp. 2014;1(2):00008.
2. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–284. doi:10.1038/nrmicro3432
3. Worku GY, Abegaz WE. Prevalence of bacterial urinary tract infection and antimicrobial susceptibility patterns among diabetes mellitus patients attending Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Infect Drug Resist.2020;14:1441–1454.
4. Sussman P, Gally M, Phd DL. The biology of cystitis: host and bacterial factors. Annu Rev Med. 1999;50(1):149–158. doi:10.1146/annurev.med.50.1.149
5. Islam MA, Khan M, Basak P, Khanam M, Bhattacharyya P. Evaluation of liver function tests in type2 diabetic patients. J Teach Ass. 2016;29(1):21–23.
6. Hickling DR, Sun TT, Wu XR. Anatomy and physiology of the urinary tract: relation to host defense and microbial infection. In: Urinary Tract Infections: Molecular Pathogenesis and Clinical Management. Wiley Online Library; 2017:1–25.
7. Jatileni NJV, Maposa I, Mavenyengwa RT. A retrospective study of the variability in etiological agents of urinary tract infections among patients in Windhoek-Namibia. Open J Med Microbiol. 2015;5(04):184. doi:10.4236/ojmm.2015.54023
8. Pargavi B, Mekala T, Selvi AT, Moorthy K. Prevalence of urinary tract infection (UTI) among diabetics patients in Vandavasi, Tamil Nadu, India. Int J Biotechnol. 2011;2(2):42–45.
9. Beyene G, Tsegaye W. Bacterial uropathogens in urinary tract infection and antibiotic susceptibility pattern in Jimma university specialized hospital, southwest Ethiopia. Ethiop J Health Sci. 2011;21(2):141–146. doi:10.4314/ejhs.v21i2.69055
10. Yismaw G, Asrat D, Woldeamanuel Y, Unakal CG. Urinary tract infection: bacterial etiologies, drug resistance profile and associated risk factors in diabetic patients attending Gondar University Hospital, Gondar, Ethiopia. Eur J Experiment Biol. 2012;2(4):889–898.
11. Gizaw M, Harries A, Ade S, et al. Diabetes mellitus in Addis Ababa, Ethiopia: admissions, complications and outcomes in a large referral hospital. Public Health Action. 2015;5(1):74–78. doi:10.5588/pha.14.0107
12. Bloom DE, Cafiero E, Jané-Llopis E, et al. The global economic burden of noncommunicable diseases. Program on the Global Demography of Aging; 2012.
13. El-Nagar MM, Abd El-Salam AE, Gabr HM, Abd El EE. Prevalence of urinary tract infection in Damietta diabetic patients. Menoufia Med J. 2015;28(2):559. doi:10.4103/1110-2098.163918
14. Worku S, Derbie A, Sinishaw MA, Adem Y, Biadglegne F. Prevalence of bacteriuria and antimicrobial susceptibility patterns among diabetic and nondiabetic patients attending at Debre Tabor Hospital, Northwest Ethiopia. Int J Microbiol. 2017;2017:1–8. doi:10.1155/2017/5809494
15. Sasirekha R. A Study on Comparison of Different Phenotypic Methods for Detection of Extended Spectrum Beta Lactamase Production Among Enterobacteriaceae in Urinary Tract Infection in a Tertiary Care Centre. Madurai: Madurai Medical College; 2017.
16. Abubakar E-M-M. Antimicrobial susceptibility pattern of pathogenic bacteria causing urinary tract infections at the Specialist Hospital, Yola, Adamawa state, Nigeria. J Clinic Med Res. 2009;1(1):1–8.
17. Yu S, Fu AZ, Qiu Y, et al. Disease burden of urinary tract infections among type 2 diabetes mellitus patients in the US. J Diabetes Complications. 2014;28(5):621–626. doi:10.1016/j.jdiacomp.2014.03.012
18. Boyko EJ, Fihn SD, Scholes D, Chen C-L, Normand EH, Yarbro P. Diabetes and the risk of acute urinary tract infection among postmenopausal women. Diabetes Care. 2002;25(10):1778–1783. doi:10.2337/diacare.25.10.1778
19. Kumar Jha P, Baral R, Khanal B. Prevalence of uropathogens in diabetic patients and their susceptibility pattern at a tertiary care center in Nepal-a retrospective study. Int J Bio Lab Sci. 2014;3:29–34.
20. Abdul-Sahib KY. Study of ciprofloxacin resistant Escherichia coli (CREC) in type 2 diabetic patients with symptomatic urinary tract infections. IRAQI J Community Med. 2008;21(1):58–63.
21. Baqai R, Aziz M, Rasool G. Urinary tract infections in diabetic patients and biofilm formation of uropathogens. Infect Dis J Pak. 2008;17(1):21–24.
22. Longdoh NA, Assob JCN, Nsagha S, et al. Uropathogens from diabetic patients with asymptomatic bacteriuria and urinary tract infections. West Lond Med J. 2013;5(1):7–14.
23. Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: a review of pathogenesis. Indian J Endocrinol Metab. 2012;16(Suppl1):S27. doi:10.4103/2230-8210.94253
24. Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015;8:129. doi:10.2147/DMSO.S51792
25. Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinic Infect Dis. 2011;52(5):e103–e20. doi:10.1093/cid/ciq257
26. Woldemariam HK, Geleta DA, Tulu KD, et al. Common uropathogens and their antibiotic susceptibility pattern among diabetic patients. BMC Infect Dis. 2019;19(1):1–10. doi:10.1186/s12879-018-3669-5
27. Mohammed A, Beyene G, Teshager L. Urinary pathogenic bacterial profile, antibiogram of isolates and associated risk factors among diabetic patients in Hawassa town, southern Ethiopia: a cross-sectional study. Urol Nephrol Open Access J. 2020;8(4):84–91. doi:10.15406/unoaj.2020.08.00282
28. Wkler MA, Cockerill FR, Bush K, et al. Clinical and Laboratory Standard Institute: Performance Standards for Antimicrobial Disc susceptibility Tests; Approved Standard. Clinical and Laboratory Standard Institute; 2010.
29. Jorgensen JH, Turnidge JD. Susceptibility test methods: dilution and disk diffusion methods. In: Manual of Clinical Microbiology.
30. Abate D, Kabew G, Urgessa F, Meaza D. Bacterial etiologies, antimicrobial susceptibility patterns and associated risk factors of urinary tract infection among diabetic patients attending diabetic clinics in Harar, Eastern Ethiopia. East Afr J Health Biomed Sci. 2017;1(2):11–20.
31. Gutema T, Weldegebreal F, Marami D, Teklemariam Z. Prevalence, antimicrobial susceptibility pattern, and associated factors of urinary tract infections among adult diabetic patients at Metu Karl Heinz Referral Hospital, Southwest Ethiopia. Int J Microbiol. 2018;2018:1–7. doi:10.1155/2018/7591259
32. Kebamo S, Dabso R, Deressa A, Gebrie M. Urinary tract infection: bacterial etiologies, drug resistance profile and associated risk factors among diabetic patients attending Nekemte Referral Hospital, Ethiopia. Am J Curr Microbiol. 2017;5(1):19–31.
33. Evans J, McOwan A, Hillman R, Forster G. Incidence of symptomatic urinary tract infections in HIV seropositive patients and the use of cotrimoxazole as prophylaxis against Pneumocystis carinii pneumoniae. Sex Transm Infect. 1995;71(2):120–122. doi:10.1136/sti.71.2.120
34. Nashtar SB, Hashim I, Hamdan SJ. Assessment of antimicrobial susceptibility patterns in urine culture of patients with urinary tract infection attending Al-Kindy teaching hospital. Iraqi Med J. 2018;64(1):37–41.
35. Nigussie D, Amsalu A. Prevalence of uropathogen and their antibiotic resistance pattern among diabetic patients. Turk J Urol. 2017;43(1):85. doi:10.5152/tud.2016.86155
36. Chiţă T, Timar B, Muntean D, et al. Urinary tract infections in Romanian patients with diabetes: prevalence, etiology, and risk factors. Ther Clin Risk Manag. 2016;13:1–7. doi:10.2147/TCRM.S123226
37. Sewify M, Nair S, Warsame S, et al. Prevalence of urinary tract infection and antimicrobial susceptibility among diabetic patients with controlled and uncontrolled glycemia in Kuwait. J Diabetes Res. 2016;2016:1–7. doi:10.1155/2016/6573215
38. Sharma V, Gupta V, Mittal M. Prevalence of uropathogens in diabetic patients and their antimicrobial susceptibility pattern. Natl J Lab Med. 2012;1(1):26–28.
39. Nabaigwa BI, Mwambi B, Okiria J, Oyet C. Common uropathogens among diabetic patients with urinary tract infection at Jinja Regional Referral Hospital, Uganda. Afr J Lab Med. 2018;7(1):1. doi:10.4102/ajlm.v7i1.621
40. Mama M, Manilal A, Gezmu T, Kidanewold A, Gosa F, Gebresilasie A. Prevalence and associated factors of urinary tract infections among diabetic patients in Arba Minch Hospital, Arba Minch province, South Ethiopia. Turk J Urol. 2019;45(1):56. doi:10.5152/tud.2018.32855
41. Hamdan HZ, Kubbara E, Adam AM, Hassan OS, Suliman SO, Adam I. Urinary tract infections and antimicrobial sensitivity among diabetic patients at Khartoum, Sudan. Ann Clin Microbiol Antimicrob. 2015;14(1):1–6. doi:10.1186/s12941-015-0082-4
42. Pragash DS, Girija S, Sekar U, Rayapu V, Sheriff D. Uropathogens and diabetes mellitus-a perspective. IOSR J Dent Med Sci. 2017;16(5):29–32. doi:10.9790/0853-1605052932
43. Kumar D, Singh AK, Ali MR, Chander Y. Antimicrobial susceptibility profile of extended spectrum β-lactamase (ESBL) producing Escherichia coli from various clinical samples. Infect Dis. 2014;7:
44. Mulvey MA. Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol. 2002;4(5):257–271. doi:10.1046/j.1462-5822.2002.00193.x
45. Anejo-Okopi JA, Okojokwu OJ, Ramyil SM-C, et al. Bacterial and antibiotic susceptibility pattern of urinary tract infection isolated from asymptomatic and symptomatic diabetic patients attending tertiary hospital in Jos, Nigeria. Trends Med. 2017;17(1):1–5.
46. Bishu KG, Jenkins C, Yebyo HG, Atsbha M, Wubayehu T, Gebregziabher M. Diabetes in Ethiopia: a systematic review of prevalence, risk factors, complications, and cost. Obes Med. 2019;15:100132. doi:10.1016/j.obmed.2019.100132
47. Majeed HT, Aljanaby AAJ. Antibiotic susceptibility patterns and prevalence of some extended spectrum beta-lactamases genes in gram-negative bacteria isolated from patients infected with urinary tract infections in Al-Najaf City, Iraq. Avicenna J Med Biotechnol. 2019;11(2):192.
48. Yeshitela B, Gebre-Selassie S, Feleke Y. Asymptomatic bacteriuria and symptomatic urinary tract infections (UTI) in patients with diabetes mellitus in Tikur Anbessa Specialized University Hospital, Addis Ababa, Ethiopia. Ethiop Med J. 2012;50(3):239–249.
49. Alemu M, Belete MA, Gebreselassie S, Belay A, Gebretsadik D. Bacterial profiles and their associated factors of urinary tract infection and detection of extended spectrum beta-lactamase producing gram-negative uropathogens among patients with diabetes mellitus at Dessie referral hospital, northeastern Ethiopia. Diabetes Metab Syndr Obes. 2020;13:2935. doi:10.2147/DMSO.S262760
50. Alebiosu C, Osinupebi O, Olajubu F. Significant asymptomatic bacteriuria among Nigerian type 2 diabetics. J Natl Med Assoc. 2003;95(5):344.
51. Hall JE, Kuo JJ, da Silva AA, de Paula RB, Liu J, Tallam L. Obesity-associated hypertension and kidney disease. Curr Opin Nephrol Hypertens. 2003;12(2):195–200. doi:10.1097/00041552-200303000-00011
52. Haile Hantalo A, Haile Taassaw K, Solomon Bisetegen F, Woldeamanuel Mulate Y. Isolation and antibiotic susceptibility pattern of bacterial uropathogens and associated factors among adult people living with HIV/AIDS attending the HIV Center at Wolaita Sodo University Teaching Referral Hospital, South Ethiopia. HIV/AIDS Res Palliat Care. 2020;12:799–808. doi:10.2147/HIV.S244619
53. Alo M, Saidu A, Ugah U, Alhassan M. Prevalence and antibiogram of bacterial isolates causing urinary tract infections at Federal Teaching Hospital Abakaliki I (FETHA I). Br Microbiol Res J. 2015;8(2):403–417. doi:10.9734/BMRJ/2015/16696
54. Nayaju T, Upreti MK, Ghimire A, et al. Higher prevalence of ESBL producing uropathogenic Escherichia coli among Diabetic patients from a Tertiary Care Hospital of Kathmandu; 2020.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
