Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
HPV Vaccine Knowledge and Hesitancy Among Health Colleges’ Students at a Saudi University
Authors Aldawood E , Dabbagh D, Alharbi S, Alzamil L, Faqih L, Alshurafa HH, Dabbagh R
Received 26 September 2023
Accepted for publication 9 November 2023
Published 14 November 2023 Volume 2023:16 Pages 3465—3476
DOI https://doi.org/10.2147/JMDH.S438633
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Esraa Aldawood,1 Deemah Dabbagh,1 Sarah Alharbi,1 Lama Alzamil,1 Layla Faqih,1 Hassan H Alshurafa,2 Rufaidah Dabbagh3
1Department of Clinical Laboratory Science, College of Applied Medical Science, King Saud University, Riyadh, Kingdom of Saudi Arabia; 2College of Medicine, King Saud University, Riyadh, Saudi Arabia; 3Department of Family and Community Medicine, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Esraa Aldawood, Email [email protected]
Introduction: Human papillomavirus (HPV) infection is a widespread sexually transmitted infection linked to various types of cancer. Although vaccination against HPV is available, global HPV vaccination rates remain low.
Aim: This study aimed to evaluate the awareness and knowledge of the HPV vaccine and to identify predictors associated with vaccine hesitancy among health college students at King Saud University, Saudi Arabia.
Methods: A cross-sectional survey was distributed during December 2022 to students enrolled in health colleges. The survey link was randomly distributed via social media platforms and in-person interactions. The number of participants was 405 including both males and females. The data was analyzed using the Statistical Package for Social Sciences (SPSS). The correct response rate for all knowledge items was calculated, and they were stratified by gender and college. The association of vaccine hesitancy with sociodemographic characteristics was examined using logistic regression analysis.
Results: The study found that approximately half of the students (49.9%) were aware of the HPV vaccine. However, only a small percentage of students answered all to all HPV knowledge items correctly. Additionally, only a small proportion (5.2%) reported receiving the vaccine. The overall HPV vaccine hesitancy was 59.1% (43.9% for female and 75.9% for male). The most common reasons for vaccine hesitancy was not knowing enough about it. Males were two times more likely than females to believe that they did not need the HPV vaccine. The odds for HPV vaccine hesitancy were greater among males and younger age groups compared to females and older age groups.
Conclusion: This study underscores the importance of implementing university-wide interventions and educational campaigns to enhance awareness and knowledge of the HPV vaccine.
Keywords: HPV vaccine, vaccine awareness, vaccine hesitancy, college students
Introduction
Human papillomavirus (HPV) infection is the most common sexually transmitted infection worldwide.1 High-risk genotypes of HPV genotypes can cause various types of cancer, including almost nearly 100% of cervical cancers, 95% of anal cancers, 60% of penile cancers, 75% of vaginal cancers, 70% of vulvar cancers and 75% of oropharyngeal cancers.2–5 In Saudi Arabia, cervical cancer ranks as the 8th most common cancer and the 9th leading cause of cancer deaths.6 The data about HPV epidemiology in Saudi is not as comprehensive as in some other parts of the world, several studies have shed light on the prevalence of HPV among women in Saudi Arabia reported inconsistent rates with some suggesting the prevalence of HPV infection in Saudi Arabia is among the lowest in the world, with an estimated rate of 1.9 cases per 100000 women.7 While others have reported higher rates, indicating that the prevalence of HPV in Saudi women is comparatively significant.8,9 In a 10-year retrospective study conducted in Saudi Arabia in 2021, showed that 54.2% of cervical cancer cases tested positive for HPV.10
While specific national screening programs have not been consistently implemented in Saudi Arabia, cervical cancer screening practices have been evolving, with efforts to establish effective guidelines and protocols for detecting precancerous lesions and early-stage cervical cancer. The Pap test (Pap smear) remains the commonly used screening method in Saudi Arabia, with the recommended age for cervical cancer screening set at 21 years, aligning with international guidelines. The frequency of screening varies based on individual patients’ risk profiles and previous screening results.11
In 2006, the United States Food and Drug Administration (FDA) approved the first HPV vaccine to protect against HPV infection and related diseases such as genital warts and cervical cancer.12 And in 2018, the World Health Organization (WHO) launched a global strategy to eliminate cervical cancer by 2030 with one of its pillars being to ensure that 90% of girls are fully vaccinated with the HPV vaccine by the age of 15.13 Since the announcement, many countries have adapted vaccine strategies to achieve this goal. In 2010, Saudi Arabia approved the HPV vaccine, but it was not widely administered until 2017, when the Ministry of Health included it in the national immunization schedule at no cost for girls aged 11 or 12, with mainly targeted school campaigns.14 Although it should be mentioned that there is limited information on vaccine accessibility for adults in the country. Despite the efforts, the global vaccine coverage and uptake remain low, which hinders a great public health impact.6
In Saudi Arabia, the HPV vaccination coverage is unknown. However, several surveys have reported low HPV vaccination uptake. One study found that in 2020, only 2% of Saudi females received the HPV vaccine.7 Another recent study conducted in the Eastern Province to assess awareness and knowledge of the HPV vaccine among females and males found that only 4% of the participants had received the HPV vaccination.15 Additionally, a study conducted in Riyadh showed that a high percentage (89%) of Saudi parents had not received the HPV vaccine.16 Interestingly, a low HPV vaccine uptake (8.7%) was also reported among medical students.17
Various social, cultural, and economic factors are associated with the observed slow global uptake of the HPV vaccine.18,19 A recent study performed in Jazan province, Saudi Arabia, found that 30% of participants opposed the vaccine due to religious or moral reasons.20 Vaccine hesitancy has been identified as the main factor contributing to suboptimal vaccine uptake and coverage rates worldwide. The Strategic Advisory Group of Experts (SAGE) on immunization, a group established by the WHO, defines hesitancy as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services”.21 In 2019, the WHO listed vaccine hesitancy as one of the top ten threats to global health.22 Vaccine hesitancy is a complex phenomenon influenced by factors such as concerns about vaccine safety, misconceptions, and cultural or religious beliefs.21 A recent study reported that although the vaccine hesitancy in the Saudi population was low, only 20% thought that new vaccines, such as HPV, were safe. If not adequately addressed, HPV vaccine hesitancy could have a negative impact on current efforts to control HPV infection, leading to an increased burden of HPV infection and its associated diseases.
Several local studies have provided insight into the knowledge and awareness of HPV infection and vaccination.15,17,20,23–26 However, there are no local studies, especially in Riyadh, that examine the determinants of HPV vaccine hesitancy among university students. Understanding vaccine hesitancy is crucial for identifying the factors that influence public attitudes, beliefs, and behaviors regarding the HPV vaccine. This understanding is imperative for the development of appropriate interventions to achieve high vaccine coverage. Furthermore, there is a scarcity of studies that have assessed the knowledge of the HPV vaccine among health college students. Closing this knowledge gap is essential for preparing future healthcare workers before they enter the workforce. Additionally, health college students often possess the potential to influence their communities. In our conservative society, a significant proportion of them may not yet be sexually active. Hence, including universities in vaccination campaigns becomes vital to ensure that students are well-informed about the vaccine and its accessibility. Therefore, this study aimed to assess the awareness and knowledge of the HPV vaccine and identify the key determinants of HPV vaccine hesitancy among health college students in Saudi Arabia.
Material and Methods
Study Design and Setting
The present study was a cross-sectional survey targeting students enrolled in health colleges at King Saud University (KSU), Riyadh, Saudi Arabia. Data was collected in December 2022 from both male and female campuses of the following health colleges: College of Medicine, College of Dentistry, College of Pharmacy, College of Applied Medical Sciences, and College of Nursing.
Study Measures
A self -administered 17-item questionnaire was adapted from Farsi et al17 and the questions related to HPV vaccine knowledge were formulated and validated by Waller et al.27 The first part included six questions about sociodemographic characteristics (gender, age, marital status, cumulative grade point average (GPA), smoking status and history of Sexually Transmitted Infections (STIs)). Note that GPA is a standardized way to measure a student’s academic performance. In the Saudi Arabian educational system, a GPA on a 5.0 scale is used, and it typically ranges from 0.0 to 5.0. We included GPA as a variable to examine whether a student’s GPA might contribute to their overall knowledge and information-seeking behavior regarding the HPV vaccine. According to a recent study,28 GPA was found to have a direct relationship with HPV knowledge. This was followed by a question asking whether or not they had heard of the HPV vaccine. If the participants answered yes, they were directed to the second part which consisted of seven “True/False/I Don’t Know” questions measuring HPV vaccine knowledge. Based on these responses, a percentage of correct answers were calculated for each individual, in reference to Waller et al.27 The last part focused on participants’ vaccine acceptability, starting with a question about whether they had received the HPV vaccine. If they had not received it, they were asked about their willingness to receive it with the question: “Would you be interested in getting the HPV vaccine?” Any one responded with “I don’t know” or “No” was considered to be hesitant. The reasons behind their hesitancy were assessed by asking: “What are the main reasons you would NOT want to get the vaccine?”.
Data Collection
Using Cochran’s Formula n0 = (Z2 p (1-p) / e2), where Z= 1.96 for a confidence level of 95%, p = the estimated proportion of the population (0.5) and e = the margin of error (0.05), the sample size was determined to be 385. The sample size was increased to 403 in order to reduce the possibility of sampling errors. The survey link was randomly distributed to students in each of the five health colleges at KSU, as well as via social media platforms and in-person interactions. Inclusion criteria was being a male or female undergraduate student at any health college at KSU. Students in the foundation year, internship students and postgraduate students were excluded. The study purpose was clearly explained to the participants, and they were asked to voluntarily fill out the survey after providing their consent.
Ethical Consideration
Participants were informed about the study’s purpose and were asked voluntarily to fill out the survey after informed consent. Responses were completely anonymous and confidential. This study was conducted in accordance with the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of KSU, Riyadh, Saudi Arabia (Ref. No. 22/0843/IRB). All responses were kept anonymous and confidential.
Statistical Analysis
We calculated frequency and percentage for categorical variables, while means and standard deviations were measured for continuous variables. We estimated the percentage of awareness and vaccine hesitancy as well as the reasons. For each of the knowledge items, we calculated the proportion of responses (true, false and I do not know). This summary was presented in a table with correct responses specified. We also calculated the percentage of responding correctly for all the knowledge items and stratified them by gender and college. We estimated the odds of vaccine hesitancy by gender, college, age group, GPA, smoking status, and awareness about HPV vaccine using logistic regression analysis, for which we reported the adjusted odds ratios (AOR) and 95% confidence intervals (CI). We compared awareness of HPV vaccine and vaccine hesitancy across genders and colleges using chi-square (X2) test. We also compared reasons for hesitancy between males and females using X2. We set an alpha level of 5% for testing statistical significance. The data was analyzed using the Statistical Package for Social Sciences (SPSS) version 26 (Armonk, NY, USA) for IBM.
Results
Student Characteristics
The survey was distributed to 450 students, and 403 students responded, achieving a 100% completion rate. The highest proportion of students were sampled from the College of Applied Medical Sciences (42.2%). Furthermore, there was unequal sampling of males and females across the colleges, with only 6 males sampled from the College of Nursing, while only 7 females were sampled from the College of Pharmacy (Table 1). The vast majority of the students were single and reported no history of sexually transmitted infection (STI) (Table 1).
 |
Table 1 Descriptive Characteristics of Students Participating in the Survey (N=403) |
Awareness About the HPV Vaccine
Overall, only 201 students reported ever hearing about the HPV vaccine (49.9%), with 57.1% for females, and 41.9% for males. Among these, the highest proportion of awareness was among students from the College of Medicine (81.2%), while the lowest was among students from the College of Applied Medical Sciences (24.1%) (Figure 1). When comparing awareness between males and females, it was consistently higher among females compared to males. Furthermore, this gender discrepancy was statistically significant among students from the College of Applied Medical Sciences (X2=29.0, df=1, p-value < 0.0001), and those from the College of Dentistry (X2=11.6, df=1, p-value=0.001).
Knowledge About HPV Vaccine
Students who reported hearing about the vaccine were assessed on their vaccine knowledge. Detailed responses by gender and college are presented in Table 2. Only a small percentage of students answered all the items correctly, which may reflect the lack of exposure to HPV vaccine information in their curricula. Even among the students who are expected to have the most exposure to this information, medical students, only 25% of the women and 9.8% of men responded correctly for all items (Table 2).
 |
Table 2 Assessment of Knowledge About HPV Vaccine Among Those Who Have Heard of the Vaccine, by Gender and College (N=201) |
HPV Vaccine Hesitancy and Its Reasons
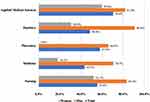
Overall, only 21 students (5.2%) reported receiving the HPV vaccine; with 6.6% among females and 3.7% among males. When asked about their willingness to receive the vaccine, a total of 165 students (40.9%), including 56.1% of females and 24.1% of males expressed their willingness. Thus, the overall HPV vaccine hesitancy in this study was 59.1% with rates of 43.9% for females and 75.9% for males (X2=42.7; df=1; p-value <0.0001). The highest proportion of HPV vaccine hesitancy was among students from the College of Applied Medical Sciences (70.6%) (Figure 2). Furthermore, vaccine hesitancy was significantly higher among males compared to females. Among males, the highest proportion of vaccine hesitancy was observed in the College of Dentistry (90.9%), while among females, it was in the College of Applied Medical Sciences (59.8%).
When asked about the reasons for not being willing to receive the HPV vaccine, the most common reason was not knowing enough about the vaccine (39.7%). Moreover, a significantly greater proportion of males (47.1%) believed they did not need the HPV vaccine compared to females (22.4%) (Figure 3).
 |
Figure 3 Reasons for hesitancy towards HPV vaccine by gender. *X2=27.2; df=1; p-value < 0.0001. **X2=5.1; df=1; p-value=0.024. |
Predictors of HPV Vaccine Hesitancy
The odds of HPV vaccine hesitancy among males were around six-fold more than among females (AOR=6.2; 95% CI=3.44, 11.16). Although not statistically significant, compared to the students from the College of Applied Medical Sciences, the odds of vaccine hesitancy were slightly greater among students from the Colleges of Dentistry (AOR=1.2; 95% CI=0.50, 3.14), and Nursing (AOR=1.2; 0.59, 2.49). Compared to students between 18 and 20 years of age, the odds of vaccine hesitancy were 60% lower among those age 21 to 23 years of age (AOR=0.4; 95% CI=0.20, 0.65). Furthermore, awareness about the HPV vaccine was associated with a 50% reduction in the odds of vaccine hesitancy (AOR=0.5; 95% CI=0.28, 0.83) (Table 3).
 |
Table 3 Assessing the Odds for Vaccine Hesitancy by Student Characteristics (N=403) |
Discussion
Given that HPV infection is a preventable disease, it is of utmost importance to bridge the knowledge gap among prospective healthcare professionals before they enter the workforce. In order to accomplish this, we assessed the level of HPV knowledge among health students enrolled in the five health colleges KSU in the central province of Saudi Arabia.
Findings from this study can be summarized in the following points: First, nearly half of the students had some awareness of the HPV vaccine. The highest proportion of awareness was among College of Medicine (81.2%), while the lowest was among students from the College of Applied Medical Sciences (24.1%). Second, knowledge assessment of participants who claimed to be aware of HPV vaccine showed that only a few of them answered all the items correctly across all the colleges. Third, only a small minority (5.2%) reported actually receiving the vaccine. The overall rate of HPV vaccine hesitancy was high (59.1%) with significant differences between genders (43.9% for females and 75.9% for males). Fourth, the main reason for vaccine hesitancy was a lack of sufficient information about the vaccine. Notably, males were twice as likely as females to believe that they did not require the HPV vaccine. Lastly, the odds for HPV vaccine hesitancy were greater among males and younger age groups compared to females and older age groups.
Numerous local studies have contributed to our understanding of HPV infection and vaccination.15,17,20,23–26 Nevertheless, a noticeable research gap exists, especially in Riyadh, the capital of Saudi Arabia, where investigations into the factors influencing HPV vaccine hesitancy among university students are notably absent. Additionally, this study’s distinctiveness lies in its inclusion of both male and female students within the gender-segregated education system in Saudi Arabia. It highlights the gap in HPV vaccine hesitancy between the two genders, despite their shared curriculum.
When compared to global studies, our findings revealed a higher level of awareness (49.9%) of the HPV vaccine in comparison to a pooled estimate meta-analysis among Chinese college students, which reported 40.27% awareness.29 Nevertheless, the level of awareness among our subjects was slightly lower than that of women visiting a gynecological clinic in Kazakhstan, where 52% of them were aware of the HPV vaccine.30 In contrast with local studies targeting different populations, our subjects demonstrated slightly better awareness compared to others, with reported HPV vaccine awareness rates that ranged from 30.8% to 42%.15,17,23 This outcome is unsurprising, as health college students are expected to have a higher level of awareness compared to the general population, a trend also observed by researchers in India.31 Moreover, our study was conducted in a capital city, and the results may reflect the liberal attitudes often associated with such urban centers. Therefore, caution should be exercised when interpreting these results in the context of the whole country.
When comparing HPV vaccine awareness across the health colleges, students in the College of Medicine demonstrated higher awareness levels. This finding is consistent with a study conducted in the northern and central regions of Saudi Arabia, which reported that medical students exhibited greater awareness and knowledge about the HPV vaccine compared to their peers in non-medical colleges.32,33 Our study underscores the need to enhance HPV vaccine education at all health colleges to ensure that students consistently receive well-informed education on this important topic. Additionally, female students demonstrated higher awareness of the HPV vaccine compared to male students in all colleges. This observation aligns with previous global29,34,35 and national studies36,37 that have reported a gender disparity favoring females in HPV vaccine awareness. Notably, this gender discrepancy was particularly evident among students from the College of Applied Medical Sciences and the College of Dentistry. It is important to acknowledge that there was an imbalance in the sampling of males and females from the different colleges, and this imbalance should be considered when interpreting the results of this study.
When examining the knowledge of individuals who were aware of the HPV vaccine, it was unexpected to find that only 25% of females and 9.8% of males from the College of Medicine answered all the items correctly. This level of knowledge is significantly lower compared to the HPV vaccine knowledge in developed countries. For instance, a recent study conducted in Switzerland reported that 70% of the participants were knowledgeable regarding the HPV vaccine.38
Our study uncovered low HPV vaccination uptake among health college students at KSU. Only 5.2% of participants indicated that they had received the HPV vaccine, primarily females. This rate aligns with a similar study conducted by Bencherit et al on Algerian college students, which reported a vaccination rate of 5.8%.39 Among all colleges, 59.1% of students expressed hesitancy toward the HPV vaccine, with male students consistently exhibiting higher level of vaccine hesitancy compared to females. In the context of male awareness, it is noteworthy that promotional strategies used in vaccination programs can profoundly influence their perception. Misleading messaging within these programs could potentially lead males to assume that they are not the primary target demographic, consequently diminishing the perceived importance of receiving the vaccine. Interestingly, a recent study on medical students in China showed contrasting results, with female students displaying a higher hesitancy rate than male students.40 Additionally, a study conducted with female university students in Kuwait reported a much lower vaccine hesitancy rate (~20%) compared to our findings.41 When comparing hesitancy rates among male student from different colleges, no significant variation in vaccine acceptance was observed. However, female students’ differences in hesitancy were apparent between colleges, with females from the College of Applied Medical Sciences exhibiting the highest level of hesitation. This suggests that factors other than gender may influence vaccine acceptance among students in this particular college.
We also identified various reasons for HPV vaccination hesitancy among participants. The most frequently mentioned reasons by both male and female participants were a lack of sufficient knowledge about the vaccine (39.7%) and being sexually inactive (39.4%). Additionally, approximately 22.4% of participants, regardless of gender, expressed uncertainty about where to access the HPV vaccine.
It is important to note that in Saudi Arabia, the HPV vaccine is part of the national immunization program, and it is provided to females between the ages of 9 and 13. The vaccine is available at no cost in both private and government hospitals. Girls aged 9–14 receive two doses of the HPV vaccination, while those aged 15 and older are recommended to receive three doses.42 Furthermore, a school-based program has been recently introduced to promote HPV vaccination. These findings suggest that there is a need to enhance awareness among university students regarding the availability and accessibility of the HPV vaccine. To address this, we recommend including universities in vaccination campaigns to ensure that students are well-informed about the vaccine and where to receive it.
A gender-based comparison of vaccine hesitancy reasons revealed that males (47.1%) were two times more likely than females (22.4%) to believe that they did not need the HPV vaccine, indicating a potential lack of awareness among males regarding the risks associated with not receiving the vaccine. On the other hand, females were significantly more concerned about the safety of the HPV vaccine compared to males. These reasons for vaccine hesitancy align with those reported in previous studies. For example, Zhou et al’s study on college students in China identified factors such as lack of convenience (not knowing where to get the vaccine, distant vaccination sites, and lack of reliable information) and concerns about vaccine safety as deterrents to seeking HPV vaccination.40 Studies conducted in the USA and Kuwait also revealed concerns about vaccine safety as a contributing factor to vaccine hesitancy among college students.41,43 The survey conducted among with Algerian students revealed that approximately 30% of students believed they did not require the HPV vaccine.39
Several factors were identified as potential predictors of HPV vaccine hesitancy in our study. Male gender increased the odds of vaccine hesitancy by six-fold. In addition to gender, age was also found to be a predictor of vaccine acceptance. Students between the ages of 22 and 23 had lower odds of vaccine hesitancy compared to those in the 18–20-year age group, suggesting that older individuals may be more willing to receive the HPV vaccine. The association of older age with an increased likelihood of HPV vaccine acceptance has been previously reported in studies by Alhusayn et al on Saudi parents’ attitudes towards the vaccine16 and by Alsanafi et al among college students in a Kuwaiti university.41 Furthermore, our analysis revealed that awareness of the HPV vaccine was associated with 50% reduction in the odds of vaccine hesitancy, indicating that educating students about the HPV vaccine may be an effective strategy for promoting vaccine uptake.
This study has some limitations that should be acknowledged. The absence of data on HPV infection status among students introduces a factor that may affect the results of the study. A second concern is the unequal sampling across participating colleges, which raises the possibility of selection bias. Thirdly, the current study involved health colleges’ students from one academic institution in Saudi Arabia’s central region. For a more comprehensive understanding of HPV vaccine awareness and hesitancy among Saudi students, similar studies should be conducted at other universities in multiple Saudi Arabian regions. Notwithstanding these limitations, our study provides valuable insights into the relatively understudied HPV vaccine awareness and knowledge among male and female students in health colleges within the socially conservative society of Saudi Arabia. Health college students play a pivotal role in disseminating HPV vaccine awareness within their communities. Enhancing their understanding is essential for effective HPV prevention. This can be carried out by incorporating comprehensive information about HPV and its vaccination into their curricula. Universities and health colleges should train and encourage students in health-related programs to act as peer educators to disseminate accurate information regarding the benefits of the HPV vaccine.
Conclusion
In conclusion, this study highlights the evident lack of knowledge regarding the HPV vaccine among health college students. It also underscores the low uptake of the vaccine and the substantial hesitancy, largely attributed to inadequate awareness and knowledge. Therefore, we propose a more comprehensive integration of the HPV vaccine’s benefits into the curricula of all university health college students. The implementation of university-wide interventions and educational campaigns offers the potential to enhance awareness and knowledge of the HPV vaccine, ultimately facilitating increased community acceptance of HPV vaccination. Additionally, we recommend further investigation into the impact of expanding vaccination locations and disseminating information about the vaccine’s safety and effectiveness, as these measures may contribute to higher vaccination rates among college students.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author.
Acknowledgments
The authors extend their appreciation to the Deputyship for Research and Innovation, “Ministry of Education” in Saudi Arabia for funding this research (IFKSUOR3-113-1).
Funding
This research was financially supported by The Deputyship for Research and Innovation, Ministry of Education in Saudi Arabia for funding this research work though the project no. IFKSUOR3-113-1.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kombe Kombe AJ, Li B, Zahid A, et al. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Pub Heal. 2021;8:1–19. doi:10.3389/fpubh.2020.552028
2. Jemal A, Edgar P, Dorell C, et al. Annual report to the nation on the status of cancer, 1975 – 2009 featuring the burden and trends in human papillomavirus (hpv)– associated cancers and hpv vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175–201. doi:10.1093/jnci/djs491
3. de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int J Cancer. 2017;141(4):664–670. doi:10.1002/ijc.30716
4. Okunade KS. Human papillomavirus and cervical cancer. J Obstet Gynaecol. 2020;40(5):602–608. doi:10.1080/01443615.2019.1634030
5. Pimple S, Mishra G. Cancer cervix: epidemiology and disease burden. Cytojournal. 2022;19:21. doi:10.25259/CMAS_03_02_2021
6. HOV Information Centre. Human papillomavirus and related diseases report; 2023. Available from: https://hpvcentre.net/statistics/reports/SAU.pdf.
7. Akkour K, Alghuson L, Benabdelkamel H, et al. Cervical Cancer and Human Papillomavirus Awareness among Women in Saudi Arabia. Medicina. 2021;57(12):1–9. doi:10.3390/medicina57121373
8. Ali MAM, Bedair RN, Rasha M. Cervical high-risk human papillomavirus infection among women residing in the gulf cooperation council countries: prevalence, type-specific distribution, and correlation with cervical cytology. Cancer Cytopathol. 2019;127(9):567–577. doi:10.1002/cncy.22165
9. Al-Muammar T, Al-Ahdal MN, Hassan A. Human Papilloma Virus-16/18 cervical infection among women attending a family medical clinic in Riyadh. Ann Saudi Med. 2007;27(1):6–10. doi:10.5144/0256-4947.2007.1
10. Alhamlan F, Obeid D, Khayat H, et al. Prognostic impact of human papillomavirus infection on cervical dysplasia, cancer, and patient survival in Saudi Arabia: a 10-year retrospective analysis. Ann Saudi Med. 2021;41(6):350–360. doi:10.5144/0256-4947.2021.350
11. Arabia MOHS. Ministry Of Health Saudi Arabia, Communicable Diseases HPV (Human Papillomavirus). Available from: https://www.moh.gov.sa/en/Pages/Default.asp.
12. McLemore MR. Gardasil: introducing the new human papillomavirus vaccine. Clin J Oncol Nurs. 2006;10(5):559–560. doi:10.1188/06.CJON.559-560
13. World Health Organization. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Geneva: World Health Organization; 2020.
14. Saudigazette. More than 131,087 Girl students received the hpv vaccine in Saudi Arabia. Available from: https://saudigazette.com.sa/article/627948/SAUDI-ARABIA/More-than-131087-girl-students-received-the-HPV-vaccine-in-Saudi-Arabia?ref=rss&format=simple&link=link.
15. Almaghlouth AK, Bohamad AH, Alabbad RY, Alghanim JH, Alqattan DJ, Alkhalaf RA. Acceptance, awareness, and knowledge of human papillomavirus vaccine in eastern province, Saudi Arabia. Cureus. 2022;14(11). doi:10.7759/CUREUS.31809
16. Alhusayn K, Alkhenizan A, Abdulkarim A, Sultana H, Alsulaiman T, Alendijani Y. Attitude and hesitancy of human papillomavirus vaccine among Saudi parents. J Fam Med Prim Care. 2022;11(6):2909. doi:10.4103/JFMPC.JFMPC_2377_21
17. Farsi NJ, Baharoon AH, Jiffri AE, Marzouki HZ, Merdad MA, Merdad LA. Human papillomavirus knowledge and vaccine acceptability among male medical students in Saudi Arabia. Hum Vaccines Immunother. 2021;17(supp 7):1968–1974. doi:10.1080/21645515.2020.1856597
18. Gallagher KE, LaMontagne DS, Watson-Jones D. Status of HPV vaccine introduction and barriers to country uptake. Vaccine. 2018;36(32 Pt A):4761–4767. doi:10.1016/J.VACCINE.2018.02.003
19. Bruni L, Diaz M, Barrionuevo-Rosas L, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4(7):e453–e463. doi:10.1016/S2214-109X(16)30099-7
20. Darraj AI, Arishy AM, Alshamakhi AH, et al. Human papillomavirus knowledge and vaccine acceptability in Jazan province, Saudi Arabia. Vaccines. 2022;10(8):1337. doi:10.3390/VACCINES10081337
21. MacDonald NE, Eskola J, Liang X, et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi:10.1016/J.VACCINE.2015.04.036
22. World Health Organization. Ten threats to global health in; 2019. Available from: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
23. Alshammari F, Khan KU. Knowledge, attitudes and perceptions regarding human papillomavirus among university students in Hail, Saudi Arabia. PeerJ. 2022;10. doi:10.7717/PEERJ.13140
24. Almehmadi MM, Salih MM, Al-Hazmi AS. Awareness of human papillomavirus infection complications, cervical cancer, and vaccine among the Saudi population: a cross-sectional survey. Saudi Med J. 2019;40(6):555–559. doi:10.15537/smj.2019.6.24208
25. Al-Shaikh GK, Almussaed EM, Fayed AA, Khan FH, Syed SB, Al-Tamimi TN. Knowledge of Saudi female university students regarding cervical cancer and acceptance of the human papilloma virus vaccine – Pub med. Saudi Med J. 2014;35(10):1223–1230.
26. Aldawood E, Alzamil L, Faqih L, et al. Awareness of human papillomavirus among male and female University students in Saudi Arabia. Healthc. 2023;11(5):1–12. doi:10.3390/healthcare11050649
27. Waller J, Ostini R, Marlow LAV, McCaffery K, Zimet G. Validation of a measure of knowledge about human papillomavirus (HPV) using item response theory and classical test theory. Prev Med. 2013;56(1):35–40. doi:10.1016/j.ypmed.2012.10.028
28. Mohammed S, Abdelaliem F, Kuaia AM, et al. Knowledge and attitudes toward human papillomavirus and vaccination: a survey among nursing students in Saudi Arabia; 2023.
29. Yin G, Zhang Y, Chen C, Ren H, Guo B, Zhang M. Have you ever heard of human papillomavirus (hpv) vaccine? The awareness of hpv vaccine for college students in China based on meta-analysis. Hum Vaccin Immunother. 2021;17(8):2736–2747. doi:10.1080/21645515.2021.1899731
30. Issa T, Babi A, Issanov A, et al. Knowledge and awareness of human papillomavirus infection and human papillomavirus vaccine among Kazakhstani women. PLoS One. 2021:1–14. doi:10.1371/journal.pone.0261203
31. Rashid S, Labani S, Das BC. Knowledge, awareness and attitude on HPV. HPV Vaccine C C Coll Stud In. 2016;1–11. doi:10.1371/journal.pone.0166713
32. Altamimi T. Human papillomavirus and its vaccination: knowledge and attitudes among female university students in Saudi Arabia. J Fam Med Prim Care. 2020;9(4):1849. doi:10.4103/JFMPC.JFMPC_1205_19
33. Azer SA, Alsaleem A, Albassam N, et al. What do university students know about cervical cancer and HPV vaccine? Eur Rev Med Pharmacol Sci. 2022;26(10):3735–3744. doi:10.26355/EURREV_202205_28870
34. Chen G, Wu B, Dai X, et al. Gender differences in knowledge and attitude towards hpv and hpv vaccine among college students in Wenzhou, China. Vaccines. 2021;10(1):10. doi:10.3390/VACCINES10010010
35. Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017;13(11):2713–2722. doi:10.1080/21645515.2017.1363133
36. Lingam AS, Koppolu P, Alhussein SA, et al. Dental students’ perception, awareness and knowledge about hpv infection, vaccine, and its association with oral cancer: a multinational study. Infect Drug Resist. 2022;15:3711–3724. doi:10.2147/IDR.S365715
37. Farsi NJ, Sharif S, Marzouki H, Merdad L, Marzouki H, Merdad L. knowledge of human papillomavirus (hpv) and oropharyngeal cancer and acceptability of the hpv vaccine among dental students. Asian Pac J Cancer Prev. 2020;21(12):3595–3603. doi:10.31557/APJCP.2020.21.12.3595
38. Schwendener CL, Kiener LM, Jafflin K, et al. HPV vaccine awareness, knowledge and information sources among youth in Switzerland: a mixed methods study. BMJ Open. 2022:1–11. doi:10.1136/bmjopen-2021-054419
39. Bencherit D, Kidar R, Otmani S, et al. Knowledge and awareness of Algerian students about cervical cancer, hpv and hpv vaccines: a cross-sectional study. Vaccines. 2022;10(9):1420. doi:10.3390/VACCINES10091420
40. Zhou L, Wang J, Cheng P, Li Y, Liu G, Zhang X. HPV vaccine hesitancy among medical students in china: a multicenter survey. Front Public Health. 2022;10. doi:10.3389/FPUBH.2022.774767
41. Alsanafi M, Salim NA, Sallam M. Willingness to get HPV vaccination among female university students in Kuwait and its relation to vaccine conspiracy beliefs. Hum Vaccin Immunother. 2023;19(1). doi:10.1080/21645515.2023.2194772
42. Saudi Gazette report. MoH calls for giving girls HPV vaccine at an early age; 2022. Available from: https://saudigazette.com.sa/article/620264.
43. Goldfarb JA, Comber JD. Human papillomavirus (HPV) infection and vaccination: a cross-sectional study of college students’ knowledge, awareness, and attitudes in Villanova, PA. Vaccine X. 2022;10:100141. doi:10.1016/J.JVACX.2022.100141
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.