Back to Journals » Advances in Medical Education and Practice » Volume 14
How Much Experience is Required to Acquire the Skills to Independently Perform Spine Surgery? What Milestones are Needed for Successful Surgery?
Authors Fukushi R , Teramoto A , Yoshimoto M, Miyakoshi N , Kudo D , Emori M, Shimada Y , Yamashita T
Received 4 March 2023
Accepted for publication 13 June 2023
Published 28 June 2023 Volume 2023:14 Pages 657—667
DOI https://doi.org/10.2147/AMEP.S411047
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Ryunosuke Fukushi,1 Atsushi Teramoto,1 Mitsunori Yoshimoto,1 Naohisa Miyakoshi,2 Daisuke Kudo,2 Makoto Emori,1 Yoichi Shimada,2 Toshihiko Yamashita1
1Department of Orthopaedic Surgery, Sapporo Medical University School of Medicine, Sapporo, Japan; 2Department of Orthopaedic Surgery, Akita University School, Akita, Japan
Correspondence: Ryunosuke Fukushi, Department of Orthopaedic Surgery, Sapporo Medical University School of Medicine, S1 W16, Sapporo, Hokkaido, 060-8543, Japan, Tel +81-11-611-2111, Fax +81-11-621-8059, Email [email protected]
Purpose: To assess the number of surgeries needed to acquire the necessary skills to perform spine surgery independently.
Patients and Methods: A questionnaire on 12 different spinal procedures was sent to orthopedic surgeons affiliated with the spine teams of orthopedic departments at either the Akita University or Sapporo Medical University. Participants were asked to identify whether they (A) could independently perform each procedure, (B) could perform each procedure with the assistance of a senior doctor, or (C) were unable to perform each procedure. Those whose response was (A) were asked how many surgeries were required to acquire the necessary skills. Those who responded to (B) or (C) were asked how many surgeries they believed were required to acquire the skills necessary to operate independently. Participants also responded to 10 questions on surgical training techniques and rated the usefulness of each method.
Results: A total of 55 spine surgeons responded to the questionnaire. Group A required significantly fewer surgeries in the following categories to become independent than required Group C: upper cervical spine surgery (7.3/19.3), anterior cervical decompression/fusion (6.7/28.8), posterior cervical decompression/fusion (9.5/27.3), lumbar discectomy (12.6/26.7), endoscopic lumbar discectomy (10.2/24.2), spinal tumor resection (6.5/37.2), and spinal kyphosis surgery (10.3/32.3). Over 80% of participants responded that the following were effective methods: “surgeries where a senior doctor is the main surgeon, and the respondent is the assistant and observer”; “surgeries where the respondent is the main surgeon, and a senior doctor is an assistant”; “self-study using surgery manuals, articles, and textbooks”; and “training through video surgery sessions”.
Conclusion: Surgeons who do not perform specific procedures independently require more surgical experience than those who operate independently. Our results may help develop more efficient training methods for spine surgeons.
Keywords: surgical experience, surgical training, training system, inexperienced spine surgeons
Plain Language Summary
Surgical experience is essential for mastering the skills required to perform spine surgery effectively, and on-The-job training with actual patients is indispensable to learn the appropriate techniques. This study aimed to assess the number of surgeries needed to acquire the necessary skills to perform spine surgery independently. A questionnaire on 12 different spinal procedures was sent to orthopedic surgeons affiliated with the spine teams of orthopedic departments at our institutions. We found that surgeons who do not perform specific procedures independently require more surgical experience than those who operate independently. Our results may help develop more efficient training methods for spine surgeons.
Introduction
Surgical experience is essential for mastering the skills required to perform spine surgery effectively, and on-The-job training with actual patients is indispensable to learn the appropriate techniques. In previous reports, Li et al1 have demonstrated that for spine surgery, most surgeons and procedures performed per year in a hospital positively correlated with lower morbidity and mortality, shorter length of stay, and fewer readmissions and hospitalization costs. Similarly, De la Garza Ramos et al2 Blais et al3 and Frankel et al4 and Schoenfeld et al5 reported lower complication rates in anterior cervical decortication and fusion, lumbar spine surgery, and cervical lumbar spine surgery, respectively, with a similarly higher-than-average annual number of hospital operations.
These studies consistently focused on the number of surgeons and operations in a hospital and did not investigate the number of operations performed by a single surgeon.
One orthopedic study reported the number of cases required to gain autonomy based on a survey of 727 surgery residents trained in an orthopedic training program in the United States.6 However, to the best of our knowledge, no study has focused on one spine surgeon and assessed the number of operations required to acquire the skills necessary to perform each spine operation independently. Identifying the number of surgeries required to acquire these skills can help develop an efficient training system for surgeons and enable inexperienced spine surgeons to plan their careers. This can also prevent inexperienced surgeons from prematurely performing spine surgery independently on patients.
We surveyed spine surgeons to determine the number of surgeries required to obtain the skills necessary to perform various spinal surgeries independently and to investigate effective training methods to improve their surgical skills.
Materials and Methods
A questionnaire survey was sent to 70 orthopedic surgeons affiliated with the spine teams of orthopedic departments at either the Akita University or Sapporo Medical University. The questionnaire was administered via e-mail using a computer-based input method. We excluded those in the early stages of their medical internship. This study met the criteria for exemption from Institutional Review Board approval; therefore, the requirement for informed consent was waived.
Our questionnaire aimed to assess the following items pertaining to the acquisition of independent surgical skills: the number of years since obtaining a medical license; type of hospital where the surgeon was working (university hospital, private hospital [general or orthopedic hospital], or clinic); whether the surgeon was certified as a Japanese Society of Spine and Spinal Cord Diseases instructor; number of independent spine surgeries the surgeon performed per year; and current state of skill acquisition by the surgeon.
In this survey, the surgeons were asked questions concerning 12 different types of spine surgeries, namely upper cervical surgery, anterior cervical decompression/fusion, posterior cervical decompression/fusion, anterior lumbar fusion, posterior lumbar decompression, endoscopic posterior lumbar decompression, posterior lumbar decompression and fixation, lumbar discectomy, endoscopic lumbar discectomy, spinal tumor resection, spinal kyphosis surgery, and percutaneous vertebroplasty. For each procedure listed, the participants were asked to identify whether (A) they could perform the procedure independently, (B) they could perform the procedure with the help of a senior doctor, or (C) they could not perform the procedure. If participants selected (A) for any of the procedures, they were asked to state the number of surgeries they had to perform to acquire the necessary skills. If the participants selected options (B) or (C) for any of the procedures, they were asked how many surgeries they believed were necessary to acquire the skills required to independently perform the procedures.
To gain information on training related to surgical skill improvement, the following information on actual surgical training was collected: (1) surgeries where the participant was the main surgeon and a senior doctor was the assistant; (2) surgeries where a senior doctor was the main surgeon and the participant was the assistant and observer; (3) surgeries where the participant was the main surgeon and a doctor with less experience in spinal surgery was the assistant; and (4) participation in orthopedic surgeries not involving the spine. The following simulation-related information was also collected: (5) surgical training on cadavers; (6) surgical training on animals; (7) surgical training using simulation models; and (8) virtual reality surgical training. As for self-education training, information was sought on (9) self-study with surgery manuals, articles, and textbooks and (10) training sessions using surgery videos. For these 10 items, respondents were asked to evaluate whether each training method was effective using the following 5-option scale: “strongly agree”, “agree”, “neither agree nor disagree”, “disagree”, and “strongly disagree”.
As a secondary evaluation, the same analysis was conducted with two groups: one group of surgeons who obtained a medical license <22 years (3–21 years) ago (young group) and another group of senior surgeons who obtained their license >22 years ago (senior group). We also interviewed the senior group to determine what they could do to improve their surgical skill.
Statistical Analyses
The average number of surgeries performed by the participants who positively answered to (A), (B), or (C) was compared for each surgical procedure. Fisher’s exact probability test was used to assess the significance of the data among the three groups, while the Mann–Whitney U-test was used to assess the significance of non-parametric data between groups. A p-value <0.05 was considered statistically significant. Non-parametric tests were employed for this study as the “small sample size”, “inclusion of outliers” and “qualitative data” raised doubts regarding the normality of the data.
Results
Of the 70 surgeons surveyed, 55 responded (response rate, 78.6%; 25 of 29 surgeons from the Akita University and 31 of 40 surgeons from the Sapporo Medical University). Demographic data are summarized in Table 1. Regarding the time since obtaining a medical license, the largest percentage of participants had obtained a license ≥22 years ago (42%), followed by 16–18 (15%) and 7–9 (15%) years ago. The largest percentage of surgeons worked in university hospitals (35%), followed by private general and orthopedic hospitals. Qualified spine surgery instructors comprised 19 of 55 participants. The annual number of spine surgeries in which the surgeons participated was within the range of 61–90 for the largest percentage of surgeons (25%), followed by 31–60 (18%) and 121–150 (13%) surgeries.
 |
Table 1 Demographic Data |
As for the current state of technical acquisition, 80% of participants were able to perform lumbar discectomy, posterior lumbar decompression, and posterior cervical decompression/fusion, and nearly 50% were able to perform anterior lumbar fusion and endoscopic lumbar discectomy. The number of participants who answered (A), (B), or (C) for each spinal surgery item is summarized in Table 2.
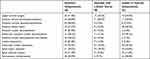 |
Table 2 Summary of Participants’ Responses |
The number of surgeries reported for each type of spinal surgery (for Groups A, B, and C) is summarized in Table 3. The participants who reported autonomy (Group A) responded that they required fewer surgeries to adequately perform the surgeries independently than what was believed to be necessary by those with an inability to perform the surgeries (Group C). This difference was significant for upper cervical spine surgery (Group A, 7.3/ Group C, 19.3), anterior cervical decompression/fusion (6.7/28.8), posterior cervical decompression/fusion (9.5/27.3), lumbar discectomy (12.6/26.7), endoscopic lumbar discectomy (10.2/24.2), spinal tumor resection (6.5/37.2), and spinal kyphosis surgery (10.3/32.3) (Table 3). In Group A, the average number of surgeries deemed necessary to acquire the skills to act independently was ranked as follows: posterior lumbar decompression and fixation ranked highest (n=15), followed by posterior lumbar decompression (n=14.2), endoscopic posterior lumbar decompression (n=13.3), lumbar discectomy (n=12.6), other operations (n ≤10), and percutaneous vertebroplasty (n=4.2) (Figure 1). The average number of surgeries considered necessary to achieve autonomy ranked differently in Group C than in Group A, with spinal tumor resection ranking the highest (n=37.2), followed by posterior lumbar decompression and fixation (n=33.6), spinal kyphosis surgery (n=32.3), and anterior cervical fusion (n=28.8) (Figure 1).
 |
Table 3 Number of Surgeries Necessary or Believed to Be Necessary to Master Each Type of Spinal Surgery |
 |
Figure 1 Number of surgeries necessary (Group A) or believed to be necessary (Group C) to master each type of spine surgery. |
Table 4 shows the frequency of participant ratings for the 10 surgical training technique questions. Over 80% of surgeons responded that they had considered the following training methods to be effective: “surgeries where a senior doctor was the main surgeon, and the respondent was the assistant and observer”; “surgeries where the respondent was the main surgeon, and a senior doctor was the assistant”; “self-study with surgery manuals, articles, and textbooks”; and “training using video surgery sessions”.
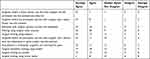 |
Table 4 Participants’ Ratings for the 10 Surgical Training Technique Questions |
The number of participants in the young and senior groups who responded (A), (B), or (C) to each spinal surgery item is summarized in Table 5. The senior Group A had a higher percentage of positive responses to (A) than had the young group, and 100% of the Group A participants responded positively for posterior cervical decompression/fusion, posterior lumbar decompression, posterior lumbar decompression and fixation, and lumbar discectomy.
 |
Table 5 Summary of Participants’ Responses for the Young Group and Senior Group |
The number of surgeries reported for each type of spinal surgery for Groups A, B, and C among both young and senior surgeons is summarized in Table 6. Compared with the young group, the senior group responded that they required fewer surgeries to perform independently. There were significant differences between both groups, except for endoscopic posterior lumbar decompression. Furthermore, the number of surgeries tended to be lower than in Table 3.
 |
Table 6 Number of Surgeries Necessary or Believed to Be Necessary to Master Each Type of Spinal Surgery for the Young and Senior Groups |
Table 7 shows the frequency of participant ratings for the 10 surgical training technique questions in the young and senior groups. This trend is similar to that shown in Table 4. When stratified according to age, no change in surgical training techniques improved surgical skills.
 |
Table 7 Participants’ Ratings for the 10 Surgical Training Technique Questions for the Young and Senior Groups |
The senior group made the following statements in response to what should be done to improve surgical skills: “watching good surgeons perform surgeries”, “being humble and remembering the first visit”, “always having the desire to improve”, “clarifying any uncertainties you have by image training, acting as if you are performing the actual surgery before going into surgery”, “accumulating know-how by taking notes”, “writing your own surgical record even if you are an assistant”, “observing surgeries at other facilities and multiple facilities”, and “being close to your peers to stimulate each other”.
Discussion
Surgical experience is required to acquire the skills necessary to perform spinal surgery. However, no studies have determined the number of spine surgical procedures required to independently perform specific spine surgeries. Not knowing how many surgeries are required to acquire competence may be challenging for physicians deciding a career path and choosing training hospitals to develop their required skills. Furthermore, understanding the number of spine surgeries that need to be performed is beneficial when designing training programs for inexperienced surgeons, as it ensures that inexperienced surgeons do not prematurely perform surgeries independently.
Our questionnaire survey found that spine surgeons must perform 4–15 surgeries to acquire the necessary skills for each surgical procedure. These values differed somewhat from the number of surgeries required for skill acquisition by inexperienced surgeons (Figure 1). Surgeons performing these surgeries independently require more basic spinal surgical procedures (eg, lumbar discectomy, endoscopic posterior lumbar decompression, posterior lumbar decompression, posterior lumbar decompression, and fixation). The results of this survey showed that without prior experience in spine surgery, surgeons would typically need to perform 12–15 basic posterior lumbar spine surgeries. Furthermore, our data suggest that once a surgeon acquires the skills necessary for basic spinal procedures, it is possible to acquire the skills required to perform what are typically considered more difficult spine surgeries throughout less than 10 corresponding surgeries. According to our findings, surgeons found it preferable to ask for assistance from a senior doctor during the first 12–15 surgeries and operate on typical cases to prevent harm to the patient (Figure 2). Our survey findings suggest that spine surgeons unable to independently perform each type of spine surgery believed that they needed to perform more surgeries than those who were already able to perform such surgeries independently. Significant differences in the number of surgeries were noted in upper cervical surgery, anterior cervical decompression/fusion, posterior cervical decompression/fusion, lumbar discectomy, spinal tumor resection, and spinal kyphosis surgery. These surgical procedures, except for lumbar discectomy, are not performed as often as other surgeries, indicating fewer opportunities to experience and learn these techniques. Table 8 summarizes the actual number of spinal surgeries performed at each hospital. The results suggest that inexperienced spine surgeons find these surgeries difficult. To develop the skills required for these surgical procedures, surgeons must acquire the necessary experience in a facility that performs many of these surgeries. Building a system in which inexperienced spine surgeons can obtain this experience is desirable.
 |
Table 8 Number of Spine Surgeries Performed at Orthopedic Clinics |
 |
Figure 2 Spinal surgery skill acquisition plan. |
Regarding Group B, the surgeries where “the number of positive responses to B is between those of positive responses to A and C” included “anterior cervical decompression/fusion” and “upper cervical surgery” cervical spine-related surgeries, while the surgeries where “the number of positive responses B was similar to that of positive responses to A” included “endoscopic posterior lumbar decompression”, “lumbar discectomy”, “endoscopic lumbar discectomy”, and “spinal tumor resection” endoscopic and lumbar spine-related surgeries. “Endoscopic posterior lumbar discectomy”, “endoscopic posterior lumbar decompression”, “lumbar discectomy”, and “endoscopic lumbar discectomy” are procedures that are often performed alone without an assistant. When participants can perform surgery with an assistant, it is likely that they have already mastered the technique and are primarily independent (ie, the contribution of the senior physician to the surgery is relatively small in “endoscopic posterior lumbar decompression”, “lumbar discectomy”, and endoscopic lumbar discectomy). These factors might not have differed between Groups B and A. However, in “anterior cervical decompression/fusion” and “upper cervical surgery”, cervical spine-related surgery involves many vital tissues, including the esophagus, trachea, and carotid artery, and the importance of assistants is relatively high due to the difficulty of approach and number of complications. There may have been a gap between Group B, where surgery can be performed with an assistant, and Group A, where surgery can be performed independently (ie, without assistance from a senior physician).
Over 80% of respondents indicated that having a senior doctor participating as an assistant, assisting a senior doctor who taught the procedure, and using surgical textbooks, research articles, lectures, and surgical videos were effective training methods. In contrast, > 50% of participants responded that surgical training on animals was ineffective. Training methods requiring special equipment, including cadavers or animal models, simulations, and virtual reality, have yielded inconsistent results, being deemed useful by some and unhelpful by others. In previous reports, cadaveric and animal models were reportedly less available and inferior in terms of cost and effectiveness.7,8 However, virtual reality has been reported to be an effective training method.9 Due to the COVID-19 pandemic, cadaver and animal model training has become less accessible, making it more difficult for inexperienced surgeons to acquire valuable training. However, simulations and virtual reality have become more popular.7,10 These training methods can be more effective if an appropriate training environment is established. In recent years, robot-assisted surgery has also been reported to improve the learning curve for complicated operations;11 however, its availability varies, and the number of surgeries performed is low.12 Elimination of bias with respect to the number of surgeries and equipment at training facilities is likely to promote a more efficient training system for spine surgeons.
Participants in Group C were younger and less experienced than were those in Group A. Because it is useful to stratify the results according to experience, we performed the same analysis in the young and senior groups. Table 5 and Table 6 show that the senior group required fewer surgeries to perform independently than required the young group, and the number of surgeries tended to be lower than those shown in Table 3. Stratifying the results according to age (years of experience) rather than grouping the results according to the surgeon’s personal opinion may provide more relevant information. However, even if the senior group has been working for a long time, has previously engaged in basic research, or worked in a hospital that is primarily an outpatient or rehabilitation center, it cannot be said that they generally have good surgical skills. Nonetheless, some physicians have good surgical skills, even if they have been in the hospital for a short period. Therefore, both comparisons, classified according to Groups A, B, and C, and according to age (years of experience), are relevant.
As shown in Table 7, there was no difference between the young and senior groups in terms of the training required to improve their surgical skills. The recently introduced virtual reality technology is not highly rated, and it seems that textbooks and videos remain essential to assist both skilled senior surgeons and those less skilled in spine surgery to improve surgical skills, as has been the case for many years.
Previous studies have often focused on the number of surgeons and number of operations in a hospital1–5 but have not investigated the number of operations that a surgeon should experience. Although one article has discussed the number of operations required in general orthopedic surgery,6 to our knowledge, our study is the first to focus specifically on spine surgery, which highlights its novelty.
There also seems to be a slight difference between the number of operations required to acquire general orthopedic and spine surgery skills. In other words, as surgeons gain more surgical experience, even in non-spinal surgery, they develop knowledge of the basic principles of orthopedic surgery and spatial anatomy and, consequently, even if starting from zero knowledge and skills, likely required less surgeries to master spinal surgery compared with general orthopedic surgery. This information will contribute to developing careers and educational systems for spine surgeons.
Limitations
This study has a few limitations. First, the survey involved self-evaluation, and the accuracy of the reported surgical techniques and skill levels were not investigated. Second, the response rate and number of participants were low. Third, most surgeons involved in this study performed <90 cases yearly. This study queried spine surgeons at two university hospitals and affiliated hospitals primarily involved in community medicine. The professors of these two medical departments were from the same university; therefore, there would be fewer differences in the assessment of surgical indications and details of surgical procedures between both hospitals. Moreover, since each hospital is affiliated with a medical department responsible for community medicine, spine surgeons must routinely perform not only spine surgery but also trauma surgery, resulting in fewer spine surgeries per year (Table 8). Moreover, the hospitals that cooperated in the survey were university hospitals and affiliated hospitals whose purpose is to educate young spine surgeons, and this also tended to lower the number of spine surgeries performed per year. Spine specialty hospitals and private hospitals, including spine centers located in urban centers that perform a large number of spine surgeries, were not included in the survey because of the possibility of bias due to possible differences in the assessment of surgical indications, surgical methods, and educational methods. Although this study may be significantly improved if it is more geographically and demographically diverse, it is still relevant because the data were obtained from hospitals with the same evaluation of surgical indications, surgical procedures, and educational policies.
Conclusion
The number of surgeries considered necessary for spine surgeons to operate independently ranged from 12 to 15 for basic posterior lumbar spine surgery and <10 for other surgeries. Compared to surgeons who were able to perform a certain surgery independently, surgeons who were not yet independent believed that they required more experience in performing such surgeries. Preoperative preparation using textbooks and surgical procedure books, watching surgical videos, and participating in on-The-job training with patients are effective strategies for acquiring and improving surgical skills. Therefore, an efficient training system for spinal surgeons must be developed.
Ethics Approval and Informed Consent
This study met the criteria for exemption from Institutional Review Board approval; therefore, the requirement for informed consent was waived.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li HZ, Lin Z, Li ZZ, et al. Relationship between surgeon volume and outcomes in spine surgery: a dose-response meta-analysis. Ann Transl Med. 2018;6(22):441. doi:10.21037/atm.2018.10.48
2. De la Garza Ramo R, Nakhla J, Nasser R, et al. Volume-outcome relationship after 1 and 2 level anterior cervical discectomy and fusion. World Neurosurg. 2017;105:543–548. doi:10.1016/j.wneu.2017.05.060
3. Blais MB, Rider SM, Sturgeon DJ, et al. Establishing objective volume-outcome measures for anterior and posterior cervical spine fusion. Clin Neurol Neurosurg. 2017;161:65–69. doi:10.1016/j.clineuro.2017.08.009
4. Frankel WC, Navarro SM, Haeberle HS, Ramanathan D, Ramkumar PN. Optimizing the volume-value relationship in laminectomy: an evidence-based analysis of outcomes and economies of scale. Spine. 2019;44(9):659–669. doi:10.1097/BRS.0000000000002910
5. Schoenfeld AJ, Sturgeon DJ, Burns CB, Hunt TJ, Bono CM. Establishing benchmarks for the volume-outcome relationship for common lumbar spine surgical procedures. Spine J. 2018;18(1):22–28. doi:10.1016/j.spinee.2017.08.263
6. Kohring JM, Harrast JJ, Stotts AK, et al. Resident Independence performing common orthopaedic procedures at the end of training: perspective of the graduated resident. J Bone Joint Surg Am. 2020;102(1):e2. doi:10.2106/JBJS.18.01469
7. Falavigna A, Guiroy A, Taboada N. Teaching training and surgical education in minimally invasive surgery (MIS) of the spine: what are the best teaching and learning strategies for MIS? Do we have any experience and data? Global Spine J. 2020;10(2_Suppl):126S–129S. doi:10.1177/2192568219875087
8. Parr WCH, Burnard JL, Wilson PJ, Mobbs RJ. 3D printed anatomical (bio)models in spine surgery: clinical benefits and value to health care providers. J Spine Surg. 2019;5(4):549–560. doi:10.21037/jss.2019.12.07
9. Lohre R, Wang JC, Lewandrowski KU, Goel DP. Virtual reality in spinal endoscopy: a paradigm shift in education to support spine surgeons. J Spine Surg. 2020;6(S1):S208–S223. doi:10.21037/jss.2019.11.16
10. McKechnie T, Levin M, Zhou K, Freedman B, Palter VN, Grantcharov TP. Virtual surgical training during COVID-19: operating room simulation platforms accessible from home. Ann Surg. 2020;272(2):e153–e154. doi:10.1097/SLA.0000000000003999
11. Soomro NA, Hashimoto DA, Porteous AJ, et al. Systematic review of learning curves in robot-assisted surgery. BJS Open. 2020;4(1):27–44. doi:10.1002/bjs5.50235
12. Dırvar F, Dırvar SU, Yıldırım T, Cengiz Ö, Talmaç MA. Survey on the surgical skills of orthopedics and traumatology residents from accredited and nonaccredited institutions in İstanbul. Acta Orthop Traumatol Turc. 2020;54(2):168–177. doi:10.5152/j.aott.2020.02.158
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
