Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 13
Home noninvasive ventilatory support for patients with chronic obstructive pulmonary disease: patient selection and perspectives
Authors Storre JH, Callegari J, Magnet FS , Schwarz SB , Duiverman ML , Wijkstra PJ , Windisch W
Received 21 October 2017
Accepted for publication 28 December 2017
Published 28 February 2018 Volume 2018:13 Pages 753—760
DOI https://doi.org/10.2147/COPD.S154718
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Jan Hendrik Storre,1,2 Jens Callegari,3 Friederike Sophie Magnet,3 Sarah Bettina Schwarz,3 Marieke Leontine Duiverman,4,5 Peter Jan Wijkstra,4,5 Wolfram Windisch3
1Department of Intensive Care, Sleep Medicine and Mechanical Ventilation, Asklepios Fachkliniken Munich-Gauting, Gauting, Germany; 2Department of Pneumology, University Medical Hospital, Freiburg, Germany; 3Department of Pneumology, Cologne Merheim Hospital, Kliniken der Stadt Köln gGmbH Witten/Herdecke University, Faculty of Health/School of Medicine, Cologne, Germany; 4Department of Pulmonary Diseases, University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 5Groningen Research Institute of Asthma and COPD (GRIAC), University of Groningen, Groningen, the Netherlands
Abstract: Long-term or home mechanical noninvasive ventilation (Home-NIV) has become a well-established form of therapy over the last few decades for chronic hypercapnic COPD patients in European countries. However, meta-analyses and clinical guidelines do not recommend Home-NIV for COPD patients on a routine basis. In particular, there is ongoing debate about Home-NIV in chronic hypercapnic COPD regarding the overall effects, the most favorable treatment strategy, the selection of eligible patients, and the time point at which it is prescribed. The current review focuses on specific aspects of patient selection and discusses the various scientific as well as clinical-guided perspectives on Home-NIV in patients suffering from chronic hypercapnic COPD. In addition, special attention will be given to the topic of ventilator settings and interfaces.
Keywords: exacerbation, pulmonary emphysema, hypercapnia, mechanical ventilation, respiratory insufficiency
Introduction
Patients with end-stage COPD can present with hypoxemic and hypercapnic respiratory failure.1 Long-term oxygen therapy (LTOT) is a well-established, frequently prescribed treatment for hypoxemic respiratory failure that has been reported to improve long-term survival in patients suffering from COPD.1 Although long-term or home mechanical noninvasive ventilation (Home-NIV) is a widely accepted therapeutic option for restrictive thoracic and neuromuscular patients once hypercapnic respiratory failure occurs,1 this is not the case for patients with chronic hypercapnic COPD.2 A systemic review and data meta-analysis from 2014 concluded that there was not enough evidence at the time to support the routine use of Home-NIV in patients with stable hypercapnic COPD.3 Remarkably, this is in clear contrast to clinical practice, where Home-NIV for chronic hypercapnic COPD has been a well-established treatment in many European countries during at least the last two decades.2,4 Furthermore, this topic has received a high amount of scientific attention, as demonstrated by the number of recent studies related to COPD patients and long-term NIV following acute hypercapnic respiratory failure5,6 and chronic hypercapnic respiratory failure.7,8
Patients with chronic hypercapnic respiratory failure (type II) are the subgroup of COPD patients most likely to benefit from Home-NIV. Patients presenting with hypoventilation are thought to suffer from an imbalance between increased inspiratory muscle load and reduced inspiratory muscle capacity.1 One major limitation for alveolar ventilation in advanced COPD with emphysema is hyperinflation-induced diaphragm shortening, which is associated with ineffective muscle function.1 The physiological background and types of respiratory failure associated with COPD are described in more detail elsewhere.1
Patient selection and timing of Home-NIV
A recently published online survey of physicians involved in the provision of Home-NIV revealed that COPD patients mainly benefit from NIV in terms of a subsequent reduction in hospital admissions, an improvement in quality of life, and relief of dyspnea.2 Furthermore, both recurrent exacerbations (>3) requiring NIV and failed weaning from inpatient NIV therapy were each found to constitute the most important reasons for implementing Home-NIV. Despite this, there is a large variability in the rate of NIV prescription for COPD patients among different countries.2 This variability is in line with that reported by the Eurovent Study (2001), which included 27,118 patients from 483 centers across Europe.4 Nevertheless, there is now increasing scientific evidence (see in the following paragraphs) to support a number of indications for Home-NIV in patients suffering from chronic hypercapnic COPD (Table 1).
  | Table 1 Recommendations for Home-NIV in chronic hypercapnic respiratory failure and COPD based on scientific as well as clinical-guided perspectives |
The indication for Home-NIV in the subgroup of COPD patients with stable chronic hypercapnic COPD has been a controversial topic over the last two decades.1 In three long-term studies published between 2000 and 2009, no clear benefits of NIV therapy were shown for COPD patients when compared with the effects of LTOT/standard therapy alone.1,11–13 Casanova et al (N=44) and Clini et al (N=86) also reported that COPD patients with moderate chronic hypercapnia did not gain any survival benefits from the introduction of Home-NIV.11,12 In a study by McEvoy et al (N=144), survival was found to be slightly improved by Home-NIV in comparison to standard therapy.13 However, this benefit was associated with reduced health-related quality of life (HRQL).13 All three studies investigated the effects of Home-NIV in a subgroup of COPD patients with a mean hypercapnia below 55 mmHg (7.33 kPa).11–13 By contrast, a more recent multicenter German study reported a substantial survival benefit for chronic hypercapnic COPD patients using Home-NIV in comparison to those undergoing standard therapy (including LTOT alone).7 This trial included patients with higher mean arterial pressure of carbon dioxide (PaCO2) levels of 59 mmHg (7.8 kPa) in the NIV group and 58 mmHg (7.7 kPa) in the control group.7 Furthermore, it was shown that when a multidisciplinary rehabilitation program for COPD patients with (moderate) chronic hypercapnic respiratory failure was supplemented with nocturnal NIV, there was an improvement in outcome in terms of exercise tolerance, HRQL, and lung function, in comparison to rehabilitation alone.8,14
This discrepancy in outcome might be explained by the following factors. First, it appears that severe hypercapnic patients benefit more from Home-NIV.1,3 Second, the provision of optimal standard care treatment (eg, a well-organized rehabilitation program) enhances the positive outcomes that are usually associated with nocturnal Home-NIV. Finally, the studies that showed positive outcomes used different approaches to ventilation, including those related to the settings and targets for reducing PaCO2 (see next section for more detail).
COPD patients who suffer from an acute exacerbation and hence require immediate mechanical ventilation generally have a poor prognosis.15 The readmission rate for COPD patients after an exacerbation with acute hypercapnic respiratory failure and the need for acute NIV therapy is reportedly around 35% after the first month and 70% after 4 months.16 In line with this limited prognosis, Titlestad et al reported that the 1-year survival rate in this subgroup of COPD patients is around 50%.17
In response to these poor outcome data, studies were initiated to investigate whether survival could be improved with the continuation of Home-NIV after an exacerbation.5,6,15 Struik et al investigated the effect of Home-NIV versus standard medical treatment in COPD patients with prolonged hypercapnia after acute respiratory failure requiring acute NIV therapy.5 A total of 201 patients with a PaCO2 level of >45 mmHg (6.0 kPa) after 48 hours of termination of acute NIV were randomized to either standard medical treatment or standard medical treatment in combination with Home-NIV. Baseline PaCO2 was 59.3 mmHg (7.9 kPa) in the Home-NIV group (N=101) and 57.8 mmHg (7.7 kPa) in the control group (N=100). Follow-up after 1 year demonstrated that in this subgroup of COPD patients, no improvements in the time until readmission or death were achieved by supplementing the treatment strategy with Home-NIV.5 Nevertheless, Home-NIV was capable of improving day- and night-time hypercapnia, and there was a trend toward an improvement in HRQL.5 In contrast to this, a recently published multicenter study in the UK showed that the initiation of Home-NIV following an acute exacerbation of COPD requiring acute NIV therapy was associated with a substantially better outcome.6 In this study, patients were included if they presented with a PaCO2 level of >53 mmHg (7.1 kPa) after 2–4 weeks of resolution of respiratory acidosis in the period following acute-NIV.6 In a similar paradigm to that used in the Dutch study,5 patients (N=116) were randomized to receive either standard medical treatment that included LTOT (N=59) or standard medical treatment/LTOT in combination with Home-NIV. Each of the two groups showed a mean daytime PaCO2 level of 59 mmHg (7.9 kPa). After a 12-month follow-up, patients who received Home-NIV in addition to LTOT experienced a longer time period until their next readmission or death (Home-NIV + LTOT: 4.3 months vs LTOT: 1.4).6 The main difference between the Dutch and the British studies was the time point at which the patient was recruited, and Home-NIV was initiated. Struik et al included patients after 48 hours of the acute event, whereas Murphy et al screened patients at a later time point, namely at around 2–4 weeks after resolution of respiratory acidosis.5,6 Patients from both studies showed a similar level of hypercapnia and respiratory failure type II at study initiation. Interestingly, however, Struik et al reported that a high number of patients in the standard treatment arm without Home-NIV (26%) become eucapnic within the first 3 months of follow-up.5 This difference in the timing of patient selection might be an explanation for the different outcomes, since initiation of Home-NIV with persistent hypercapnia at least 2 weeks after acute exacerbation of COPD demonstrated a better outcome.6
In addition to the aforementioned criteria for prescribing Home-NIV, physicians involved in the provision of Home-NIV in Europe suggested that one of the most important indications for long-term NIV in COPD patients is the failure to wean from acute NIV.2 Although scientific evidence for this particular subgroup is lacking, it was noted in one of the abovementioned studies6 that 252 (12%) out of the 2,021 patients screened for the study eventually dropped out due to the inability to wean from in-hospital NIV. In line with these findings, Schönhofer et al analyzed data from the German WeanNet register to show that out of 6,899 patients who underwent prolonged weaning from mechanical ventilation (registered between March 2008 and February 2014), 19.4% started NIV during the weaning process due to persistent respiratory failure (type II).18 Within this patient cohort, the COPD subgroup showed marginal weaning success and thus represented the subgroup with the highest rate of NIV prescription.18 Furthermore, recently published German guidelines recommend Home-NIV therapy for COPD patients after prolonged weaning from mechanical ventilation if the patient’s symptoms of hypoventilation and hypercapnia can only be controlled with continuous use of NIV following weaning from invasive mechanical ventilation.10 This subgroup of COPD patients who fail to wean from acute NIV is a topic that urgently requires further clinical investigation, since it is practiced in many countries across Europe without any scientific basis.
Overall, it would be an interesting topic to investigate cost-effectiveness for the health care system regarding introduction of NIV. However, there are currently no data available regarding this valuable topic and it would be difficult to compare this issue in regard to the divergence of health care systems and reimbursements from country to country. Nevertheless, in regard to the positive outcome in the aforementioned British trial6 with a longer time period until their next hospital readmission in patients with COPD following establishment of NIV, one might speculate a positive effect on costs for the health care system. But this remains speculative and needs further attention in future investigations.
Ventilator settings and compliance
Besides the abovementioned issues of patient selection, adequate establishment of ventilator settings and targets for Home-NIV are thought to play a substantial role in treatment success.1,19 Table 2 summarizes the ventilator settings, interface selection, and compliance data associated with the most important Home-NIV trials on chronic hypercapnic COPD patients;5–8,11–13 this summary demonstrates that different approaches to ventilator settings have been used over the last two decades (Table 2). The increase in inspiratory positive airway pressures (IPAPs) is particularly apparent. This aspect is also addressed in Figure 1, where the IPAP levels used in short- and long-term trials are presented in graph form. In line with an Australian study,13 initial studies used moderate IPAP levels with a mean of 12–14 cm H2O and pressure support modes in combination with a nasal mask (Table 2).11–13 In all three of these trials, the chronic hypercapnic COPD patient subgroup was represented by a mean hypercapnia level of less than 55 mmHg (7.33 kPa) and showed no clear overall gain in benefit from Home-NIV therapy, despite an acceptable level of tolerance to its daily use. By contrast, two more recent studies used a substantially different approach, with the higher IPAP levels of 22–24 cm H2O in combination with either a pressure-controlled ventilation mode or a pressure-support mode with higher backup rates (Table 2).6,7 Each of these studies showed a significant improvement in outcome following the application of Home-NIV, as already discussed.6,7 Based on this observation, one could conclude that a substantial improvement in alveolar ventilation is needed both for treatment success and a better outcome in chronic hypercapnic COPD patients.1
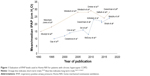  | Figure 1 Evaluation of IPAP levels used in Home-NIV for patients with chronic hypercapnic COPD. |
Using Home-NIV with the aim of achieving normocapnia (“high-intensity NIV”) in chronic hypercapnic COPD patients was first proposed by Windisch et al in 2009.23 The same research group from Freiburg, Germany, then carried out a randomized cross-over short-term trial to demonstrate that this novel approach using high-intensity NIV was better tolerated by patients and was also superior in controlling nocturnal hypoventilation compared with conventional NIV, where IPAP levels of ~15 cm H2O were used.11–13,19 It is also worth noting that there was a substantial difference in compliance (3.6 hours) in favor of high-intensity NIV.19 In line with this, Dreher et al showed in another study that sleep quality was not negatively influenced by high-intensity NIV when compared with the effects of a conventional NIV mode with lower IPAP levels.28 The results gained from these trials highlight the increasing trend toward the application of higher IPAP levels over the last two decades (Figure 1). Accordingly, Struik et al reported in their 2014 meta-analysis that higher IPAP levels, better compliance data, and higher baseline PaCO2 might contribute to improving PaCO2 outcome under Home-NIV therapy.3 This observation has been reinforced by positive results from more recent trials on the effects of NIV in COPD patients.3,6,7 Therefore, it has been proposed that improving elevated PaCO2 levels should form one of the main goals of Home-NIV.1,19
Regarding the application of increased IPAP levels, it should be noted that mechanical ventilation can affect cardiac output.15,29 An earlier physiological study reported that besides the positive effects of high-intensity NIV, it can also markedly reduce cardiac output, a factor that needs to be taken into consideration in patients with coexisting cardiac disease.30 On the other hand, the improvements conferred upon gas exchange by high-intensity NIV might be beneficial to the heart.15 This topic was addressed in a recent randomized-controlled feasibility study comparing the effects of high- vs low-intensity Home-NIV on cardiac output after 6 weeks of treatment.29 Here, cardiac output was assessed at baseline, at follow-up, and during NIV, as were gas exchange, lung function, and HRQL.29 The authors found no overall changes in patients (N=14) with respect to cardiac output or N-terminal pro b-type natriuretic peptide, although individual effects were observed, depending on the pressures applied or the coexistence of heart failure.29 Nevertheless, cardiac output can be reduced by the application of higher IPAP levels, especially in patients with preexisting heart failure and should therefore be applied with caution.29,30 Despite this, there has so far been no reason for withholding Home-NIV therapy from chronic hypercapnic COPD patients due to concerns about adverse cardiac outcome.29
Next to IPAP levels, the mode of ventilation used in Home-NIV is an interesting aspect that has differed across countries over the last two decades.2,4 Nearly half the physicians who prescribed Home-NIV reported using techniques that were aimed at maximally reducing elevated PaCO2 levels, by the way of pressure-controlled or pressure-support ventilation modes with high inspiratory support of more than 20 cm H2O.2 The evolution of this treatment approach is in line with the aforementioned trend displayed in Figure 1 and Table 2. However, despite this trend, according to the European survey by Crimi et al, pressure-support ventilation with low-intensity settings of less than 20 cm H2O remained the most-prescribed technique.2
Nowadays, volume-controlled ventilation only has a limited use in Home-NIV compared to its role 20 years ago.2,4 However, hybrid modes with target-volume settings on top of a pressure preset mode have become more popular over the last few years and have been the focus of several studies investigating the effects of Home-NIV on chronic hypercapnic COPD.31–35 All of these studies investigated patients with chronic hypercapnic COPD who were subjected to higher levels of IPAP, in line with the recommendation by Windisch et al.23 Three out of the four studies investigated patients who were already familiar with Home-NIV,31–33 while the remaining study focused on the new hybrid mode in a Home-NIV-naive COPD subgroup.34 The randomized crossover trials investigating COPD patient subgroups who were already familiar with Home-NIV showed that adding target volume to pressure-preset NIV yielded neither benefits nor disadvantages with respect to sleep quality measured by polysomnography, HRQL, compliance, or gas exchange monitoring.31–33 However, patients who used target volume Home-NIV rated their own sleep quality at home as more restful compared to patients using the conventional NIV mode in one study.33 These results are corroborated by a randomized, parallel-group study of a COPD cohort naive to Home-NIV, where target-volume Home-NIV vs conventional NIV showed similar effects (eg, improvements in gas exchange monitoring, exercise capacity, compliance, pulmonary function, and HRQL).34 However, one advantage of target-volume NIV was that fewer titration days (secondary endpoint) were needed with this treatment approach (3.3±1.6 days) compared to the number required with conventional NIV (5.2±2.8 days).34 In light of this, target-volume NIV might serve as a means for faster establishment of Home-NIV in chronic hypercapnic COPD patients, although this remains speculative and needs to be investigated further.
Selection of interface
In contrast to the topic of ventilator settings, the basis for selecting the appropriate ventilation interface has only so far received limited scientific attention.36,37 This is somewhat surprising because the type of interface has been reported to be crucial for the success of NIV therapy in the acute and chronic settings.38 In most of the studies discussed here, mask selection was based on patient comfort and/or the recommendation provided by the supervising ventilation center (Table 2). There is a broad variety of interfaces available, including nasal masks, oronasal masks, total face masks, or mouth pieces, depending on patient needs and ventilation strategies.36 Nowadays, most of the interfaces are commercially manufactured, with the use of custom-made masks being less frequent. In addition, different types of masks are available with respect to the type of ventilator and circuit used for Home-NIV. Varieties of interfaces, including their advantages and disadvantages, are described in more detail elsewhere.36 The Eurovent Trial that was published 20 years ago revealed that the predominant type of interface for patients using chronic ventilatory support was the nasal mask.4 This is in clear contrast to today, where prescribers in Europe reported using oronasal or full-face masks more often.2 In the Home-NIV studies outlined in Table 2 and Figure 1, a clear trend toward the more frequent use of masks that cover the nose and mouth can be seen. This development is likely attributable to the switch in ventilator settings (Table 2). Minor IPAP levels were generally applied at around the time of the Casanova et al, Clini et al, and McEvoy et al trials, and nasal masks served as the common interface, whereas later studies using higher IPAP levels were most likely to enlist the use of oronasal- or full-face masks (Table 2). As stated earlier, this decision was mainly triggered by patient comfort and/or the recommendation of the supervising ventilation center. Although the scientific basis for interface selection is lacking, a recent single-center study in Germany investigated the distribution of interfaces among chronic hypercapnic COPD patients who were prescribed high-intensity Home-NIV.37 It was found that the majority (77%) of study patients (N=123) used a full-face mask, while only 23% used a nasal mask. Ventilator settings corresponded to those used in the Köhnlein et al study, which showed positive survival benefits in this particular subgroup.7,37 Figure 2 represents the distribution of oronasal and nasal masks among different subgroups of COPD patients who received Home-NIV therapy.37 In particular, patients with the highest IPAP levels, a lower body mass index, or in whom Home-NIV was initiated following acute exacerbation of their COPD were those with the highest degree of oronasal mask use.37 It is also important to note that there is a clear trend toward the increased use of masks covering the nose and mouth, as the practical application of IPAP levels rises (Table 2).2,37 However, further research is needed to elucidate the role of the interface in Home-NIV treatment of COPD and other subgroups of patients.
  | Figure 2 Distribution of oronasal (FFMs, dark gray) and nasal (NM, light gray) masks in different subgroups of COPD patients receiving Home-NIV therapy. |
Conclusion
Home-NIV for patients with end-stage COPD has become a well-established form of therapy over the last few decades, despite a lack of consensus among the corresponding scientific literature. However, recent research trials have provided evidence that Home-NIV is associated with long-term survival benefits as well as improvements in HRQL, gas exchange, and lung function. These positive results were first observed in the stable hypercapnic COPD patient subgroup. Accordingly, a current study reported similar positive effects of Home-NIV therapy in this particular subgroup of COPD patients who suffer from an acute exacerbation that requires mechanical ventilation therapy and is accompanied by persistent hypercapnia – a generally severe event that is associated with a poor prognosis. Furthermore, there is a substantial number of patients who cannot be weaned from acute mechanical ventilation and hence qualify for Home-NIV. However, this indication needs further attention, since scientific evidence is lacking. A treatment strategy with higher inspiratory pressures aimed at reducing elevated carbon dioxide levels appears to form the basis of therapeutic success, while a clear trend toward the use of oronasal masks is becoming apparent. New studies in this area are warranted to better understand the pathophysiological changes occurring in patients using long-term ventilation. Focus should also be placed on selecting the most eligible candidates for Home-NIV, taking into account – but not solely focusing on – the degree of hypercapnia.
Acknowledgment
We acknowledge Dr Sandra Dieni for helpful comments on the manuscript.
Disclosure
The Cologne Study Group (JHS, JC, FSM, SBS, and WW) received an open research grant from Weinmann/Germany, Vivisol/Germany, Heinen und Löwenstein/Germany, and VitalAire/Germany. FSM, JC, JHS, and SBS received personal travel grants from companies dealing with LTOT and Home-NIV. FSM, WW and JHS received speaking fees from companies dealing with LTOT and Home-NIV. MLD reported receiving research grants from Philips/Respironics and ResMed, and speaking fees from Vivisol Nederland BV. PJW reports grants and personal fees from Philips Respironics, ResMed, Vivisol, grants from MedicqTEFA and Air Liquide, outside the submitted work. The authors report no other conflicts of interest in this work.
References
Windisch W, Storre JH, Köhnlein T. Nocturnal non-invasive positive pressure ventilation for COPD. Expert Rev Respir Med. 2015;9(3):295–308. | ||
Crimi C, Noto A, Princi P, et al. Domiciliary non-invasive ventilation in COPD: an international survey of indications and practices. COPD. 2016;13(4):483–490. | ||
Struik FM, Lacasse Y, Goldstein RS, Kerstjens HA, Wijkstra PJ. Nocturnal noninvasive positive pressure ventilation in stable COPD: a systematic review and individual patient data meta-analysis. Respir Med. 2014;108(2):329–337. | ||
Lloyd-Owen SJ, Donaldson GC, Ambrosino N, et al. Patterns of home mechanical ventilation use in Europe: results from the Eurovent survey. Eur Respir J. 2005;25(6):1025–1031. | ||
Struik FM, Sprooten RT, Kerstjens HA, et al. Nocturnal non-invasive ventilation in COPD patients with prolonged hypercapnia after ventilatory support for acute respiratory failure: a randomised, controlled, parallel-group study. Thorax. 2014;69(9):826–834. | ||
Murphy PB, Rehal S, Arbane G, et al. Effect of home noninvasive ventilation with oxygen therapy vs oxygen therapy alone on hospital readmission or death after an acute COPD exacerbation: a randomized clinical trial. JAMA. 2017;317(21):2177–2186. | ||
Köhnlein T, Windisch W, Köhler D, et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med. 2014;2(9):698–705. | ||
Duiverman ML, Wempe JB, Bladder G, et al. Two-year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease patients: a randomized controlled trial. Respir Res. 2011;12:112. | ||
Windisch W, Walterspacher S, Siemon K, Geiseler J, Sitter H; German Society for Pneumology. Guidelines for non-invasive and invasive mechanical ventilation for treatment of chronic respiratory failure. Published by the German Society for Pneumology (DGP). Pneumologie. 2010;64(10):640–652. | ||
Schönhofer B, Geiseler J, Dellweg D, et al. S2k-Guideline “Prolonged Weaning”. Pneumologie. 2015;69(10):595–607. | ||
Casanova C, Celli BR, Tost L, et al. Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest. 2000;118(6):1582–1590. | ||
Clini E, Sturani C, Rossi A, et al; Rehabilitation and Chronic Care Study Group, Italian Association of Hospital Pulmonologists (AIPO). The Italian multicentre study on noninvasive ventilation in chronic obstructive pulmonary disease patients. Eur Respir J. 2002;20(3):529–538. | ||
McEvoy RD, Pierce RJ, Hillman D, et al; Australian trial of non-invasive Ventilation in Chronic Airflow Limitation (AVCAL) Study Group. Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax. 2009;64(7):561–566. | ||
Duiverman ML, Wempe JB, Bladder G, et al. Nocturnal non-invasive ventilation in addition to rehabilitation in hypercapnic patients with COPD. Thorax. 2008;63(12):1052–1057. | ||
Duiverman ML, Windisch W, Storre JH, Wijkstra PJ. The role of NIV in chronic hypercapnic COPD following an acute exacerbation: the importance of patient selection? Ther Adv Respir Dis. 2016;10(2):149–157. | ||
Chu CM, Chan VL, Lin AW, Wong IW, Leung WS, Lai CK. Readmission rates and life threatening events in COPD survivors treated with non-invasive ventilation for acute hypercapnic respiratory failure. Thorax. 2004;59(12):1020–1025. | ||
Titlestad IL, Lassen AT, Vestbo J. Long-term survival for COPD patients receiving noninvasive ventilation for acute respiratory failure. Int J Chron Obstruct Pulmon Dis. 2013;8:215–219. | ||
Schönhofer B, Geiseler J, Herth F, Jany B, Pfeifer M, Westhoff M; WeanNet Study Group. WeanNet: the network of weaning units of the DGP (Deutsche Gesellschaft für Pneumologie und Beatmungsmedizin) – results to epidemiology an outcome in patients with prolonged weaning. Dtsch Med Wochenschr. 2016;141(18):e166–e172. German [with English abstract]. | ||
Dreher M, Storre JH, Schmoor C, Windisch W. High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax. 2010;65(4):303–308. | ||
Strumpf DA, Millman RP, Carlisle CC, et al. Nocturnal positive-pressure ventilation via nasal mask in patients with severe chronic obstructive pulmonary disease. Am Rev Respir Dis. 1991;144(6):1234–1239. | ||
Meecham Jones DJ, Paul EA, Jones PW, Wedzicha JA. Nasal pressure support ventilation plus oxygen compared with oxygen therapy alone in hypercapnic COPD. Am J Respir Crit Care Med. 1995;152(2):538–544. | ||
Windisch W, Kostić S, Dreher M, Virchow JC Jr, Sorichter S. Outcome of patients with stable COPD receiving controlled noninvasive positive pressure ventilation aimed at a maximal reduction of Pa(CO2). Chest. 2005;128(2):657–662. | ||
Windisch W, Haenel M, Storre JH, Dreher M. High-intensity non-invasive positive pressure ventilation for stable hypercapnic COPD. Int J Med Sci. 2009;6(2):72–76. | ||
Salturk C, Karakurt Z, Takir HB, et al. Comparison of exercise capacity in COPD and other etiologies of chronic respiratory failure requiring non-invasive mechanical ventilation at home: retrospective analysis of 1-year follow-up. Int J Chron Obstruct Pulmon Dis. 2015;10:2559–2569. | ||
Duiverman ML, Huberts AS, van Eykern LA, Bladder G, Wijkstra PJ. Respiratory muscle activity and patient-ventilator asynchrony during different settings of noninvasive ventilation in stable hypercapnic COPD: does high inspiratory pressure lead to respiratory muscle unloading? Int J Chron Obstruct Pulmon Dis. 2017;12:243–257. | ||
Gay PC, Hubmayr RD, Stroetz RW. Efficacy of nocturnal nasal ventilation in stable, severe chronic obstructive pulmonary disease during a 3-month controlled trial. Mayo Clin Proc. 1996;71(6):533–542. | ||
Sin DD, Wong E, Mayers I, et al. Effects of nocturnal noninvasive mechanical ventilation on heart rate variability of patients with advanced COPD. Chest. 2007;131(1):156–163. | ||
Dreher M, Ekkernkamp E, Walterspacher S, et al. Noninvasive ventilation in COPD: impact of inspiratory pressure levels on sleep quality. Chest. 2011;140(4):939–945. | ||
Duiverman ML, Maagh P, Magnet FS, et al. Impact of high-intensity-NIV on the heart in stable COPD: a randomised cross-over pilot study. Respir Res. 2017;18(1):76. | ||
Lukácsovits J, Carlucci A, Hill N, et al. Physiological changes during low- and high-intensity noninvasive ventilation. Eur Respir J. 2012;39(4):869–875. | ||
Oscroft NS, Ali M, Gulati A, et al. A randomised crossover trial comparing volume assured and pressure preset noninvasive ventilation in stable hypercapnic COPD. COPD. 2010;7:398–403. | ||
Storre JH, Matrosovich E, Ekkernkamp E, et al. Home mechanical ventilation for COPD: high-intensity versus target volume noninvasive ventilation. Respir Care. 2014;59(9):1389–1397. | ||
Ekkernkamp E, Storre JH, Windisch W, Dreher M. Impact of intelligent volume-assured pressure support on sleep quality in stable hypercapnic chronic obstructive pulmonary disease patients: a randomized, crossover study. Respiration. 2014;88(4):270–276. | ||
Oscroft NS, Chadwick R, Davies MG, Quinnell TG, Smith IE. Volume assured versus pressure preset non-invasive ventilation for compensated ventilatory failure in COPD. Respir Med. 2014;108(10):1508–1515. | ||
Arellano-Maric MP, Gregoretti C, Duivermann M, Windisch W. Long-term volume-targeted pressure-controlled ventilation: sense or nonsense? Eur Respir J. 2017;49(6):pii:1602193. | ||
Storre JH, Schönhofer B. Noninvasive mechanical ventilation in chronic respiratory failure: ventilators and interfaces. Eur Respir Mon. 2008;41:319–337. | ||
Callegari J, Magnet FS, Taubner S, et al. Interfaces and ventilator settings for long-term noninvasive ventilation in COPD patients. Int J Chron Obstruct Pulmon Dis. 2017;12:1883–1889. | ||
Elliott MW. The interface: crucial for successful noninvasive ventilation. Eur Respir J. 2004;23(1):7–8. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

