Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
HIV/AIDS Related Knowledge of University Students in Southeast Ethiopia: A Cross-Sectional Survey
Authors Kene C, Deribe L , Adugna H , Tekalegn Y , Seyoum K , Geta G
Received 7 January 2021
Accepted for publication 19 May 2021
Published 17 June 2021 Volume 2021:13 Pages 681—690
DOI https://doi.org/10.2147/HIV.S300859
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bassel Sawaya
Chala Kene,1 Leul Deribe,2 Haweni Adugna,2 Yohannes Tekalegn,3 Kenbon Seyoum,1 Girma Geta1
1Department of Midwifery, School of Health Science, Madda Walabu University, Goba, Ethiopia; 2Department of Midwifery, Tikur Anbessa Referral Hospital, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Public Health, School of Health Sciences, Madda Walabu University, Goba, Ethiopia
Correspondence: Chala Kene Email [email protected]
Purpose: University students are often a sexually active group that is at risk of acquiring and transmitting HIV. This risk depends on their level of knowledge towards the disease. Hence, HIV/AIDS related knowledge represents the acquisition of scientific facts and information regarding the symptoms, way of transmission, adverse consequences, and prevention strategies of the disease. Therefore, this study aimed to assess level of HIV/AIDS related knowledge among regular undergraduate students of Madda Walabu University, Southeast Ethiopia.
Methods: A cross-sectional study was conducted from February 10– 25, 2020. A simple random sampling technique was employed to select the study participants. Data were entered to Epi Data version 4.6.0.2 and analyzed using SPSS version 26 software. A bivariate and multivariable binary logistic regression model was used to identify factors associated with level of HIV/AIDS knowledge. Odds ratio with 95% confidence interval and p-value< 0.05 was used to declare statistical significance.
Results: A total of 442 study participants were included in the study. The level of HIV/AIDS knowledge among study participants was found to be 51.4%. Health science students [AOR=16.28 (8.21– 32.28)], being in year III and above [AOR=5.34 (2.92– 9.76)] and having monthly stipend > 300 birr from parents and relatives [AOR=2.70 (1.34– 5.48)] had a higher odds of a good level of HIV/AIDS knowledge.
Conclusion: Nearly half of the students had a poor level of HIV/AIDS knowledge. Field of study, year of the study, and monthly income were significantly associated with level of HIV/AIDS related knowledge. University-based HIV/AIDS education considering year of study has to be given, and risk reduction on focusing on behavioral change intervention are recommended.
Keywords: HIV/AIDS, knowledge, university students, risky behavior
Introduction
The world has entered the fourth decade of the Acquired Immunodeficiency Syndrome (AIDS) epidemic.1 A global HIV/AIDS disease burden report published in 2019 shows there were 1,940,000 [966,000 Female, 976,000 Male], 1,210,000 [723,000 Female, 487,000 Male] and 14,500 [9,080 Female, 5,400 Male] new infections globally, in Sub-Saharan Africa, and in Ethiopia, respectively.2 The new infection rate is projected to rise from 250,000 in 2015 to nearly 400,000 among adolescents annually by 2030 if progress in reaching adolescents stalls globally.3
According to a report from a Ethiopian demographic health survey (EDHS) data of 2016, in Ethiopia around 24% of young women and 39% of young men aged 15–24 years have knowledge about HIV prevention.4 However, studies among university students reported a Sero-prevalence of HIV/AIDS infection ranges between 0.36–1.2%.5,6 Recent preliminary reports indicate that the risky behaviors among university students are increasing at an alarming rate.7 Sexually transmitted infections including HIV/AIDS are high among students having poor knowledge.8 University students are at higher risk of engaging in risky sexual behavior, especially if they are under the influence of alcohol or drugs and lack the necessary maturity in handling negative peer pressure.9
Level of personal knowledge is considered essential for acquiring optimum health, in which, in this context, HIV/AIDS knowledge represents the acquisition of scientific facts and information regarding the symptoms, way of transmission, adverse consequences, and prevention strategies of the disease.10 The mean level of HIV/AIDS knowledge of undergraduate students is not universal, it varies among universities. For instance, studies from Historically Black College among African-American undergraduate students university (America) reported a high (96.5%) level of knowledge11 and Bahir Dar university (Ethiopia) reported a relatively low (45.7%) level of knowledge.12 Other studies found the level of HIV/AIDS knowledge to be from 61–66%.12–15
In Ethiopia, interventions targeting the general public do not directly respond to higher education institution students’ needs which have an elevated risk for becoming infected with HIV.17 Perhaps most importantly, it has become increasingly clear that preventing the transmission and the acquisition of HIV must focus upon promoting knowledge and bringing behavioral changes.1
Since university students are a valuable resource of society, it is imperative that they are armed with the HIV/AIDS information to protect themselves from falling prey to this infectious disease. They may have shorter relationships and more partners, or engage in risky sexual practices. Therefore, assessing the level of knowledge of HIV/AIDS among university students will provide vital information on the students’ knowledge and possible misconceptions of the disease. Hence, this study aimed to assess level of HIV/AIDS related knowledge and its associated factors among regular undergraduate students of Madda Walabu University, southeast Ethiopia.
Methods and Materials
Study Design and Period
An institutional cross-sectional study design was conducted from February 10 to 25, 2020.
Study Setting
The study was conducted in Madda Walabu University on undergraduate regular students. The university was established in 2006 and located in Bale Zone, in the town of Robe, about 430 km away from the capital city, Addis Ababa. According to the data obtained from the registrar record office, currently the university has 50 undergraduate programs, eight schools, one institute, and two colleges of health sciences. It has three campuses, Robe, Goba and Shashamane College of Health Sciences. During the data collection, the university had a total number of 9,253 regular undergraduate students.18
Sample Size Determination
Sample size was calculated using a single population proportion formula, assuming a 49.37% proportion of knowledge on HIV/AIDS,19 95% confidence interval (CI), and 5% margin of error. n= (1.96)2 0.5 (0.5)/(0.05)2=384. After adding a 15% non-response rate, the final sample size was found to be 442.
Sampling Procedure
First, Madda Walabu University was selected from public universities found in Ethiopia. Then the identification of the number of the campus, colleges, and number of students in each campus was checked from university registrar record office by principal investigator. After that samples were allocated for each campus accordingly (Goba College of health science and Shashamane, and Robe campus). Then from the total eight schools in Robe campus, six schools were selected randomly. Then students were stratified for selected schools and colleges of health sciences. After that students were further stratified in class year under selected schools and colleges of health science. Finally, simple random sampling was implemented using students list obtained from registrar as sampling frame per selected departments.
Study Variables and Outcomes
Sociodemographic and risk behavior variables were study variables whereas level of HIV/AIDS related knowledge was outcome variable. A series of 20 questions related with HIV/AIDS were asked. Study participants who scored at least 50% of the knowledge questions were categorized as having “good knowledge” and else were categorized as having poor knowledge.
Data Collection Tools and Procedures
A self-administered English language questionnaire was used to collect data. Four diploma nurses and three university instructors were assigned as data collectors and supervisors, respectively. The data collection tool adopted from a previous study pertinent to the topic, with well validated instruments of internal consistency reliability analysis of HIV-KQ (Knowledge Question) (α=0.91)20 and internal consistency reliability as measured by Kuder-Richardson formula (KR-20)(α=0.58) (n=483) and test–re-test=0.59 (n=39).21 The ensuing knowledge section, based on the HIV-KQ-20 scale, consisted of 20 questions related to HIV, modes of its transmission, and prevention. For each of the 20 Yes/No, HIV-related questions, a score of 1 was assigned to each “correct” answer, whereas a score of 0 was assigned to “incorrect” answers and coded. Questions with opposite statements were recoded. No deductions were made for any answer. Assessments were based on the analysis of the summation of these scores, which had a possible range of 0–20, whereby scores greater than or equal to mean indicates good knowledge of HIV, else were considered as having poor knowledge of HIV. In addition, the tool for assessing risk behavior adopted from literature reviewed pertinent to the topic20,21 and from standard questionnaires designed by Family Health International for Behavioral Surveillance Survey (BSS) on high-risk behavior for HIV-124 and contextualized.
Data Quality Assurance
Pretest was done on 5% of the sample size in the non-selected department of MWU, in order to check the clarity of the tool and allocate time needed for filling the questionnaires. Training was provided for data collectors and supervisors. Through the course of data collection, the data collectors were supervised and there was regular phone contact between principal investigator and data collectors to know the data collection progress. Incomplete data were discarded and considered as non-response. The data was said to be incomplete when half of the items in each section were not filled. Therefore, 12 questionnaires were discarded based on this criterion. Finally, the collected data was reviewed and checked for full completeness before data entry.
Data Processing and Analysis
The data was entered to Epi Data version 4.6.0.2 and coded. After that it was exported to SPSS version 26 and cleaned before analysis. Descriptive statistics like frequency, percentage, and mean was computed for the variables. The results of the study were presented using tables, graphs, charts, and text, based on the data obtained. Statistical significance and strength of the association between independent variables and the outcome variable was measured by using a logistics regression model. A variable with p-value of less than 0.2 during bivariate binary logistic regression analysis was transferred to a multivariable binary logistics regression model to adjust for possible confounders. Adjusted odds ratios (AOR) with their 95% confidence intervals were used to determine the presence and strength of associations. Enter method was used in the final regression model. P-value<0.05 was used to declare statistical significance.
Ethical Consideration
Ethical approval was obtained from the ethical review committee of the Department of Midwifery, school of Nursing and Midwifery Institutional Review Board, University of Addis Ababa, and IRB gave protocol number of A023/20/SNM for this work. Permission was obtained from MWU management and respective schools. Voluntary written consent was obtained from each study participant and the participants were informed about the purpose of the study. To protect students’ confidentiality and increase chances of releasing honest information, questionnaires were kept anonymous and the class was designed so students could never read over others’ shoulder. This study was conducted in accordance with the Declaration of Helsinki.
Results
Of the total sample size, 430 study participants completed the questionnaire, yielding a response rate of 97%. The remaining 12 (3%) responses were excluded from analysis due to incompleteness of the data.
Socio-Demographic Characteristics of the Respondents
The mean age of the participants was 21.93 years with a standard deviation of 1.91 years. The study participant’s age ranged from 18–28 years. Three hundred and eight (71.6%) of the participants were Oromo by ethnicity, followed by Amhara (73, 17.0%). Of the total respondents, 290 (67.4%) were male, 314 (73.0%) belonged to departments of non-health, and 119 (27.7%) were year II students (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Regular Undergraduate Students of Madda Walabu University Bale Zone, Southeast Ethiopia February 10–25, 2020 |
Risk Behavior of the Respondents
Regarding substance use, 100 (23.3%), 78 (18.1%), and 45 (10.5%) participants had ever drunk alcohol, chewed chat, and smoked cigarettes, respectively. During staying on campus, 57 (13.3%) participants had tried different ranges of drugs in which 22 (5.1%) tried cocaine, 20 (4.7%) tried shisha/gaya, and 15 (3.5%) had tried hashish (Table 2).
 |
Table 2 Substance Use Risk Behaviors for Having HIV/AIDS among Regular Undergraduate Students of Madda Walabu University Bale Zone, Southeast Ethiopia February 10–25, 2020 |
Among the total respondents, around 262 (60.9%) were had been tested for HIV, of which 95 (22.1%) tests were done more than a year ago (Figure 1). Of 160 (37.2%) participants who had ever sexual intercourse, only 30 (7%) of them had used a condom in their first sexual contact. The mean ages at first sexual intercourse of the participants were 18.21 years, with a standard deviation of 2.11 years, in which it was 18.55±2.11 and 17.28±1.89 for males and females, respectively. Regarding sexual partners, 42 (9.8%) participants had more than two sexual partners in their lifetime and 11 (2.6%) had more than two sexual partners during the study time. Among participants with a history of sexual intercourse, 23 (5.3%) reported having sex after drinking alcohol and 13 (3.0%) reported having sex after using psychoactive drugs (Table 3).
 |
Table 3 Risky Sexual Behaviors for HIV Infection aong Regular Undergraduate Students of Madda Walabu University Bale Zone, Southeast Ethiopia February 10–25, 2020 |
 |
Figure 1 HIV test characteristics of regular undergraduate students of Madda Walabu University, Southeast Ethiopia, 2020. |
HIV/AIDS Knowledge of the Participants
The sum of questions was obtained to range from 4–20, with mean HIV/AIDS knowledge of 13.60 and SD of 3.74. Of the total participants, only 23 participants answered all questions correctly.
Of the total participants, around 344 (80.0%) respondents answered “correctly” to the question that asked if condoms are 100% effective in preventing HIV. In addition, 304 (70.7%) participants answered “correctly” to the question that asked if they can get HIV from a mosquito bite, and almost 70% of the respondents (298, 69.3%) answered correctly the question which asked if all pregnant women infected with HIV will have babies born with HIV/AIDS (Table 4).
 |
Table 4 HIV/AIDS Knowledge among Regular Undergraduate Students of Madda Walabu University Bale Zone, Southeast Ethiopia February 10–25, 2020 (n=430) |
As described in Figure 2, nearly half (209, 48.6%) of the respondents had a poor level of knowledge about HIV/AIDS.
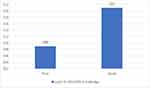 |
Figure 2 Level of HIV/AIDS Knowledge among regular undergraduate students of Madda Walabu University Bale Zone, Southeast Ethiopia, 2020. |
Factors Associated with Level of HIV/AIDS Related Knowledge
After adjusting for confounders, the field of study, year of study, and monthly income from the parent and relatives were found to be statistically significant predictors of HIV/AIDS related knowledge.
As presented in Table 5, health science students had 16-times (AOR=16.28. 95% CI=8.21–32.28) higher odds of HIV/AIDS knowledge. In addition, year III and above students were 5-times more likely to have good HIV/AIDS knowledge compared to year II students (AOR=5.34, 95% CI=2.92–9.76). Furthermore, students who had a monthly income >300 from the parents and relatives were 2.7-times more likely to have good HIV/AIDS knowledge (AOR=2.70; 1.34–5.48).
Discussion
This study has assessed the level of HIV/AIDS knowledge and associated factors among regular undergraduate students of Madda Walabu University. The finding of this study revealed that 51.4% of respondents were knowledgeable about HIV/AIDS in the study area. This finding is higher than in a study conducted at Bahir Dar university (45.7%),12 but lower than the study conducted at Dilla (53%),10 Addis Ababa (66%),16 Malaysia (64%),13 United Arab Emirates (61%),14 Turkey university (61%),15 and Historically Black College and University (96.5%).11 The difference in the finding may be due to a difference in assessment tools and population sample used. This further may be due to a difference in health education regarding HIV/AIDS and ways of delivering the education. For instance, in developed countries probably there was an active involvement of governmental and non-governmental organizations in HIV/AIDS related issues (education, providing different training, etc.), resulting in a higher level of knowledge. However, from my observation in developing countries like Ethiopia there is a limited involvement of the non-governmental organization, in which government mainly take the responsibility related issues of HIV/AIDS result in limited accessibility. Furthermore, in Ethiopia the reason why there was a discrepancy in level of HIV/AIDS knowledge among different university students was supposed to be due to differences in characteristics of the participants and differences in access and activeness of HIV/AIDS related programs implemented in these universities. In the study area, even if there is a club and office work on HIV/AIDS related issues, it still needs attention to be actively involved in health education regarding HIV/AIDS and fulfil the needs of the university students in all aspects.
The present study revealed that health science students were 16-times more likely to have good knowledge of HIV/AIDS compared to non-health science students. This finding is in line with a study conducted in Addis Ababa University (Ethiopia) in which students enrolled in health departments were almost 3-times more knowledgeable than students in non-health departments,16 and a related study conducted at a university in Turkey which found that students involved in health fields had higher HIV/AIDS knowledge compared to their counterparts.23 The probable reason may be that health science students were more informed about reproductive health and could get HIV/AIDS education in their courses. This could be better explained due to the fact that the curriculum of health science programs incorporated facts about infectious diseases in general and HIV/AIDS in particular.
In this study participants earning >300 birr monthly stipend from their families and relatives were found to be almost 3-times more likely to have good HIV/AIDS related knowledge. This finding resembles the study conducted in the university of Malaysia in which students from a family of high monthly income were found to be more knowledgeable about HIV/AIDS13 and oanther related study conducted in Turkey university students who reported a positive correlation between HIV/AIDS preventive self-efficacy and monthly stipend level.23 This may be due to participants from a family of high income being exposed most of the time to other extra sources of information and supportive reading materials which is the alternative source of information for HIV/AIDS education. This could be better explained due to students who were earning less money not being able to watch alternative source information (like youtube) because of its charges being more than the income they get from their family and relatives.
In this study students in year III and above were found to be 5-times more likely to had good HIV/AIDS knowledge compared to year II. This is supported by a study conducted among Wolkite University students in which junior students had significantly lower odds of being knowledgeable related to HIV/AIDS than their seniors. The possible reason may be that health students took courses related to infectious disease sand HIV infection particularly in most cases if they reached year III and above according to the curriculum, and non-health science students may access more information and some training regarding this infection as the year of study advanced even if there was no course entitled with infectious disease and HIV infection in their curriculum. Another reason may be that most of the time students above year III may be exposed to the practical attachment, mainly in the department of health, in which it helps to increase their knowledge related to HIV/AIDS since they face cases in the hospital and may involve themselves in health education given in health facilities.
Strengths and Limitations of the Study
As with all other research, this research had certain strengths and limitations. The study carefully used an appropriate design to answer the research question. Data was carefully analyzed and interpreted. As limitations, the study was restricted to local (only university level), which decreases its representativeness because it was not done in the general population. Since this study was a cross-section study design, the nature of the study may be difficult to ascertain the causal relationship between the study variables.
Conclusion
In this study area, nearly half of the students had a poor level of HIV/AIDS related knowledge. The field of study, year of the study, and monthly income were associated with level of HIV/AIDS knowledge. To improve the students’ level of knowledge related to HIV/AIDS; specified, focused, continued, and strengthened, university-based HIV/AIDS education especially targeting year of study has to be given. In addition, supporting by offering reading materials for students from poor family and risk reduction on behavior change focused intervention are recommended.
Abbreviations
WHO, World Health Organization; EDHS, Ethiopia Demographic and Health Survey; KQ, knowledge question; NASTAD, National Alliance of State and Territorial AIDS Directors; UNICEF, United Nations Children’s Fund; USAID, United States Agency for International Development; SPSS, Statistical Package of Social Science; CI, confidence interval; COR, crude odds ratio; AOR, adjusted odds ratio; AAU, Addis Ababa University; MWU, Madda Walabu University.
Data Sharing Statement
The data set analyzed during the current study is available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to thank the participants in this study, data collectors, and supervisors for all their cooperation. We would like to thank Addis Ababa University for funding.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. UNAIDS. World AIDS day report. 2012.
2. Frank TD, Carter A, Jahagirdar Det al. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980 – 2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet. 2019;18(19):1–29.
3. UNICEF. Annual results report humanitarian action. 2016; Available from: https://www.unicef.org/publicpartnerships/files/2016arr_humanitarianaction(1).pdf%0A.
4. Agency CS. Ethiopia Demgraphic and Health Survey; 2016.
5. Zewdie YG, Tilahun AT, Alamirew BA. Assessment of sero-prevalence of HIV and associated factors among Debre Berhan University Students, Ethiopia. Clin Med Res. 2019;8(2):47–52. doi:10.11648/j.cmr.20190802.13
6. Mulu W, Abera B, Yimer M. Prevalence of human immunodeficiency virus infection and associated factors among students at Bahir Dar University. Ethiop J Health Dev. 2014;28(3):170–177.
7. NASTAD. University HIV and STI Prevention University Package Implementation Guide, Ethiopia; 2012.
8. Kassie BA, Yenus H, Berhe R, Kassahun EA. Prevalence of sexually transmitted infections and associated factors among the University of Gondar students, Northwest Ethiopia: a cross-sectional study. Reprod Health. 2019;16(1):1–8. doi:10.1186/s12978-019-0815-5
9. CDC Vital signs. HIV Among Youth in US November; 2012.
10. Gemeda TT, Gandile AU, Bikamo DS. HIV/AIDS knowledge, attitude university students, Ethiopia and practice among dilla. Afr J Reprod Health. 2017;21(3):49–61. doi:10.29063/ajrh2017/v21i3.4
11. Andrew PO, Bhuiyan A, Mawson A, Buxbaum SG, Sung JH, Shahbazi M. HIV/AIDS knowledge of undergraduate students at a Historically Black College and University. MDPI Dis. 2018;6(98):1–8.
12. Mulu W, Abera B, Yimer M. Knowledge, attitude and practices on HIV/AIDS among students of Bahir Dar University. Sci J Public Heal. 2014;2(2):78–86.
13. Talwar P, Fadzil M. Assessment of HIV knowledge among university students using the HIV-KQ-18 scale: a cross-sectional study. South East Asia J Public Health. 2015;5(1):33–38. doi:10.3329/seajph.v5i1.24849
14. Haroun D, Saleh OE, Wood L, Mechli R, Marzouqi NA. Assessing knowledge of, and attitudes to, HIV/AIDS among University Students in the United Arab Emirates. PLoS One. 2016;11(2):2. doi:10.1371/journal.pone.0149920
15. Maimaiti N, Tekin HHSM. Level of knowledge and attitude towards HIV/AIDS among undergraduate students in Konya, Turkey. J Community Med Health Educ. 2018;8:4.
16. Woldeyohannes D, Asmamaw Y, Sisay S, Hailesselassie W. Risky HIV sexual behavior and utilization of voluntary counseling and HIV testing and associated factors among undergraduate students in Addis Ababa, Ethiopia. BMC Public Health. 2017;1–10. doi:10.1186/s12889-017-4060-y
17. USAID. HIV/AIDS and Sexual Reproductive Health Among University Students in Ethiopia. A Policy Intervention Framework; 2013.
18. Madda walabu registrar office report. 2020.
19. Obsa AG, Weldihanes B. Knowledge and self- efficacy on Hiv/Aids among undergraduate students of Maddawalabu University, Southeast Ethiopia. Glob J Hum Social Sci G Ling Educ. 2017;17(1).
20. Michael P; Carey KEES. Development and psychometric evaluation of brief HIV knowledge questionnaire. AIDS Educ Prev. 2008;14(2):172–182.
21. Zometa CS, Robert D, Knox MD, Wayne W, Simán SR, Ann D. Translation, cross-cultural adaptation and validation of an HIV/AIDS knowledge and attitudinal instrument. AIDS Educ Prev. 2007;19(3):231–244. doi:10.1521/aeap.2007.19.3.231
22. Kidane F. Knowledge, attitude, risk behavior on hiv/aids and willingness to participate in an hiv vaccine trial among high school teachers in addis ababa city, ethiopia. 2002.
23. Bulduk S, Erdo S. Reliability and validity of a self-efficacy scale for AIDS prevention among Turkish university students. Int J Hum Sci. 2008;5(2).
24. Abdu AO, Teshome G, Melese DM, Girma A, Daniel K, Agizie A. Knowledge, attitude, practice and associated factors of voluntary counseling and testing for HIV/AIDS among Wolkite university students in Ethiopia. J AIDS HIV Res. 2017;9(5):98–105. doi:10.5897/JAHR2015.0362
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

