Back to Journals » Infection and Drug Resistance » Volume 15
Histiocytic Necrotizing Lymphadenitis with Cupriavidus Pauculus Infection in a Patient with Graves Hyperthyroidism: A Case Report
Authors Tian S, Zhu B, Tian Y, Li J , Peng C
Received 16 November 2021
Accepted for publication 24 February 2022
Published 10 March 2022 Volume 2022:15 Pages 1019—1025
DOI https://doi.org/10.2147/IDR.S349655
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Shan Tian,1,* Bin Zhu,1,* Youyou Tian,2 Junyuan Li,1 Cheng Peng1
1Department of Infectious Diseases, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, Hubei, People’s Republic of China; 2Department of Infectious Diseases, Taihe Hospital, Hubei Medical University, Shiyan, 442000, Hubei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Cheng Peng, Department of Infectious Diseases, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, No. 1277 Jiefang Avenue, Wuhan, Hubei, People’s Republic of China, Email [email protected]
Abstract: Histiocytic necrotizing lymphadenitis (HNL) is a self-limiting inflammatory disease presenting with fever and cervical lymphadenopathy. However, no case of HNL with confirmed bacterial infection has been reported. A 38-year-old man was admitted to our hospital owing to an intermittent fever from 8 days. He was diagnosed with Graves hyperthyroidism 3 months prior and began taking methimazole tablets orally. Physical examination revealed superficial lymphadenopathy and goiter of the thyroid (grade II). Blood routine showed a decrease in peripheral blood cells, including significant reduction in leukocytes and platelets. A bone marrow culture identified a very rare pathogen, Cupriavidus pauculus, but the antibiotic effect of meropenem was unsatisfactory. Biopsy of the left cervical lymph node revealed HNL, and the patient had no fever after using glucocorticoids. This case report indicates that clinicians should be aware of the coexistence of HNL and bacterial infections, especially in patients with Graves hyperthyroidism.
Keywords: histiocytic necrotizing lymphadenitis, leucopenia, Graves hyperthyroidism, Cupriavidus pauculus, glucocorticoid
Introduction
Histiocytic necrotizing lymphadenitis (HNL) is a reactive proliferative disease in the lymph nodes, which is not common in clinical settings.1 Previous literature reported that this disease has a recurrence rate of 3.5%, and 1.7% of individuals pass from untimely treatment or serious complications.2 The disease commonly occurs in young patients under the age of 40 and is characterized by high fever and chills. Some patients may have superficial lymphadenopathy and hepatosplenomegaly, and a few patients may experience local skin rashes. This rare disease has been reported in patients with connective tissue diseases, such as systemic lupus erythematosus or rheumatoid arthritis, but has never been reported in individuals with Graves hyperthyroidism. Herein, we describe a young patient with HNL secondary to Graves hyperthyroidism. Notably, this patient was infected with a very rare pathogen, Cupriavidus pauculus.
Case Description
A 38-year-old man was admitted to the Department of Infectious Diseases, Wuhan Union Hospital on July 19, 2021, with the chief complaint of intermittent fever for 8 days. On day 1 of symptom presentation, the patient experienced a fever as high as 40 °C without an obvious cause of fever, accompanied by headache, sore throat, fatigue discomfort, and diarrhea (4–5 times per day). He visited the local hospital, and his blood routine examination showed leucopenia. His body temperature returned to normal and frequency of diarrhea was reduced after anti-infection treatment. He visited the local hospital again for the recurrence of fever on day 7. No obvious infectious lesions were observed on his chest computed tomography (CT). Blood routine showed low levels of leukocytes (0.87 G/L, range:3.5–9.5 G/L), platelets (14 G/L, range:125–350 G/L), hemoglobin (99 g/L, range: 115–150 g/L), and high levels of C-reactive protein (CRP) (151.86 mg/L, range:<8.0 mg/L). However, there was no relief of symptoms after combined therapy with antibiotics, elevation of white blood cells, and platelets (specific drugs are not available). Therefore, he went to the infection department of Wuhan Union Hospital for further treatment on day 8. During the course of fever, he exhibited sleeplessness and poor appetite. Three months ago, the patient was diagnosed with Graves hyperthyroidism in the external hospital, and was treated with oral methimazole (10 mg, two tablets each in the morning and evening).
Blood routine plus reticulocyte revealed reduction of the ternary systems (white blood cell count of 0.68 G/L (range: 3.5–9.5 G/L), red blood cell count of 3.29 T/L (range:3.8–5.1, T/L), hemoglobin of 92 g/L (range:115–150 g/L), and platelet count of 26 G/L, range:125–350 G/L), and myelosuppression (reticulocyte percentage of 0.26%, range:0.5%-1.5%, reticulocyte count of 0.01 G/L, range:0.024–0.084). Thyroid function examination identified hyperthyroidism (FT4: 24.7 pmol/L, range:9–19.8 pmol/L, FT3: 5.0 pmol/L, range:2.63–5.7 pmol/L, TSH: 0.0001 UU/mL, range: 0.35–4.94 UU/mL, TPO: 26.28 IU/mL, range:<5.61IU/mL, and anti-TG: 14.68 IU/mL, range: <4.11 IU/mL). Inflammatory indexes were also increased (Hs-CRP: 215 mg/L range: <8.0 mg/L, ESR: 40 mm/h range:<15 mm/h, procalcitonin:11.4 mg/L range:<0.5 mg/L, ferritin: 2179.5 ug/L range:21.8–275 ug/L). Extractable nucleic acid antibody (ENA) revealed that antinuclear antibody karyotype is nuclear homogeneous, and the titer of antinuclear antibody was 1:320 (range: <1:100). In addition, the ratio of Sm to RNP was 3.4, and titer of anti SM antibody was 0.8. However, the result of the lupus anticoagulant test was negative. On day 11, thyroid ultrasound showed goiter with diffuse lesions and rich blood perfusion (Figure 1A). Color Doppler ultrasonography of the cervical lymph nodes demonstrated that several lymph node echoes can be seen on both sides of the neck with clear boundaries, and the sizes of the two lymph nodes were about 25.3 mm × 8.9 mm (Figure 1B) and 15.1 mm × 5.4 mm (Figure 1C). On day 18, results of the chest CT were the following: (1) scattered nodules existed in both lungs, (2) small flocculent shadow in the anterior mediastinum, and (3) decreased density of the thyroid and slight splenomegaly. On day 26, results of the bone marrow biopsy reported that the proliferation of hematopoietic tissue was inhibited, the ratio of hematopoietic tissue to adipose tissue was about 2:8, the ratio of granulocyte to erythrocyte was reduced, and the number of granulocytes was significantly reduced. There were less megakaryocytes (1–2/HPF) and a small number of lymphocytes and plasma cells (Figure 2). Bone marrow bacterial culture (No. 214010885) identified a rare bacteria, Cupriavidus pauculus (Table 1). On day 31, results of the lymph node biopsy of the left cervical lymph node (pathology No. 21-1055) reported HNL (Kichuchi lymphadenitis). The excisional lymph node was partially destroyed, with multiple irregular necrotic foci, and many macrophages existed in and around the necrotic areas (Figure 3). Immunohistochemical staining was performed to identify the exact cell types in the lesions. The positive results of CD3, CD4, and CD8 indicated that the lesions were dominated by T cells. The positive results of CD68, CD123, and MPO showed abundant histiocytes and plasma dendritic cells. CD21(+) showed focal staining of the disrupted follicular dendritic cell meshwork remnants. The proliferation index of Ki-67 was about 70%, and EBV was negative (EBER: 2–3/HPF) as detected by in situ hybridization (Figure 4).
 |
Table 1 Results of Bone Marrow Bacterial Culture and Drug Sensitivity Test |
 |
Figure 1 Color Doppler ultrasound images indicate the enlarged thyroid (A) and swollen lymph nodes ((B) left, (C) right). |
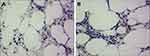 |
Figure 2 Pathological picture of bone marrow tissues from this case ((A) 200×; (B) 400×). |
 |
Figure 3 Hematoxylin and eosin stained section of the resected lymph node ((A) 100×; (B) 200×; (C) 400×). |
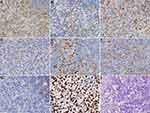 |
Figure 4 Immunohistochemical results of a lymph node ((A) CD3; (B) CD4; (C) CD8; (D) CD68; (E) CD123; (F) MPO; (G) CD21; (H) Ki-67; (I) EBER). |
The patient sustained high fever after admission. Considering the patient’s history of Graves hyperthyroidism, high fever may be a secondary infection caused by leucopenia induced by methimazole. Blood culture, bone marrow culture, fungal examination, tuberculosis, and other etiological examinations were further performed to determine the potential pathogen. As an empirical treatment, we combined ceftazidime tazobactam sodium (2.4 g, twice a day) and levofloxacin lactate (0.6 g, once a day) for anti-infection therapy, and human granulocyte stimulating factor (100 μg, once a day) and recombinant human thrombopoietin (7500 IU, once a day) were prescribed to improve leukocytes and platelets. At the same time, we consulted the endocrinology department who recommended ceasing the use of methimazole tablets and suggested the use of propranolol (10 mg, 3 times/day) to control heart rate. To prevent thyroid crisis after drug withdrawal, methimazole tablets were crushed and mixed with vitamin E cream and applied on the skin of the thyroid surface on day 22. The patient’s haemocytes did not further deteriorate (Table 2), and the thyroid function was also improved. Based on the results of the bone marrow culture (Cupriavidus pauculus +), the antibiotic was upgraded to meropenem (1000 mg, 3 times/day). After 3 days of treatment with meropenem, although the inflammatory index of the patient decreased (Table 2), the patient was still febrile, indicating that the fever was not only caused by an infectious agent. On day 25, the swollen lymph node located in the left side of the neck was removed in the plastic surgery department for pathological examination. The pathological results were in line with HNL. For anti-infection treatment, dexamethasone (3 mg, once a day) was delivered intravenously. Fortunately, his body temperature went back to normal on the same day and the superficial lymph nodes gradually disappeared in the following days. On day 29, intravenous dexamethasone was changed to prednisone acetate tablets (15 mg in the morning and 5 mg in the evening). The patient was discharged from the hospital after his symptoms improved on day 36. The patient was advised to reduce one prednisone acetate tablet per week after discharge. Two months after discharge, the patient stopped taking prednisone acetate tablets and had no fever, as determined through a telephonic follow-up.
 |
Table 2 Dynamic Changes of Blood Routine and Inflammatory Indexes |
Discussion
HNL is an uncommon autoimmune condition characterized by fever, leukopenia, and enlarged lymph nodes. Despite quite a few studies related to HNL in the literature, the etiology and pathogenesis of HNL remain unknown, which poses significant diagnostic challenges to clinicians and pathologists, especially when this disease complicates with acute bacterial infection. The exact etiology of HNL is not clear, which may be related to viral infection or autoimmune diseases.3–5 In this case, EBV and CMV were negative, but the potential infection of other viruses could not be conclusively ruled out. Three months ago, the patient was diagnosed with Graves hyperthyroidism, which is an autoimmune disease occurring in the endocrine system.6 His titer of antinuclear antibody was 1:320. Given the most recent international consensus,7 autoimmune disease should be considered when the antinuclear antibody titer exceeds 1:100. In addition, the patient’s autoimmune antibody showed a ratio of Sm to RNP as 3.4, and the titer of anti SM antibody as 0.8, but the patient had no skin rash specifically for systemic lupus erythematosus. Based on the negative result of the lupus anticoagulant test, the possibility of systemic lupus erythematosus could be ruled out. However, Graves hyperthyroidism is an autoimmune disease, which can lead to the rise of relevant autoimmune antibodies. A prospective study with 3209 participants8 reported that 16.7% of patients with Graves hyperthyroidism also had connective tissue diseases, such as rheumatoid arthritis, systemic lupus erythematosus, psoriasis, and multiple sclerosis. To our knowledge, this is the first clinical case of HNL that is secondary to Graves hyperthyroidism. Therefore, his abnormal autoimmune antibody may indicate that he complicates with undifferentiated connective tissue disease on the basis of Graves hyperthyroidism. Whether this case will develop into an established connective tissue disease in the future is not clear, and close follow-up is still needed.
Long term use of methimazole occasionally leads to leucopenia, which could lead to opportunistic infection. Leucopenia caused by methimazole is usually reversed by drug withdrawal, but this was not the case for our patient. Leucopenia is commonly seen in patients with HNL due to abnormal immune response.9 The possible pathogenesis of HNL is abnormal immune response mediated by activated T cells to a variety of antigens, including autoimmune antibodies,10 which may lead to dysregulated and declined body immunity. In this case, HNL destroyed lymphocytes and weakened immunity, which commonly leads to infection. Bacterial culture of the bone marrow revealed a very rare bacteria, Cupriavidus pauculus,11 which occasionally incurs severe human infections, especially in immunosuppressive cases. Although Cupriavidus pauculus is viewed as a rare opportunistic pathogen, it can also cause septic shock.12 The occurrence of HNL is reported to be related to infection, especially viral infection, but whether the infection of Cupriavidus pauculus leads to the occurrence of HNL is still unknown.
This patient had no chronic diseases in the past, except for the newly diagnosed Graves hyperthyroidism. He was found to have simultaneous reduction of the ternary systems after taking methimazole for 3 months. Hence, infection of Cupriavidus pauculus might also be related to leukopenia. It is worth noting that sole antibiotic treatment was not suitable for HNL complicated with infection (Cupriavidus pauculus). Although the levels of the inflammatory indexes (CRP, PCT, ESR, and ferritin) were decreased after the use of meropenem, the patient still had intermittent fever. The fever was relieved only with the use of glucocorticoids when he was diagnosed with HNL via lymph node biopsy. To our knowledge, this is the first clinical case of HNL complicated with infection of cupriavidus pauculus. Previously reported cases were simple types of HNL, and their bacterial tests were all negative. Although we have completed blood culture tests for patients several times, only the bacterial culture from the bone marrow was positive. Therefore, clinicians should be vigilant against testing patients with HNL for bacterial infection, and a bone marrow culture is helpful to identify pathogens.
High fever caused by HNL secondary to Graves hyperthyroidism needs the attention of clinicians. Most patients with Graves hyperthyroidism use methimazole to control thyroid function; however, long-term use will cause leucopenia and even bone marrow suppression, which can often lead to opportunistic infection and fever. Fever caused by reduction of the ternary systems can very easily cover up a diagnosis of HNL. However, the patient exhibited a poor response to antibiotic, even with the anti-infection therapy from the drug sensitivity test, and the fever was relieved with the combined use of glucocorticoids. Moreover, steroid therapy not only normalized the body temperature, but also ameliorated the superficial lymphadenopathy.
Conclusion
This study reported the course of diagnosis and treatment of HNL with Cupriavidus pauculus infection in a patient with Graves hyperthyroidism. Patients with Graves hyperthyroidism may have opportunistic infections due to reduction of the ternary systems by methimazole or/and HNL, and a timely stop to methimazole use is critical to prevent subsequent severe complications. Therefore, we need to be vigilant against rare bacterial infections among such patients. A bone marrow culture may help search for the potential pathogen.
Ethics Statement
This case report was performed in line with the principles of Declaration of Helsinki. Ethical approval was not required to publish the case report in accordance with the requirements of Wuhan Union Hospital’s clinical ethics committee. Written informed consent was obtained from the patient for publication of this case report.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Perry AM, Choi SM. Kikuchi-Fujimoto disease: a review. Arch Pathol Lab Med. 2018;142(11):1341–1346. doi:10.5858/arpa.2018-0219-RA
2. Bezek S, Tucci V, Kalra S, Fisher A. State of the globe: time to revisit Kikuchi Fujimoto disease. J Glob Infect Dis. 2014;6(4):139–140. doi:10.4103/0974-777X.145228
3. Tanasescu C, Nitescu D, Staniceanu F, Ardeleanu C, Atanasiu C. Kikuchi’s disease associated with systemic lupus erythematosus and autoimmune-like hepatitis. Rom J Intern Med. 2003;41(3):299–305.
4. Shusang V, Marelli L, Beynon H, et al. Autoimmune hepatitis associated with Kikuchi-Fujimoto’s disease. Eur J Gastroenterol Hepatol. 2008;20(1):79–82. doi:10.1097/MEG.0b013e32825a6a9e
5. Rosado FG, Tang YW, Hasserjian RP, McClain CM, Wang B, Mosse CA. Kikuchi-Fujimoto lymphadenitis: role of parvovirus B-19, Epstein-Barr virus, human herpesvirus 6, and human herpesvirus 8. Hum Pathol. 2013;44(2):255–259. doi:10.1016/j.humpath.2012.05.016
6. Subekti I, Pramono LA. Current diagnosis and management of Graves’ disease. Acta Med Indones. 2018;50(2):177–182.
7. Agmon-Levin N, Damoiseaux J, Kallenberg C, et al. International recommendations for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. Ann Rheum Dis. 2014;73(1):17–23. doi:10.1136/annrheumdis-2013-203863
8. Ferrari SM, Fallahi P, Ruffilli I, et al. The association of other autoimmune diseases in patients with Graves’ disease (with or without ophthalmopathy): review of the literature and report of a large series. Autoimmun Rev. 2019;18(3):287–292. doi:10.1016/j.autrev.2018.10.001
9. Kang HM, Kim JY, Choi EH, Lee HJ, Yun KW, Lee H. Clinical characteristics of severe histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease) in children. J Pediatr. 2016;171:208–212. doi:10.1016/j.jpeds.2015.12.064
10. Ohshima K, Shimazaki K, Kume T, Suzumiya J, Kanda M, Kikuchi M. Perforin and Fas pathways of cytotoxic T-cells in histiocytic necrotizing lymphadenitis. Histopathology. 1998;33(5):471–478. doi:10.1046/j.1365-2559.1998.00532.x
11. Huda SA, Yadava S, Kahlown S, Jilani MH, Sharma B. A rare case of ventilator-associated pneumonia caused by Cupriavidus pauculus. Cureus. 2020;12(6):e8573. doi:10.7759/cureus.8573
12. Bianco G, Boattini M, Audisio E, Cavallo R, Costa C. Septic shock due to meropenem- and colistin-resistant Cupriavidus pauculus. J Hosp Infect. 2018;99(3):364–365. doi:10.1016/j.jhin.2018.03.025
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
