Back to Journals » Journal of Inflammation Research » Volume 16
Higher High-Mobility Group Box-1 Levels are Associated with White Matter Lesions in Ischemic Stroke Patients
Authors Zhao J, Xu F, Xu W, Lv R, Wang J, Yang X
Received 24 July 2023
Accepted for publication 27 September 2023
Published 9 October 2023 Volume 2023:16 Pages 4441—4449
DOI https://doi.org/10.2147/JIR.S432109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Jie Zhao,1 Fang Xu,2 Wanying Xu,1 Rong Lv,1 Juan Wang,3 Xufeng Yang1
1Department of Geriatrics, Suzhou Ninth People’s Hospital, Soochow University, Suzhou, Jiangsu, 215200, People’s Republic of China; 2Department of Obstetrics and Gynecology, Suzhou Wujiang District Hospital of Traditional Chinese Medicine, Suzhou, Jiangsu, 215200, People’s Republic of China; 3Department of Endocrine, Suzhou Ninth People’s Hospital, Soochow University, Suzhou, Jiangsu, 215200, People’s Republic of China
Correspondence: Xufeng Yang, Department of Geriatrics, Suzhou Ninth People’s Hospital, Soochow University, No. 2666 Ludang Road, Suzhou, Jiangsu, 215200, People’s Republic of China, Tel/Fax +86 0512-82881332, Email [email protected]
Background and Purpose: High-mobility group box-1 (HMGB1) is a useful biomarker for disease severity stratification and prognosis prediction. We aim to explore whether the circulating HMGB1 concentrations are associated with the white matter lesions (WMLs) burden in stroke patients.
Methods: Between 2022 June and December 2022, patients with acute ischemic stroke were prospectively enrolled. HMGB1 levels were measured by an enzyme-linked immunosorbent assay after admission for all patients. The WMLs severity was assessed by the Fazekas scale. We dichotomized patients into those with moderate–severe WMLs (Fazekas score 3– 6) versus those with none–mild WMLs (Fazekas score 0– 2). Furthermore, based on the severity of periventricular WMLs (PWMLs) and deep WMLs (DWMLs), patients were categorized as none–mild (Fazekas score 0– 1) or moderate–severe (Fazekas score 2– 3).
Results: A total of 287 participants (mean age: 64.9 years; 157 male) were analyzed. The median serum HMGB1 levels were 7.3 ng/mL (interquartile, 4.3 ng/mL– 12.3 ng/mL). After adjustment for potential confounders, elevated HMGB1 levels were associated with the presence of moderate–severe WMLs (first quartile vs fourth quartile, odds ratio [OR], 4.101; 95% confidence interval [CI], 1.948– 8.633; P = 0.001) and moderate–severe PWMLs (first quartile vs fourth quartile, OR, 9.181; 95% CI, 4.078– 20.671; P = 0.001). Similar results were found when the HMGB1 levels were analyzed as a continuous variable.
Conclusion: This study demonstrated that increased HMGB1 levels were associated with the severity of WMLs, mainly in the periventricular region.
Keywords: ischemic stroke, high-mobility-group box 1, white matter lesions, inflammation
Introduction
White matter lesions (WMLs), also known as leukoaraiosis, are frequently detected by magnetic resonance imaging in elderly individuals.1–3 As one of the neuroimaging features of chronic cerebral small vessel disease,4 WMLs have a substantial clinical impact through associations with an increased risk of ischemic and hemorrhagic stroke, cognitive impairment, and depression.5–7 Moreover, it may adversely affect the final functional outcome after ischemic stroke.8,9 Although age and vascular risk factors are widely considered as major contributors to WMLs, they appear inadequate to fully explain the pathogenesis of WMLs. Therefore, early diagnosis and determining the mechanism of WMLs are important for the functional recovery of stroke patients.
As a 30-kDa nuclear and cytosolic ubiquitous protein, HMGB1 (high-mobility group box-1) plays an important role in inflammatory and immune responses to proinflammatory activity.10–12 Under ischemic conditions, HMGB1 is actively secreted by stimulated inflammatory cells.13 In the experimental model of middle cerebral artery occlusion, extracellularly secreted HMGB1 induced an inflammatory response via blood–brain barrier disruption.14 Recently, a prospective study reported that elevated serum HMGB1 levels at admission independently predict poor functional outcome at 1 year.15 Nevertheless, the relationship between serum HMGB1 and WMLs burden in ischemic stroke patients remains unknown. Interestingly, HMGB1 may mediate white matter injury following traumatic brain injury.16 We therefore hypothesized that increased HMGB1 levels may be linked to the severity of WMLs.
Thus, the aim of this study was to examine whether the circulating HMGB1 levels were associated with the severity of WMLs in patients with ischemic stroke. Additionally, we explore the associations of HMGB1 with WMLs burden in different regions.
Materials and Methods
Study Population
Between 2022 June and December 2022, patients with first-ever ischemic stroke were prospectively enrolled from Suzhou Ninth People’s Hospital. The diagnosis of ischemic stroke was based on a definition from World Health Organization and confirmed by brain computed tomography and/or magnetic resonance imaging.17 Patients were included in the study if they met these criteria: (1) age ≥ 18 years old; (2) time from onset to admission < 7 days. Patients with a history of leukodystrophy, demyelinating disease, central nervous system infection, immunosuppressive therapy, severe hepatic or renal disease, and active infections within the prior 14 days were excluded from this study. We also excluded patients who were unable to perform magnetic resonance imaging examination during hospitalization. This study was performed in accordance with the 1964 Helsinki Declaration and was approved by the ethics committees of Suzhou Ninth People’s Hospital. All participants gave written informed consent before entering the study.
Baseline Data
Data collection was performed after admission using a standardized case report form. The following clinical variables were recorded: demographic characteristics (gender and age), vascular risk factors (hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, and current smoking), and clinical data (blood pressure, neurological deficit, and stroke subtypes). Neurological deficits were measured using the National Institutes of Health Stroke Scale (NIHSS) score.18 Stroke subtypes were defined according to TOAST (Trial of Org 10172 in Acute Stroke Treatment) criteria,19 which included large-artery arteriosclerosis, cardioembolism, small vessel occlusion, stroke of other determined etiology, and stroke of undetermined etiology. Laboratory data including lipid profile, hyper-sensitive C-reactive protein (Hs-CRP), and fasting blood-glucose were also recorded.
HMGB1 Measurement
Blood samples (5 mL) were collected within 24 hr after admission and processed under standard laboratory procedure. Serum HMGB1 concentrations were measured using the enzyme-linked immunosorbent assay kit (IBL International) according to the manufacturer’s instructions. Laboratory test was performed by a technician who was blinded to the clinical data.
Imaging Assessment
Magnetic resonance imaging images were obtained for all patients including T1-weighted, T2-weighted, diffusion-weighted, and axial fluid attenuated inversion recovery (FLAIR) sequence images within 7 days after admission. WMLs were defined on FLAIR images according to the STandards for ReportIng Vascular changes on nEuroimaging criteria20 and graded according to the Fazekas scale21,22 on the basis of visual assessment of both periventricular and deep white matter areas. The total Fazekas score was calculated by adding the score of periventricular white matter lesions (PWMLs) and deep white matter lesions (DWMLs), which range from 0 to 6. According to previous studies,21,23,24 all subjects were dichotomized into none–mild WMLs (Fazekas score 0–2) and moderate–severe WMLs (Fazekas score 3–6) according to the total Fazekas score. Furthermore, we categorized the severity of PWMLs and DWMLs as none–mild (Fazekas score 0–1) or moderate–severe (Fazekas score 2–3). Images were independently read and measured by two trained neurologists who were blinded to the clinical data. All disagreements were resolved by consensus.
Statistical Analysis
Continuous data were demonstrated as mean ± standard deviation or median (interquartile range) and were analyzed with the Student’s t-test, Mann–Whitney U-test, Kruskal–Wallis test, and one-way analysis of variance where appropriate. Categorical data were expressed as percentages and were analyzed with the Fisher's exact test or χ2 test for categorical variables, where appropriate. Logistic regression models were utilized to determine the association between HMGB1 levels and WMLs severity. Model 1 was adjusted for demographic characteristics; Model 2 was adjusted for demographic characteristics and P value < 0.1 in the univariate analysis (including age, hypertension, diabetes mellitus, coronary heart disease, and Hs-CRP levels). The results are expressed as an adjusted odds ratio (OR) with the corresponding 95% confidence interval (CI).
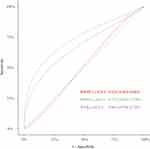
Furthermore, we performed the receiver operating characteristic curve (ROC) to investigate the overall predicted accuracy of HMGB1, and the results were reported as the area under the curve (AUC). All statistical analyses were performed with SPSS for Windows, version 25.0 (SPSS Inc., Chicago, IL, USA). A 2-tailed P value < 0.05 was considered to be statistically significant in all tests.
Results
Cohort Characteristics
During the study period, 287 patients eventually met the eligibility criteria. The mean age of the study sample was 64.9 years, and 54.7% of patients were male. Among these patients, 70.0% had hypertension, 29.6% had diabetes mellitus, 15.7% had hyperlipidemia, and 16.0% had coronary heart disease. The median circulating HMGB1 concentrations were 7.3 ng/mL (interquartile, 4.3 ng/mL–12.3 ng/mL). The baseline data are demonstrated in Table 1. Patients with increased HMGB1 levels were more likely to have higher Hs-CRP levels (P = 0.008). There were no significant differences in the distribution of demographic characteristics, baseline NIHSS score, and stroke etiology stratified by the levels of HMGB1 quartiles (all P > 0.05).
 |
Table 1 Baseline Data of the Study Sample According to the HMGB1 Quartiles |
Association Between WMLs Severity and HMGB1 Levels
There were 129 (44.9%) patients with moderate–severe WMLs (Fazekas score 3–6) and 158 (55.1%) patients with none–mild WMLs (Fazekas score 0–2). Table 2 illustrates the results of comparison of baseline characteristics stratified by the WMLs severity. As compared to patients without moderate–severe WMLs, those with it were older (P = 0.017), more likely to have hypertension (P = 0.047), diabetes mellitus (P = 0.022), and coronary heart disease (P = 0.003), and higher levels of Hs-CRP (P = 0.007) and HGMB1 (P = 0.001). Table 3 summarizes the results of the binary logistic regression of the association between HMGB1 levels and WMLs burden. On univariate logistic regression analysis, increased HMGB1 concentrations (odds ratio, [OR], 1.115; 95% confidence interval [CI], 1.095–1.218; P = 0.001) were associated with moderate–severe WMLs. After adjusting for covariates, higher HMGB1 levels remained an independent predictor of moderate–severe WMLs with an adjusted OR of 1.161 (95% CI, 1.096–1.229; P = 0.001). Similar results were found when HMGB1 was analyzed as a categorical variable.
 |
Table 2 Comparison of Baseline Characteristics Stratified by the Status of WMLs |
 |
Table 3 Binary Logistic Regression Analysis for the Association Between HMGB1 Levels and WMLs Severity |
We further explored the associations of PWMLs and DWMLs with serum HMGB1 levels separately. There were 104 (36.2%) patients with moderate–severe PWMLs and 99 (34.5%) patients with moderate–severe DWMLs. When comparing with the lowest quartile of circulating HMGB1 levels, the adjusted OR of the highest quartile for moderate–severe PWMLs was 9.181 (95% CI, 4.078–20.671; P = 0.001) after adjusting for demographic characteristics and variables with P < 0.1 in univariate analysis. However, there was no significant association between HMGB1 levels with moderate–severe DWMLs (first quartile vs fourth quartile, OR, 1.428; 95% CI, 0.675–3.022; P = 0.351; Table 3).
The Accuracy of HMGB1 in Predicting WMLs Severity
Figure 1 shows the results of the ROC curve. The AUC of HMGB1 in predicting the moderate–severe WMLs, moderate–severe PWMLs, and moderate–severe DWMLs were 0.661 (95% CI, 0.596–0.726, P = 0.001), 0.735 (95% CI, 0.670–0.799, P = 0.001) and 0.524 (95% CI, 0.445–0.603, P = 0.511), respectively. The optimal cutoff point of circulating HMGB1 levels in predicting moderate–severe WMLs was 9.0 ng/mL, with a sensitivity of 52.7% and a specificity of 73.4%. Also, the optimal cutoff point of circulating HMGB1 levels in predicting moderate–severe PWMLs was 9.5 ng/mL, with a sensitivity of 63.5% and a specificity of 76.5%.
Discussion
In our cohort of patients with ischemic stroke, circulating HMGB1 concentrations were strongly and positively associated with the moderate–severe burden of WMLs and PWMLs. Our findings indicated that HMGB1 might be considered a biomarker of WMLs in ischemic stroke patients.
For a long time, WMLs was considered to be a benign condition with no clinical significance. Cumulative evidence demonstrated that WMLs was associated with an increased risk of symptomatic stroke, cognitive impairment, and death.25,26 In our study, we found that 44.9% of patients who suffered an ischemic stroke present with moderate-severe WMLs. These results broadly agree with the findings of previous studies.23,27 A significant association was found between Large-artery atherosclerosis and WMLs burden, which is not supported by some other studies.21,28 This discrepancy is partly due to the differences in the study population and methods of assessing WMLs.
In a previous study, we found that patients with increased levels at admission were more likely to develop depression after ischemic stroke.29 Furthermore, to our best knowledge, this is the first study demonstrating that HMGB1 might be a biomarker of WMLs burden in ischemic stroke patients. The mechanisms by which serum HMGB1 affects WMLs burden in ischemic stroke patients are unclear, but multiple potential pathophysiological processes have been proposed. Firstly, increasing evidence confirms an extraordinarily important role of inflammation in the presence and progression of WMLs.30 After ischemic stroke, HMGB induces neuroinflammation via toll-like receptors, receptors for advanced glycation end products, or other receptors, which in turn aggravate the burden of WMLs. Secondly, HMGB1 could interact with matrix metalloproteinase enzymes and thus lead to the breakdown of blood–brain barrier.31 Zhang et al14 found that anti-HMGB1 mAb could be an effective therapy for brain ischemia by inhibiting the development of brain edema through the protection of the blood–brain barrier and the efficient clearance of circulating HMGB1. Meanwhile, blood–brain barrier dysfunction is regarded as a key point of WMLs.32 Other possible pathways include damaging endothelial cells, increasing oxidative stress, and activating glial cells.33–35
Our intriguing results further indicate that high HMGB1 levels are associated with PWMLs, but not with DWMLs. We speculate that it is due in part to anatomical, histological, as well as pathophysiological differences between PWMLs and DWMLs. The neural fibers in periventricular regions are longer than those in deep white matter regions, which might lead to the periventricular white matter being more vulnerable to hypoperfusion.36 According to data from histopathological studies, regions of periventricular white matter contained more immunoreactive microglia and astrocytes than deep white matter.37 Furthermore, prior pathology studies have confirmed that PWMLs are more likely linked to chronic hypoperfusion and inflammation, while DWMLs are more associated with ischemic damage.36,38 Further studies should be performed to explore the detailed mechanisms.
Several limitations should be considered in the interpretation of our study. Firstly, all ischemic stroke patients were enrolled from a single stroke center in China with a relatively small sample, which limits the generalization to other populations. Secondly, we did not quantify WMLs volume, which may be more sensitive for detecting subtle intergroup differences. However, the Fazekas scale is well established and frequently utilized in clinical studies,39,40 has been reported to correlate well with the WMLs volume, and we illustrate high inter-rater reliability of the assessment of WMLs. Thirdly, we only measured circulating HMGB1 at a single point after admission, which was not able to identify the dynamic change of HMGB1 after stroke. Finally, due to the observational nature of this study, it is difficult to infer causality. Therefore, future longitudinal cohort studies with large samples are warranted to confirm the association of HMGB1 levels with WMLs burden.
In conclusion, our present study showed that elevated serum HMGB1 levels appear to be associated with PWMLs severity, but not with DWMLs severity in ischemic stroke patients. Further longitudinal studies with large sample sizes are warranted to evaluate these associations comprehensively, which may open the way to the proposal of new therapeutic options for WMLs.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors took part in drafting, revising, or critically reviewing the article. All authors have provided their final approval for the version to be published; have reached an agreement on the journal to which the article has been submitted; and have committed to be accountable for all aspects of the work.
Funding
This study was supported in part by the Science and Technology Development Program of Suzhou (SYSD2018202), Jiangsu senile health research project (LSD2022019), the Science, Education, and Health Promotion Project in Wujiang District, Suzhou City (WWK201926).
Disclosure
The authors report no conflicts of interest in this work.
References
1. de Leeuw F, de Groot J, Achten E, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J Neurol Neurosurg Psychiatry. 2001;70(1):9–14. doi:10.1136/jnnp.70.1.9
2. Honda Y, Noguchi A, Maruyama K, et al. Volumetric analyses of cerebral white matter hyperintensity lesions on magnetic resonance imaging in a Japanese population undergoing medical check-up. Geriatr Gerontol Int. 2015;15:43–47. doi:10.1111/ggi.12672
3. Hilal S, Mok V, Youn Y, Wong A, Ikram M, Chen C. Prevalence, risk factors and consequences of cerebral small vessel diseases: data from three Asian countries. J Neurol Neurosurg Psychiatry. 2017;88(8):669–674. doi:10.1136/jnnp-2016-315324
4. Rudilosso S, Rodríguez-Vázquez A, Urra X, Arboix A. The potential impact of neuroimaging and translational research on the clinical management of lacunar stroke. Int J Mol Sci. 2022;23(3):1497. doi:10.3390/ijms23031497
5. Bos D, Wolters F, Darweesh S, et al. Cerebral small vessel disease and the risk of dementia: a systematic review and meta-analysis of population-based evidence. Alzheimers Dement. 2018;14(11):1482–1492. doi:10.1016/j.jalz.2018.04.007
6. Charidimou A, Pasi M, Fiorelli M, et al. Leukoaraiosis, cerebral hemorrhage, and outcome after intravenous thrombolysis for acute ischemic stroke: a meta-analysis (v1). Stroke. 2016;47(9):2364–2372. doi:10.1161/STROKEAHA.116.014096
7. Zhang X, Tang Y, Xie Y, et al. Total magnetic resonance imaging burden of cerebral small-vessel disease is associated with post-stroke depression in patients with acute lacunar stroke. Eur J Neurol. 2017;24(2):374–380. doi:10.1111/ene.13213
8. Henninger N, Lin E, Haussen D, et al. Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke. 2013;44(1):61–67. doi:10.1161/STROKEAHA.112.679084
9. Giurgiutiu D, Yoo A, Fitzpatrick K, et al. Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerv Surg. 2015;7(5):326–330. doi:10.1136/neurintsurg-2013-011083
10. Wang H, Bloom O, Zhang M, et al. HMGB-1 as a late mediator of endotoxin lethality in mice. Science. 1999;285(5425):248–251. doi:10.1126/science.285.5425.248
11. Fonken L, Frank M, Kitt M, et al. The Alarmin HMGB1 mediates age-induced neuroinflammatory priming. J Neurosci. 2016;36(30):7946–7956. doi:10.1523/JNEUROSCI.1161-16.2016
12. Lu B, Wang C, Wang M, et al. Molecular mechanism and therapeutic modulation of high mobility group box 1 release and action: an updated review. Expert Rev Clin Immunol. 2014;10(6):713–727. doi:10.1586/1744666X.2014.909730
13. Agnello D, Wang H, Yang H, Tracey K, Ghezzi P. HMGB-1, a DNA-binding protein with cytokine activity, induces brain TNF and IL-6 production, and mediates anorexia and taste aversion. Cytokine. 2002;18(4):231–236. doi:10.1006/cyto.2002.0890
14. Zhang J, Takahashi H, Liu K, et al. Anti-high mobility group box-1 monoclonal antibody protects the blood-brain barrier from ischemia-induced disruption in rats. Stroke. 2011;42(5):1420–1428. doi:10.1161/STROKEAHA.110.598334
15. Tsukagawa T, Katsumata R, Fujita M, et al. Elevated serum high-mobility group box-1 protein level is associated with poor functional outcome in ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(10):2404–2411. doi:10.1016/j.jstrokecerebrovasdis.2017.05.033
16. Ved R, Manivannan S, Tasker I, Zaben M. High mobility group box protein 1 and white matter injury following traumatic brain injury: perspectives on mechanisms and therapeutic strategies. Neural Regen Res. 2022;17(8):1739–1740. doi:10.4103/1673-5374.332135
17. Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke. 1989;20(10):1407–1431. doi:10.1161/01.STR.20.10.1407
18. Sucharew H, Khoury J, Moomaw C, et al. Profiles of the national institutes of health stroke scale items as a predictor of patient outcome. Stroke. 2013;44(8):2182–2187. doi:10.1161/STROKEAHA.113.001255
19. Adams HJ, Bendixen B, Kappelle L, Biller J, Love B, Gordon D. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi:10.1161/01.STR.24.1.35
20. Wardlaw J, Smith E, Biessels G, et al. STandards for ReportIng Vascular changes on nEuroimaging (STRIVE v1). Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12(2):822–838. doi:10.1016/S1474-4422(13)70124-8
21. Helenius J, Henninger N. Leukoaraiosis burden significantly modulates the association between infarct volume and national institutes of health stroke scale in ischemic stroke. Stroke. 2015;46(7):1857–1863. doi:10.1161/STROKEAHA.115.009258
22. Fazekas F, Niederkorn K, Schmidt R, et al. White matter signal abnormalities in normal individuals: correlation with carotid ultrasonography, cerebral blood flow measurements, and cerebrovascular risk factors. Stroke. 1988;19(10):1285–1288. doi:10.1161/01.STR.19.10.1285
23. Xie Y, Zhuo X, Xing K, et al. Circulating lipocalin-2 as a novel biomarker for early neurological deterioration and unfavorable prognosis after acute ischemic stroke. Brain Behav. 2023;13(5):e2979. doi:10.1002/brb3.2979
24. Patti J, Helenius J, Puri A, Henninger N. White matter hyperintensity-adjusted critical infarct thresholds to predict a favorable 90-day outcome. Stroke. 2016;47(10):2526–2533. doi:10.1161/STROKEAHA.116.013982
25. Sun L, Hui L, Li Y, Chen X, Liu R, Ma J. Pathogenesis and research progress in leukoaraiosis. Front Hum Neurosci. 2022;16:902731. doi:10.3389/fnhum.2022.902731
26. Grau-Olivares M, Arboix A. Mild cognitive impairment in stroke patients with ischemic cerebral small-vessel disease: a forerunner of vascular dementia? Expert Rev Neurother. 2009;9(8):1201–1217. doi:10.1586/ern.09.73
27. Shi G, Ke D, Gong P, et al. Serum YKL-40 levels and white matter hyperintensities in patients with acute ischemic stroke. J Inflamm Res. 2023;16:311–319. doi:10.2147/JIR.S398701
28. Suda S, Kanamaru T, Okubo S, et al. Urinary albumin-to-creatinine ratio is associated with white matter lesions severity in first-ever stroke patients. J Neurol Sci. 2017;373:258–262. doi:10.1016/j.jns.2017.01.011
29. Shan W, Xu L, Qiu Z, et al. Increased high-mobility group box 1 levels are associated with depression after acute ischemic stroke. Neurol Sci. 2022;43(5):3131–3137. doi:10.1007/s10072-021-05571-x
30. Gao Y, Li D, Lin J, et al. Cerebral small vessel disease: pathological mechanisms and potential therapeutic targets. Front Aging Neurosci. 2022;14:961661. doi:10.3389/fnagi.2022.961661
31. Nishibori M, Wang D, Ousaka D, Wake H. High mobility group box-1 and blood-brain barrier disruption. Cells. 2020;9(12):2650. doi:10.3390/cells9122650
32. Zupan M, Šabović M, Zaletel M, Popovič K, Žvan B. The presence of cerebral and/or systemic endothelial dysfunction in patients with leukoaraiosis--a case control pilot study. BMC Neurol. 2015;15:158. doi:10.1186/s12883-015-0416-z
33. Choi J, Jin X, Kim H, Koh S, Cho H, Kim B. High mobility group box 1 as an autocrine chemoattractant for oligodendrocyte lineage cells in white matter stroke. Stroke. 2023;54(2):575–586. doi:10.1161/STROKEAHA.122.041414
34. Tang D, Kang R, Zeh HJ, Lotze MT. High-mobility group box 1, oxidative stress, and disease. Antioxid Redox Signal. 2011;14(7):1315–1335. doi:10.1089/ars.2010.3356
35. Huo X, Su B, Qin G, Zhao L. HMGB1 promotes Ox-LDL-induced endothelial cell damage by inhibiting PI3K/Akt signaling pathway. BMC Cardiovasc Disord. 2022;22(1):555. doi:10.1186/s12872-022-03003-y
36. Fazekas F, Kleinert R, Offenbacher H, et al. Pathologic correlates of incidental MRI white matter signal hyperintensities. Neurology. 1993;43(9):1683–1689. doi:10.1212/WNL.43.9.1683
37. Simpson J, Ince P, Higham C, et al. Microglial activation in white matter lesions and nonlesional white matter of ageing brains. Neuropathol Appl Neurobiol. 2007;33(6):670–683. doi:10.1111/j.1365-2990.2007.00890.x
38. Fernando M, Simpson J, Matthews F, et al.; MRC Cognitive Function and Ageing Neuropathology Study Group. White matter lesions in an unselected cohort of the elderly: molecular pathology suggests origin from chronic hypoperfusion injury. Stroke. 2006;37(6):1391–1398. doi:10.1161/01.STR.0000221308.94473.14
39. Valdés Hernández Mdel C, Morris Z, Dickie D, et al. Close correlation between quantitative and qualitative assessments of white matter lesions. Neuroepidemiology. 2013;40(1):13–22. doi:10.1159/000341859
40. Kim G, Park K, Avery R, et al. Extensive leukoaraiosis is associated with high early risk of recurrence after ischemic stroke. Stroke. 2014;45(2):479–485. doi:10.1161/STROKEAHA.113.003004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.