Back to Journals » Infection and Drug Resistance » Volume 15
High Pretreatment Level of Neutrophil to Lymphocyte Ratio, Monocyte to Lymphocyte Ratio and Other Factors Associated with Delayed Sputum Conversion in Patients with Pulmonary Tuberculosis
Authors Suryana K , Dharmesti NWW, Rai IBN
Received 5 July 2022
Accepted for publication 29 August 2022
Published 15 September 2022 Volume 2022:15 Pages 5455—5462
DOI https://doi.org/10.2147/IDR.S380166
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Ketut Suryana,1,2 Ni Wayan Wina Dharmesti,3 IB Ngurah Rai4
1Division of Clinical Allergy-Immunology, Department of Internal Medicine, Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia; 2Department of Internal Medicine, Merpati Clinic, Wangaya Hospital, Denpasar, Bali, Indonesia; 3Department of Internal Medicine, Faculty of Medicine, Udayana University, Denpasar, Bali, Indonesia; 4Division of Pulmonology, Department of Internal Medicine, Faculty of Medicine, Udayana University, Sanglah Hospital, Denpasar, Bali, Indonesia
Correspondence: Ketut Suryana, Division of Clinical Allergy-Immunology, Department of Internal Medicine, Faculty of Medicine, Udayana University, Denpasar, Bali, 80114, Indonesia, Tel +62 859 537 839 44, Fax +62361 235982, Email [email protected]
Introduction: Patients with delayed intensive phase sputum conversion have a higher risk of multidrug resistant-tuberculosis (MDR-TB) and poorer treatment outcomes. Both, host (immune response and comorbidity) and pathogen factors play important roles in determining sputum conversion after treatment initiation. Impaired host immune response, especially the cellular components, as defined by the increased pre-treatment level of neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR) and other additional factors, were associated with severe active TB.
Purpose: To evaluate whether impaired immune responses (high pre-treatment level of NLR and MLR) and other factors associate with delayed sputum conversion at the end of the intensive phase treatment.
Patients and Methods: This was a case–control study from 2016 to 2020, which retrospectively analyzed the pre-treatment level of NLR, MLR and other factors among patients with new cases of pulmonary tuberculosis (PTB).
Results: A total of 62 patients (31 cases and 31 control). The cut-off value of high pretreatment level of NLR and MLR was 5.065 and 0.585, respectively. Bivariate analysis showed that pretreatment NLR ≥ 5.065 (OR 8.23, CI 95% 2.48– 27.32, p < 0.001), MLR ≥ 0.585 (OR 10.18, 95% CI 3.13– 33.18, p < 0.001) and BMI < 18.5 (OR 2.91, 95% CI 1.03– 8.20, p = 0.041) were associated with an increased risk of delayed sputum conversion. Multivariate analysis, however, showed that pretreatment NLR ≥ 5.065 was not significantly associated with delayed sputum conversion (AOR 3.370, 95% CI 0.71– 15.91, p value 0.125). A high pretreatment of MLR (AOR 30.802, 95% CI 3.22– 287.55, p value 0.003) and lower BMI (AOR 10.942, 95% CI 1.121– 98.563, p value 0.033) were significantly associated with an increased risk of delayed intensive phase sputum conversion.
Conclusion: High MLR pretreatment and a low BMI were significantly associated with an increased risk of delayed sputum conversion at the end of the PTB intensive phase treatment. High NLR pretreatment, smoking, diabetes, and HIV were not associated with sputum conversion.
Keywords: neutrophil to lymphocyte ratio, monocyte to lymphocyte ratio, intensive phase treatment, pulmonary tuberculosis, delayed sputum conversion
Introduction
Tuberculosis (TB) is the leading cause of death from an infectious disease and remains as a major health problem worldwide, with a persistently high annual incidence and mortality rate, according to the World Health Organization (WHO) annual report. Another disease burden was the significant proportion (7.3–25.4%) of pulmonary tuberculosis (PTB) patients with positive sputum who did not achieve sputum conversion at the end of intensive phase treatment.1–3 Delayed intensive phase sputum conversion has a high risk of multidrug resistant-tuberculosis (MDR-TB) and poorer treatment outcome.4 Immune response, comorbidity and pathogen factors play important roles in determining sputum conversion after treatment initiation. An adequate host immune response and other factors such as body mass index (BMI), diabetes, human immunodeficiency virus (HIV), and smoking were paramount to contain the infection as well as to achieve the target of treatment. Impaired host immune response, especially the cellular components, as defined by increased pre-treatment level of neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR) and other additional factors were associated with severe active TB,5,6 higher retreatment rate,7 and higher mortality rate.8,9 Furthermore, if high pre-treatment levels of NLR and MLR are associated with delayed sputum conversion at the end of intensive phase treatment, it could be preferred in practice as a simple, cheap and effective alternative method to monitor routinely for TB patients.
Methods
Study Design and Ethics
This was a matched case–control study, which retrospectively evaluated the pre-treatment level of NLR and MLR of new PTB cases at a pulmonary outpatient clinic in Sanglah Hospital and Wangaya Hospital from 2016 to 2020. This study was approved by the Faculty of Medicine Udayana University’s ethical review board with register No: 349/UN14.2.2.VII.14/LT/2021. The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all the participants.
Patient and Public Involvement
It was not appropriate or possible to involve patients or the public in the design, conduct, reporting or dissemination plans of our research.
Population
The inclusion criteria of cases was patients aged ≥18 years old, who were treated as new case PTB with WHO standard regimen (fixed dose combination) for 2 months (intensive phase) with good adherence, and did not show sputum conversion at the end of the intensive phase treatment. The inclusion criteria for controls are similar with the cases, except for the observed sputum conversion at the end of the intensive phase treatment. The exclusion criteria included patients that did not receive a WHO standard TB regimen, patients who were resistant to rifampicin, patients with secondary bacterial infections, heart diseases, autoimmune diseases, malignancy, and incomplete data of pre-treatment NLR and MLR. Control subjects were matched with case subjects (1:1), according to age (5-year age range) and sex. The confounding factors that were controlled by analysis including, diabetes, HIV, body mass index (BMI), and smoking habit.
Procedures
Patients’ characteristics as well as the pre-treatment level of NLR and MLR were obtained from medical records. The initial sputum evaluation to diagnose PTB is done using the Gene-Xpert MTB/RIF assay. Sputum evaluation after the intensive phase treatment is done using the acid-fast bacilli smear.
Statistical Analysis
The cut-off point of high pre-treatment levels of NLR and MLR was determined from ROC curve analysis. The Chi-square test was done and statistical significance was declared at p < 0.05. Multiple logistic regression was used to evaluate high pre-treatment levels of NLR, MLR and other associated factors with sputum conversion. All of the statistical analysis was analyzed with the software Statistical Package for the Social Sciences (SPSS) version 20.0.
Result
We found a total of 73 patients with delayed intensive phase sputum conversion from 2016 to 2020. Exclusion was made for 2 patients due to having secondary bacterial infections, 1 patient with a malignancy, and 39 patients without complete data of pre-treatment NLR, MLR and other factors. The number of patients with delayed sputum conversion that enrolled to this study was 31.
Thirty-one subjects with sputum conversion and matched by age and gender were enrolled as controls (Figure 1).
 |
Figure 1 Flow diagram of study cases and controls included in data analysis. |
Patients’ characteristics are shown in Table 1. The majority of our patients were male, with the mean age in the case group being 40.55 ± 16.06 (19–75) and 40.71 ± 15.26 (18–76) in the control group. The mean of body mass index of patients in the case group was 18.18 ± 2.92 (13.1–23.7) and it was 19.24 ± 4.89 (18.3–27.67) in the control group. The mean of pre-treatment NLR in the case group was 8.74 ± 3.87 (1.47–17.4) and the patients in the control group had a lower mean of pre-treatment NLR of 6.24 ±4.50 (1.3–23.3); this difference was statistically significant. The case group also had a significantly high mean of pre-treatment MLR (0.97 ±0.77 (0.28–4.70)) compared to the control group (0.45±0.19 (0.13–0.90)).
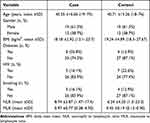 |
Table 1 The Characteristics of Subjects According to Case and Control Groups |
The cut-off point of high pre-treatment NLR and MLR was determined using the analysis of the ROC curve. The best cut-off point for high pre-treatment NLR and MLR was 5065 (sensitivity 83.9%, specificity 61.3%, AUC 0.725, IK 95% 0.594–0.856, p value 0.002) and 0.585 (sensitivity 80.6%, specificity 77.4%, AUC 0.855, 95% CI 0.760–0.950, p value 0.049), respectively (Figure 2).
 |
Figure 2 Receiver operating characteristics (ROC) curve of high pre-treatment NLR and MLR as risk factors of delayed intensive phase sputum conversion. |
A high pre-treatment NLR was found in 83.9% of the case group and in 38.7% of the control group and was associated with a delayed intensive phase sputum conversion (OR 8.23, 95% CI 2.482–27.317, p value <0.001). A high pre-treatment MLR was found in 80.6% of the case group and showed a significant association with the delay of intensive phase sputum conversion (OR 10.18, 95% CI 3.125–33.188, p value <0.001). Body mass index was further categorized into <18.5 and ≥18.5 (kg/m) and we found BMI <18.5 was associated with a delay in the intensive phase sputum conversion (OR 2.908,95% CI 1031–8204, p value 0.041). Diabetes mellitus, HIV infection, and smoking were not significantly associated with a delay in the intensive phase sputum conversion. The data were analyzed using the Chi-square test to determine the association between the dependent and independent variables with a significant value <0.05. The results of the analysis can be seen in Table 2.
 |
Table 2 Bivariate Analysis of NLR, MLR, and Other Variables as Risk Factors for Delayed Intensive Phase Sputum Conversion |
Multivariate analysis was done by multiple logistic regressions to consider factors such as NLR, MLR, BMI, smoking, diabetes and HIV in order to deduce the extent to which each of these variables correlates with risk factors for delayed intensive phase sputum conversion. We found high pre-treatment NLR was not associated with a delayed intensive phase sputum conversion, after adjustment by confounding factors. A high pre-treatment MLR showed consistent association with a delayed intensive phase sputum conversion in multivariate analysis (AOR 30.80, 95% CI 3.299–287.558, p value 0.003). A low level BMI (<18.5 kg/m) also showed significant association with a delayed intensive phase sputum conversion in multivariate analysis (AOR 10.942, 95% CI 1.121–98.563, p value 0.033) (Table 3).
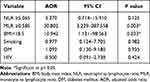 |
Table 3 Multivariate Analysis of High Pre-treatment NLR and MLR as Risk Factors for Delayed Intensive Phase Sputum Conversion |
Discussion
A high NLR on active PTB was associated with high neutrophil and low lymphocyte counts, that were further associated with extensive pulmonary destruction and persistent infection.10 In our study, the cut-off point of a high pretreatment NLR (5.065) was found in 83.9% of the case group and significantly associated with a delayed intensive phase sputum conversion in bivariate analysis (OR 8.23, 95% CI 2.482–27.317, p value <0.001). This cut-off point was higher than those found by Yin et al in 2017 (2.53), which was associated with retreatment in PTB patients. A study to evaluate the prognostic performance of hematologic indices to predict the outcome of intensive phase treatment was done previously by Stefanescu et al,11 however in their study the cut-off point of NLR was showing inadequate performance (AUC<7). Based on an ROC curve analysis, our cut-off point showed a fair value of AUC (0.725). However, in our study high pre-treatment NLR was, not showing consistent association with delayed intensive phase sputum conversion in multivariate analysis. This finding signified the non-specific nature of NLR as an inflammatory marker, in which the high level of NLR in our study might be affected by other condition such as malnutrition, HIV, or diabetes.
All of our subjects with low BMI (54.8% of the case group) showed high pre-treatment levels of NLR. This finding is supported by previous studies which found high NLR in pulmonary TB patients who were was associated with malnutrition and pulmonary cavities.12,13 Patients with diabetes showed significantly higher levels of NLR compared to the non-diabetic patients, which represented the continuous low grade inflammation in patients with diabetes.14 In our study, 84% patients with diabetes also showed high pretreatment NLR, nonetheless, diabetes was not associated with delayed intensive phase sputum conversion in our study. This result was possibly due to a smaller sample size than the previous studies15 and the possible role of the degree of glycemic control in our patients. Patients with HIV-TB co-infections, as well as HIV patients with uncontrolled disease also showed a high NLR level.16 HIV infection by itself has been shown as a strong predictor of active TB disease and a poor TB treatment outcome.17,18 On the contrary, in our study HIV was not associated with a delayed intensive phase sputum conversion, which is possibly due to a smaller number of HIV patients involved in our study, therefore it was inadequate to detect the different outcomes of TB treatment between HIV patients and non-HIV patients.
In our study we found that high pre-treatment MLR (≥0.585) was significantly associated with an increased risk of delayed sputum conversion at the end of the intensive phase treatment (OR 10.18, 95% CI 3.125–33.188, p value <0.001), even after adjustment for confounding factors (AOR 30.80, 95% CI 3.299–287.558, p value 0.003). This result is supported by the results of a prior molecular study of monocyte which showed that the function of monocyte as a defence mechanism against MTB was mainly described by the level of MLR, rather than its absolute count.19 High levels of MLR in patients with active TB is associated with an increased level of type I IFN, which lead to a poor phagocytosis function, necrosis of macrophage, and bacterial expansion. An extreme level of immune response, both inadequate and excessive, was associated with the growth of mycobacterium.20 A previous study showed that patients with active TB disease were having either lower (<9th percentile) or higher (>25th percentile) levels of MLR compared to healthy subjects.21 On the other hand, infection by MTB per se would cause a change of monocyte subsets balance in peripheral blood, which favoured the expansion of CD16+ subsets, resulting in the growth of bacteria and progression of the disease.22 A study by Stefanescu et al,11 was also aimed at evaluating the prognostic performance of MLR to predict the outcome of intensive phase treatment, which found patients with delayed intensive phase sputum conversion showed persistently high MLR after two months of treatment. Nonetheless, pre-treatment MLR was not associated with the outcome of intensive phase treatment in that study, due to the inadequate performance of MLR based on the result of ROC curve analysis.
Low BMI (<18.5 kg/m2) at diagnosis was associated with an increased risk of delayed intensive phase sputum conversion (OR 2.90, 95% CI 1031–8204, p value 0.041, AOR 10,942, 95% CI 11,215–98,563, p value 0.033). This result is similar with the findings of a previous study that also showed poor nutrition (BMI <18.5 kg/m2) at diagnosis and after 2 months of treatment was associated with poor treatment outcome (treatment failure, relapse).23 Nutrition plays a paramount role in maintaining and enhancing the immune response, both innate and adaptive, against pathogens, including MTB. The presence of malnutrition would impair the function of macrophages, the complement system, dendritic cells, and lymphocytes, which would further cause an increase of susceptibility to tuberculosis infection and reactivation of any latent infection.24 Patients with low BMI appeared to have a low level of pro-inflammatory cytokines and a high level of regulatory cytokine, the opposite condition was found in patients with higher BMI, which conferred protective benefits of high BMI to TB disease progression.25 However, high BMI was also associated with an increased risk of diabetes, which subsequently negates the beneficial effect of higher BMI to reduced the risk of TB infection and disease progression.26,27
A limitation of our study was the small sample size, owing to the design of this study, which obtained the result of hematologic examination from medical records, meanwhile this examination was not routinely performed in Wangaya Hospital. This caused substantial exclusions of subjects with delayed intensive phase sputum conversion in whom pretreatment complete blood count examination was not performed. A further prospective study with a bigger sample size is needed in the future to evaluate the factors associated with delayed sputum conversion to enhance the cure rate of PTB.
Conclusion
High pretreatment levels of MLR and a low BMI were significantly associated with an increased risk of delayed sputum conversion at the end of the intensive phase treatment of pulmonary TB. High pretreatment levels of NLR, smoking, diabetes, and HIV were not associated with an increased risk of a delay in the intensive phase sputum conversion.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Calderwood CJ, Wilson JP, Fielding KL, et al. Dynamics of sputum conversion during effective tuberculosis treatment: a systematic review and meta-analysis. PLoS Med. 2021;18(4):e1003566. doi:10.1371/journal.pmed.1003566
2. Gunda DW, Nkandala I, Kavishe GA, Kilonzo SB, Kabangila R, Mpondo BC. Prevalence and risk factors of delayed sputum conversion among patients treated for smear positive PTB in northwestern rural Tanzania: a retrospective cohort study. J Trop Med. 2017;2017:1–5. doi:10.1155/2017/5352906
3. Su WJ, Feng JY, Chiu YC, Huang SF, Lee YC. Role of 2-month sputum smears in predicting culture conversion in pulmonary tuberculosis. Eur Respir J. 2011;37(2):376–383. doi:10.1183/09031936.00007410
4. Shah NS, Wright A, Bai GH, et al. Worldwide emergence of extensively drug-resistant tuberculosis. Emerg Infect Dis. 2007;13(3):380–387. doi:10.3201/eid1303.061400
5. Wang W, Wang L, Liu Y, Yang F, Zhu L. Value of the ratio of monocytes to lymphocytes for monitoring tuberculosis therapy. Can J Infect Dis Med Microbiol. 2019;2019:3270393.
6. Eliaw A. The utility and validity of immunological, inflammatory, and nutritional-based scores and indices in active pulmonary tuberculosis. Int Clin Pathol J. 2018;6:199–213. doi:10.15406/icpjl.2018.06.00188
7. Kayigamba FR, Bakker MI, Mugisha V, et al. Adherence to tuberculosis treatment, sputum smear conversion and mortality: a retrospective cohort study in 48 Rwandan clinics. PLoS One. 2013;8(9):e73501. doi:10.1371/journal.pone.0073501
8. Yin Y, Kuai S, Liu J, et al. Pretreatment neutrophil-to-lymphocyte ratio in peripheral blood was associated with pulmonary tuberculosis retreatment. Arch Med Sci. 2017;13(2):404–411. doi:10.5114/aoms.2016.60822
9. Han Y, Kim SJ, Lee SH, et al. High blood neutrophil-lymphocyte ratio associated with poor outcomes in miliary tuberculosis. J Thorac Dis. 2018;10(1):339–346. doi:10.21037/jtd.2017.12.65
10. La Manna MP, Orlando V, Dieli F, et al. Quantitative and qualitative profiles of circulating monocytes may help identifying tuberculosis infection and disease stages. PLoS One. 2017;12(2):e0171358. doi:10.1371/journal.pone.0171358
11. Stefanescu S, Cocos R, Turcu-Stiolica A, et al. Evaluation of prognostic significance of hematological profiles after the intensive phase treatment in pulmonary tuberculosis patients from Romania. PLoS One. 2021;16(4):e0249301. doi:10.1371/journal.pone.0249301
12. Nakao M, Muramatsu H, Arakawa S, et al. Immunonutritional status and pulmonary cavitation in patients with tuberculosis: a revisit with an assessment of neutrophil/lymphocyte ratio. Respir Investig. 2019;57(1):60–66. doi:10.1016/j.resinv.2018.08.007
13. Duman TT, Aktas G, Atak BM, Kocak MZ, Erkus E, Savli H. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. Afri Health Sci. 2019;19(1):1602–1606. doi:10.4314/ahs.v19i1.35
14. Chiang CY, Bai KJ, Lin HH, et al. The influence of diabetes, glycemic control, and diabetes-related comorbidities on pulmonary tuberculosis. PLoS One. 2015;10(3):e0121698. doi:10.1371/journal.pone.0121698
15. Caetano Mota P, Carvalho A, Valente I, Braga R, Duarte R. Predictors of delayed sputum smear and culture conversion among a Portuguese population with pulmonary tuberculosis. Rev Port Pneumol. 2012;18(2):72–79. English, Portuguese. doi:10.1016/j.rppneu.2011.12.005
16. Cailleaux-Cezar M, Loredo C, Silva JRLE, Conde MB. Impact of smoking on sputum culture conversion and pulmonary tuberculosis treatment outcomes in Brazil: a retrospective cohort study. J Bras Pneumol. 2018;44(2):99–105. doi:10.1590/s1806-37562017000000161
17. Merriman RC, Dissanayake O, Alnjar S, Burns F, Miller RF. Incidence and significance of elevated platelet-to-lymphocyte and neutrophil-to-lymphocyte ratios among hospitalized HIV-positive adult patients. Int J STD AIDS. 2019;30(13):1329–1332. doi:10.1177/0956462419868881
18. Raviglione MC. Tuberculosis. In: Jameson JL, Kasper DL, Longo DL, Fauci AS, Hauser SL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine.
19. Rees CA, Pineros DB, Amour M, et al. The potential of CBC-derived ratios (monocyte-to-lymphocyte, neutrophil-to-lymphocyte, and platelet-to-lymphocyte) to predict or diagnose incident TB infection in Tanzanian adolescents. BMC Infect Dis. 2020;20:609. doi:10.1186/s12879-020-05331-w
20. MbatchouNgahane BH, Ebenezer AT, Eveline ND, et al. Diagnostic value of leukocyte count abnormalities in newly diagnosed tuberculosis patients. Open J Respir Dis. 2020;10:1–10. doi:10.4236/ojrd.2020.101001
21. Moreira-Teixeira L, Mayer-Barber K, Sher A, O’Garra A. Type 1 interferons in tuberculosis: foe and occasionally friend. J Exp Med. 2018;215(5):1273–1285. doi:10.1084/jem.20180325
22. Tobin DM, Roca FJ, Oh SF, et al. Host-genotype-specific therapies can optimize the inflammatory response to mycobacterial infection. Cell. 2012;148(3):434–446. doi:10.1016/j.cell.2011.12.023
23. Wang J, Yin Y, Wang X, et al. Ratio of monocytes to lymphocytes in peripheral blood in patients diagnosed with active tuberculosis. Braz J Infect Dis. 2015;19(2):125–131. doi:10.1016/j.bjid.2014.10.008
24. Lastrucci C, Benard A, Balboa L, et al. Tuberculosis is associated with expansion of a motile permissive and immunomodulatory CD16+ monocyte population via the IL-10/STAT3 axis. Cell Res. 2015;25(12):1333–1351. doi:10.1038/cr.2015.123
25. Sahile Z, Tezera R, Marlam DH, Collins J, Ali JH. Nutritional status and TB treatment outcomes in Addis Ababa, Ethiopia: an ambi-directional cohort study. PLoS One. 2021;16(3):e0247945. doi:10.1371/journal.pone.0247945
26. Chandrasekaran P, Saravanan N, Bethunaickan R, Tripathy S. Malnutrition: modulator of immune response in tuberculosis. Front Immunol. 2017;8:1316. doi:10.3389/fimmu.2017.01316
27. Kubiak RW, Sarkar S, Horsburgh CR, et al. Interaction of nutritional status and diabetes on active and latent tuberculosis: a cross-sectional study. BMC Infect Dis. 2019;19:267. doi:10.1186/s12879-019-4244-4
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
