Back to Journals » International Journal of General Medicine » Volume 15
High C-Terminal Fibroblast Growth Factor-23, Intact Parathyroid Hormone, and Interleukin-6 as Determinants of Valvular Calcification in Regular Hemodialysis Patients
Authors Kandarini Y, Mahadita GW , Herawati S, Wibhuti IBR, Widiana IGR, Ayu NP
Received 21 January 2022
Accepted for publication 30 March 2022
Published 20 April 2022 Volume 2022:15 Pages 4227—4236
DOI https://doi.org/10.2147/IJGM.S359168
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yenny Kandarini,1 Gede Wira Mahadita,1 Sianny Herawati,2 Ida Bagus Rangga Wibhuti,3 I Gde Raka Widiana,1 Nyoman Paramita Ayu1
1Department of Internal Medicine, Division of Nephrology and Hypertension, Udayana University Sanglah Hospital, Denpasar, Bali, Indonesia; 2Department of Clinical Pathology and Laboratory Medicine, Udayana University Sanglah Hospital, Denpasar, Bali, Indonesia; 3Department of Cardiology and Vascular Medicine, Udayana University Sanglah Hospital, Denpasar, Bali, Indonesia
Correspondence: Yenny Kandarini, Department of Internal Medicine, Division of Nephrology and Hypertension, Udayana University Sanglah Hospital, P.B. Sudirman Street, Dangin Puri Klod, West Denpasar, Denpasar, 80234, Bali, Indonesia, Tel +628123803844 ; +62361 223797, Email [email protected]
Purpose: Biggest cause of death in chronic kidney disease-hemodialysis (CKD-HD) patients is cardiovascular disease (CVD). Cardiovascular disease is often associated with mineral bone disorders (MBD), especially vascular and valvular calcification. Biomarkers such as C-terminal-fibroblast growth factor-23 (FGF-23), intact parathyroid hormone (iPTH), and interleukin-6 (IL-6) were investigated. Only few studies have focused on valvular calcification in CKD-HD patients, with controversial results. The present study aimed to investigate whether high C-terminal-FGF-23, iPTH, and IL-6 can be used as determinants of valvular calcification in CKD-MBD patients undergoing regular HD.
Patients and Methods: This was an analytical cross-sectional study which involved CKD-HD patients aged 18– 60 years with no history of CVD, malignancy, and diabetes mellitus. C-terminal FGF-23 was measured using enzyme-linked immunosorbent assay (ELISA) kit, iPTH using chemiluminescent immunometric method, and IL-6 using sandwich enzyme immunoassay technique. Valvular calcification on aortic and mitral valves was examined with echocardiography. Data analysis was done using Chi-squared test or Fisher’s exact test as appropriate and multivariate logistic regression analysis.
Results: Bivariate analysis with Fisher’s exact test showed significant association of prevalence ratio (PR) of C-terminal FGF-23 (PR = 1.33; p = 0.003; CI (1.017– 1.748)), iPTH (PR = 1.361; p = 0.002; CI (1.02– 1.816)), and IL-6 (PR = 1.2; p = 0.019; CI (1.000– 1.446)) with valvular calcification. Multivariate analysis with logistic regression showed high C-terminal FGF-23 (exp (B) value of 16.44; p = 0.045; CI (1.07– 252.75)), iPTH (exp (B) value of 33.312; p = 0.016; CI (1.94– 571.71)), and IL-6 (exp (B) value of 21.58; p = 0.0381; CI (1.18– 394.87)) were determinants of valvular calcification in CKD-MBD patients undergoing regular HD.
Conclusion: This study demonstrated that high C-terminal FGF-23, iPTH, and IL-6 were determinants of valvular calcification in CKD-MBD patients undergoing regular HD.
Keywords: dialysis, end-stage renal disease, inflammation, hormone
Introduction
Chronic kidney disease (CKD) is a worldwide problem. It is estimated that 10% of the world’s population suffer from it and the number keeps increasing especially in developing countries, including Indonesia.1,2 In Indonesia, prevalence of CKD reached 3.8% in 2018, up from 1.8% in 2013.3 This number is followed by increasing number of active renal replacement therapy (RRT) patients with hemodialysis (HD) still playing a primary role. In 2017, data from Indonesia Renal Registry (IRR) showed number of active patients undergoing HD reached 77,892 people.4
High incidence of CKD and increasing number of RRT patients cause several problems, such as high financial burden and high mortality rate. In America, health cost burden of CKD keeps increasing from 41.2 billion US Dollars (USD) in 2010 to 50.4 billion USD in 2014.1 In Indonesia, the average annual cost per patient was 7,845.6 USD with HD as the largest proportion of the cost (4,217.2 USD), followed by the cost of medicine (1,286.1 USD).5 This shows CKD-HD is causing high financial burden to patients and health social security in the world.
Msaad et al did a cohort study on CKD-HD patients and found high mortality rate in those patients. Cardiovascular disease (CVD), inflammation, and age were associated with CVD and all-cause mortality.6 In 2017, highest cause of death in CKD-HD patients in Indonesia was CVD with mortality rate reaching 1,480 patients (37.3%).4
Chronic complications of CKD that are often associated with CVD are mineral and bone disorders in CKD (CKD-MBD). Mineral bone disorder causes vascular and valvular calcification. Current evidence suggests that impaired mineral homeostasis, hormonal imbalance, and inflammation play a role in promoting vascular calcification. Mineral homeostasis and hormonal balance are closely related to Fibroblast Growth Factor-23 (FGF-23) and intact Parathyroid Hormone (iPTH).7,8 High FGF-23 has been associated with vascular calcification in CKD and dialysis patients,9–11 but studies regarding iPTH are still controversial.12,13 In an observational study on Asian population with CKD, serum inflammatory markers such as C-reactive Protein (CRP) and Interleukin-6 (IL-6) were significantly higher in patients with vascular calcification.14
While most studies have investigated association between those biomarkers and vascular calcification, only few studies have focused on valvular calcification in CKD-HD patients. Studies regarding valvular calcification are needed because both vascular and valvular calcification increase risk of CVD, CVD-related mortality, and all-cause mortality.15,16 The present study aimed to investigate whether high C-terminal FGF-23, iPTH, and IL-6 can be used as determinants of valvular calcification in CKD-MBD patients undergoing regular HD.
Materials and Methods
Study Population
This was an analytical cross-sectional study carried out in Hemodialysis Unit in Sanglah General Hospital, Denpasar, Bali between April and October 2019. We enrolled CKD-HD patients aged 18–60 years that were willing to participate as research subjects by signing written informed consent. This study procedure was approved by Ethics Committee of Udayana University/Sanglah General Hospital with register number 1767/UN14.2.2.VII.14/LP/2019. This study was conducted in line with the principles of the Helsinki declaration. The exclusion criteria were: 1) > 60 years old, 2) prior history of CVD (myocardial infarct, angina, stroke, heart failure, atrial fibrillation, coronary angioplasty or artery bypass graft, and valve replacement), 3) malignancy, and 4) diabetes mellitus. Seventy-six CKD-HD patients were examined to investigate whether high FGF-23, iPTH, and IL-6 can be used as determinants of valvular calcification in CKD-MBD patients undergoing regular HD.
Chronic kidney disease is defined as abnormalities in kidney structure or function for more than three months based on Kidney Disease: Improving Global Outcome (KDIGO) 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease.17 Chronic kidney disease – mineral bone disorders is defined as a syndrome consisting of one or combination of the following: biochemical abnormalities (calcium, phosphorus, iPTH and vitamin D), bone abnormalities and vascular or valvular calcification based on KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of CKD-MBD.18
Baseline Characteristics
Baseline characteristics were evaluated at study enrollment. Age was determined by date of birth in identity cards or medical records. Age was expressed in years and rounded to the nearest year. Body mass index (BMI) was calculated with the following formula: (weight in kg)/(height in m)2. Weight was measured using digital scale with capacity of 120 kg and accuracy of 0.1 kg. Weight was measured by researchers themselves. Weight measurement was done in fasting state with minimal clothing. Height was measured using digital scale with headboard and accuracy of 0.1 cm. Blood pressure was measured with Riester® mercury sphygmomanometer which had been calibrated periodically. It has 16×20 cm cuff. The cuff was placed 2–3 cm above antecubital fossa and inflated to 30 mmHg above the point where radial pulse disappeared. Phase I korotkoff sound was defined as systolic blood pressure (SBP) and Phase V korotkoff sound was defined as diastolic blood pressure (DBP). Korotkoff sounds were heard with bell of Littmann® stethoscope placed over brachial artery. Blood pressure was measured at least two times with one minute interval. Hemodialysis duration was determined by date of first HD initiation as seen from medical records or history taking and was expressed in months.
Assessment of C-Terminal FGF-23, iPTH, and IL-6
Fibroblast Growth Factor - 23 used in this study was C-terminal FGF-23. Samples for C-terminal FGF-23 were stored at 70°C and measured using Enzyme-linked Immunosorbent Assay (ELISA) kit. Intact Parathyroid Hormone was measured with chemiluminescent immunometric method. Samples for IL-6 measurement were stored at −20°C. Samples were centrifuged for 10 minutes and measured with sandwich enzyme immunoassay technique using Quantikine HS immunoassay kit (R&D System Inc. 614 McKinley N.E. Minneapolis, MN 55413 USA). Lowest value detected was 0.5 pg/mL.
Assessment of Valvular Calcification
Valvular calcification was defined as calcification in aortic and/or mitral valves on echocardiography with echo-2D using multiphase 3.3-mHz probe. Echocardiography examinations were carried out by experts. If valvular calcification was found, total area of calcification would be measured in mm2.
Statistical Analysis
Results were expressed as means ± standard deviation (SD) or median (interquartile) for continuous variables and as frequencies and percentage for categorical variables. Normality for continuous variables was analyzed with Kolmogorov–Smirnov test. Analysis with ROC curve was done to determine optimal cut-off value of C-terminal FGF-23, iPTH, and IL-6 in order to classify these variables as high and low. Bivariate analysis was done between high or low C-terminal FGF-23, high or low iPTH, and high and low IL-6 with valvular calcification using Chi-squared test or Fisher’s exact test as appropriate. If p < 0.25 in bivariate analysis, we included variables in multivariate analysis.
Multivariate logistic regression analysis was performed to investigate effect of each independent variable simultaneously with valvular calcification. Results were presented as OR (odds ratio). All tests were performed using SPSS version 22.0 (SPSS, Inc., Chicago, IL, USA). A p-value less than 0.05 was considered statistically significant.
Results
Baseline Characteristics of Patients
Seventy-six patients consisting of 49 men (64.5%) and 27 women (35.5%) with mean age of 50.96 ± 11.77 years were involved in this study. We found high mean C-terminal FGF-23 in regular HD patients: 11,228.6 ± 6,740 RU/mL. High mean C-terminal FGF-23 was also accompanied by high iPTH with a median value of 660.45 (25.4–4,192) pg/mL. Inflammation was evaluated with IL-6. Mean IL-6 in this study was 42.91 ± 27.80 pg/mL.
Echocardiography examinations showed high prevalence of valvular calcification, reaching 92.1% (70 patients). From 70 patients with valvular calcification, 15 patients (21.4%) had mitral valve calcification, 13 patients (18.6%) had aortic valve calcification, and 42 patients (60%) had mitral and aortic valve calcification. Quantitatively, median valve calcification area was 20.75 mm2 with range of 0–178.8 mm2. Baseline characteristics of patients consisting of demographic status, anthropometric/nutritional status, basic laboratory results and heart valve echocardiography results are presented in Table 1.
 |
Table 1 Baseline Characteristics of Patients |
High FGF-23, iPTH, and IL-6 to Valvular Calcification
Analysis with ROC curve was done to determine optimal cut-off value of C-terminal FGF-23, iPTH, and IL-6 in relation with valvular calcification in order to classify those biomarkers as high and low. Optimal cut-off value of C-terminal FGF-23 was 5,857 RU/mL (sensitivity = 80%; specificity = 83.3%), with area under the curve (AUC) 87.6% (p=0,002; CI 0.785–0.968). C-terminal FGF-23 ≥ 5,857 RU/mL was classified as high and C-terminal FGF-23 < 5,857 RU/mL was classified as low. Optimal cut-off value for iPTH was 200 pg/mL with AUC = 83.1% (p = 0.007; CI 0.722–0.94). Intact parathyroid hormone ≥ 200 pg/mL was classified as high and iPTH < 200 pg/mL was classified as low. Optimal cut-off value for IL-6 was 30 pg/mL with AUC 76.7% (p = 0.031; CI 0.645–0.888). Interleukin 6 ≥ 30 pg/mL was classified as high whereas IL-6 < 30 pg/mL was classified as low. ROC curve for C-terminal FGF-23, iPTH, and IL-6 was presented in Figure 1.
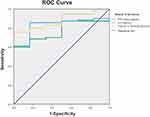 |
Figure 1 ROC curve for optimal cut-off value for C-terminal FGF-23, iPTH, and IL-6. |
Bivariate analysis with Fisher’s exact test showed prevalence ratio (PR) of C-terminal FGF-23 in association with valvular calcification was 1.33 (p = 0.003; CI 1.017–1.748). Prevalence ratio of iPTH to valvular calcification was higher, reaching 1.36 (p = 0.002; CI 1.02–1.816). High IL-6 was also found to have significant association with valvular calcifications with PR 1.20 (p = 0.019; CI 1.000–1.446) (Table 2).
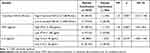 |
Table 2 Results of Bivariate Analysis with Fisher’s Exact Test |
Multivariate analysis with logistic regression analysis showed high C-terminal FGF-23, iPTH, and IL-6 as determinants of valvular calcification in CKD-MBD patients undergoing regular HD (Table 3). High C-terminal FGF-23 had exp (B) value of 16.44 which means it was 16.44 times more likely to cause valvular calcification compared to low, and was statistically significant (p = 0.045; CI 1.07–252.75). Exp (B) value of iPTH to valvular calcification was 33.31 (p = 0.016; CI 1.94–571.71). High IL-6 as a determinant of valvular calcification showed it was 21.58 times more likely to cause valvular calcification compared to low with exp (B) value of 21.58 (p = 0.0381; CI 1.18–394.87).
 |
Table 3 Results of Multivariate Analysis with Logistic Regression |
Discussion
We found high levels of C-terminal FGF-23, iPTH, and IL-6 in regular HD patients. After further analysis, we found that high C-terminal FGF-23 (≥ 5,857 RU/mL), iPTH (≥ 200 pg/mL), and IL-6 (≥ 30 pg/mL) were determinants for valvular calcifications in CKD-MBD patients undergoing regular HD.
C-Terminal FGF-23 and Valvular Calcification
This study found high mean C-terminal FGF-23 in regular HD patients (11,228.6 ± 6,740 RU/mL). High FGF-23 in CKD happens due to hyperphosphatemia. Hyperphosphatemia causes hypocalcemia that stimulates PTH secretion. In bone, PTH stimulates FGF-23 production.11 It was reported that FGF-23 concentrations are often 100–1,000-fold above the normal range in CKD patients.19 Choi et al found that circulating FGF-23 concentration gradually increased as CKD advanced, hence higher concentrations in end stage renal disease (ESRD) patients.20
We found significant relationship between C-terminal FGF-23 with valvular calcification in patients with CKD-MBD undergoing regular HD with PR = 1.22 (p = 0.003; CI 1.017–1.748). Further multivariate analysis showed high C-terminal FGF-23 was a determinant of valvular calcification with exp(B) value of 16.44 (p = 0.045; CI 1.07–252.75).
Findings of association between FGF-23 and valvular calcification in CKD patients varies. Di Lullo et al found FGF-23 had significant relationship in aortic valve calcification (r2 = 0.272; p = 0.01) in CKD stage 3–4 patients.21 An observational study in diabetic CKD patients found high FGF-23 was an independent predictor of mitral valve calcification.22 Chen et al stated that FGF-23 was an independent risk factor for aortic and mitral valve calcifications in CKD stage 2–5.23 Ganidagli et al found that FGF-23 was not significantly associated with valvular calcification in HD patients. This different finding was due to Ganidagli et al using intact FGF-23 (iFGF-23) for measurement and this study used C-terminal FGF-23.24 Lack of association between measures was demonstrated.25 This is probably due to higher intra-individual biological variability of iFGF-23 compared to C-terminal FGF-23 (18.3% vs 8.3%), therefore the use of iFGF-23 in diagnostics and medical management is limited.26 Further studies regarding FGF-23’s association with valvular calcification in CKD-HD patients are still needed.
High FGF-23 has been associated with vascular calcification in CKD and dialysis patients.9–11 Ragb et al studied 90 regular HD patients and found patients with valvular calcification had high abdominal aortic calcification score.27 Other studies found that aortic and mitral valve calcification on echocardiography was linked to coronary atherosclerosis in regular HD patient. This suggests that vascular and valvular calcification might share common determinants.28
The role of FGF-23 in pathogenesis of valvular calcification is related to its role in calcium-phosphate homeostasis. In CKD patients, there is resistance of FGF-23ʹs phosphate lowering actions due to higher levels necessary to handle a given phosphate load.29 This resistance will cause constant hyperphosphatemia. This condition will cause constant hyperparathyroid that results in hypercalcemia.30,31 Fibroblast Growth Factor-23 also inhibits vitamin D synthesis which further aggravates hyperparathyroid.8,21,32 Hypercalcemia and hyperphosphatemia will cause increased Calcium Phosphate Product (CaxP) deposit in cardiac valves, resulting in valvular calcification.30,31 Besides vascular and valvular calcification, FGF-23 can increase risk of CVD in HD patients by activating inflammation and Renin-Angiotensin-Aldosterone System (RAAS).8,21,32
Another biomarker related to FGF-23, Klotho, has been studied in its relation to calcification in CKD patients. Fibroblast Growth Factor-23 binds to FGF-receptors (FGF-R) in kidney using cofactor Klotho.33 Poor kidney function will negatively affect Klotho concentration with detectable reduction starting from CKD stage 2.34 In dialysis patients, Klotho concentration was correlated with FGF-23.35 In rats, high FGF-23 and low Klotho had been reported to promote vascular calcification and arterial stiffness.36 Chen et al stated that Klotho was one of the risk factors for valvular calcification in CKD patients.23 Klotho shows promising results to be used as determinant of valvular calcification.
iPTH and Valvular Calcification
Our patients had high median iPTH (660,45 (25,4–4192) pg/mL) with optimal cut-off value of 200 pg/mL (AUC= 83.1%; p = 0.007; CI 0.722–0.94). Ardahanli et al studied 49 HD patients and found significantly higher iPTH levels than in control group (578.2 pg/mL vs 36.2 pg/mL).37 Mechanism of hyperparathyroid in CKD has been explained previously. Moreover, in CKD, there is decreased expression of calcium sensing receptor (CaSR) and increased set-point for calcium-regulated PTH secretion in thyroid gland.38 All of this further stimulates PTH production. Prevalence ratio of iPTH to valvular calcification was 1.36 (p = 0.002; CI (1.02–1.816)). Further multivariate analysis showed Exp (B) value of high iPTH to valvular calcification was 33.31 (p = 0.016; CI 1.94–571.71).
Multiple studies regarding association between iPTH and valvular calcification have been done. Liu et al stated that iPTH was significantly associated with higher risk of valvular calcification in dialysis patients.9 Parathyroid hormone was also significantly correlated with valvular calcification in HD patients.37 Studies found iPTH was independently associated with aortic valve calcification in CKD and regular HD patients.21,39 Chung et al stated that iPTH was also correlated with vascular calcification.12 Primary hyperparathryoid without CKD has also been associated with valvular calcification.40
Not all findings are consistent, as Faqih et al found that iPTH did not correlate significantly with valvular calcifications in HD patients. They found that only HD duration played a significant role in valvular calcification.13 Low prevalence of valvular calcification in Faqih et al’s work (15% vs 92.1%) may contribute to this disparity. Rong et al also found no association between iPTH and valvular calcification in CKD patients. They did not find a significant difference between valvular and non-valvular calcification group (59.12 pg/mL vs 50.37 pg/mL; p = 0.897).14 This disparity could be caused by lower PTH concentration in the study by Rong et al. In our study median iPTH was approximately ten times higher. We found that optimal cut-off value of iPTH was 200 pg/mL and found that iPTH > 200 pg/mL was a determinant of valvular calcification. Intact parathyroid hormone concentration in Rong et al’s work did not reach our cut-off value. Soleymanian et al found that iPTH < 200 mg/dL was not associated with all-cause mortality in HD patients.41 We believe further studies with larger sample size are needed. Mechanism of PTH causing valvular calcification in CKD patient overlaps with FGF-23. Hyperparathyroid will cause hypercalcemia which causes calcification.37
IL-6 and Valvular Calcification
High IL-6 had a significant association with valvular calcifications with PR 1.20 (p = 0.019; CI 1.000–1.446). High IL-6 as a determinant of valvular calcification showed it was 21.58 times more likely to cause valvular calcification compared to low, with exp (B) value of 21.58 (p = 0.0381; CI 1.18–394.87).
Multiple studies have shown IL-6 was associated with vascular calcification in CKD and dialysis patients.14,42,43 Kamińska et al found that IL-6 was significantly associated with coronary artery calcification in CKD patients.44 It is also associated with vascular calcification progression in HD patients.45 Studies regarding valvular calcification are limited but consistent. Ikee et al found that inflammatory markers are associated with aortic valve calcification in HD patients.46 Lee at al found higher IL-6 and lower fetuin A in HD patients with valvular calcification.47 Fetuin A is closely related to IL-6 and calcification. Interleukin-6 causes calcification by decreasing fetuin A production. Fetuin A prevents CaxP deposit by forming soluble particles.48 In the general population, IL-6 promotes aortic valve calcification.49
Elevated IL-6 is commonly observed in CKD patients. This is due to increased oxidative stress, chronic inflammation, and fluid overload. Impaired renal function also contributes due to decreased IL-6 clearance. Dialysis further stimulates inflammatory response and increases IL-6 production.50 Fibroblast Growth Factor-23 and IL-6 have a reciprocal relationship. Fibroblast Growth Factor-23 stimulates the liver to produce IL-6 by FGF receptor-4 (FGFR4) on the surface of hepatocytes. In return, IL-6 also stimulates FGF-23 production. Therefore, CKD patients with high FGF-23 tend to have high IL-6.8,32 Also, inflammatory cytokines, such as IL-6 and CRP, can promote vascular smooth muscle cell calcification, through the activation of Msx2-Wnt/β-catenin signaling. Moreover, IL-6 may promote osteogenic gene expression and mineralization of valve interstitial cells.48,49
Limitations
Our cross-sectional study has several limitations. First, this research is limited by the scope of a single center study of participants. A study with larger sample size and wider demographics of patients may represent the general population more accurately. Second, we excluded patients aged more than 60 years old in order to exclude degenerative valvular calcification, thereby further limiting our sample number. Third, we did not include continuous ambulatory peritoneal dialysis (CAPD) patients in our study.
Conclusion
This study demonstrated that high C-terminal FGF-23, iPTH, and IL-6 were determinants of valvular calcification in CKD-MBD patients undergoing regular HD. Further research regarding early management and prevention of these variables is needed.
Acknowledgments
The authors would like to thank all participants in this study. Authors would also like to thank all staff of Hemodialysis Unit, Echocardiography Unit and Laboratory in Sanglah General Hospital. Authors would like to thank all staff of Department of Internal Medicine in Division of Nephrology and Hypertension, Department of Clinical Pathology and Laboratory Medicine and Department of Cardiology and Vascular Medicine in Udayana University. This work was supported by Udayana University Research and Community Service Institute, Denpasar, Bali.
Author Contributions
Yenny Kandarini: coordinator of research, conceptualization, study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article. Gede Wira Mahadita: problem identification and conceptualization, study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article. Sianny Herawati: performed C-terminal FGF-23, iPTH and IL-6 examination, study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article. Ida Bagus Rangga Wibhuti: performed echocardiography examination, study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article. I Gde Raka Widiana: study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article. Nyoman Paramita Ayu: study design, execution, acquisition of data, designed and performed data analysis, drafted the manuscript, reviewed and agreed to the final manuscript, and takes responsibility and accountability for the article.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Bello AK, Levin A, Tonelli M, et al. Global Kidney Health Atlas: a report by the International Society of Nephrology on the current state of organization and structures for kidney care across the globe. Brussels Int Soc Nephrol. 2017;4:e45.
2. Abdurahman A, Bandiara R, Supriyadi R. MON-055 The growing burden of end stage renal disease in Indonesia: ten years of the Indonesian renal registry reports. Kidney Int Rep. 2019;4(7):S327. doi:10.1016/j.ekir.2019.05.843
3. Health Research and Development Agency, Ministry of Health, Republic of Indonesia. Main Results of RISKESDAS 2018. Jakarta; 2018. [Badan Penelitian dan Pengembangan Kesehatan Kementerian Kesehatan RI. Hasil Utama RISKESDAS 2018. Jakarta; 2018.]
4. Pernefri. 10th Report of Indonesian Renal Registry. Jakarta; 2017.
5. Kristina SA, Endarti D, Andayani TM, Aditama H. Cost of illness of hemodialysis in Indonesia: a survey from eight hospitals in Indonesia. Int J Pharm Res. 2021;13(1):2815–2820.
6. Msaad R, Essadik R, Mohtadi K, et al. Predictors of mortality in hemodialysis patients. Pan Afr Med J. 2019;33:61. doi:10.11604/pamj.2019.33.61.18083
7. Moe SM, Sprague SM. Chronic kidney disease-mineral bone disorder. In: Skorecki K, Chertow GM, Marsden PA, Taal M, Yu AS, editors. Brenner & Rector’s the Kidney.
8. Vervloet M. Renal and extrarenal effects of fibroblast growth factor 23. Nat Rev Nephrol. 2019;15(2):109–120.
9. Liu Z-H, Yu X-Q, Yang J-W, et al. Prevalence and risk factors for vascular calcification in Chinese patients receiving dialysis: baseline results from a prospective cohort study. Curr Med Res Opin. 2018;34(8):1491–1500. doi:10.1080/03007995.2018.1467886
10. Rudenko LI, Batiushin MM, Kastanayan AA, et al. Complex assessment of risk factors for the development of cardiovascular calcification in hemodialysis patients. Int J BioMed. 2016;6(1):22–26. doi:10.21103/Article6(1)_OA4
11. Zaki S, El Gohary I, Elsharkawy E, Hashad D, Emara D, El Hameed Marwa RA. Fibroblast growth factor-23 and vascular calcification in chronic kidney disease and hemodialysis patients. J Egypt Soc Nephrol Transplant. 2018;18(1):17. doi:10.4103/jesnt.jesnt_28_17
12. Chung W-S, Shih M-CP, Wu P-Y, et al. Progression of aortic arch calcification is associated with overall and cardiovascular mortality in hemodialysis. Dis Markers. 2020;2020:1–7. doi:10.1155/2020/6293185
13. Faqih SA, Noto-Kadou-Kaza B, Abouamrane LM, et al. Calcifications valvulaires chez l’hémodialysé au Maroc. Pan Afr Med J. 2016;24. doi:10.11604/pamj.2016.24.115.7147
14. Rong S, Qiu X, Jin X, et al. Risk factors for heart valve calcification in chronic kidney disease. Medicine. 2018;97(5):e9804. doi:10.1097/MD.0000000000009804
15. Kraus MA, Kalra PA, Hunter J, Menoyo J, Stankus N. The prevalence of vascular calcification in patients with end-stage renal disease on hemodialysis: a cross-sectional observational study. Ther Adv Chronic Dis. 2015;6(3):84–96. doi:10.1177/2040622315578654
16. Wang Z, Jiang A, Wei F, Chen H. Cardiac valve calcification and risk of cardiovascular or all-cause mortality in dialysis patients: a meta-analysis. BMC Cardiovasc Disord. 2018;18(1):12. doi:10.1186/s12872-018-0747-y
17. International Society of Nephrology. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150.
18. International Society of Nephrology. KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD). Kidney Int Suppl. 2017;Jul(1):1–59.
19. Gutiérrez OM, Mannstadt M, Isakova T, et al. Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med. 2008;359(6):584–592. doi:10.1056/NEJMoa0706130
20. Choi H-M, Kwon Y-E, Kim S, Oh D-J. Changes in FGF-23, neutrophil/platelet activation markers, and angiogenin in advanced chronic kidney disease and their effect on arterial stiffness. Kidney Blood Press Res. 2019;44(5):1166–1178. doi:10.1159/000502526
21. Di Lullo L, Gorini A, Bellasi A, et al. Fibroblast growth factor 23 and parathyroid hormone predict extent of aortic valve calcifications in patients with mild to moderate chronic kidney disease. Clin Kidney J. 2015;8(6):732–736. doi:10.1093/ckj/sfv073
22. Silva AP, Gundlach K, Büchel J, et al. Low magnesium levels and FGF-23 dysregulation predict mitral valve calcification as well as intima media thickness in predialysis diabetic patients. Int J Endocrinol. 2015;2015:1–10. doi:10.1155/2015/308190
23. Chen Y, Chen Y-X, Huang C, Duan Z-B, Xu C-Y. The clinical value of klotho and FGF23 in cardiac valve calcification among patients with chronic kidney disease. IJGM. 2021;14:857–866. doi:10.2147/IJGM.S299197
24. Ganidagli B, Nacar H, Yildiz YS, et al. The relationship between serum osteopontin and FGF 23 levels with valvular calcification in hemodialysis patients. CN. 2019;91(1):9–16. doi:10.5414/CN109505
25. Bożentowicz-Wikarek M, Owczarek A, Kocełak P, Olszanecka-Glinianowicz M, Więcek A, Chudek J. C-Terminal to intact fibroblast growth factor 23 ratio in relation to estimated glomerular filtration rate in elderly population. Kidney Blood Press Res. 2016;41(5):519–526. doi:10.1159/000443452
26. Smith ER, Cai MM, McMahon LP, Holt SG. Biological variability of plasma intact and C-Terminal FGF23 measurements. J Clin Endocrinol Metab. 2012;97(9):3357–3365. doi:10.1210/jc.2012-1811
27. Ragb TM, Saad AAEA, Abd Elaal MOA. The relationship between abdominal aortic calcification and cardiac abnormalities in hemodialysis patients. EJHM. 2017;68(1):1059–1068. doi:10.12816/0038209
28. Wang AY-M. Cardiac valvular calcification as a marker of atherosclerosis and arterial calcification in end-stage renal disease. Arch Intern Med. 2005;165(3):327. doi:10.1001/archinte.165.3.327
29. Bortnick AE, Bartz TM, Ix JH, et al. Association of inflammatory, lipid and mineral markers with cardiac calcification in older adults. Heart. 2016;102(22):1826–1834. doi:10.1136/heartjnl-2016-309404
30. Vervloet MG, van Ballegooijen AJ. Prevention and treatment of hyperphosphatemia in chronic kidney disease. Kidney Int. 2018;93(5):1060–1072. doi:10.1016/j.kint.2017.11.036
31. Martin K, Floege J, Ketteler M. Bone and mineral disorders in chronic kidney diseases. In: Feehally J, Floege J, Tonelli M, Johnson R, editors. Comprehensive Clinical Nephrology.
32. Mohamed BA, Yang W, Litt H, Rosas SE. Valvular calcification, inflammation, and mortality in dialysis patients. J Heart Valve Dis. 2013;22(4):584–590.
33. Russo D, Battaglia Y. Clinical significance of FGF-23 in patients with CKD. Int J Nephrol. 2011;2011:364890. doi:10.4061/2011/364890
34. Baralić M, Brković V, Stojanov V, et al. Dual roles of the mineral metabolism disorders biomarkers in prevalent hemodialysis patients: in renal bone disease and in vascular calcification. J Med Biochem. 2019;38(2):134–144. doi:10.2478/jomb-2018-0026
35. Anand Y, Madhusudan V, Rajeevalochana P, Milly M, Deepu G, Georgi A. Correlation of serum soluble Klotho with fibroblast growth factor 23 levels in chronic kidney disease patients; a single centre study. J Neuropharmacol. 2020;9(1):1–5.
36. Jimbo R, Kawakami-Mori F, Mu S, et al. Fibroblast growth factor 23 accelerates phosphate-induced vascular calcification in the absence of Klotho deficiency. Kidney Int. 2014;85(5):1103–1111. doi:10.1038/ki.2013.332
37. Ardahanli I, Cengizhan MS, Celik M, Kader S, Akarslan M, Takir M. Carotid artery intima-media thickness and heart valve calcifications in hemodialysis patients with hyperparathyroidism (A Pilot Study). Arch Nephrol Urol. 2019;02(02):52–61.
38. Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6(4):913–921. doi:10.2215/CJN.06040710
39. Matsuo H, Dohi K, Machida H, et al. Echocardiographic assessment of cardiac structural and functional abnormalities in patients with end-stage renal disease receiving chronic hemodialysis. Circ J. 2018;82(2):586–595. doi:10.1253/circj.CJ-17-0393
40. Iwata S, Walker MD, Di Tullio MR, et al. Aortic valve calcification in mild primary hyperparathyroidism. J Clin Endocrinol Metab. 2012;97(1):132–137. doi:10.1210/jc.2011-2107
41. Soleymanian T, Nikzad N, Mahjoub A, Argani H, Saavaj S. Serum levels of intact parathyroid hormone, calcium, and phosphorus and risk of mortality in hemodialysis patients. Nephrourol Mon. 2016;9(1):41.
42. Hénaut L, Massy ZA. New insights into the key role of interleukin 6 in vascular calcification of chronic kidney disease. Nephrol Dialysis Transpl. 2018;33(4):543–548. doi:10.1093/ndt/gfx379
43. Desjardins M, Sidibe A, Fortier C, Deserres S, Lariviere R, Agharazii M. [PP.17.20] Interleukin-6 is positively associated with aortic stiffness and mortality in end-stage renal disease patients. J Hypertens. 2017;35(Supplement 2):e229–e230. doi:10.1097/01.hjh.0000523658.43883.91
44. Kamińska J, Stopiński M, Mucha K, et al. IL 6 but not TNF is linked to coronary artery calcification in patients with chronic kidney disease. Cytokine. 2019;120:9–14. doi:10.1016/j.cyto.2019.04.002
45. Choi SR, Lee Y-K, Cho AJ, et al. Malnutrition, inflammation, progression of vascular calcification and survival: inter-relationships in hemodialysis patients. PLoS One. 2019;14(5):e0216415. doi:10.1371/journal.pone.0216415
46. Ikee R, Honda K, Ishioka K, et al. Differences in associated factors between aortic and mitral valve calcification in hemodialysis. Hypertens Res. 2010;33(6):622–626. doi:10.1038/hr.2010.44
47. Lee C-T, Chua S, Hsu C-Y, et al. Biomarkers associated with vascular and valvular calcification in chronic hemodialysis patients. Dis Markers. 2013;34(4):229–235. doi:10.1155/2013/846059
48. Viaene L, Behets GJ, Heye S, et al. Inflammation and the bone-vascular axis in end-stage renal disease. Osteoporos Int. 2016;27(2):489–497. doi:10.1007/s00198-015-3233-8
49. Mathieu P, Bouchareb R, Boulanger M-C. Innate and adaptive immunity in calcific aortic valve disease. J Immunol Res. 2015;2015:1–11. doi:10.1155/2015/851945
50. Su H, Lei C-T, Zhang C. Interleukin-6 signaling pathway and its role in kidney disease: an update. Front Immunol. 2017;8:405. doi:10.3389/fimmu.2017.00405
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
