Back to Journals » Clinical Epidemiology » Volume 9
Healthy lifestyle behavior and risk of long duration troublesome neck pain or low back pain among men and women: results from the Stockholm Public Health Cohort
Authors Skillgate E , Pico-Espinosa OJ, Hallqvist J, Bohman T , Holm LW
Received 30 June 2017
Accepted for publication 6 September 2017
Published 11 October 2017 Volume 2017:9 Pages 491—500
DOI https://doi.org/10.2147/CLEP.S145264
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Vera Ehrenstein
Eva Skillgate,1,2 Oscar Javier Pico-Espinosa,1 Johan Hallqvist,3 Tony Bohman,1 Lena W Holm4
1Unit of Cardiovascular Epidemiology, Musculoskeletal and Sports Injury Epidemiology Center, Institute of Environmental Medicine, Karolinska Institutet, 2Naprapathögskolan - Scandinavian College of Naprapathic Manual Medicine, Stockholm, 3Department of Public Health and Caring Sciences, Uppsala University, Uppsala, 4Unit of Epidemiology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden
Background: The role of healthy lifestyle behavior (HLB) in terms of physical activity, alcohol intake, smoking, and diet put together has not yet been explored for the risk of low back pain (LBP) and neck pain (NP). Our aim was to study if an HLB is protective against the onset of long duration troublesome LBP and NP in men and women.
Methods: Two cohorts from the Stockholm Public Health Cohort, free from LBP (n=12,483) and NP (n=10,539), respectively, in 2006, were surveyed with questionnaires. Baseline information about physical activity, alcohol intake, diet, and smoking were dichotomized into being healthy/not healthy and combined in a categorical variable according to the number of healthy behaviors present. Binomial regression analyses were used to evaluate the role of HLB for the outcomes 4 years later.
Results: When men with three or four healthy lifestyles were compared to men with none or one, the risk ratio (RR) of LBP was 0.63 (95% confidence interval [CI]: 0.39–1.02). The corresponding RR for LBP in women was 0.86 (95% CI: 0.56–1.32). When men with three or four healthy lifestyles were compared to men with none or one, the RR for NP was 1.13 (95% CI: 0.74–1.71). The corresponding RR for NP in women was 0.52 (95% CI: 0.35–0.77).
Conclusion: An HLB seems to be protective for long duration troublesome LBP in men, and for long duration troublesome NP in women.
Keywords: neck pain, low back pain, lifestyle, physical activity, smoking, alcohol, healthy diet, prevention, musculoskeletal
Introduction
Neck pain (NP) and low back pain (LBP) are huge public health problems due to their high incidence, long duration, and social and economic impact.1 The 1-year prevalence of NP ranges between 16.7% and 75.1% (mean 37.2%) according to a global review2 and the prevalence of troublesome (activity limiting) NP lies between 1.7% and 11.5%.3 For LBP, the calculated 1-year prevalence is around 38% (0.8–82.5).4
Interest in studying the role of healthy lifestyle behaviors (HLBs) started in the sixties and an early study from the US explored how a number of behaviors correlated with better general health.5 Further, the impact of lifestyle behavior on health outcomes has been widely studied, mainly in the field of cardiovascular6 and cancer7 epidemiology, and it has been shown to be a risk factor for all-cause mortality.8 Explored risk factors or risk indicators for LBP and NP include among others, female sex, age, psychological distress, depression, and job characteristics.3,9–15 We have published a study exploring the role of an HLB for the prognosis of occasional LBP showing its importance as a protective factor for long duration troublesome back pain in women.16
Evidence for the role of lifestyle as a risk factor for these conditions is, in general, scarce and the body of literature exploring such associations consists mainly of cross-sectional studies. Analyses from the National Health and Nutrition Examination Survey showed that smoking was the strongest predictor of LBP, once analyzed with different strata of body mass index (BMI), and that moderate physical activity as well as sedentarism were associated with pain at this location.17 Another national cross-sectional study from the US shows that physical activity (even at low levels), tobacco use, alcohol intake, sleep quality, and BMI are all associated with LBP.18 Similarly, studies conducted at a national level in Iran19 and Canada20 on LBP, and in Spain on NP,21 suggest the importance of lifestyle behavior. However, longitudinal studies have shown either weak or nonsignificant associations.22–24 Understanding the role of HLB in the risk of LBP and NP may potentially have high impact implications for public health, since this can provide information on prevention strategies for the public.
Previous studies from our group have explored the role of physical activity in the risk25 and recovery of NP and back pain,26,27 suggesting it as having a protective effect in women. Similarly, previous studies on the effect of smoking and alcohol consumption on sick leave due to unspecific LBP or NP showed that the former is associated with an increased risk and the latter suggested neither an association nor a protective effect.28 Other studies have investigated the role of lifestyle by grouping HLBs (physical activity, smoking, BMI, healthy diet, and alcohol intake) in order to study a set of HLBs as one risk factor instead of treating them as individual exposures.16,29–31 A Swedish register-based cohort on the risk of atrial fibrillation combined information about BMI, physical activity, smoking, and alcohol intake and showed a significant protective effect for both men and women starting from three healthy behaviors.30 Another study on pancreatic cancer combined five factors (BMI, healthy diet, smoking, alcohol intake, and physical activity) and showed a reduction of risk among men but not among women, starting from four behaviors.29 Additionally, a meta-analysis examined the effect of different combinations of lifestyle behaviors on mortality, showing high heterogeneity of the definitions, that the effect varied depending on the reference category used, that the inclusion of BMI did not affect the main results, and that there were no differences between sexes.31
To the best of our knowledge, this way of grouping lifestyle factors into a behavior has not been used before in studies investigating associations with NP and there is only one study on the association of back pain.32 The aim of this study was therefore to determine whether HLB is protective against the onset of long duration troublesome back pain and NP in adult men and women.
Materials and methods
Ethics
All participants provided written informed consent. The present study was approved by the ethics committee at Karolinska Institutet (diary nr 2013/497-32).
Source and study population
This study is based on the Stockholm Public Health Cohort, a population-based cohort study established within the framework of Stockholm County Council public health surveys. Participants filled in an extensive baseline questionnaire and were followed longitudinally for health, lifestyle, and social outcomes via follow-up surveys. A detailed description of this cohort has previously been published.33 We included individuals (aged 18–84 years) who responded to the baseline questionnaire in 2006 and the follow-up questionnaire in 2010 for the analyses in the present study. The sample was filtered by using two questions from the 2006 questionnaire regarding NP and LBP to define “non-diseased” populations at risk.
In Cohort I, to identify potential participants to include in the study of the risk of long duration troublesome LBP, the question “During the past 6 months, have you had pain in the lower back?” with five possible answers (“no”, “yes, a few days in the past 6 months”, “yes, a few days per month”, “yes, a few days per week,” or “yes, every day”) was used. Those who answered “no” were considered to be free from LBP and therefore formed the study population at risk for LBP. For cohort II participants, to study the risk of long duration troublesome NP, the question “During the past 6 months, have you had pain in the neck, the shoulders, or the arms?” was used, with equal response options as for the question to identify cohort I. Those who answered “no” were considered to be free from NP and therefore formed the study population at risk for NP. Furthermore, those with incomplete information about the exposure were excluded from Cohorts 1 and 2. These two cohorts are not mutually exclusive (Figure 1): 55% of those in Cohort I had NP and 65% of those in Cohort II had LBP.
  | Figure 1 Flow chart of participants of the Stockholm Public Health Cohort between 2006 and 2010 and sample included in the study populations. Abbreviations: LBP, low back pain; NP, neck pain. |
Exposure
Information about lifestyle behavior was collected from the baseline questionnaire in 2006, by grouping four lifestyle behaviors into being healthy/not healthy. Physical activity was dichotomized using 150 minutes of physical activity at moderate intensity or 75 minutes at high intensity per week, or a combination of these as cutoff points based on two questions: the first one asking for the level of intensity of physical activity and the other one using the number of days of physical activity per week.34 Smoking was assessed by asking whether the person smoked daily or not.35 Alcohol intake was evaluated with various questions: the person was asked to fill in the amount, type, and frequency of average consumption of various alcoholic drinks. The amount of grams of alcohol consumed per week was then calculated from these data. The value was dichotomized following World Health Organization recommendations on no risk consumption of alcohol (≤168 g 100% alcohol/week for men and ≤108 g 100% alcohol/week for women).36 Consuming alcohol corresponding to approximately half a bottle of spirits on the same occasion less than once a month was also classified as no risk drinking. Healthy diet was dichotomized using the cutoff point of four portions of fruits and vegetables per day.37 Finally, a three categories variable was built according to the number of variables and regardless of the type of habit. These categories are none or one healthy behavior (reference category), two behaviors, and three and/or four healthy behaviors.
Outcomes
There are two outcomes in this study: long duration troublesome LBP and long duration NP. These categorizations were based on the following questions in the questionnaire from 2010: “During the past 6 months, have you had pain in the lower part of the back” (Cohort I) and “During the past 6 months, have you had pain in the upper part of the back or neck?” (Cohort II). Those who answered “yes, a couple of days per week” or more often, and additionally reported at least some extent of interference in their daily activities including work were considered to have the outcomes of interest. The question was “Has such pain caused a decreased ability to work or impairment in daily activities?”. The answer alternatives were yes, to a high extent; yes, to some extent; and not at all.
Potential confounders
A number of potential confounders obtained from the literature3,15,38–41 and from clinical considerations were considered for the association between exposure and outcome (Table 1).
  | Table 1 Potential confounding variables Notes: aTested as confounder in Cohort II. bTested as confounder in Cohort I. Abbreviations: LBP, low back pain; NP, neck pain. |
Statistical analyses
Analyses were performed separately for each of the two sub-cohorts and stratified by sex. Cross-tabulation was done for the variables of interest to describe the study subpopulations. Generalized linear models with a binomial link function were used to estimate the association between exposure and outcome, and to test for and adjust for confounding. The results are presented as risk ratio (RR) together with 95% confidence intervals (CI). Potential confounders were entered to the model one at a time. If a factor made a change of at least 5% on the RR, it was included in the final multivariable model. This procedure was performed separately for men and women and for each cohort. All the computations were executed with Stata v. 13.0 (StataCorp LP, College Station, TX, USA).
Results
Prevalence of HLBs at baseline
In Cohort I (risk of LBP), 23% (19% women and 27% men) reported no or one HLB at baseline. The prevalence of two HLBs was 42% (women 39%; men 44%), the prevalence of three was 28% (women 31%; men 26%), and the prevalence of four was 7% (women 11%; men 3%).
In Cohort II (risk of NP), 23% (19% women and 27% men) reported no or one HLB at baseline. The prevalence of two HLBs was 41% (women 39%; men 44%), the prevalence of three was 28% (women 31%; men 25%), and the prevalence of four was 8% (women 11%; men 4%).
Risk of LBP
For cohort I (risk of LBP), women accounted for 50% of the population at risk and represented a higher proportion in the upper category of the exposure, and the mean age was 48 years. The most common social class corresponded to intermediate nonmanual employees and professionals (Table 2). The proportion that at the follow-up in 2010 had developed LBP that was long-lasting and troublesome was 3% (n=379) (3% of men and 4% of women).
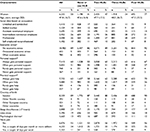  | Table 2 Baseline characteristics of Cohort I (risk of LBP) in relation to number of HLBs Notes: aEach category corresponds to the answer provided to the question on economic stress as presented in Table 1: no in the last 12 months (no economic stress), in one occasion in the last 12 months (occasional economic stress), and in various occasions in the last 12 months (often economic stress). bSimilarly, personal and practical support correspond to the answers provided as presented in Table 1. Yes, always (always gets help/personal support); yes, most of the time (often gets help/personal support); no, not most of the time (rarely gets help/personal support); no, never (never gets help/personal support). cPsychological distress was calculated and dichotomized based on 12 questions from the General Health Questionnaire, using the scoring system 0–0–1–1, with ≥3 points indicating the presence of it. Abbreviations: HLBs, healthy lifestyle behaviors; SD, standard deviation; LBP, low back pain. |
An RR of 0.72 (95% CI: 0.53–0.98) was observed for those with three or four HLBs in comparison to those with none or one, in the group of all individuals. In the sex-stratified analyses, the corresponding figure for men was 0.63 (95% CI: 0.39–1.02), and 0.86 (95% CI: 0.56–1.32) for women (Table 3). For individuals with two HLBs, the RR was 0.87 (95% CI: 0.65–1.16).
Risk of NP
For cohort II (risk of NP), women accounted for 43% of the population at risk and represented a lower proportion in the first two categories of the exposure. The mean age was 49 years. The most common social class corresponded to intermediate nonmanual employees and professionals (Table 4). The proportion that at the follow-up in 2010 had developed NP that was long-lasting and troublesome was 5% (n=464) (5% of men and 6% of women).
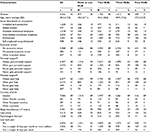  | Table 4 Baseline characteristics of Cohort II (risk of NP) in relation to number of HLBs Notes: aEach category corresponds to the answer provided to the question on economic stress as presented in Table 1: no in the last 12 months (no economic stress), in one occasion in the last 12 months (occasional economic stress), and in various occasions in the last 12 months (often economic stress). bSimilarly, personal and practical support correspond to the answers provided as presented in Table 1. Yes, always (always gets help/personal support); yes, most of the time (often gets help/personal support); no, not most of the time (rarely gets help/personal support); no, never (never gets help/personal support). cPsychological distress was calculated and dichotomized based on 12 questions from the General Health Questionnaire, using the scoring system 0–0–1–1, with ≥3 points indicating the presence of it. Abbreviations: NP, neck pain; HLB, healthy lifestyle behavior; SD, standard deviation. |
An RR of 0.79 (95% CI: 0.59–1.06) was observed for those with three or four HLBs in comparison to those with none or one, in the group of all individuals. In the sex-stratified analyses, the corresponding figure for men was 1.13 (95% CI: 0.74–1.71), and for women was 0.52 (95% CI: 0.35–0.77) (Table 5). For individuals with two HLBs, the RR was 1.05 (95% CI: 0.81–1.37).
Discussion
Our study indicates that HLB in a group free from pain in the lower back and neck, respectively, may protect against long duration troublesome pain in the back or neck 4 years later. The effect tends to differ between sexes, since sex-stratified analyses showed a more explicit protection from LBP in men and a more explicit protection from NP in women.
As stated in the “Introduction” section, the combined effect of lifestyle behaviors has not been widely studied in relation to the risk of LBP or NP. In our previously published study, also based on the Stockholm Public Health Cohort 2006–2010, we used similar definitions to operationalize the exposure (used “none” healthy behaviors instead of “none or one” as reference category and there were in total five instead of three categories) to study the prognosis of occasional LBP, for the risk of troublesome LBP.16 The study showed that women with healthier lifestyle behavior had a better prognosis compared to their male counterparts, and no significant association was observed among men. Even though the study concerned the risk of a worse prognosis instead of the risk of actually getting LBP, its results contrast those of the present study since no clear effect in women was found. A study by Pronk et al, that compared the combined effect of healthy behaviors on the risk of back pain, showed a protective effect for those in the category of four and three healthy behaviors;32 nonetheless, that study had a risk of selection bias due to the so-called healthy worker effect.
Some considerations should be made concerning the classification of exposures in our study when interpreting the results. A more detailed categorization of HLB has been used in previous studies,31 but that would require an even larger study population for sufficient statistical power. Although efforts were made to capture a valid measure of lifestyle behavior, measurement error and misclassification of exposure may be present. For instance, smoking was measured with a yes/no question about daily smoking, which is a rough measure of such exposure. By categorizing former smokers as nonsmokers and smokers who only smoke a few cigarettes a day as smokers, we might have introduced a misclassification of this exposure, which most likely would be non-differential, thus diluting the associations.
One study derived from our literature review included diet as a potential risk factor. It considered animal protein intake instead of fruit and vegetable consumption and showed a negative association with LBP.45 The rationale behind these findings is, however, not clear, but opens up the discussion on whether other components of diet such as fish, whole grains, legumes, sweetened beverages, or sodium might play a more direct role in the pathophysiology of pain.
The time between the measurement of exposure and the outcome was 4 years, and lifestyle behaviors might have changed over this period. Since the study aimed to investigate the association between HLB in the previous 12 months and the risk of pain 4 years later, such changes of exposure status may not be considered a source of bias in this study. Nevertheless, information bias cannot be excluded, being likely non-differential in its nature, with a risk of dilution of a true association. Regarding this, we think it is unlikely that such potential bias differs by sex. In a similar way, and considering the fluctuating characteristic of NP and LPB, there is a risk of misclassification of the outcome, especially considering that some individuals might be indecisive between reporting “a couple of days per week” or “a couple of days per month”. Such misclassification of the outcome is most probably non-differential in its nature, leading to dilution of a true association.
One strength of this study is the relative large sample size which permitted exploring the risk along different levels of HLB. The longitudinal design allowed a temporal relation of risk between the studied exposure and the outcomes. We have considered a long row of potential confounders in this study, but we cannot rule out that there is unmeasured or residual confounding. These include passive smoking, which was not addressed in the Stockholm Public Health Cohort questionnaire and has been reported as a potential factor associated with pain in the knee, neck, and/or back;19 specific psychiatric diagnoses;46 or specific occupations.47
The response rate for the baseline questionnaire was 67% in women and 56% in men33 and 2%–3% of the responders at baseline had missing values at questions about the exposure. Nonparticipation at baseline is not likely to create a selection bias in a prospective etiological study. The response rate between 2006 and 2010 was acceptable (around 75%), but there is still a risk for selection bias. By comparing those who did and did not respond to the follow-up questionnaire, we found that the former had a higher compliance to better lifestyle behavior (37% of those who remained in the cohorts had three or four HLBs in comparison to 30% in those who withdrew). If the nonresponders also had a higher occurrence of the outcome compared to the responders, our results may be somewhat underestimated.
A methodological consideration is that we have interpreted our results as the presence of an association between HLB and LBP/NP despite the results not always being statistically significant. Various authors have previously addressed this discussion in epidemiological journals encouraging researchers to consider the interplay of factors beyond the results of statistical testing.48,49 Therefore, the authors consider that this study has enough elements to support the presence of an association.
No single explanation can be given to the potential mechanism behind the protective association between HLB and risk of developing NP or LBP, but rather it is likely that there is an interaction of emotional, biochemical, and mechanical components. For instance, individuals with a healthy lifestyle might feel more confident on their decreased risk of chronic diseases or their ability to overcome pain; the protective effect of HLB might be mediated by low-grade inflammation; and individuals with HLB are more likely to be fitter, less obese, and more self-conscious in general. Likewise, given that it is unknown how long the induction period for NP or LBP is, no theory provides sound support in this case.
It is hard to explain sex differences of the effect observed in this study. It is well known that differences between men and women exist in terms of pain characteristics and/or intensity for chronic nonspecific pain. In inflammatory arthritis, for example, women have more often peripheral instead of axial pain, and in disc herniation, they often have more radiating pain.13,42–44 However, such differences in the occurrence of pain does not explain why lifestyle may have a differential degree of protection by sex and pain location. This, however, might in fact just be a chance finding. Although a different cutoff point was used to define risky consumption of alcohol by sex, the cutoff follows international recommendations and does not explain the discordant results in this study.
Conclusion
A HLB seems to be protective for the risk of developing long duration troublesome LBP in men and long duration troublesome NP in women. Authors recommend the promotion of a healthy lifestyle for both men and women given the evidence regarding its benefits for these and other health conditions.
Disclosure
The authors report no conflicts of interest in this work.
References
Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(9995):743–800. | ||
Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J. 2006;15(6):834–848. | ||
Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population. Results of the Bone and Joint Decade 2000–2010 Task Force on neck pain and its associated disorders. J Manipulative Physiol Ther. 2009;32(2):S46–S60. | ||
Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. | ||
Belloc NB, Breslow L. Relationship of physical health status and health practices. Prev Med. 1972;1(3):409–421. | ||
Claas SA, Arnett DK. The role of healthy lifestyle in the primordial prevention of cardiovascular disease. Curr Cardiol Rep. 2016;18(6):56. | ||
Khan N, Afaq F, Mukhtar H. Lifestyle as risk factor for cancer: evidence from human studies. Cancer Lett. 2010;293(2):133–143. | ||
Ford ES, Bergmann MM, Boeing H, Li C, Capewell S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med. 2012;55(1):23–27. | ||
Pinheiro MB, Ferreira ML, Refshauge K, et al. Symptoms of depression and risk of new episodes of low back pain: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2015;67(11):1591–1603. | ||
Rasmussen-Barr E, Grooten WJ, Hallqvist J, Holm LW, Skillgate E. Are job strain and sleep disturbances prognostic factors for neck/shoulder/arm pain? A cohort study of a general population of working age in Sweden. BMJ Open. 2014;4(7):e005103. | ||
Paanalahti K, Holm LW, Magnusson C, Carroll L, Nordin M, Skillgate E. The sex-specific interrelationship between spinal pain and psychological distress across time in the general population. Results from the Stockholm Public Health Study. Spine J. 2014;14(9):1928–1935. | ||
McLean SM, May S, Klaber-Moffett J, Sharp DM, Gardiner E. Risk factors for the onset of non-specific neck pain: a systematic review. J Epidemiol Community Health. 2010;64(7):565–572. | ||
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–485. | ||
Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum. 2007;57(4):656–665. | ||
Kääriä S, Laaksonen M, Rahkonen O, Lahelma E, Leino-Arjas P. Risk factors of chronic neck pain: a prospective study among middle-aged employees. Eur J Pain. 2012;16(6):911–920. | ||
Bohman T, Alfredsson L, Jensen I, Hallqvist J, Vingård E, Skillgate E. Does a healthy lifestyle behaviour influence the prognosis of low back pain among men and women in a general population? A population-based cohort study. BMJ Open. 2014;4(12):e005713. | ||
Smuck M, Kao MJ, Brar N, Martinez-Ith A, Choi J, Tomkins-Lane CC. Does physical activity influence the relationship between low back pain and obesity? Spine J. 2014;14(2):209–216. | ||
Yang H, Haldeman S. Behavior-related factors associated with low back pain in the US adult population. Spine (Phila Pa 1976). Epub 2016 Apr 26. | ||
Noormohammadpour P, Mansournia MA, Koohpayehzadeh J, et al. Prevalence of chronic neck pain, low back pain and knee pain and their related factors in community-dwelling adults in Iran: a population-based national study. Clin J Pain. 2017;33(2):181–187. | ||
Bath B, Trask C, Jesse M, Lawson J. Demographic and health characteristics of rural- and urban-dwelling Canadians with chronic back disorders. A population-based comparison. Spine (Phila Pa 1976). 2014;39(23):1960–1968. | ||
Palacios-Ceña D, Alonso-Blanco C, Hernández-Barrera V, Carrasco-Garrido P, Jiménez-García R, Fernández-de-las-Peñas C. Prevalence of neck and low back pain in community-dwelling adults in Spain: an updated population-based national study. Eur Spine J. 2015;24:482–492. | ||
Brady SRE, Hons M, Hons B, Hussain SM. Predictors of back pain in middle aged women: data from the Australian longitudinal study on women’s health. Arthritis Care Res (Hoboken). 2017;69(5):709–716. | ||
Heuch I, Heuch I, Hagen K, Zwart J. Is there a U-shaped relationship between physical activity in leisure time and risk of chronic low back pain? A follow-up in the HUNT Study. BMC Public Health. 2016;16:306. | ||
Nakamura M, Nishiwaki Y. Prevalence and characteristics of chronic musculoskeletal pain in Japan: a second survey of people with or without chronic pain. J Orthop Sci. 2014;19:339–350. | ||
Palmlöf L, Holm LW, Alfredsson L, Magnusson C, Vingård E, Skillgate E. The impact of work related physical activity and leisure physical activity on the risk and prognosis of neck pain – a population based cohort study on workers. BMC Musculoskelet Disord. 2016;17:219. | ||
Bohman T, Alfredsson L, Hallqvist J, Vingård E, Skillgate E. The influence of self-reported leisure time physical activity and the body mass index on recovery from persistent back pain among men and women: a population-based cohort study. BMC Public Health. 2013;13:385. | ||
Rasmussen-Barr E, Bohman T, Hallqvist J, Holm LW, Skillgate E. Do physical activity level and body mass index predict recovery from persistent neck pain in men and women of working age? A population-based cohort study. Eur Spine J. 2013;22(9):2077–2083. | ||
Skillgate E, Vingard E, Josephson M, Holm LW, Alfredsson L. Is smoking and alcohol consumption associated with long-term sick leave due to unspecific back or neck pain among employees in the public sector? Results of a three-year follow-up cohort study. J Rehabil Med. 2009; 41:550–556. | ||
Jiao L, Mitrou P, Reedy J, et al. A combined healthy lifestyle score and risk of pancreatic cancer – a large cohort study. Arch Intern Med. 2009;169(8):764–770. | ||
Larsson SC, Drca N, Jensen-Urstad M, Wolk A. Combined impact of healthy lifestyle factors on risk of atrial fibrillation: prospective study in men and women. Int J Cardiol. 2016;203:46–49. | ||
Loef M, Walach H. The combined effects of healthy lifestyle behaviors on all cause mortality: a systematic review and meta-analysis. Prev Med. 2012;55(3):163–170. | ||
Pronk NP, Lowry M, Kottke TE, Austin E, Gallagher J, Katz A. The association between optimal lifestyle adherence and short-term incidence of chronic conditions among employees. Popul Health Manag. 2010;13(6):289–295. | ||
Svensson AC, Fredlund P, Laflamme L, et al. Cohort profile: the Stockholm Public Health Cohort. Int J Epidemiol. 2013;42(5):1263–1272. | ||
WHO. Physical activity and adults. Global strategy on diet, physical activity and health [updated 2015]. Available from: http://www.who.int/dietphysicalactivity/factsheet_adults/en/. Accessed November 18, 2016. | ||
WHO. Tobacco free initiative (TFI) [updated 2015]. Available from: http://www.who.int/tobacco/en/. Accessed November 18, 2016. | ||
Andreason S, Allebeck P. Alkohol Och Hälsa. Stockholm: Statens Folkhälsoinstitut; 2005. Swedish. | ||
WHO. A healthy lifestyle [updated 2014]. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle. Accessed November 18, 2016. | ||
Unden AL, Orth-Gomer K. Development of a social support instrument for use in population surveys. Soc Sci Med. 1989;29(12):1387–1392. | ||
Dario AB, Ferreira ML, Refshauge KM, Lima TS, Ordoñana JR, Ferreira PH. The relationship between obesity, low back pain, and lumbar disc degeneration when genetics and the environment are considered: a systematic review of twin studies. Spine J. 2015;15(5):1106–1117. | ||
Palmlöf L, Skillgate E, Alfredsson L, et al. Does income matter for troublesome neck pain? A population-based study on risk and prognosis. J Epidemiol Community Health. 2012;66:1063–1070. | ||
Goldberg DP, Gater R, Sartorius N, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27(1):191–197. | ||
Barnabe C, Bessette L, Flanagan C, et al. Sex differences in pain scores and localization in inflammatory arthritis: a systematic review and metaanalysis. J Rheumatol. 2012;39(6):1221–1230. | ||
Tschugg A, Loscher WN, Hartmann S, Neururer S, Wildauer M, Thome C. Gender influences radicular pain perception in patients with lumbar disc herniation. J Womens Health (Larchmt). 2015;24(9):771–776. | ||
Mogil JS, Bailey AL. Sex and gender differences in pain and analgesia. Prog Brain Res. 2010;186:141–157. | ||
Karunanayake AL, Pathmeswaran A, Kasturiratne A, Wijeyaratne LS. Risk factors for chronic low back pain in a sample of suburban Sri Lankan adult males. Int J Rheum Dis. 2013;16:203–210. | ||
Larson SL, Clark MR, Eaton WW. Depressive disorder as a long-term antecedent risk factor for incident back pain: a 13-year follow-up study from the Baltimore Epidemiological Catchment Area sample. Psychol Med. 2004;34(2):211–219. | ||
Côté P, van der Velde G, Cassidy JD, et al. The burden and determinants of neck pain in workers. Results of the Bone and Joint Decade 2000–2010 Task Force on neck pain and its associated disorders. J Manipulative Physiol Ther. 2009;32(2):S70–S86. | ||
Ahlbom A. Significance testing: why does it prevail? Eur J Epidemiol. 2017;32(1):1–2. | ||
Senn SJ, Rothman KJ, Carlin JB, et al. Statistical tests, P values, confidence intervals, and power: a guide to misinterpretations. Eur J Epidemiol. 2016;31(4):337–350. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


