Back to Journals » International Journal of General Medicine » Volume 16
Healthcare Workers’ Vulnerability to SARS-CoV-2 in Western Romania: A Study on Incidence and Risk Factors for Non-Vaccination and Reinfection
Authors Gal-Nădășan EG, Popescu IM , Bădițoiu LM , Gal-Nădășan N , Cioca F, Popovici ED , Dinu AR, Horhat FG , Margan MM, Vulcănescu DD , Anghel A, Marian C, Căpraru ID
Received 3 October 2023
Accepted for publication 16 November 2023
Published 28 November 2023 Volume 2023:16 Pages 5621—5632
DOI https://doi.org/10.2147/IJGM.S442098
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Emanuela-Georgiana Gal-Nădășan,1 Irina-Maria Popescu,2 Luminița Mirela Bădițoiu,2,3 Norbert Gal-Nădășan,4 Flavius Cioca,5 Emilian Damian Popovici,2 Anca-Raluca Dinu,6 Florin George Horhat,3,7 Mădălin-Marius Margan,8 Dan Dumitru Vulcănescu,7 Andrei Anghel,9 Cătălin Marian,9 Ionuț Dragoș Căpraru2,10
1Dr. Sandesc’ Medpoint Medical Center, Mosnita-Nouă, Romania; 2Department of Epidemiology, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 3Multidisciplinary Research Center on Antimicrobial Resistance, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 4Department of Automation and Applied Informatics, Faculty of Automation and Computers, Politehnica University, Timişoara, Romania; 5Department of Medical Informatics and Biostatistics, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 6Department of Medical Recovery, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 7Department of Microbiology, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 8Department of Functional Sciences, Discipline of Public Health, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 9Department of Biochemistry, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 10Public Health Authority of Timis County, Timisoara, Romania
Correspondence: Irina-Maria Popescu, Department of Epidemiology, “Victor Babes” University of Medicine and Pharmacy, Eftimie Murgu Square, No. 2, Timisoara, 300041, Romania, Tel +40 744 476 380, Email [email protected]
Purpose: The COVID-19 pandemic has severely impacted healthcare workers, a professional category at risk of infection in both hospital and community settings. The aim of the study was to compare morbidity among hospital staff and that in general population, as well as the factors predicting non-vaccination and reinfection.
Patients and Methods: The present study is a retrospective, cross-sectional study. It was conducted by including all the confirmed COVID-19 infection cases in medical staff members during the period 01.01.2021– 31.03.2022 that were reported to the Public Health Authority of Timis County, Timisoara, Western Romania.
Results: Direct, strong, statistically significant correlations were found between the incidence of COVID-19 recorded in all categories of medical personnel and the community pandemic trend, with maximum values for auxiliary and medium medical staff (rho = 0.852/0.821, p < 0.001). The high socio-economic level, as well as the advanced medical education level, were predictor factors for anti-SARS-COV-2 vaccination among the personnel. The non-vaccinated status as well as incomplete vaccination or even the 2-dose vaccination represented independent risk factors for reinfection in 2022. Conversely, receiving a higher number of vaccine doses emerged as the primary protective factor. Notably, reduced adherence to the administration of the following doses was observed particularly among medium and auxiliary staff, leading to additional risks of infection with the Omicron variant.
Conclusion: Despite over 70% vaccination coverage among all studied medical personnel categories, there was low adherence to repeat doses of vaccination, particularly among medium and auxiliary staff. The study highlighted a distinct necessity for enhanced training on preventive behaviours and targeted prevention/control strategies for all professional groups interacting with patients, including caretakers, ambulance workers, receptionists, physiotherapists, and psychologists.
Keywords: COVID-19, healthcare workers, incidence, vaccination, predictor factors
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Fikri has been published for this article.
Introduction
The easy transmission via Flugge’s droplets and aerosols, respectively, the infectivity of asymptomatic carriers and the general receptivity to the emerging virus, quickly categorised the infection with SARS-COV-2 as an occupational pathology, especially for medical unit personnel. As early as the onset of the pandemic, certain studies focused on the possible classification of COVID-19 as occupational pathology.1,2 In 2021, most EU countries regarded the SARS-COV-2 infection either as an occupational disease or as a work-related accident. In Romania, by February 2022 the legislation was adjusted to include the emerging infection in the list of occupational pathologies.3,4 However, starting with 2020, it became clear that only a portion of the total number of infections among medical staff members could be attributed to healthcare, the rest being correlated to community transmission. A Centers for Disease Control and Prevention study conducted on infected medical staff members in the USA and published in 2022 revealed that 52.0% reported known exposures at the workplace, 30.8% at home and 25.6% in the community.5
In the scientific literature, the incidence of COVID-19 ranged from 0.4%, based on 498 healthcare providers in Spain, up to 57.06% in a study conducted on medical staff members in New York.6,7 In a study conducted between 31.01.2020 and 31.01.2021, in which 9 European countries took part, the attack rate among medical personnel (versus workers in other fields) was 3.0[95% confidence interval (CI) 2.2–4.0] for infection, 1.8[95% CI 1.2–2.7] for hospitalization, 1.9[95% CI 1.1–3.2] for ICU admission and 0.9[95% CI 0.4–2.0] for death. The case-fatality ratio was 1.8% among hospitalised medical staff.8
Although the onset stage of the pandemic was the most challenging (in Spain, for instance, 24.1% of the cases confirmed during the first pandemic wave were medical staff members), each pandemic wave increased the risks of exposure for the staff in medical units.9 In Canada, from June 2021 to January 2022, the number of positive cases in healthcare providers increased from 94,873 to 150,546, representing 4.5% of the total COVID-19 cases recorded, as compared to 19.4% of the total number of cases in the period between January 15 and July 23, 2020.10
In terms of fatality, between January 2020 and May 2021, the surveillance data worldwide recorded 6643 deaths among medical and healthcare personnel. The estimation performed by the International Labour Organization, aiming to address under-reporting, identifies a range between 80,000 and 180,000 deaths, with an average of 115,500 deaths.11,12
Romania occupies a special position among European countries. Factors such as the lack of vaccine-supportive legislation, the significant and consistent emigration of medical personnel over the past 30 years, the consecutive decrease in medical care, especially in rural areas, the pronounced ageing of primary care physicians, the reduced emphasis on health education for younger generations, contributed to one of the lowest anti-COVID-19 vaccine coverages in the European Union.13 In February 2022, the percentage of vaccinated subjects was 44.62% of the eligible population over 5 years and 50.43%, of the adult population.14 Given these circumstances, over 2.8 million cases had been reported until May 2022, with 65,540 COVID-19 attributable deaths and a mean fatality of 2.34%, and until August 2022, there had been 3,195,253 confirmed cases with 66,547 deaths and 16,065,431 administered vaccine doses.15,16
Regarding the medical personnel, 3267 cases were recorded until June 2020 (14% of the total number of infections with the novel coronavirus SARS-COV-2) and 18,616 cases (1.02%), with 103 deaths until the end of 2021.17,18 The vaccination of medical staff members who were regarded as being at maximum infection risk started on the 27th of December 2020 but the hesitancy/refusal percentage has also been significantly higher than in other European countries.13
The present study followed the analysis of COVID-19 infection cases in medical staff members of the administrative-territorial units of Western Romania, highlighting certain predictor factors for non-vaccination and reinfection, respectively.
Materials and Methods
Study Design
We conducted an observational, retrospective, cross-sectional study, including all confirmed COVID-19 infection cases in medical staff members during the period 01.01.2021–31.03.2022 and reported to the Public Health Authority of Timis County, in Western Romania.
The reporting entities were 8 tertiary medical units (6 public hospitals and 2 private hospitals) and the Timis County Ambulance Service. All the units were located in urban areas, most of them in Timisoara and only 2 in the rest of the county, most with mixed medical-surgical profiles and 2 with clinical medical – oncology/metabolic diseases and medical rehabilitation specialities. Together with the 6 units with regional addressability (patients coming from 4 counties in the West and South-West of Romania), there were 1 city hospital and one medical centre with a unique medical profile treating patients from the entire country. One hospital exclusively cares for paediatric cases, while the other 3 include paediatrics departments. None of the 8 hospitals is exclusively dedicated to the treatment of transmissible diseases but 5 of them were included on the list of support-COVID-19 medical institutions.
All the confirmed cases of COVID-19 infection in the employees of these medical institutions in 2021 and the first 3 months of 2022 reported to the surveillance authorities were included. The confirmation was done according to the case definitions in the Methodologies of COVID-19 surveillance elaborated by the National Institute of Public Health in Romania. Thus, a possible case was suspected in the presence of at least one of the following symptoms: cough, shortness of breath, sudden onset of anosmia, ageusia or dysgeusia. A probable case was represented by persons with the previously mentioned clinical criteria and with epidemiologic links (direct contact with a COVID-19 case during the 14 days before the onset – in 2021 and 10 days in January 2022 and 7 days starting from February 2022, respectively) or persons who fulfil the imagistic diagnosis criteria – the presence of radiological aspects suggestive for COVID-19.19–21
The confirmed case was represented by subjects who fulfilled the laboratory criteria: the detection of the nucleic acid by RT-PCR (N = 2131/90.26%) or identification of the SARS-COV-2 antigen by rapid tests (N = 230/9.74%), in the nasal-pharyngeal swab or another biological sample. The collection of specimens was done in the medical units included in the study or in laboratories authorised to perform RT-PCR tests in the county. The Romanian methodology required that confirmation of cases by rapid tests be conducted in an institutional environment, excluding self-testing.
All the cases included in the study are found in Corona Forms, the national system used for the surveillance of the infection with SARS-COV-2.
These cases were further grouped and statistically analysed depending on gender, vaccine status, the presence of COVID-19 medical history (officially recorded in Corona Forms), classification in the pandemic waves – 3 (January–March 2021), 4 (September–November 2021) or 5 (January–March 2022), and depending on the category of staff. According to the latter criterion, 4 sub-samples were formed:
- E1 higher education medical staff – including medical residents, specialists/consultants or other staff with university studies: biologists, chemists, physicists, pharmacists, psychologists;
- E2 medium education medical staff – composed of medical nurses, kinesiotherapists, pharmacy nurses and imaging technicians;
- E3 auxiliary medical staff – hospital attendants, caretakers, ambulance workers, medical record keepers or receptionists;
- and E4 administrative staff – management and office staff, guard and protection services, kitchen staff, maintenance staff etc.
To identify the predictors for reinfection, the cases were grouped into 2 samples – personnel members with the first infection versus those with reinfection defined as the presence in the national surveillance system of another COVID-19 infection in the same individual with at least 180 days before. Also, to reveal predictive factors for non-vaccination, the entire sample was subdivided into a group of persons who were not vaccinated at the time of infection and another group with complete vaccination (2 doses or 1 dose for the J&J vaccine).
The community monthly incidence of novel coronavirus infection in Timis county was calculated as the arithmetic mean of the daily incidence of COVID-19. The latter is a cumulative incidence over the last 14 days, in 1000 inhabitants and provided on the website of the Public Health Authority of Timis County.22 The monthly incidence of cases reported to the county health authorities, recorded in medical staff members was calculated as the total number of cases in the month in question reported to the number of medical staff members in Timis county, as provided by the database of the Public Health Authority of Timis County.
Data were collected according to the requirements of the EU Regulation 679/2016 on the protection of individuals regarding the processing of personal data and their free circulation. The study was conducted with the approval of the Ethics Commission of the Public Health Authority of Timis County no. 29517/15.11.2021.
Statistical Analysis
The statistical analysis of data was done with EPI INFO version 7.2.50 and IBM SPSS Statistics 20 (SPSS Inc., Chicago, IL). Numerical variables were defined by median and interquartile range (IQR), and category variables were defined by value and percentage. The Kolmogorov–Smirnov test was used to test data distribution. The numerical variables were compared using the non-parametric Mann–Whitney U-test for independent samples or the ANOVA parametric test. The category-type variables were compared with the 2×2 and 2×3/2×4 contingency tables, respectively, and the hi2 test (Fisher exact test). For the bivariate correlation, the Spearman rho correlation coefficient was applied. The variables that met the criteria of statistical significance in the univariate analysis (p < 0.05) were investigated by logistic regression, choosing the model depending on the Nagelkerke R2 coefficient and the test for the assessment of deviation from the theoretical model of Hosmer and Lemeshow. The tests were two-tailed, and the threshold value was set at p <0.05.
Results
The sample included 2361 cases of SARS-COV-2 infection in medical staff members of health units in 2021 and the first 3 months of 2022, a period during which community waves 3, 4 and 5 were recorded. One thousand fifty-seven positive cases (44.77% of the total number of reported cases) were recorded during the entire year 2021, while 1304 (55.23%) were identified only during the first 3 months of 2022.
The incidence peaks for all categories of staff, during the monitored period, were recorded in January 2022, with 5.80% among the higher education medical staff, 7.82% for the medium education medical staff, 7.65% for the auxiliary and 4.08% for the administrative staff. The average monthly incidence was 1.92% for auxiliary staff, 1.77% for middle education medical staff, 1.19% for higher education medical staff and 0.82% for administrative staff. The incidence of COVID-19 reported in the medical staff correlated directly, strongly and significantly with the community incidence in the respective territory (E1-rho = 0.752, p = 0.001; E2-rho = 0.821, p < 0.001; E3-rho = 0.852, p < 0.001 and E4-rho=0.739, p = 0.002), as shown in Figure 1.
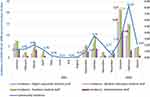 |
Figure 1 The evolution of COVID-19 incidence in the community and among medical personnel. |
The distribution of cases depending on the category of personnel revealed the preponderance of the medical staff with medium education with 979 cases (41.46%), followed by the medical staff with university education with 630 cases (26.68%), the auxiliary personnel – 620 cases (26.26%) and the administrative sector with 132 cases (5.59%).
The impact on the various categories of medical staff differed depending on specialty (Figure 2).
 |
Figure 2 The impact on various categories of medical personnel depending on specialty. |
The 3 categories of surgical and medical staff (adults) were similarly affected (p = 0.422/0.854), in paediatric and intensive care units the higher education staff pre-vailed (p = 0.046/0.005), in paraclinical departments, the medium staff was more affected (p = 0.036) while in ambulance/emergency room services, the auxiliary personnel were significantly more affected (p < 0.001).
The vaccine status, at the end of the period supervised, varied with extreme statistical significance (p < 0.001), with minimal values of non-vaccination in E1 (6.83%) and maximal values among auxiliary medical staff members (29.35%). The Comirnaty vaccine (Pfizer-BioNTech) was chosen by most higher education medical staff and administrative staff, while the Janssen/J&J vaccine was significantly more frequently administered in medium and auxiliary staff (p < 0.001) (Figure 3).
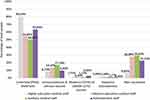 |
Figure 3 Vaccine status of medical staff reported as COVID-19-positive. |
Other recorded differences between the 4 sub-samples are presented in Table 1.
 |
Table 1 Variables with Statistically Significant Differences Between the 4 Categories of Personnel |
The gender-based comparison of personnel members identified a statistically significant higher percentage of non-vaccinated women - 24.18% versus 15.93% (p < 0.001), OR = 1.68[1.29–2.19], together with a lower average number of vaccine doses - 1.60 versus 1.91 (p < 0.001). The number of symptoms was significantly higher in women - 1.90 versus 1.44 (p < 0.001).
To identify the differences occurring in time, the first 3 months of 2021 representing the 3rd pandemic wave were compared to the September–November period of 2021 corresponding to the 4th wave when the predominant circulating variant was Delta (B.1.617.2) and to January–March 2022 that reflect the 5th wave when the prevalent SARS-COV-2 variant was Omicron (B.1.1.529). The relevant differences were recorded in Table 2.
 |
Table 2 The Analysis of Cases Recorded During the 3 Community Waves |
The case fatality rate during the entire period 01.01.2021–31.03.2022 was 0.085% [95% CI 0.02–0.31], more prominent 0.43% [95% CI 0.12–1.57] during wave 3 and 0% in waves 4 and 5. Two medical staff members, one medium education medical staff and one auxiliary staff member died; one was not vaccinated, and the other was infected after the first vaccine dose.
The univariate analysis of variables when comparing the non-vaccinated versus completely vaccinated subsamples at the time of infection shows 19 statistically significant differences. Of these, the residence in the metropolitan area of the county capital city and the medical profession, regardless of the professional degree, were identified as independent protection factors against non-vaccination, while the detection of infection by screening as well as the presence of anosmia and nausea reached values that plea for the non-vaccinated status (Table 3).
 |
Table 3 The Analysis of Predictor Factors for the Vaccine Status of the Personnel |
The logistic regression identified the predictive factors for reinfection – the non-vaccinated status, incomplete vaccination with 1 dose, but also the complete vaccination status (as it was initially defined – 1 dose for the J&J vaccine/2 doses for the other manufactures). Also, the presence of odynophagia fulfilled the condition of a predictive factor for reinfection. On the other hand, a high number of vaccine doses, as well as vaccination with the mRNA-based product of Pfizer-BioNTech were identified as independent protection factors against reinfection, as did the presence of myalgia, anosmia, and the detection of the case by screening (Table 4).
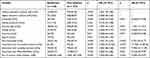 |
Table 4 The Analysis of Predictor Factors for Reinfection |
Discussion
Contact with the emergent pathogen while providing healthcare or by cohabitation in the nosocomial environment generated a COVID-19 infection risk three times higher in medical staff members as compared to the general population, at the onset of the pandemic.23
In this study, during the surveyed period, the incidence of COVID-19 infections reported in medical staff directly and strongly correlates with community incidence, a fact that supports the importance of community transmission of SARS-COV-2 among medical staff members, in addition to nosocomial transmission. Family contacts, especially during periods of intense community circulation, as well as the existence of asymptomatic carriers, facilitate transmission within the community and nosocomial environments, aspects also revealed in the studies conducted by Kluytmans or Sikkema.24,25
The highest correlations were found for auxiliary and environmental medical staff, the lowest for non-medical, administrative staff, which also argues for the risk of close/prolonged contact with patients, especially in the case of deficiencies in the application of standard/faculty precautions and the wearing of protective equipment, similar to the findings of a French study from 2022.26
Despite the average monthly incidence, which is highest among the auxiliary medical staff (explained by the lower total number of employees versus doctors or nurses), the distribution of COVID-19 cases registers the highest percentage 41.46%[95% CI 39.49–43.47], in the medium education medical staff. This trend of higher infection rates among nurses is also found in a meta-analysis published in January 2021, where the percentage of infections among medium education medical staff was 48% [95% IC 41–56].27
An exception was in emergency medicine, where auxiliary staff were significantly more affected compared to other categories (a finding also present in other studies), which can be explained by closer and more frequent contact with patients, lower knowledge or lower adherence to preventive measures, or a higher percentage of unvaccinated personnel.28
Of the entire sample of 3261 cases, 530 were not vaccinated (22.45%[95% CI 20.81–24.18]), with a minimum percent among higher education medical staff 6.83%[95% CI 5.11–9.07], followed by the administrative personnel 22.73%[95% CI 15.89–30.83], medium education medical staff 28.09% [95% CI 25.36–30.99] and a maximum in the auxiliary personnel members 29.35%[95% CI 25.91–33.06], while in the community of the same geographic area, the vaccine coverage was 50.08%.29 Scientific studies found that higher education medical personnel members accept vaccination more easily although the entire staff is preoccupied with vaccine safety, efficacy and potential side effects.30 Other Romanian studies identified a higher vaccine acceptance rate among physicians, together with the choice of mRNA vaccines over vector-based formulas.31
Before the infection, about 1 in 2 doctors (58.10%), and only 1 in 3 auxiliary and administrative staff (35.65% and 36.36% respectively) were fully vaccinated. By the end of the period under surveillance, 44.67% of doctors had also had the booster dose, while only 12.90% in E3, 21.04% in E2 and 27.27% in E4 had taken the 3rd dose, which influenced the risk of infection in 2022, in full pandemic wave with the omicron variant.
The circulation of SARS-COV-2 variants during the various pandemic waves generated the variation presented in Table 2. While wave 3 affected mainly older age groups of medical staff, with manifest comorbidities and more evident fatality (at the beginning of vaccination), wave 5 affected younger age groups of higher education medical staff, in medical specialities with better vaccine coverage. The percentage of asymptomatic subjects was higher during wave 3, as was the number of subjects detected by screening tests performed when returning to work from vacation, while the dominant variant (according to National Institute of Public Health data) Alpha (B.1.1.7) and Delta (B.1.617.2) more frequently caused anosmia and ageusia.18 Wave 4 mainly affected the unvaccinated staff members, categories with immunization hesitancy, and clinically it was characterized by rhinorrhoea, myalgia, and cough. The Omicron variant (B.1.1.529) caused dysphagia and an increase in the number of reinfections, while only about 1/3 (35.05%) of infected staff between January and March 2022 were vaccinated, including with the booster dose. The importance of screening asymptomatic medical staff was noted since the beginning of the pandemic in studies conducted by Rivett L and later by Bergwerk M.32,33
When comparing the non-vaccinated and fully vaccinated subsamples, before infection, the identified predictor factors for the vaccinated status were residence in the metropolitan area and being a physician. The high socio-economic level of the population in the metropolitan area as well, as the fact that this area includes the locality with the highest vaccine coverage in Romania (63.81% in February 2022) explains the result of logistic regression. The advanced medical studies of physicians involve a deeper knowledge of the risks generated by the SARS-COV-2 infection, the active immunization by vaccination, the research results in the field of novel vaccines, and as a consequence, less adherence to conspiracy theories and hyperbolisation of post-vaccine side effects.
On the other hand, in screening-based case identification, the presence of anosmia and nausea met the statistical criteria as independent factors for non-vaccination. The significant percentage of non-vaccinated persons during the circulation of the Alpha variant (when the medical personnel was undergoing vaccination), the high percentage of asymptomatic infections during wave 3 and the more frequent association of anosmia/digestive symptoms with the Alpha and Delta variants versus Omicron determined the association between non-vaccination and these items.34,35
The logistic regression performed to identify predictive factors for reinfection retained 4 variables – first incomplete vaccination, with a single dose (HR 17.70[5.10–68.54], p < 0.001), then vaccination with 2 doses/1 dose for the J&J vaccine (HR 7.99[5.33–11.99], p < 0.001), followed by the non-vaccinated status (HR 2.75[1.59–4.77], p < 0.001), but also the presence of odynophagia (HR 1.43[1.13–1.81], p = 0.003). In interpreting this result, it should be taken into account that 86.45% of the cases of reinfections analysed in this study occurred in the year 2022, when the majority of staff were actively immunised. In addition, the Omicron variant reduced the efficiency of anti-SARS-COV-2 vaccines, the 5th wave being the wave of infections among vaccinated medical staff. Other studies also reveal a lower vaccine efficacy of anti-SARS-COV-2 vaccines against the Omicron variant, with protection against severe clinical forms but with reduced protection against infection, by decreasing neutralizing antibody levels.36–39
Nevertheless, the vaccination with Comirnaty (Pfizer-BioNTech), as well as high number of vaccine doses, with the presence of the booster dose, recorded values of independent protection factors against reinfection (HR 0.61[0.38–0.99, p = 0.046/ HR 0.49[0.37–0.47], p < 0.001), although these booster doses cause increased antibody production, without long-lasting persistence.40
Limitations of the study: The surveillance of COVID-19 infection did not include the first pandemic year 2020, when the medical personnel did not have access to the advantages of active immunization as the national system of online surveillance was instituted at the end of October 2020. No data regarding the clinical form, hospitalization, or long-COVID status were available for the study, and cases were not investigated by sequencing (to confirm the type of variant), also, the level of anti-spike/anti-nucleocapsid antibodies was not monitored (to reveal the post-vaccinal or natural post-disease protection). The recorded comorbidities were at very low levels of fact which supports under-reporting.
Conclusion
The incidence of the infection with the SARS-COV-2 in medical personnel was strongly correlated with the community pandemic trend, supporting the intricate community and nosocomial transmission. The predominance of medium and auxiliary medical staff requires intensified training on preventive behaviour and focus of the prevention/control strategy on all professional groups interacting with patients (so including caretakers, stretcher bearers, ambulance workers, receptionists or physiotherapists, psychologists, etc.).
Although vaccination coverage in all the categories of medical personnel studied (at the end of March 2022) was over 70%, higher than the community coverage (ranked penultimate in the European Union), the study highlights the low adherence of medical personnel (especially medium and auxiliary staff) to vaccination schemes that include repeat doses, which requires increased educational efforts on active immunization, but also the need to administer these booster doses to maintain and improve protection against the circulation of new variants of coronavirus.
Abbreviations
COVID-19, coronavirus disease 2019; EU, European Union; IQR, interquartile range; mRNA, messenger Ribonucleic Acid; RT- PCR, Reverse transcription polymerase chain reaction; SARS-CoV-2, novel severe acute respiratory syndrome coronavirus; USA, The United States of America.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Ethics Approval
The study was conducted according to the guidelines of the Declaration of Helsinki, EC Directive 86/609/EEC for animal experiments, and Uniform Requirements for manuscripts submitted to Biomedical journals. The study protocol was approved by the Public Health Authority of Timis County no. 29,517/15.11.2021.
Consent for Publication
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
The authors would like to acknowledge Dr. Dana Brehar Cioflec for her technical support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no external funding.
Disclosure
The authors report no conflicts of in this work.
References
1. Koh D. Occupational risks for COVID-19 infection. Occup Med. 2020;70(1):3–5. doi:10.1093/occmed/kqaa036
2. Moen BE. COVID-19 should be recognized as an occupational disease worldwide. Occup Med. 2020;70(5):299. doi:10.1093/occmed/kqaa086
3. European Union. Possibility of recognizing COVID-19 as being of occupational origin at national level in EU and EFTA countries. Luxembourg: Publications Office of the European Union; 2021. Available from: https://ec.europa.eu/eurostat/documents/7870049/13464590/KS-FT-21-005-EN-N.pdf/d960b3ee-7308-4fe7-125c-f852dd02a7c7?t=1632742856466.
4. Romanian Government. DECISION No. 259/2022 of 23 February 2022 on the amendment and completion of the methodological norms for the application of the provisions of the law on safety and health at work No. 319/2006, approved by Government Decision No. 1.425/2006. Available from: http://www.mmuncii.ro/j33/images/Documente/Legislatie/HG_259_2022.pdf.
5. Billock MR, Groenewold RM, Sweeney Haring M, et al. Reported exposure trends among healthcare personnel COVID-19 cases, USA, March 2020–March 2021. Am J Infect Control. 2022;50(5):548–554. doi:10.1016/j.ajic.2022.01.007
6. Olalla J, Correa MA, Martín-Escalante M D, et al. Search for asymptomatic carriers of SARS-CoV-2 in healthcare workers during the pandemic: a Spanish experience. QJM. 2020;113(11):794–798. doi:10.1093/qjmed/hcaa238
7. Breazzano MP, Shen J, Abdelhakim AH, et al. New York City COVID-19 resident physician exposure during exponential phase of pandemic. J Clin Invest. 2020;130(9):4726–4733. doi:10.1172/JCI139587
8. Ferland L, Carvalho C, Gomes Dias J, et al. Risk of hospitalization and death for healthcare workers with COVID-19 in nine European countries, January 2020–January 2021. J Hosp Infect. 2022;119:170–174. doi:10.1016/j.jhin.2021.10.015
9. Tabueña NO, Fuertes GR, Del Val García JL, et al. Characteristics and factors associated with the severity of COVID-19 in primary care professionals followed in a basic prevention unit. Rev Esp Salud Publica. 2021;95:e202110173.
10. Canadian Institute for Health Information. COVID-19 cases and deaths in health care workers in Canada. Available from: https://www.cihi.ca/en/covid-19-cases-and-deaths-in-health-care-workers-in-canada.
11. World Health Organization. Health and care worker deaths during COVID-19. Available from: https://www.who.int/news/item/20-10-2021-health-and-care-worker-deaths-during-covid-19.
12. World Health Organization. The impact of COVID-19 on health and care workers: a closer look at deaths. Geneva, 2021:1. Available from: https://apps.who.int/iris/bitstream/handle/10665/345300/WHO-HWF-WorkingPaper-2021.1-eng.pdf.
13. Dascalu S, Geambasu O, Raiu CV, et al. COVID-19 in Romania: what went wrong? F Pub H. 2021;9:813941. doi:10.3389/fpubh.2021.813941
14. Romanian Government. Vaccination situation in Romania. Available from: https://vaccinare-covid.gov.ro/situatia-vaccinarii-in-romania/.
15. National Institute of Public Health. COVID-19 – map of the number of people in isolation, at the national level. Available from: https://instnsp.maps.arcgis.com/apps/dashboards/5eced796595b4ee585bcdba03e30c127.
16. World Health Organization. Romania Situation. Available from: https://covid19.who.int/region/euro/country/ro.
17. Herdea V, Duduciuc A, Ghionaru R, Comnea L, Păduraru L, Diaconescu S. Assessment of the risk of infection among Romanian physicians at the outbreak of the SARS CoV-2 pandemic. Eur J Gen Pract. 2021;27(1):235–240. doi:10.1080/13814788.2021.1963434
18. National Institute of Public Health. Analysis of the evolution of communicable diseases under surveillance. Report for 2020 and 2021. București; 2022:2. Available from: https://insp.gov.ro/download/analiza-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2020-2021/.
19. National Institute of Public Health. COVID-19 surveillance methodology, update 04/01/2021. Available from: https://www.cnscbt.ro/index.php/metodologii/infectia-2019-cu-ncov/2199-metodologia-de-supraveghere-a-covid-19-actualizare-04-01-2021-1.
20. National Institute of Public Health. COVID-19 surveillance methodology, update 11/01/2022. Available from: https://www.cnscbt.ro/index.php/metodologii/infectia-2019-cu-ncov/2928-metodologia-de-supraveghere-a-covid-19-actualizare-11-01-2022-1.
21. National Institute of Public Health. COVID-19 surveillance methodology, update 08/02/2022. Available from: https://www.cnscbt.ro/index.php/metodologii/infectia-2019-cu-ncov/3006-metodologia-de-supraveghere-a-covid-19-actualizare-08-02-2022-1.
22. Public Health Authority of Timis County. Covid-19 incidence by localities. Available from: https://www.dsptimis.ro/incidenta-pe-localitati.
23. Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9):e475–e483. doi:10.1016/S2468-2667(20)30164-X
24. Kluytmans-van den Berghn MFQ, Buiting AGM, Pas SD, et al. SARS-CoV-2 infection in 86 healthcare workers in two Dutch hospitals in March 2020. JAMA Netw Open. 2020;3(5):e209673. doi:10.1001/jamanetworkopen.2020.9673
25. Sikkema RS, Pas SD, Nieuwenhuijse DF, et al. COVID-19 in health-care workers in three hospitals in the south of the Netherlands: a cross-sectional study, 2020. Lancet Infect Dis. 2020;20(11):1273–1280. doi:10.1016/S1473-3099(20)30527-2
26. Paris C, Tadie E, Heslan C, et al. Risk factors for SARS-CoV-2 infection among health care workers. Am J Infect Control. 2022;50(4):375–382. doi:10.1016/j.ajic.2021.11.001
27. Gómez-Ochoa SA, Franco OH, Rojas LZ, et al. COVID-19 in health-care workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161–175. doi:10.1093/aje/kwaa191
28. Mutambudzi M, Niedzwiedz C, Macdonald EB, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120075 UK Biobank participants. Occup Environ Med. 2021;78(5):307–314. doi:10.1136/oemed-2020-106731
29. Public Health Authority of Timis County. Vaccination coverage. Available from: https://www.dsptimis.ro/data_files/content/prima-pagina/files/acoperire-vaccinala-20-01-2022.pdf.
30. Biswas N, Mustapha T, Khubchandani J, Price JH. The nature and extent of COVID-19 vaccination hesitancy in healthcare workers. J Community Health. 2021;46(6):1244–1251. doi:10.1007/s10900-021-00984-3
31. Dima A, Jurcut C, Balaban DV, et al. Physicians’ experience with COVID-19 vaccination: a survey study. Health Care. 2021;9(12):1746. doi:10.3390/healthcare9121746
32. Rivett L, Sridhar S, Sparkes D, et al. Screening of healthcare workers for SARS-CoV-2 highlights the role of asymptomatic carriage in COVID-19 transmission. eLife. 2020;9:e58728. doi:10.7554/eLife.58728
33. Bergwerk M, Gonen T, Lustig Y, et al. Covid-19 breakthrough infections in vaccinated health care workers. N Engl J Med. 2021;385(16):1474–1484. doi:10.1056/NEJMoa2109072
34. Pouwels KB, Pritchard E, Matthews PC, et al. Effect of delta variant on viral burden and vaccine effectiveness against new SARS-CoV-2 infections in the UK. Nat Med. 2021;27(12):2127–2135. doi:10.1038/s41591-021-01548-7
35. Boscolo-Rizzo P, Tirelli G, Meloni P, et al. COVID-19-related smell and taste impairment with widespread diffusion of SARS-CoV-2 Omicron variant. Int Forum Allergy Rhinol. 2022;2(10):1273–1281. doi:10.1002/alr.22995
36. Reeves KD, Polk CM, Cox LA, et al. Severe acute respiratory coronavirus virus 2 (SARS-CoV-2) infections occurring in healthcare workers after booster vaccination: a comparison of delta versus omicron variants. ASHE. 2022;2(1):e143. doi:10.1017/ash.2022.239
37. Woodbridge Y, Amit S, Huppert A, Kopelman NM. Viral load dynamics of SARS-CoV-2 Delta and Omicron variants following multiple vaccine doses and previous infection. Nat Commun. 2022;13(1):6706. doi:10.1038/s41467-022-33096-0
38. Kahn F, Bonander C, Moghaddassi M, et al. Risk of severe COVID-19 from the Delta and Omicron variants in relation to vaccination status, sex, age and comorbidities – surveillance results from southern Sweden, July 2021 to January 2022. Euro Surveill. 2022;27(9):2200121. doi:10.2807/1560-7917.ES.2022.27.9.2200121
39. Pople D, Monk EJM, Evans S, et al. Burden of SARS-CoV-2 infection in healthcare workers during second wave in England and impact of vaccines: prospective multicentre cohort study (SIREN) and mathematical mode. BMJ. 2022;378:e070379. doi:10.1136/bmj-2022-070379
40. Goldblatt D, Alter G, Crotty S, Plotkin SA. Correlates of protection against SARS-CoV-2 infection and COVID-19 disease. Immunol Rev. 2022;310(1):1–21. doi:10.1111/imr.13091
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
