Back to Journals » International Journal of General Medicine » Volume 16
Health-Related Quality of Life and Influencing Factors in Coronary Heart Disease Based on the Scale QLICD-CHD (V2.0): A Cross-Sectional Study
Authors Rao S, Xu C, Wan C , Huang Z, Huang X, Chen S
Received 12 July 2023
Accepted for publication 31 October 2023
Published 6 November 2023 Volume 2023:16 Pages 5119—5129
DOI https://doi.org/10.2147/IJGM.S430169
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Shuying Rao,1 Chuanzhi Xu,2 Chonghua Wan,1 Zhiwen Huang,3 Xingping Huang,4 Shu Chen1
1Research Center for Quality of Life and Applied Psychology, School of Humanities and Management, Guangdong Medical University, Dongguan, People’s Republic of China; 2Department of Statistics, School of Public Health, Kunming Medical University, Kunming, People’s Republic of China; 3Cardiovascular Department, the Affiliated Hospital of Guangdong Medical University, Zhanjiang, People’s Republic of China; 4Department of Research and Teaching, Dongguan Eighth’ Hospital, Dongguan, People’s Republic of China
Correspondence: Chonghua Wan, Tel/Fax +86-0769-22896255, Email [email protected]
Purpose: Coronary heart disease (CHD) is difficult to cure, so more attention should be paid to improving patients’ health-related quality of life (HRQoL). This paper focuses on identifying factors that affect HRQoL.
Patients and Methods: Overall, 189 in-patients with coronary heart disease were investigated at the Affiliated Hospital of Guangdong Medical University between 2015 and 2016. The scale Quality of Life Instruments for Chronic Diseases-Coronary heart disease (QLICD-CHD V2.0) was used to evaluate HRQoL and collect demographic information. Medical records were applied to collect patients’ clinical indicators. A simple correlation analysis, Student’s t-test, and a one-way analysis of variance were first performed to filter factors that might associate with HRQoL, and multiple linear regression was applied to finally identify related factors.
Results: Findings from multiple linear regression showed that the total score was related to family economy, treatment, indirect bilirubin, and albumin with regression coefficient B=5.209, − 6.615, 0.378, and 0.548, respectively. The physical functions were related to treatment, albumin, globular proteins, chloride, and red blood cell count with B=− 9.031, 1.000, 0.612, 1.320, and 5.161, respectively. The psychological function was in association with family economy, clinical course, serum phosphorus, and percentage of lymphocyte population with B=7.487, 6.411, − 16.458, and 0.090, respectively. The social function was associated with family economy, blood urea nitrogen, serum creatinine, and platelet distribution width with B=7.391, 1.331, − 0.060, and − 0.929, respectively. The special module was in association with treatment, indirect bilirubin, and serum calcium with B=− 7.791, 0.414, and 23.017, respectively.
Conclusion: Clinical indicators including albumin, globular proteins, chloride, red blood cell count, serum phosphorus, percentage of lymphocyte population, blood urea nitrogen, serum creatinine, platelet distribution width, indirect bilirubin, and serum calcium, as well as socio-demographic factors including the family economy, clinical course, and treatment, may affect coronary heart disease patients’ HRQoL.
Keywords: quality of life, coronary heart disease, socio-demographic factors, clinical indicators, scale
Introduction
Coronary heart disease (CHD) has high morbidity and mortality, leading to low health-related quality of life (HRQoL).1,2 It can narrow blood vessel lumens, decrease blood circulations, and cause cardiac ischemia,3,4 posing a great risk to human health. Unfortunately, considerable numbers of people suffered from CHD: 126.5 million patients globally in 20175 and 17.06 million in China in 2018,6 among which more than 0.9 million needed interventional treatment.7 Doctors are used to focus on determining patients’ health conditions through electrocardiograms and coronary arteriography, while patients care more about eliminating discomfort and pain, because long-lasting and incurable CHD requires lifetime regular medication and monitoring visits, probably resulting in workability loss, early retirement,8 and even mental health issues. Therefore, both life expectancy and quality of life are essential for patients.
HRQoL refers to patients’ subjective evaluation of their physical, psychological, and social health, and overall well-being level.9 Due to the rise of the “biology-psychology-social medicine” model, people pay increasing attention to it.10 Recently, researchers worldwide have veered from the treatment of CHD to enhancing patients’ HRQoL. They utilized it as an indicator to assess the progress of treatment.11 Most of the measurements of HRQoL are through scales. However, general scales may fail to precisely reflect CHD patients’ subjective feelings. Typical general scales, such as the European Quality of Life Five Dimension Five level scale (EQ-5D-5L), include self-care, pain/discomfort, usual activities, mobility, and anxiety/depression. It reflects patients’ HRQoL from different domains but does not consider the characteristics and clinical manifestations of CHD. Mei’s (2021) study showed that less than 8% of patients had problems with self-care.12 However, if more items about chest pain and chest distress that seriously bother CHD patients’ normal life are added to the scale, patients can be especially evaluated and conclusions will be more accurate. Similarly, the 36-Item Short-Form Health Survey questionnaire (SF-36) focuses on overall health status without considering the effects of specific disorders.13 In this study, we use the Quality of Life Instruments for Chronic Diseases (QLICD-CHD V2.0), a modular approach with a general module (QLICD-GM) and a specific one so common psychometric properties and distinctive disease features can be captured.14
In addition, prior work has documented that CHD patients from different European countries reported different major problems on the EQ-5D-5L scale.15 As a result, we assume that cultural variations have a significant impact on HRQoL. However, in China, specific measurement tools are demanded for the HRQoL of patients with CHD. Researchers in the United States have developed the Seattle Angina Questionnaire (SAQ), which includes physiological constraints, treatment satisfaction, disease perception, angina stability, and angina frequency, among which the stability and frequency of pain are important indicators of patients’ physical condition.16 Similarly, the Kansas City Cardiomyopathy Questionnaire (KCCQ) is a disease-specific health status measure for patients with heart disease that can discover minor clinical changes.17 However, in the process of developing and evaluating the scales above, all the patients selected were Americans. So, due to the lack of a specific Chinese social and cultural environment, these scales may be unsuitable to be used in China. Chinese people, in particular, value family. In traditional Chinese culture, a family is a social group with a clear division of labor and performing its duties. Therefore, family ties and the ability to fulfill family responsibilities will significantly impact HRQoL.18 Based on the review of the above-mentioned scales, we realized that EQ-5D-5L and SAQ lack items about family relationships. Although SF-36 and KCCQ measure the intimacy between family members, they fail to test whether patients can continue to take on corresponding family roles such as parents. In this regard, we used QLICD-CHD V2.0, which satisfies the criteria for accurate measurement of the HRQoL of CHD patients in China with important items such as family responsibility.
Some scholars have found socio-demographic characteristics that affect HRQoL but the relationships between clinical indicators and HRQoL are not well understood. Jiang19 (2017) used QLICD-CHD V2.0 to conclude that age, gender, and medical treatment can affect patients’ HRQoL, which is agreed upon by different scholars.20,21 Slepecky (2017) found that patients with depression symptoms reported lower QOL,22 and Matsuda (2017) suggested that sleep quality played an important role in HRQOL.23 Apart from socio-demographic factors, we assumed that certain clinical indicators can reflect patients’ HRQoL. Fu’s (2022)24 study showed that patients with a lower level of D-dimer felt lower HRQoL. Erdem (2016)25 observed the correlation between the severity of coronary artery disease and high red cell distribution width values. These studies indicated that biomarkers may predict CHD patients’ HRQoL, but there are few studies on its mechanism at home and abroad. We believe that through the detection of objective clinical indicators in blood routine, blood biochemistry, urine routine, and blood gas analysis, we can make up for the shortcomings of the current HRQoL research. Therefore, we intend to use QLICD-CHD (V2.0) to further explore the related socio-demographic factors and possible objective clinical indicators that affect HRQoL and provide a basis for the formulation of intervention strategies.
Methods
Study Design and Setting
A cross-sectional method is used for in-patients with CHD at the Affiliated Hospital of Guangdong Medical University from January 2015 to December 2016. It is a tertiary first-class hospital located in Zhanjiang, China.
Participants
We selected patients with CHD from the Affiliated Hospital of Guangdong Medical University as subjects.
Inclusion criteria: (1) patients diagnosed with CHD; (2) patients with necessary comprehension, writing, and reading skills.
Exclusion criteria: (1) patients who were illiterate; (2) patients with other serious diseases; (3) patients who refused to cooperate.
All patients signed an informed agreement before taking part in the trial.
Instruments and Variables
QLICD-CHD (V2.0) is about CHD in Quality of Life Instruments for Chronic Diseases (QLICD). The internal consistency α of the whole scale is higher than 0.70. The test–retest reliability coefficient in all fields is higher than 0.80, and its standardized response mean (SRM) is higher than 0.32. The scale is small, and the patient can finish it in less than 15 min. Therefore, it is a reliable indicator that can correctly reflect the actual feelings of patients and is feasible in clinical settings.26 The specific module involves 14 items and QLICD-GM contains three domains, including 9 items in physiological function, 11 items in psychological function, and 8 items in social function, with a total of 28 items. All 42 indexes are evaluated by a 5-point Likert scale. Positive items are scored in the order of 1 to 5, while negative items are reversely rated. The raw score (RS) is generated by the sum of the scores for each field. RS is transformed into Standard Score (SS) using the formula: SS=(RS-Min)×100/R, so that scores in each dimension can be compared (MIN, R represents the minimum score, and the score range). The scores range from 0 to 100. A greater HRQoL is indicated by a higher score.
Also, a self-made general information questionnaire about the basic characteristics of patients (eg, age and nation) and socio-economic characteristics (eg, occupation and medical insurance) data, and clinical status (eg, clinical course and treatment) is used.
Survey Methods
We invited the patients to finish the QLICD-CHD independently on the day of hospitalization and checked the questionnaires immediately to guarantee the integrality. Then, we compared the personal information on the scale with the medical record system to ensure it was correct and then input the data. Sixty-one biochemical indexes, such as serum calcium, total bilirubin, albumin, and so on, were collected from the hospital medical record information systems, including biochemical blood tests, liver function tests, routine urine tests, blood routine, and so on.
Statistical Analysis
The data were statistically analyzed using SPSS software. First, the statistical description was used to analyse demographic elements. Second, univariate analysis of the relations between the QLICD-CHD (V2.0) domains and socio-demographic elements was tested by one-way analysis of variance (ANOVA), followed by a two-way comparison using the LSD-t test. T-test was carried out for dichotomous variables. The correlations between QLICD-CHD (V2.0) scores and clinical parameters were assessed by the Pearson correlation test. Finally, the initial screening results of the above two stages were taken as independent variables, and multiple-regression analysis (Stepwise selection) was carried out. Physical, psychological, and social functions, the specific module, and the total score of the scale were considered as dependent variables. The selection criterion (p-in) was 0.05, and the elimination criterion (p-out) was 0.10. Before multiple linear regressions, the categorical variables were recoded. Marriage was quantified as married 1, single 2; the family economy was quantified as poor 1, moderate 2, good 3; the type was quantified as angina 1, myocardial infarction 2.
Results
Sample Characteristics
The demographic features of the selected patients are listed in Table 1. The age of patients ranged from 22 to 88. The average age was 66.90±11.40. Most patients were from Han ethic group. Most of them were men (62.4%) and married (84.7%), with moderate economic conditions (61.9%). Less than half (45.0%) have attended secondary school.
 |
Table 1 Socio-Demographic Characteristics of the Sample (n=189) |
HRQoL Scores of Patients with CHD
Table 2 shows the average scores of the patients’ HRQoL using QLICD-CHD (V2.0). Social function (SOD) with 73.67±15.57 (95% CI71.44–75.90) was the highest, followed by physical function (PHD) (63.84±16.23) (95% CI61.59–66.03) and psychological function (PSD) (63.07±17.22) (95% CI60.51–65.31); the figure was smallest in specific module (SPD) (57.63±14.73) (95% CI55.56–59.10), and the total score averaged 63.44±12.27 (95% CI61.71–65.08).
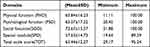 |
Table 2 The Standardized Scores of Quality of Life in CHD Patients by QLICD-CHD (V2.0) |
HRQoL Scores Comparisons by Univariate Analysis
The results of the comparative analysis of the different variables and dimensions are listed in Table 3. There were significant differences in PHD, SPD, and TOT among treatment groups and clinical types (P<0.05). Patients with interventional therapy and myocardial infarction had more severe signs and symptoms and worse cardiac function than those who have undergone thrombolytic therapy and angina pectoris. The SOD scores were inconsistent between education levels (P<0.05). Highly educated patients have a higher social function related to their mastery of health knowledge. The SOD, PSD, and TOT were statistically different between economic status (P<0.05) with better-off patients scoring higher in a two-way comparison, probably because high income and better economic conditions can guarantee lifelong treatment and improve patients’ emotional states. The PHD, PSD, and TOT exhibited differences between groups of clinical course (P<0.05). Compared to the patients during paracmasia, the patients experiencing acute attacks report higher HRQoL scores. Other socio-demographic factors were not statistically different and did not affect the scores on the dimensions of HRQoL (P>0.05). In conclusion, patients with angina type, thrombolytic therapy, acute attacks, high education, and high income had a relatively better HRQoL.
 |
Table 3 Univariate Analysis of Quality of Life in Patients with Coronary Artery Disease |
Simple Correlation Analysis
A simple correlation analysis was performed between clinical objective indicators and HRQoL scores (see Table 4). We found that there was a certain relationship between these 18 clinical indexes and HRQoL scores. Patients’ scores in physical function rise (r=0.146~0.334, P<0.05) with the increase in the total protein, albumin, globular proteins, prealbumin, chloride, serum calcium, percentage of lymphocyte population, red blood cell count, haemoglobin, and hematocrit, while dropped (r=−0.223~-0.184, P<0.05) with the increase in alanine aminotransferase, aspartate transaminase, blood urea nitrogen, and serum creatinine. A significant negative relationship exists between serum phosphorus and psychological function (r=−0.188, P<0.05). Platelet distribution width was negatively associated with the social function (r=−0.159, P<0.05). Both higher total bilirubin and indirect bilirubin contributed to higher special module scores (r=0.171, 0.193, P<0.05). The total scores showed a statistically significant positive correlation with albumin (r=0.169, P<0.05).
 |
Table 4 Simple Correlation Analysis Between Scores of Quality of Life and Clinical Indicators (r) |
Multiple Linear Regression Analysis
We took the scores of the physiological function, psychological function, specific module, and the total scale as dependent variables, 23 indexes selected by univariate analysis and simple correlation analysis as independent variables, and used the multiple linear regression method to evaluate each index comprehensively. Classification factors were re-encoded before the multiple linear regression (see Table 5). Table 6 lists the outcomes of the multiple linear regression. The variables of the physical function included in the model were treatment (B=−9.031, t=−2.784, P=0.006), albumin (B=1.000, t=2.948, P=0.004), globular proteins (B=0.612, t=2.088, P=0.038), chloride (B=1.320, t=3.990, P<0.001), and red blood cell count (B=5.161, t=2.506, P=0.013). The determination coefficient R2 was 0.239 (F=10.197, P<0.001); The psychological function included the following contents: family economy (B=7.487, t=3.433, P=0.001), clinical course (B==6.411, t=2.198, P=0.029), serum phosphorus (B=−16.458, t=−2.614, P=0.010), and percentage of the lymphocyte population (B=0.090, t=2.063, P=0.041) (F=6.678, R2=0.141, P<0.001). The variables in the social function model were as follows: family economy (B=7.391, t=3.798, P<0.001), blood urea nitrogen (B=1.331, t=2.595, P=0.010), serum creatinine (B=−0.060, t=−2.284, P=0.024), and platelet distribution width (B=−0.929, t=−2.288, P=0.023) (F=6.163, R2=0.187, P<0.001). The variables included in the model of special modules were treatment (B=−7.791, t=−2.462, P=0.015), indirect bilirubin (B=0.414, t=2.019, P=0.045), and serum calcium (B=23.017, t=2.205, P=0.029) (F=4.236, R2=0.116, P=0.001). The variables included in the total scale score model were family economy (B=5.209, t=2.253, P=0.001), treatment (B=−6.615, t=−2.583, P=0.011), indirect bilirubin (B=0.378, t=2.292, P=0.026) and albumin (B=0.548, t=2.292, P=0.023) (F=5.504, R2=0.170, P<0.001). Although R2 in these models were slightly low, these results suggest that dynamically monitoring clinical indicators such as albumin, globular proteins, chloride, and red blood cell count levels may provide more sensitive information for further observations of CHD patients’ clinical states.
 |
Table 5 The Variable Assignment of Multiple Linear Regression |
 |
Table 6 Factors Influencing Quality of Life Scores in CHD Screened by Multiple Linear Regression Analysis |
Discussion
The World Health Organization reported that 7.4 million people died of CHD in 2015.27 CHD is incurable and patients’ HRQoL is lower than healthy people28, so it is necessary to target improving it, which is an important indicator to reflect patients’ subjective well-being in the treatment progress.29 Previous studies have illustrated some factors like occupatioeported that compared with retired patients those who are employed shon and marriage may affect CHD patients’ HRQoL, Dou (2022),21 for example highele, rwer HRQoL. However, these studies have either not used disease-specific instruments or have not focused on clinical indicators. In this study, we optimised the scale QLICD-CHD (V2.0) whose general module can compare HRQoL for different chronic illnesses and the specific module reflects specific symptoms. Among all the scores of modules, SOD ranked the highest which was aligned with Tang’s study.30 Possibly because 84.7% of patients were married, they were greatly cared for in life and gained sufficient social support. PHD ranked second followed by PSD and SPD. Compared with hypertension patients measured by QLICD-HY,31 CHD patients’ PSD averaged lower possibly because of the weak heart’s inability to provide adequate blood to the brain, which leads to neurological symptoms and mental illnesses.32 So CHD patients suffer from emotional disturbance even depression with a higher likelihood.33,34 The specific module scored the lowest. Probably because patients have characteristic symptoms including shortness of breath and chest discomfort, and they are always worried about chest pain attacks leading to increased insecurity and stress. Unfortunately, chronic stress raises the risk of CHD, which also weakens psychological function.35
Results from the multiple linear regression analysis further confirmed that among the socio-demographic factors family economy correlated significantly with scores in PSD and SOD, which was in line with Zhang’s research.36 Patients with higher economic status tend to have better HRQoL because they are more accessible to emotional and material support from the surrounding environment, which can release physical stress and benefit their health physically and mentally.37 Social support exerted a promoting effect on HRQoL in patients with coronary heart disease,38 but those who stayed on breadline received a low level of social support.39
In terms of clinical indicators, chlorine is one of the vital influencers of PHD. Chlorine is the most prevalent anion in the extracellular fluid.40 It has various vital physiological functions, such as acid-base homeostasis, regulation of glomerular filtration rate, gastrointestinal function, and so on.41 Meanwhile, low chlorine level gives rise to hypochloremia, which can cause nausea and vomiting. These affect patients’ appetite and sleep, thus affecting the PHD score. Therefore, changes in chlorine should also be monitored throughout therapeutic therapy.
The percentage of the lymphocyte population was one of the vital influencers in PSD. A study suggested that when coronary artery lesions patients’ lymphocyte counts are lower, their immunity reduces, and they are susceptible to viral or bacterial infections.42,43 So patients subjectively consider that the symptoms are aggravated and feel anxiety.
Also, current study discovered that CHD patients with higher albumin levels achieve higher scores in TOT, which is consistent with previous studies.44,45 Albumin has been proven to be a nutritional marker,46 and good nutrition provides a fundamental building block for the prevention and treatment of CHD.47 However, low albumin will lead to hypoalbuminemia, which may be a risk factor accelerating CHD48 so albumin affects patients’ life quality scores.
These findings extend those of Fu’s (2022)24 and Erdem (2016),25 confirming more biomarkers related to HRQoL. Our results provide compelling evidence for the associations between objective clinical indicators and CHD patients’ subjective well-being. Measurements of blood routine, blood biochemistry, urine routine, and blood gas analysis are economical and easy to reach. As treatment progresses, doctors can closely monitor objective clinical indicators such as chloride and albumin discovered in this study and adjust treatment strategies.
We admit that this paper has some limitations. First, it should, however, be noted that in a cross-sectional method, it is difficult to prove that one variable causes another. To corroborate the causal correlations suggested by the findings, longitudinal or interventional studies would be required. Second, because the participants were selected in the same hospital, the results might not apply to all patients and more hospitals in China should be implemented in the future study. Third, only 61 clinical objective indicators were included in this study and the coefficient of determination R2 for each model was not high enough, suggesting that our selection of clinical indicators for measurement has certain limitations, so more clinical variables should be taken into account. Despite these inadequacies, this study addresses the gap that the impact of clinical indicators on HRQoL received little attention in research before and finds that clinical data such as albumin, globular proteins, and chloride are independent factors of HRQoL. They can be detected by a routine blood examination, which is inexpensive and easy. This paper explores new ideas for the improvement of HRQoL that consider clinical indicators, but the specific impact mechanism still needs to be further studied.
Conclusion
We used the disease-specific scale QLICD-CHD (V2.0) to evaluate patients’ HRQoL and utilized multiple linear regression analysis to finally confirm effective elements. From the results obtained, we conclude that demographic data like the family economy and clinical indicators such as chloride and percentage of lymphocyte population are significant factors in HRQoL for CHD patients. Clinicians can enhance their understanding of patients’ mental and physical states by closely monitoring related biomarkers. Clinicians can enhance their understanding of patients’ mental and physical states by closely monitoring related biomarkers.
Abbreviations
QLICD-CHD, Chronic Diseases-Coronary heart disease (V2.0); CHD, coronary heart disease; HRQoL, health-related quality of life; SOD, Social function; PHD, physical function; PSD, psychological function; SPD, specific module; TOT, Total scale score; EQ-5D-5L, European Quality of Life Five Dimension Five level scale; SF-36, 36-Item Short-Form Health Survey questionnaire; SAQ, Seattle Angina Questionnaire; KCCQ, Kansas City Cardiomyopathy Questionnaire.
Ethics Approval and Consent to Participate
The institutional review board of the affiliated hospital of Guangdong Medical University agreed with the study protocol and informed consent form (PJ2012052, YJYS2019010). All methods were carried out in accordance with relevant guidelines and regulations. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The paper is supported by the National Natural Science Foundation of China (71373058, 30860248).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bouchard K, Gareau A, Gallant NL, et al. Dyadic effects of anxiety and depression on quality of life among couples facing cardiovascular disease. J Psychosom Res. 2021;149:110601. doi:10.1016/j.jpsychores.2021.110601
2. Sarvasti D, Lalenoh I, Oepangat E, et al. Cardiovascular Protection Variables Based on Exercise Intensity in Stable Coronary Heart Disease Patients After Coronary Stenting: a Comparative Study. Vasc Health Risk Manag. 2020;16:257–270. doi:10.2147/VHRM.S259190
3. Wang Z, Chen X, Qi C, et al. The Relationship Between Lipoprotein A and Glycosylated Hemoglobin and The Degree of Coronary Artery Stenosis in Non-Diabetic Coronary Heart Disease Patients. Cardiol Vascular Res. 2019;3(4):15992–15997. doi:10.33425/2639-8486.1058
4. Noémi M, Renáta G, Evelin S, et al. The impact of coronary artery calcification on long-term cardiovascular outcomes. J Interdisciplin Med. 2021;6(1):15–20. doi:10.2478/JIM-2021-0007
5. Dai H, Much AA, Maor E, et al. Global, regional, and national burden of ischaemic heart disease and its attributable risk factors, 1990–2017: results from the Global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes. 2020;8(1):50–60. doi:10.1093/ehjqcco/qcaa076
6. The Writing Committee of the Report on Cardiovascular Health and Diseases in China. Interpretation of Report on Cardiovascular Health and Diseases in China 2020 (in Chinese). Chin J Cardiovasc Med. 2021;26(3):209–218.
7. Hu S, Gao R, Liu L, et al. [Summary of Chinese Cardiovascular Disease Report 2018]. Chin J Circ. 2019;34(3):209–220.
8. Pahmeier K, Neusser S, Hamm C, et al. Quality of life of patients with coronary heart disease treated with the bioresorbable vascular scaffold (ABSORB™): 2-year results from the GABI-R-registry. BMC Cardiovasc Disord. 2022;22(1):379–386. doi:10.1186/s12872-022-02815-2
9. Yuan M, Zhu HR, Li G. Literature review and progress on medical social work after the opening and reform. Chine Hospitals. 2016;20(8):1–5.
10. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–649. doi:10.1007/s40273-016-0389-9
11. Yang B, Xing M, Xu X, et al. The relation and influencing factors regarding quality of life and activity of daily living among patients with Alzheimer’s disease. Chine J Public Health Manag. 2016;32(4):427–430.
12. Mei Y, Wu H, Zhang H, et al. Health-related quality of life and its related factors in coronary heart disease patients: results from the Henan Rural Cohort study. Sci Rep. 2021;11(1):5011–5020. doi:10.1038/s41598-021-84554-6
13. Wu T, Li S, Li Z, et al. Efficacy and safety of Ginkgo biloba dropping pills in the treatment of coronary heart disease with stable angina pectoris and depression: study protocol for a randomised, placebo-controlled, parallel-group, double-blind and multicentre clinical trial. BMJ Open. 2023;13(5):e055263. doi:10.1136/bmjopen-2021-055263
14. Wan C, Wu X, Liu Y, et al. Research Status on the Second Version of the System of Quality of Life Instruments for Chronic Diseases QLICD(V2.0). J Guangdong Med Univ. 2022;40(3):243–249.
15. De Smedt D, Kotseva K, De Backer G, et al. EQ-5D in coronary patients: what are they suffering from? Results from the ESC EORP European Survey of Cardiovascular Disease Prevention and Diabetes (EUROASPIRE IV) Registry. Qual Life Res. 2020;29(4):1037–1046.
16. Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi:10.1016/0735-1097(94)00397-9
17. Green CP, Porter CB, Bresnahan DR, et al. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35(5):1245–1255.
18. Wang J, Su L, Huang Z. Effects of Family Function and Health Behavior on Quality of Life of patients with New Onset Stroke Thrombolysis. J Clin Nurs. 2021;20(3):12–16.
19. Jiang J, Ma X, Chen Z, et al. Analysis on life quality and influence Factors of 671 patients with coronary heart disease in Honghe prefecture. Soft Science of Health. 2017;31(8):59–62.
20. Ryu M. Factors Affecting on quality of life pre and post intervention in patients with coronary artery disease. J Korea Academia. 2022;23(5):151–158.
21. Dou L, Mao Z, Fu Q, et al. Health-Related Quality of Life and Its Influencing Factors in Patients with Coronary Heart Disease in China. Patient Prefer Adherence. 2022;16(1):781–795. doi:10.2147/PPA.S347681
22. Slepecky M, Kotianova A, Prasko J, et al. Which psychological, psychophysiological, and anthropometric factors are connected with life events, depression, and quality of life in patients with cardiovascular disease. Neuropsychiatr Dis Treat. 2017;13:2093–2104. doi:10.2147/NDT.S141811
23. Matsuda R, Kohno T, Kohsaka S, et al. The prevalence of poor sleep quality and its association with depression and anxiety scores in patients admitted for cardiovascular disease: a cross-sectional designed study. Int J Cardiol. 2017;228:977–982. doi:10.1016/j.ijcard.2016.11.091
24. Fu C, Yang Y, Xu M, et al. Analysis on related influencing factors of life quality of inpatients with coronary heart disease. J Jilin Univ. 2022;48(2):478–486.
25. Erdem A, Ceylan US, Esen A, et al. Clinical usefulness of red cell distribution width to angiographic severity and coronary stent thrombosis. Int J Gen Med. 2016;9:319–324. doi:10.2147/IJGM.S109452
26. Wan C, Li H, Fan X, et al. Development and validation of the coronary heart disease scale under the system of quality of life instruments for chronic diseases QLICD-CHD: combinations of classical test theory and Generalizability Theory. Health Qual Life Outcomes. 2014;12(1):82–92. doi:10.1186/1477-7525-12-82
27. World Health Organization. Cardiovascular Diseases (Cvds). Fact Sheet; 2017.
28. Xiong Q, Zhou Q, Liu Y, et al. Assessment of quality of life among patients with coronary heart disease. J Clin Cardiol. 2014;30(1):27–30.
29. Yacavone RF, Locke GR, Provenzale DT, et al. Quality of life measurement in gastroenterology: what is available? Am J Gastroenterol. 2001;96(2):285–297. doi:10.1111/j.1572-0241.2001.03509.x
30. Tang W, Quang Y, Tang J, et al. Correlation between Perceived of Empowerment and Quality of life in patients with coronary heart disease. Shanghai Nursing. 2022;22(2):26–30.
31. Zhu X, Zang P, Li C, et al. Study on quality of life and influencing factors of hypertension in community. Chine Commun Doctors. 2017;33(4):147–149.
32. Wu Y, Zhu B, Chen Z, et al. New Insights Into the Comorbidity of Coronary Heart Disease and Depression. Curr Probl Cardiol. 2021;46(3):1–43. doi:10.1016/j.cpcardiol.2019.03.002
33. Jørgensen TS, Wium-Andersen IK, Wium-Andersen MK, et al. Incidence of Depression After Stroke, and Associated Risk Factors and Mortality Outcomes, in a Large Cohort of Danish Patients. JAMA Psychiatry. 2016;73(10):1032–1040. doi:10.1001/jamapsychiatry.2016.1932
34. Tennant C, McLean L. The impact of emotions on coronary heart disease risk. J Cardiovasc Risk. 2001;8(3):175–183. doi:10.1177/174182670100800309
35. Hendricks B, Quinn TD, Price BS, et al. Impact of stress and stress mindset on prevalence of cardiovascular disease risk factors among first responders. BMC Public Health. 2023;23(1):1929. doi:10.1186/s12889-023-16819-w
36. Zhang H, Wang Y, Cai X, et al. Family functioning and health-related quality of life of inpatients with coronary heart disease: a cross-sectional study in Lanzhou city, China. BMC Cardiovasc Disord. 2022;22(1):397–407. doi:10.1186/s12872-022-02844-x
37. Sun N, Lv DM, Man J, et al. The correlation between quality of life and social support in female nurses. J Clin Nurs. 2017;26(7):1005–1010. doi:10.1111/jocn.13393
38. Wang W, Lau Y, Chow A, et al. Health-related quality of life and social support among Chinese patients with coronary heart disease in mainland China. Eur J Cardiovasc Nurs. 2014;13(1):48–54. doi:10.1177/1474515113476995
39. Nordgren L, Söderlund A. Received and needed social support in relation to sociodemographic and socio-economic factors in a population of people on sick leave due to heart failure. ESC Heart Fail. 2017;4(1):46–55. doi:10.1002/ehf2.12121
40. Megahed MM, Zidan DH, Abdelhalim ZM. Effect of chloride level on outcome in critically ill patients. Res Opinion Anesthesia Intensive Care. 2019;6(3):282–286. doi:10.4103/roaic.roaic_33_18
41. Rudloff E, Hopper K. Crystalloid and Colloid Compositions and Their Impact. Front Vet Sci. 2021;31(8):639848. doi:10.3389/fvets.2021.639848
42. Lan L, Hu W. Overview of the development process and regulation mechanism of B lymphocytes. Biology Teaching. 2022;47(07):6–8.
43. Zafrir B, Hussein S, Jaffe R, et al. Lymphopenia and mortality among patients undergoing coronary angiography: long-term follow-up study. Cardiol J. 2022;29(4):637–646. doi:10.5603/CJ.a2020.0141
44. Deveci B, Gazi E. Relation Between Globulin, Fibrinogen, and Albumin With the Presence and Severity of Coronary Artery Disease. Angiology. 2021;72(2):174–180. doi:10.1177/0003319720959985
45. Chien SC, Chen CY, Leu HB, et al. Association of low serum albumin concentration and adverse cardiovascular events in stable coronary heart disease. Int J Cardiol. 2017;241:1–5. doi:10.1016/j.ijcard.2017.04.003
46. Kim S, McClave SA, Martindale RG, et al. Hypoalbuminemia and Clinical Outcomes: what is the Mechanism behind the Relationship? Am Surg. 2017;83(11):1220–1227. doi:10.1177/000313481708301123
47. Houston M, Minich D, Sinatra ST, et al. Recent Science and Clinical Application of Nutrition to Coronary Heart Disease. J Am Coll Nutr. 2018;37(3):169–187. doi:10.1080/07315724.2017.1381053
48. Arques S. Serum albumin and cardiovascular disease: state-of-The-art review. Ann Cardiol Angeiol. 2020;69(4):192–200. doi:10.1016/j.ancard.2020.07.012
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
