Back to Journals » Risk Management and Healthcare Policy » Volume 14
Health QR Code Application in the Novel Containment Strategy and Healthcare Plan for Pregnant Women and Children Under Quarantine During the Summer Outbreak of SARS-CoV-2 Delta Variant in Chengdu, China: An Observational Study
Authors Chen S, Liu T, Li X, Luo Y, Xiao L, Zhang L, Wen R, Lin Y
Received 26 August 2021
Accepted for publication 17 October 2021
Published 3 November 2021 Volume 2021:14 Pages 4499—4510
DOI https://doi.org/10.2147/RMHP.S335803
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Haiyan Qu
Shan Chen,1,* Tianjiao Liu,1,2,* Xin Li,2,* Yingjuan Luo,3 Li Xiao,1 Libing Zhang,4 Rongkang Wen,3 Yonghong Lin2
1The Medical Administration Department, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China; 2The Department of Obstetrics and Gynecology, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China; 3The Healthcare Department, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China; 4The Department of Pediatric Surgery, Chengdu Women’s and Children’s Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yonghong Lin Tel +86 13808031895
Fax +86 28 61866003
Email [email protected]
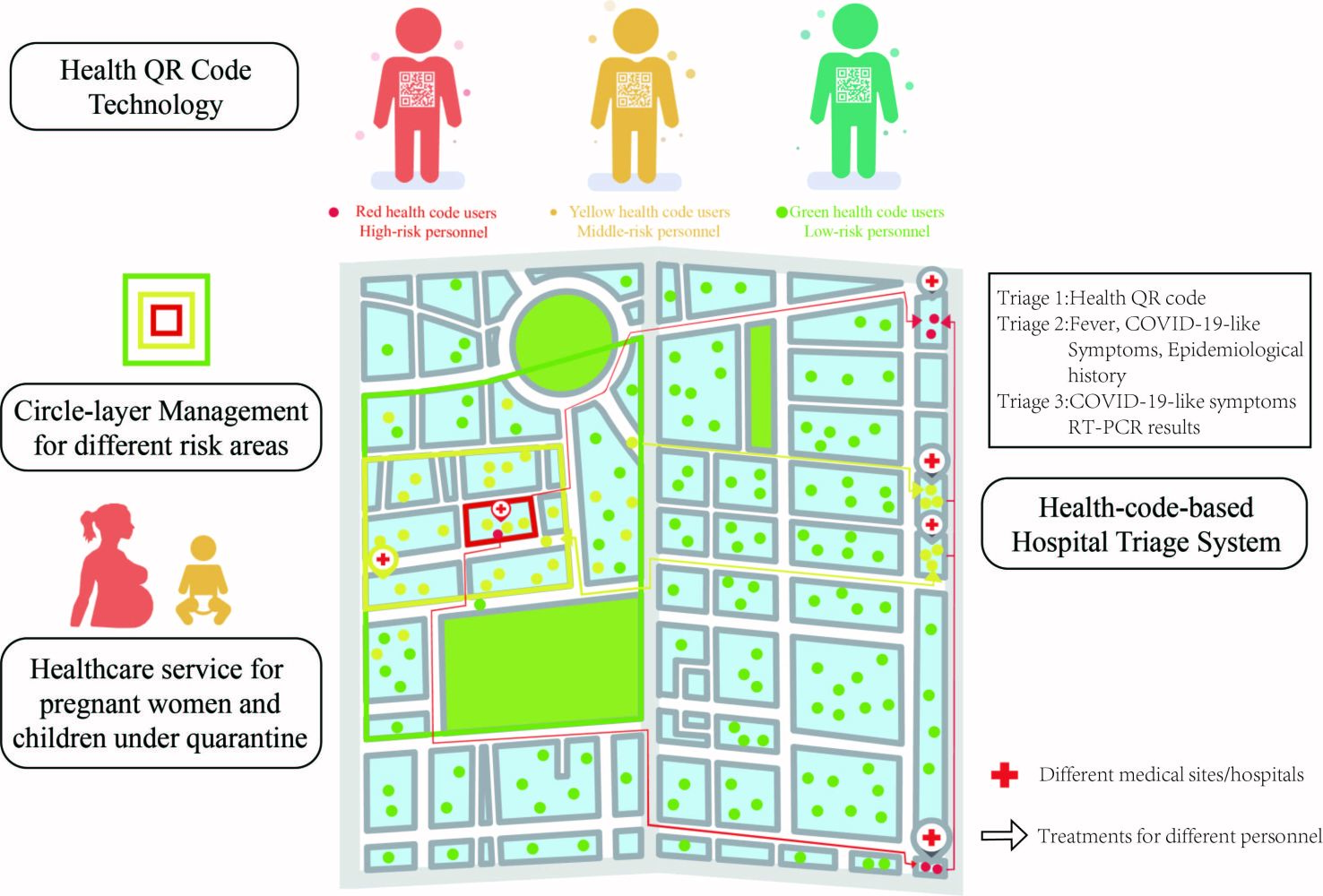
Purpose: To report the experience of health QR code application in Chengdu’s anti-epidemic measures including circle-layer management, hospital triage system and healthcare plan for quarantined pregnant women and children during the summer outbreak of SARS-CoV-2 Delta strain in 2021 and to evaluate these measures.
Methods: We comprehensively summarized Chengdu’s health code application in the circle-layer management (a set of stringent confinement measures of places confirmed cases and close contacts have recently been to and less strict quarantine measures of surrounding areas), hospital triage system, and healthcare plan for quarantined pregnant women and children. We also assessed the effectiveness or efficiency of these measures by analyzing the number of different cases with confirmed COVID-19 infections or epidemiological history, the attitude of quarantined pregnant women toward the summer outbreak and healthcare services, as well as the time needed for obtaining epidemiological history and accuracy of health-code-based hospital triage system.
Results: The circle-layer management lasted 15 days and ended with no community or nosocomial transmission happened. Approximately 70 pregnant women and 600 children below 6-year-old were quarantined. Four home visits and two patient transfers were performed. Online survey indicated that about 80% of quarantined women felt satisfactory about the healthcare service. The novel triage system identified 137/221 (61.99%) patients with epidemiological history from patients with yellow health code, and 71/4504 (1.57%) patients from patients with green health code in our hospital (p < 0.001). The health QR code markedly outperformed the traditional methods in the efficiency experiment of obtaining epidemiological history (3.52 ± 0.98 vs 78.91 ± 23.18 seconds, P < 0.001).
Conclusion: The circle-layer management has successfully and precisely prevented the spread of the summer outbreak of COVID-19 in Chengdu. The health-code-based triage system showed great effectiveness and efficiency in triaging patients with epidemiological history. The healthcare services for quarantined pregnant women has basically met their needs.
Keywords: triage, quarantine, pediatrics, obstetrics, precise prevention and control
Graphical Abstract:
Introduction
The global society has experienced an exponential increase in the number of confirmed cases of infection and death of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) since March 2020.1 Various strategies have been implemented by many countries, including social distancing, lockdown, and nation-wide vaccination,2–5 but from a global perspective, the pandemic is still rampant. Through the long-term and united efforts of all citizens, especially healthcare workers, China has almost successfully eradicated the domestic epidemic of the Coronavirus Disease 19 (COVID-19) and hence resumed the social and economic orders since April 2020.6 However, the Nanjing outbreak from mid-July to mid-August 2021 has caused about 1100 correlated confirmed infections in multiple provinces and cities. On 27th July, a family of three in Chengdu were diagnosed as confirmed cases 3 days after their travel to Zhangjiajie, a tourism hotspot that just underwent a clustered outbreak. Another 3 cases were subsequently diagnosed with confirmed infection, including an airport worker, a close contact of the beforementioned family, and a middle-aged female who also traveled to Zhangjiajie several days ago.
Considering that, unlike previous strikes of COVID-19, the summer outbreak in Chengdu was sporadic, small-scale, and traveling-correlated, thus it was unsuitable to be tackled by rigorous measures like city-wide lockdowns and home quarantine. On the other hand, close contacts of confirmed cases and personnel with epidemiological history and COVID-19 manifestations (fever, cough, and dizziness, etc.) should be identified efficiently and effectively in public places, especially hospitals. However, the traditional ways of epidemiological history inquiry were laborious, time-consuming, and unable to screen out misleading information. Noteworthily, the majority of the confirmed cases in the current epidemic were infected by the Delta variant. As described in the previous publications, this mutant strain has a 60% higher risk of community transmission than the ancestral Alpha strain. It is even able to cause asymptomatic breakthrough infections in vaccinated patients,7,8 making it unfeasible to triage patients simply based on the body temperature and COVID-19-like clinical manifestations. To address these problems, Chengdu promptly implemented the circle-layer quarantine policy, and widely applied the health QR code in the circle-layer management and the triage system of hospitals.
The circle-layer quarantine policy is a set of risk-level-based containment measures which categorized the potential risk areas into 3 circles or layers: (1) lockdown areas, the areas where the confirmed cases have recently been to; (2) restricted areas, the areas where the close contacts have recently been to; and (3) areas with potential risks, the surrounding areas of the lockdown or restricted areas. Accordingly, this policy implemented stringent confinement measures in lockdown and restricted areas and carried out relatively less strict containment measures in areas with potential risks, aiming to minimize the scale of influenced communities and citizens while stopping the spread of the epidemic.
The health QR code is a plug-in-like mini program running in social media apps like WeChat and online payment platforms like Alipay, which records and updates the users’ COVID-19 related health information such as body temperature, clinical symptoms (fever, cough, dizziness, etc.), potential contact with the infected patient and daily itinerary details.9 The three colors of the QR code match the corresponding risk levels of its user. Only users with a green code are allowed to use public transportation and facilities freely. Smartphone owners with a red or yellow health QR code will be required to be quarantined and/or get RT-PCR tests for SARS-CoV-2.9
Pregnant women and children in China are presumably vulnerable to the Delta strain due to their low vaccination rate.10,11 It was reported that the pregnant women have a significantly higher ICU admission rate if infected by the SARS-Cov-2.12 Previous publications also indicated that pregnant women and children under quarantine had higher rates of depressive symptoms, anxiety, and other negative effects.13–15 Therefore, to ensure their mental and physical health of and to avoid difficulties and inconveniences in getting medical care for quarantined pregnant women and children, a healthcare plan for them was made and implemented. In this plan, medics and community workers in quarantine sites would help monitor the health condition of pregnant women and children and do the RT-PCR tests for them. For those needed professional obstetrics and pediatrics services, they can appoint medical home visits by phone call. The patient transfer would also be performed when the patient should be taken care of in the hospital after medical evaluation.
This article aims to summarize, report, and evaluate Chengdu’s anti-epidemic measures in the summer outbreak of the Delta variant of SARS-CoV-2, in which the novel anti-epidemic technology, health QR code, played an essential role. We hope our experience could be helpful in providing some novel strategies and inspirations of swiftly containing the small-scale and imported epidemic for domestic or overseas cities and medical institutions confronted with similar situations.
Materials and Methods
Health QR Code System
The Health QR code system applied in the present research was Tianfu Health Code released by Sichuan Provincial Emergency Headquarters for Covid-19.16,17 It is a mandatory system in all public places and facilities in mainland China during the epidemic, which collects and integrates users’ spatial and temporal data using Bluetooth, Global Positioning System (GPS), geolocation information of Network base station, and online transactions.9 As shown in Supplementary Figure 1, it has a built-in module called Entrance Code required to be shown before entering communities and public places, which can record and upload the users’ visit history of public places or communities. Young and senior citizens and other non-smartphone-users can also get their health QR codes once their family applied the Family Health Code for them. Functions like senior mode and voice assistant were also available in the mini program for the elderly. Through a specific algorithm, the health code was able to identify people with epidemiological history, which includes (1) those who have traveled to or lived in the communities with confirmed cases within 14 days before onset; (2) those who have had close contact with confirmed cases and asymptomatic cases within 14 days before onset; (3) those with respiratory symptoms and have had close contact with the people from the communities with confirmed cases within 14 days before onset; (4) those who have been to foreign countries within 14 days.18 At the very beginning of the summer outbreak, 29th July, a survey on the epidemiological history of confirmed cases and their close contacts was conducted by workers of corresponding communities and local Center of Disease Control through phone calls, surveillance videos checks, and face-to-face interviews (with personal protective equipment). This information was used to identify the communities and persons at the highest risks of being infected and was uploaded to the Sichuan Big Data Center as the initial information for the circle-layer management and health QR code system.
The Classification and Management of Areas at Different Risk Levels
The classification of areas at different risk levels was based on the numbers of existing confirmed cases: areas with more than 50 existing confirmed cases and clustered onset within 14 days were defined as high-risk areas; areas with less than 50 confirmed cases were defined as middle-risk areas; areas with no confirmed cases were defined as low-risk areas.
The circle-layer management was a set of comprehensive containment measures based on the risk levels of communities with confirmed cases and their surrounding areas. These areas were classified into 3 different layers or circles and were managed accordingly as described below (Figure 1).
Lockdown areas (middle-/high-risk areas): the finding spots, living places, activity places and workplaces of confirmed cases were set as lockdown areas. No citizen would be allowed to enter or leave these areas during the circle-layer management. Citizens living in the lockdown areas were all regarded as potential close contacts thus were required to be quarantined for 14 days. They got RT-PCR tests on the 1st, 4th, 7th, and 14th days of quarantine. Community workers and volunteers were designated to offer life services such as food delivery, express delivery, and daily necessities delivery. If there were no new confirmed cases during these 14 days, the lockdown policy in these areas would be lifted. Additionally, they were still not allowed to do any group activity in the first week after the quarantine.
Restricted areas: the living and working places of the close contacts were set as restricted areas. Citizens in the restricted areas were required to be quarantined for 14 days. Individuals from outside were allowed to get into these areas but could not leave till the end of quarantine. The RT-PCR tests were performed for everyone living in the restricted areas on the 1st, 7th, and 14th days of quarantine.
Areas with potential risks: the surrounding areas of the lockdown or restricted areas were defined as areas with potential risks. Normal life activities, except group activity and mass gathering, were all allowed in these areas. The RT-PCR tests for people living in these areas were performed on the 1st and 7th day of circle-layer management.
The Classification and Management of People Groups at Different Risk Levels Using Health Code
Close contacts: According to the latest Protocol of COVID-19 Prevention and Control (Edition 8) released by the National Health Commission of the People’s Republic of China, close contacts are individuals who have had contact, without effective protection, with one or more suspected or confirmed COVID-19 cases any time starting 2 days before the onset of the suspected or confirmed cases’ symptoms or 2 days before sampling for laboratory testing of asymptomatic infected persons.18
High-risk personnel: includes confirmed cases, suspected cases, close contacts, secondary close contacts, people from overseas, people who have been to high-risk areas within 14 days.
Middle-risk personnel: includes people with potential contacts with high-risk persons within a week.
Low-risk personnel: includes people without epidemiological history.
There are 3 different colors of Health QR Code matching personnel of corresponding risk levels: red, high-risk personnel; yellow, middle-risk personnel; green, low-risk personnel (Supplementary Table 1). Citizens were managed according to their health code color and living areas during the circle-layer management:
- Red health code users with confirmed infections: these cases were transferred to infectious disease hospitals for treatment through negative pressure ambulance once identified (Figure 1 Route A&B).
- Red health code users with close contacts or secondary close contacts, or recently arrived in Chengdu from high-risk areas: these citizens were transferred to centralized isolation sites for medical observation (Figure 1 Route C&D).
- Yellow health code users in restricted areas without confirmed infections were quarantined in their own apartment.
- Yellow health code users in areas with potential risks were not allowed to use public transportation or go to public places like malls, supermarkets, movies theaters, bars, etc. Once found in public places, they would be suggested to wear proper protective equipment and transferred back to their community. They were permitted to go to designated hospitals or RT-PCR testing stations via private or community-arranged vehicles for RT-PCR tests or other medical services (Figure 1 Route E).
The yellow health codes of users from areas with potential risks would be turned into green once they got a negative nucleic acid testing result, while the red and yellow health codes of users in the lockdown and restricted areas would be turned into green only when they finished quarantine and got negative results in each nucleic acid test.
Management and Healthcare for Pregnant Women and Children Under Circle-Layer Management
The characteristics of quarantined pregnant women and children below 6 years old were listed in Supplementary Tables 2 and 3. We recorded their body temperatures, pregnancy-related clinical features, and epidemiological history. A detailed healthcare plan for them was made (Supplementary Figure 2). Door-to-door medical services were provided for quarantined yellow health code users with mild symptoms. Through phone appointments, pregnant women and children who need medical care would be treated by a standby team of obstetrics, pediatrics, emergency, nosocomial infection specialists. Patients with severe symptoms were transferred into designated hospitals by the negative pressure ambulance and settled in the isolation ward (Figure 1 Route F). Another standby team of obstetrics and pediatrics was arranged to back up the infectious disease hospital whenever necessary. The services we provided include the severity assessment, blood test, electrocardiography, two-dimensional ultrasonic image. For pregnant women, the urine pregnancy test and fetal heart rate monitoring were also provided. On the final day of their quarantine, an online survey about quarantined pregnant women’s attitude toward this summer outbreak and our healthcare services and the degree of their worry about being infected with COVID-19 was performed on the WeChat platform. The results are presented in Supplementary Table 2.
The Triage System Based on Health Code
The triage system implemented in this study was an update of our previous strategy with the application of Health QR Code.19 Only one entrance (hospital gate) and one exit (backdoor) were open for patients during the epidemic. Patients and medical staff had different designated one-way paths for entering and leaving the hospital. As shown in Figure 2, the 3 levels of our preliminary triage system had different tasks based on their locations and medical duties:
 |
Figure 2 The flowchart of the health-code-based triage system. Note: Colors of lines and boxes were matched with the color of patients’ or attendants’ health QR code. |
Triage 1 (Entrance of outpatient and emergency department): a rapid triage through body temperature detection and health code color checking. The epidemiological history of patients and their attendants were also briefly asked.
Triage 2 (Outpatient inquiries at nurse station): a detailed inquiry of patients and their attendants’ epidemiological history was performed in this triage. The health code and body temperature were also checked in case of omitted from the first triage.
Triage 3 (By the physicians who made the first diagnosis in outpatient clinic or in-patient department): a detailed inquiry or examination of patients’ chief complaint, COVID-19 correlated symptoms,19 epidemiological history was performed in this triage. The health code and body temperature would also be checked when necessary.
In this 3-level triage system, the patients were guided to different clinics or nucleic acid testing sites according to the result of the triage assessment:
- Patients with green health codes and no epidemiological history were guided to outpatient clinic. Those with fever or epidemiological history were referred to the regular fever clinic.
- Patients with green health codes, fever and epidemiological history, and patients with yellow health codes and fever/epidemiology history/COVID-19 symptoms were guided to the special fever clinic and get nucleic acid test thereby. If they got negative results in two consecutive samplings, their yellow code would turn green. If they got a positive result, they would be managed as suspected cases and get a second test to confirm their infection.19
- Patients with yellow health codes but had no fever, epidemiology history or COVID-19 symptoms were guided to the designated testing zone for yellow code users. Once they got a negative result, their health code would turn green after the result has been updated. If they got a positive result, they would also be managed as suspected cases and get a second test to confirm their infection.
Triage Efficiency Experiment of Health QR Code
An experiment testing the triage efficiency of the Health QR code and traditional face-to-face inquiry was conducted on 28th October 2021. The timing for the health QR code started when users initiated the Health QR code mini-program and ended when their smartphones showed their health QR code and itinerary information. The timing for a face-to-face inquiry began when the nurses in triage system started their first question and ended when they got a clear and satisfactory answer of epidemiological history. Our experiment equally included the results of all the 6 shifts of the triage system on that day. The results of this experiment are presented in Supplementary Table 4.
Data Collection
We collected and analyzed the daily numbers of different personnel with red health codes from the WeChat platform’s official account of the Chengdu Municipal Health Commission from July 21 to August 13, 2021. During the whole period of the circle-layer management (from July 28 to August 12, 2021), the numbers of pregnant women and children in quarantine were rendered daily by community workers or the medical professionals in the centralized isolation sites and infectious disease hospitals. The results of the online survey were gathered and processed automatically by the WeChat platform. Similarly, the numbers of patients with green and yellow health codes from regular and special fever clinics in Chengdu Women’s and Children’s Central Hospital were recorded by the doctors on duty during the circle-layer management.
Statistical Analysis
The software SPSS version 23.0 (IBM SPSS Inc., US) was applied for statistical analysis in this research. Categorical variables were all presented in the form of frequencies and percentages, including health QR code colors, age groups, educational background, monthly family income, epidemiological history, etc. Chi-square tests were used for the analysis of categorical variables. The continuous variable in the current study was the time (seconds) needed to obtain epidemiological history through different methods. It was shown in the form of mean ± SD and analyzed by Student’s t-test. A p-value < 0.05 was regarded as statistically significant.
Results
As shown in Figure 3A, after 3 indigenous confirmed cases have been identified on 27th July, the circle-layer management in Chengdu has included 3 communities and identified 2 indigenous confirmed cases and 1 asymptomatic case on 28th July. The number of imported confirmed and asymptomatic cases also remained stable during the circle-layer management (from July 28th to August 12th). Since July 29th, as the epidemiological history survey went on, about 1200 citizens have been identified and given red health codes. The circle-layer management ended on August 12th when the lockdowns in all 3 communities were lifted, with no new indigenous cases reported for 15 consecutive days. Only approximately 500 close contacts or imported cases remained, meaning that the circle-layer management controlled the transmission resource within 2 days and have prevented community chain transmission and nosocomial infection during the whole period.
The number of quarantined citizens peaked on August 9, 2021. On that day, 71 pregnant women and 575 children below 6 years old were under quarantine as shown in Figure 3B and C. During the quarantine, the staff from the Chengdu Women’s and Children’s Central Hospital has performed 4 home visits and 2 patient transfers. From Supplementary Tables 2 and 3, we can notice that the majority of quarantined pregnant women circle-layer management were from blocked communities while the children under quarantine were from disparate epidemiological history resources. All quarantined pregnant women participated in the online survey. The survey results indicated that about 80% of them did not worry about being infected with COVID-19, held an optimistic view about the summer outbreak in Chengdu, and felt quite satisfactory about the healthcare services we provided.
During the circle-layer management, as shown in Table 1, the health-code-based triage system of the hospital has identified 137 patients with epidemiological history from 211 patients with yellow health code (61.99%) and 71 patients with epidemiological history from 4504 patients with green code (1.57%) in the fever clinic (p < 0.001). As presented in Supplementary Table 4, the triage efficiency experiment showed that the health QR code remarkably outperformed the traditional face-to-face inquiry in the time (seconds) needed to obtain the epidemiological history of patients (3.52 ± 0.98 vs 78.91 ± 23.18, P < 0.001).
Discussion
Our study summarized the policies and measures taken by the local government and hospitals to stop the spread of SARS-CoV-2 Delta variants and serve for the obstetric and pediatric patients, among which the health code and a special quarantine policy (circle-layer management) played an essential role. The “circle-layer” policy had successfully exterminated the indigenous cases and avoided community transmission through widespread application of epidemiological history tracing technology, rigorous containment efforts of the communities where confirmed cases lived, and relatively less strict management of surrounding areas. The health code based 3-level triage system also played an essential role in preventing nosocomial infection. During the whole period of “circle-layer” management, pregnant women and children’s healthcare was also ensured by home visits or patient transfers provided from the medical professionals of designated women’s and children’s hospital.
Plenty of previous studies have proved the positive impact of containment in preventing the epidemic of COVID-19.5,20–23 Lau indicated that the lockdown measures in Wuhan since late January 2020 had remarkably slowed down the growth rate and extended the doubling time of confirmed cases.5 Another mathematical model-based research also implicated that the combined non-pharmaceutical interventions could achieve the strongest and quickest effect in containing the epidemic.21 However, such measures also inevitably lead to many side effects on the daily life, work, physical and mental health of citizens to varying degrees.24,25 Thus, an ideal strategy to prevent and control the epidemic must minimize the number of impacted citizens and the containment scale while stopping the transmission. The circle-layer policy, was proved precise and feasible to some extent in the scenario of sporadic or small-scale imported outbreaks like the one that occurred in Chengdu. With only 3 communities been lockdown for 2 weeks, the other 20 million inhabitants can still live a normal life and commute to their workplaces without worrying about the spread of transmission. Thus, the whole city could almost exert its full capability of providing life replenishment and medical support to those under confinement and blanketing the reignition of the epidemic at its very beginning.26,27
The status quo of the epidemic in China greatly lowered the applicability of the previous triage strategy.19,28 By mid-August, evidence showed that a quarter of the 2500 confirmed infections in China were defined as asymptomatic cases,29 suggesting that the epidemiological history is getting more critical and the previous triage systems are no longer reliable, since they heavily relied on the COVID-19 symptoms. However, the inquiry of epidemiological history is hard to be well performed in the 1st and 2nd triages, since it is too laborious and wrong information may be provided by patients and their attendants. Besides, for departments like pediatrics, respiratory, and fever clinic, it is quite impractical for them to perform the previous 3-level triage since a big percentage of their patients have COVID-19-like symptoms. The advent of the health QR code, a contact-tracing, and health surveillance mini program, had perfectly solved these problems, fulfilled the concept of precise epidemic control, and facilitated a variety of other COVID-19 containment measures. It timely and precisely collects and updates the COVID-19 correlated symptoms and itinerary information of most citizens, thus enabled governments’ prompt, coherent and accurate decisions on public health policies and the management of citizens with epidemiological history.9 It also provided a convenient platform for public facilities, especially the hospitals, to quickly identify and reject personnel at high or potential risks.30
However, the health code also harbors many hidden troubles regarding data security, accuracy, and government surveillance. For instance, at the beginning of the summer outbreak in Chengdu, quite a few citizens who declared no epidemiological history still received a yellow health code. It led to many inconveniences to those citizens and posed tremendous pressure in the nucleic acid testing capability of medical institutions, for citizens want to turn their health code to green. Other concerns about the health code would be the discrimination toward the red or yellow health code users found in public and their difficulty in getting public services, including the medical care. Moreover, the public is not well acknowledged of who manages the health code, how their information is disposed of or protected, and whether their personal information would be disclosed.9
In the present study, the group that we mainly focused on were pregnant women and children. Due to the low vaccination rate of pregnant women and children in China, they are susceptible to the Delta variant.10,11 Evidence also showed that COVID-19 infected pregnant women had a higher ICU admission rate than those without gestation.12 Therefore, we formulated a detailed plan for providing healthcare to children and pregnant women in quarantine. They could appoint the medical services they need through phone appointments, and the community workers would also pay several home visits to record their physical and mental health status. The online survey results showed that the majority of quarantined pregnant women were satisfied with the medical services we offered and were optimistic about the summer outbreak. It indicated that though only 4 home visits and 2 patient transfers were performed during the quarantine, such medical cares have basically ensured their accessibility of medical service. Previous publications indicated that pregnant women and children in quarantine had higher rates of depressive symptoms, anxiety, and negative affect.13–15 However, due to the lack of professionals with psychological backgrounds, no mental counseling was provided for the children and pregnant women in quarantine. Generally speaking, given that no community chain transmission occurred, our healthcare system had basically satisfied their healthcare needs.
Though the proper containment efforts that a city has to make should be proportionate to the epidemic scenario she is in,31 new variants with high transmissibility and morbidity continuously appear and get prevalent, making the feasibility of coexistence with the SARS-CoV-2 through large-scale vaccination decreasing noticeably.32–34 As many non-capital Chinese cities and tourism hotspots with limited resources and brittle epidemic prevention systems reported hundreds of confirmed cases in this summer outbreak, the prompt implementation of the circle-layer management of risk areas and the health code based triage system may greatly reduce the resources and efforts it would cost to exterminate the outbreak before the occurrence of medical resources panic squeeze. Chengdu’s comprehensive containment strategy had again proved the effectiveness of conservative and rigorous measures, including comprehensive surveillance, strict contact tracing, and most importantly, quarantine. Many factors contributed to the success of fighting against the summer outbreak, including anti-epidemic experience in previous strikes or from other cities, expert suggestions on the arrangement of COVID-19 control and prevention, and the publics’ cooperation and fear for the virus. Unlike previous situations, the application of health QR codes has made these efforts less time-wasting, money consuming, and less laborious. The more precise and smaller-scale quarantine policy had also brought novelty to our strategy. The way we provided healthcare to the pregnant and the young also set an example for cities under similar situations.
Conclusion
The circle-layer management successfully and precisely prevented the spread of summer outbreaks of COVID-19 in Chengdu, China in 2021. The health code-based triage system was efficient and effective in triaging patients with epidemiological history. The healthcare services had basically met quarantined pregnant women’s needs.
Data Sharing Statement
The data is available upon reasonable request to the corresponding author.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of Chengdu Women’s and Children’s Central Hospital (WCCH-202124) and conducted with the written informed consent of the participants.
Acknowledgments
We thank the quarantined citizens, health workers, and all the other personnels in Chengdu who contributed to the prevention and control of the COVID-19 during the summer outbreak.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Financial support of this work was provided by Chengdu Major Science and Technology Application Demonstration Project (No.2021-YF09-00048-SN) and Chengdu Municipal Medical Research Project (No.2020216).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
2. Hodgson SH, Mansatta K, Mallett G, Harris V, Emary KRW, Pollard AJ. What defines an efficacious COVID-19 vaccine? A review of the challenges assessing the clinical efficacy of vaccines against SARS-CoV-2. Lancet Infect Dis. 2021;21(2):e26–e35. doi:10.1016/S1473-3099(20)30773-8
3. Habas K, Nganwuchu C, Shahzad F, et al. Resolution of coronavirus disease 2019 (COVID-19). Expert Rev Anti Infect Ther. 2020;18(12):1201–1211. doi:10.1080/14787210.2020.1797487
4. Ang YY. When COVID-19 meets centralized, personalized power. Nat Hum Behav. 2020;4(5):445–447. doi:10.1038/s41562-020-0872-3
5. Lau H, Khosrawipour V, Kocbach P, et al. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J Travel Med. 2020;27(3). doi:10.1093/jtm/taaa037
6. Tu H, Tu S, Gao S, Shao A, Sheng J. Current epidemiological and clinical features of COVID-19; a global perspective from China. J Infect. 2020;81(1):1–9. doi:10.1016/j.jinf.2020.04.011
7. Lopez Bernal J, Andrews N, Gower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant. N Engl J Med. 2021;385(7):585–594. doi:10.1056/NEJMoa2108891
8. Dyer O. Covid-19: delta infections threaten herd immunity vaccine strategy. BMJ. 2021;374:n1933. doi:10.1136/bmj.n1933
9. Liang F. COVID-19 and health code: how digital platforms tackle the pandemic in China. Soc Media Soc. 2020;6(3):2056305120947657.
10. Liu S, Yuan C, Lin J, et al. Association between vaccinations and clinical manifestations in children with COVID-19. Transl Pediatr. 2021;10(1):17–25. doi:10.21037/tp-20-225
11. Transcript of the Press Conference on March 21st, 2021 by the Joint Prevention and Control Mechanism of the State Council; 2021. Available from: http://www.nhc.gov.cn/xcs/s3574/202103/b3b8103da9104fc58d7ce8f5189e9be2.shtml. Accessed March 21, 2021.
12. Pirjani R, Hosseini R, Soori T, et al. Maternal and neonatal outcomes in COVID-19 infected pregnancies: a prospective cohort study. J Travel Med. 2020;27(7). doi:10.1093/jtm/taaa158
13. Xie X, Xue Q, Zhou Y, et al. Mental health status among children in home confinement during the Coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020;174(9):898–900. doi:10.1001/jamapediatrics.2020.1619
14. López-Morales H, Del Valle MV, Canet-Juric L, et al. Mental health of pregnant women during the COVID-19 pandemic: a longitudinal study. Psychiatry Res. 2021;295:113567. doi:10.1016/j.psychres.2020.113567
15. Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741–748. doi:10.1007/s00737-020-01092-2
16. “Sichuan Tianfu Health Code” health QR code was launched across the province; 2021. Available from: http://www.sc.gov.cn/10462/12771/2021/1/13/9387f1c13bf54c2cb8cc9346e35a2380.shtml.
17. Tianfu Health Code; 2021. Available from: https://www.tfjkt.cn/.
18. Council JPaCMotS. Notice on the issuance of the protocol for prevention and control of COVID-19 (Edition 8). National Health Commission of China; 2021 [updated May 21]. Available from: http://www.gov.cn/xinwen/2021-05/14/content_5606469.htm.
19. Li C, Tang L, Luo Y, et al. The prevention and control experience of maternal health care from Chengu, China During the COVID-19 epidemic. Risk Manag Healthc Policy. 2020;13:2213–2217. doi:10.2147/RMHP.S261821
20. Li X, Liu M, Zhou R, Zhang Y, Wu C, Xu L. Centralized medical quarantine for imported COVID-19 in Shanghai, China. J Travel Med. 2020;27(5). doi:10.1093/jtm/taaa109
21. Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–413. doi:10.1038/s41586-020-2293-x
22. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2). doi:10.1093/jtm/taaa020
23. Kang C, Meng F, Feng Q, et al. Implementation of quarantine in China during the outbreak of COVID-19. Psychiatry Res. 2020;289:113038. doi:10.1016/j.psychres.2020.113038
24. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
25. Xin M, Luo S, She R, et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am Psychol. 2020;75(5):607–617. doi:10.1037/amp0000692
26. Wen J Life of blocked communities in Chengdu during the summer outbreak of COVID-19; 2021. Available from: https://m.thepaper.cn/baijiahao_13995382.
27. Fight against the Delta Variant in Chengdu; 2021. Available from: https://m.thepaper.cn/baijiahao_14017839.
28. Wang Q, Wang X, Lin H. The role of triage in the prevention and control of COVID-19. Infect Control Hosp Epidemiol. 2020;41(7):772–776. doi:10.1017/ice.2020.185
29. Council JPaCMotS. Notice on the issuance of the protocol for prevention and control of COVID-19 (Edition 6). National Health Commission of China; 2021. Available from: http://www.gov.cn/xinwen/2021-05/14/content_5606469.htm.
30. Zhu R, Cui Y, Guo L, et al. Application of QR code in three-level pre-viewing triage system in a hospital’s response to Beijing Xinfadi wholesale market COVID-19 epidemic. Chin J Nosocomiol. 2021;31(08):1267–1271.
31. Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med. 2020;27(3). doi:10.1093/jtm/taaa039
32. Callaway E. Could new COVID variants undermine vaccines? Labs scramble to find out. Nature. 2021;589(7841):177–178. doi:10.1038/d41586-021-00031-0
33. Tang JW, Tambyah PA, Hui DS. Emergence of a new SARS-CoV-2 variant in the UK. J Infect. 2021;82(4):e27–e28. doi:10.1016/j.jinf.2020.12.024
34. Rubin EJ, Baden LR, Farrar JJ, Morrissey S. Audio interview: viral variants and Covid-19. N Engl J Med. 2021;384(7):e38. doi:10.1056/NEJMe2102882
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



