Back to Journals » Risk Management and Healthcare Policy » Volume 16
Health Poverty Alleviation Project in Rural China: Impact on Poverty Vulnerability, Health Status, Healthcare Utilization, Health Expenditures
Authors Li Z , Chen Y , Ding J
Received 17 September 2023
Accepted for publication 2 December 2023
Published 8 December 2023 Volume 2023:16 Pages 2685—2702
DOI https://doi.org/10.2147/RMHP.S438352
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Zhipeng Li,1 Yuqian Chen,2 Jing Ding3
1Qu Qiubai School of Government, Changzhou University, Changzhou City, People’s Republic of China; 2School of Economics and Management, Shanghai University of Political Science and Law, Shanghai, People’s Republic of China; 3School of Public Economics and Administration, Shanghai University of Finance and Economics, Shanghai, People’s Republic of China
Correspondence: Yuqian Chen, Affiliated School of Economics and Management, Shanghai University of Political Science and Law, No. 7989 Waiqingsong Road, Qingpu District, Shanghai, 201701, People’s Republic of China, Tel +8618502116053, Fax +862139227342, Email [email protected]
Background: China has lead to the inception of the Health Poverty Alleviation Project (HPAP) in 2015. While the previous studies suggest that, despite its apparent reduction in patients’ financial strain, the long-term poverty reduction effects are yet to be fully elucidated. This study explores HPAP’s enduring impact on poverty reduction and the potential moral hazards.
Methods: Data were obtained from four waves of the China Health and Retirement Longitudinal Study (CHARLS) spanning 2011– 2018. We employed difference-in-differences (DID) models to gauge HPAP’s influence on participants’ poverty vulnerability, health outcomes, and healthcare utilization. The dynamic DID model is employed to test the robustness of HPAP policy effects. The mediation effect models were used to understand HPAP policy outcomes through physical examinations and inpatient care.
Results: Our dataset encompassed 40,384 participants, of which 5946 (14.72%) had been exposed to HPAP and 34,438 (85.28%) had not access. Our findings reveal that HPAP decreases poverty vulnerability by 3.3% (p < 0.01) and attenuates health deterioration by 1.84% (p < 0.01). Furthermore, HPAP enhances inpatient care utilization by 9.34% (p < 0.01) and self-treatment behaviors by 4.1% (p < 0.01) while significantly slashing outpatient and inpatient expenses (p < 0.05). The implementation of HPAP has significantly reduced healthcare costs by 72.8% (p < 0.05) out-of-pocket (OOP) payments of outpatient care during the past month for the last time, and 89.39% (p < 0.05) out-of-pocket (OOP) payments of inpatient care during past the year for the last time. Mechanistic analyses have shown that the indirect effect of the HPAP policy decreases poverty vulnerability by − 0.132% (p < 0.05) physical examinations and − 0.309% (p < 0.05) inpatient care.
Conclusion: The HPAP initiative markedly attenuates poverty vulnerability and forestalls health decline among the rural populace. Moreover, HPAP bolsters healthcare service use, such as physical examinations and inpatient care, primarily attributed to the release of pent-up demand rather than moral hazards.
Keywords: chronic poverty, poverty due to illness, poverty vulnerability, ex ante moral hazard, ex post moral hazard, health poverty alleviation project
A Letter to the Editor has been published for this article.
A Response to Letter by Mr Muttaqin has been published for this article.
Graphical Abstract:
Introduction
Health insurance plays a crucial role in poverty management, reducing vulnerability to poverty and elevating socio-economic security.1 This is due to the inability of the poorest of the poor to divert resources from other basic needs to health care.2 If families do not receive adequate protection from the health insurance system, low- and middle-income families are even more likely to incur catastrophic health expenditure.3–6
China has set up an information system and created electronic information files for identifying the rural poor population. There were 12.56 million poor households that had been impoverished or returned to poverty due to illness in 2013, accounting for 42.4% of the total number of registered poor families with a record,7 while the figure was 44.1% in 2015.8 This further demonstrates that a severe illness can still devastate low- and middle-income families, especially in rural areas.9 In 2003, in a strategic move to expand the scope of essential medical insurance coverage in rural locales, China instituted the New Rural Cooperative Medical System (NCMS). Research showed that the NCMS did not provide sufficient economic protection from catastrophic health expenditure for vulnerable groups.10,11 Rural residents, who enrolled in NCMS, increased utilization of outpatient and inpatient services, that may also cause by the potential supply-side moral hazard, like more expensive equipment are used by central township health center.12–16 Inequitable access to health care and financial protection for rural residents may result from the fragmentation in social health insurance schemes between urban and rural regions.17 Therefore, China has reformed the basic medical insurance system, establishing Critical Illness Insurance (CII) in 2015, and implementing the urban-rural health insurance integration to form Urban-Rural Resident Basic Medical Insurance (URRBMI) merged NCMS and Urban Resident Basic Medical Insurance (URBMI) in 2016. In order to alleviate health expenditure poverty, it is more important for the China, to improve the medical infrastructure of rural medical institutions and enhance the fairness of health resource allocation by continuously investing more financial investment in rural primary medical institutions.18 In 2015, China released a pivotal policy document, “Decision on Winning the Battle Against Poverty”. This groundbreaking document marked the debut of the Health Poverty Alleviation Project (HPAP). Subsequent to this, the Chinese Central Government promulgated a succession of policies to champion the full-fledged rollout of HPAP. Detailed insights into the procedural facets of HPAP’s deployment are cataloged in Table A1.
HPAP encompasses an array of strategic measures spanning diverse areas. First, Basic Medical Insurance Systems: The New Rural Cooperative Medical System (NCMS) and Critical Illness Insurance (CII) for rural inhabitants furnish enhanced security measures for economically disadvantaged rural families. This chiefly manifests in amplified reimbursements for severe ailments. Second, Augmentation of Medical Assistance: Enhancements to medical and charitable assistance serve as robust pillars underpinning the basic medical insurance frameworks (NCMS and CII). This symbiosis ensures robust health safeguarding for vulnerable rural households. Third, Dynamic Management System: The nation’s poverty alleviation directorate has pioneered a dynamic health-based poverty alleviation management scheme. This incorporates electronic archival systems, facilitating the precise identification of impoverished rural families and enabling a structured settlement procedure for critical ailment treatments. Fourth, Resource Equilibration: HPAP champions the equitable distribution of medical resources across urban and rural landscapes. This involves fostering consistent collaborations between preeminent tertiary medical institutions in affluent regions and county-level hospitals in underprivileged sectors. Fifth, Medical Infrastructure Development: There is a concerted effort to actualize standardized healthcare service infrastructures at county and village strata in deprived areas. Concurrently, there is a concrete policy plan for the diffusion of telemedicine diagnostic services and health consultancy into these locales. Sixth, Human Resources: HPAP enacts enabling policies to stimulate the migration of medical talent to primary health institutions in deprived territories. Additionally, it underscores the significance of comprehensive training for healthcare professionals. Seventh, Public Health Initiatives: Deliberate strides are taken to elevate the quality of fundamental public health services in impoverished zones. This includes bolstering epidemic control, enhancing pediatric nutrition, and rolling out maternal-child health programs.
The HPAP significantly promoted the utilization of inpatient care services among the poor population,19 and alleviate the multidimensional relative poverty of older adults, which has more effective for older adults with chronic diseases or disabilities.20 HPAP significantly improves financial risk protection, and reduces the economic burden of disease for poor households, such as the total annual out-of-pocket (OOP) payments by 13.1% on average (2.4% for outpatient care, 19.5% for inpatient care), and the probability of incurring catastrophic healthcare expenditures by an average of 3.9% for low-income households.21,22 However, after the implementation of HPAP, low-income poor families still have a high incidence (12.1%) of catastrophic medical expenditures in Sichuan province. HPAP can reduce the occurrence and intensity of catastrophic health expenditures by 17.1% and 31.2%, respectively. The point of divergence is that the policy effect of HPAP is more effective for poor health and extremely poor families.23 By analyzing the data of the Health Poverty Alleviation System in Shandong province from 2015 to 2017, the study found that HPAP has achieved significant policy effects on poverty reduction. But there were still a number of patients in poverty-returning due to medication expenses in some regions, indicating that medication effect needs to be improved in the disease-related poverty population.24 Some studies found that the HPAP objects lack endogenous motivation to get out of poverty due to insufficient social support and health education.25
Prior research has investigated the effects of the HPAP on catastrophic health expenditures. Yet, there is a gap in understanding the long-term consequences of HPAP on poverty and health through the perspective for a cost–benefit policy analysis. In this context, our study introduces an analytical framework for evaluating such policies. We view the influence of HPAP on the vulnerability of rural residents to poverty and health deterioration as an indicator of the long-term benefits of policy execution. Simultaneously, we consider the potential for ex-ante and ex-post moral hazards in healthcare utilization and healthcare expenditure as indicative of the hidden cost associated with policy enforcement. We then evaluate HPAP’s influence on these outcomes. Notably, the Chinese government has initiated various strategies to foster a sustainable mechanism for HPAP, shifting away from perceiving its execution as merely a transient poverty relief measure. Our research’s unique contribution is that it furnishes a compelling policy rationale, suggesting that the HPAP should be regarded by governmental bodies as a persistent strategy for poverty mitigation in all countries with poverty.
Data and Method
Data
The China Health and Retirement Longitudinal Survey (CHARLS), led by the National Development Research Institute of Peking University, is a collaboration with the China Social Science Research Centre and the Youth League Committee of the same institution. This project, funded by the National Natural Science Foundation of China, strives to gather microdata representing Chinese individuals aged 45 and older to study China’s aging population. Initiated in 2011, the CHARLS baseline survey spanned 150 county-level units in 28 regions, capturing data from approximately 17,000 individuals across 10,000 households. Subsequent waves, planned at biennial or triennial intervals, provide data for researchers post a one-year embargo. As of 2018’s fourth wave, the dataset comprises 19,000 respondents from 12,400 households. Four datasets (2011, 2013, 2015, 2018) have been released. The encompassing questionnaire details demographic, health, economic, and community aspects.
Opting for CHARLS to assess the policy effect of HPAP rested on four tenets: first, CHARLS’ outstanding interview success and data quality compared to peers; second, the provision of vital geographical data at the prefecture level, crucial for public policy assessment; third, the depth offered by CHARLS’ four waves data structure, ensuring a rigorous research design; fourth, comprehensive data on healthcare service utilization and expenditure, enabling thorough HPAP impact analysis (on both ex ante and ex post moral hazard).
This study harmonizes CHARLS individual data with city and provincial macro data, extracted from urban and provincial statistical yearbooks by the China National Bureau of Statistics.
Description of Variable
Dependent Variable
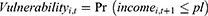
(1) Poverty vulnerability: Our study adopts the concept of vulnerability as expected poverty (VEP) by Chaudhuri et al.26 The VEP methodology is applicable to cross-sectional data, which has been widely used in academic research.27 Poverty vulnerability is generally defined as the ex-ante risk (ie, Uncertain critical illnesses and accident injuries; Reduction in agricultural production due to natural disasters; Unexpected unemployment et al) causes a household who is currently non-poor will fall below the poverty line, or a household who is currently poor will remain in poverty. The household is identified ideologically as vulnerable if probability of experiencing poverty in the future exceeds a set vulnerability line.28–30 The concept of poverty vulnerability characterizes chronic poverty experienced by household. Poverty vulnerability could be formally defined as the probability that the welfare (ie, income or consumption expenditures) of a household i at time t will be below the poverty line at time t+1 in Equation (1), where  is per capita household income and
is per capita household income and  is poverty line.
is poverty line.
HPAP’s policy targets the rural poor population, so we use the official criteria for the poverty line set by the administration.31 The current poverty standard means that the living standard of rural residents is less than 2300 yuan per capita per year at 2010 price in China, corresponding to the CHARLS sample survey time (2011 for 2536 yuan, 2013 for 2736 yuan, 2015 for 2855 yuan, 2018 for 2995 yuan). Our paper follows previous studies and uses a three-stage least squares (FGLS) approach to estimate parameter for calculating poverty vulnerability.26,32
(2) health decline: CHARLS will ask about self-assessed health in the three waves of data (2011, 2013, 2015) by randomly dividing respondents into two groups corresponding to the questions, 1) “Would you say your health is excellent, very good, good, fair, or poor?”, and 2) “Would you say your health is very good, good, fair, poor or very poor?”. Instead of randomly dividing the entire sample into two groups, the question 2) is answered directly for all respondents in the fourth wave of data (2018). We refer to the approach from previous literature that makes a significant contribution on evaluation of Chinese social health insurance for dealing with self-assessed health variable.10,33,34 The variable of self-assessed health is set to 1 for Excellent, Very good, Good; 0 for Fair, Poor, Very poor. The variable of health decline is set to 1 if self-assessed health in year t+1 is less than self-assessed health in year t, 0 for otherwise. As the health status of rural elderly aged 45 and older is declining, we want to evaluate the policy effect of the HPAP for mitigating health decline.
(3) Healthcare utilization and healthcare costs: The variables of healthcare utilization included physical examination, outpatient care, inpatient care, and self-treatment. The variables of healthcare costs included total costs and out-of-pocket (OOP) payments, which both are differentiated between the last time and a period of time (past month for outpatient care and self-treatment, and past year for inpatient care). Our study identifies whether the implementation of HPAP has triggered moral hazard by evaluating the impact of HPAP on healthcare service utilization and healthcare costs. We test the impact of HPAP on household healthcare costs, household affordability, and catastrophic health expenditures to confirm the occurrence of ex post moral hazard. Then, we identify ex ante moral hazard by evaluating the impact of HPAP on health behavior for physical examination, smoke and drink.
The Key Independent Variable
We set two types of key policy independent variables. First, the most important independent variable in the standard difference-in-difference model is the policy shock variable ( ), which indicates that individual i has experienced a policy shock in year t. To some extent the policy shock variable can be decomposed into an interaction term between the grouping variable and the policy incidence event. We include registered poor population, Dibao families, poor families with disabilities as the treatment group, and other households as the control group. We determined that the policy occurred in 2016 based on the HPAP policy document published by the Chinese government. Second, in order to conduct a dynamic evaluation of the HPAP policy effects, we combine the methodology of event studies and the characteristics of the CHARLS data structure to set the corresponding policy dynamic dummy variables, which correspond to
), which indicates that individual i has experienced a policy shock in year t. To some extent the policy shock variable can be decomposed into an interaction term between the grouping variable and the policy incidence event. We include registered poor population, Dibao families, poor families with disabilities as the treatment group, and other households as the control group. We determined that the policy occurred in 2016 based on the HPAP policy document published by the Chinese government. Second, in order to conduct a dynamic evaluation of the HPAP policy effects, we combine the methodology of event studies and the characteristics of the CHARLS data structure to set the corresponding policy dynamic dummy variables, which correspond to  for 2011,
for 2011,  for 2013, and
for 2013, and  for 2015. The CHARLS sample period is generally from July or August of the interview year to July or August of last year. There is only about one year of policy implementation in 2018, and therefore
for 2015. The CHARLS sample period is generally from July or August of the interview year to July or August of last year. There is only about one year of policy implementation in 2018, and therefore  for 2018.
for 2018.
Control Variables
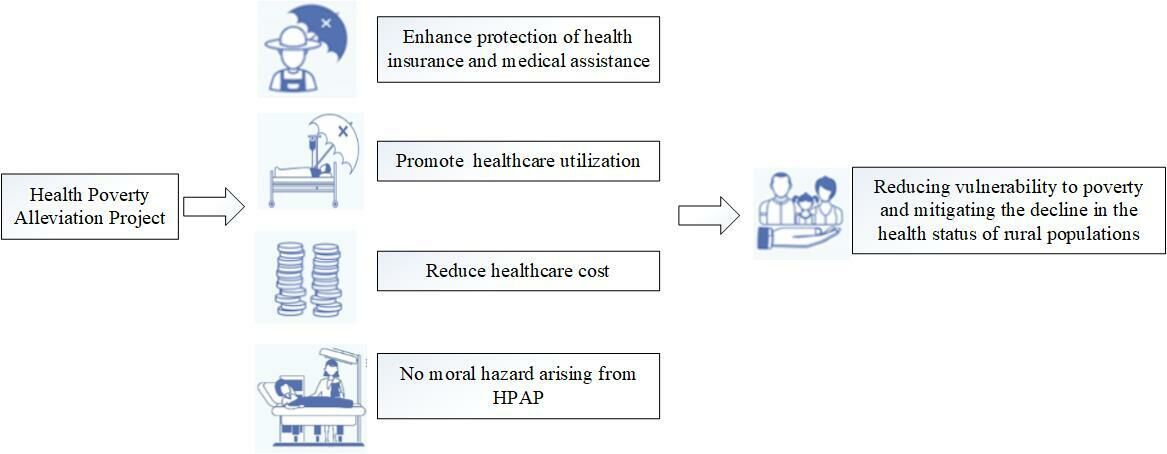
In order to obtain consistent and unbiased estimation of the HPAP policy effects, we control for potential omitted variables as much as possible at the individual, household, village, city, and provincial levels. First, a range of variables in individual and household demographic characteristics is controlled, including age, gender, marital status, education level, party membership, ethnic minority, family size, and household income. Second, we control the region characteristics of sewer system, asphalt roads in village representing the level of village infrastructure. Third, at the macro level, we also control for some characteristic variables. The per capita gross domestic product (GDP) in city for the level of urban economic development, and the number of medical institution beds per 10,000 people in province for the distribution of medical resources at the provincial level. Considering CHARLS only publishes party membership and ethnic minority in 2013, 2018 and community (or village) characteristics in 2011, we match data information across years, while potentially assumed that these individual and community characteristics keep stable in recent years. We provide more details for definition of the variables and descriptive statistics of the sample in the baseline regression in Table 1 and Table 2 respectively. Definitions and descriptive statistics of the variable for healthcare utilization and healthcare cost information are presented in Tables A2 and A3. We analyzed the impact of HPAP on ex ante and ex post moral hazard in discussion.
 |
Table 1 Definition of Variables |
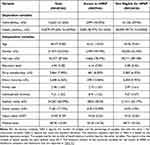 |
Table 2 The Characteristics of the Interviewees Included from Four Waves CHARLS |
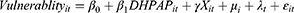
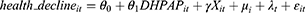
Empirical Strategy
Chinese government officially implemented the HPAP in 2016, and administrations have continued to improve the policy system of HPAP through the promulgation of a series of policy documents after 2017. The implementation of HPAP is exogenous to the entire target of policy assistance. This gives us an important quasi-experimental opportunity to evaluate the policy impact of HPAP with benefits on the reduction of the long-term poverty, health decline of the rural resident poor population, and the policy impact of HPAP with cost on moral hazard(ie, ex ante moral hazard and ex post moral hazard). We employ a standard DID model to evaluate the policy effects of HPAP in Equation (2–5). We analyze that whether the policy effect of HPAP triggers ex-ante and ex-post moral hazard by discussing the relationship between healthcare utilization and healthcare costs in Equation (4–5). The dynamic DID model is set up to test the parallel trend hypothesis in Equation (6), then we use the t-1 period ( ) as the baseline control group in dynamic test to avoid the dummy variable trap.
) as the baseline control group in dynamic test to avoid the dummy variable trap.
The HPAP provides comprehensive medical assistance, and improves the allocation of medical resources and the construction of medical infrastructures in poor areas. However, whether the rural poor population choose to receive medical assistance and access to medical resources depends on individual-level factors such as knowledge of the medical assistance policy (information bias), the degree of importance attached to health and the search for matching medical solutions (cognitive bias), and the risk preference (subjective preference) and other individual-level factors. Therefore, in order to control as much as possible for variables that are unobservable at the individual level, which may generate potential selection bias and avoiding the estimation bias introduced by nonlinear models,35 we control for individual-level fixed effects and choose a linear probability model as the identification method. Linear probability model is easier to interpret and faster to run than other logical models, especially in dealing with large data sets.36
 ,
,  ,
,  ,
,  represent the corresponding dependent variables. As the distinction between treatment and control groups is clarified in the introduction to data, the key independent of
represent the corresponding dependent variables. As the distinction between treatment and control groups is clarified in the introduction to data, the key independent of  in the model stands for the treatment of individual i affected by HPAP at time t.
in the model stands for the treatment of individual i affected by HPAP at time t.  is a bundle of control variable.
is a bundle of control variable.  is fixed effects at the individual level, and
is fixed effects at the individual level, and  is time-fixed effect.
is time-fixed effect.  is the error term.
is the error term.
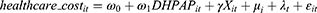
We tested the mechanism of the policy effects of HPAP through a mediation effect model based on previous studies,37,38 as shown in Equation (2, 7–10). Physical examination and inpatient care may be important channels for indirectly influencing the poverty vulnerability of rural poor population (Figure 1).
Empirical Results
Characteristics of the Population Selected
As shown in Figure 2, there are 5946 observations in the treatment group (34,438 observations in the control group). The data processing to remove the missing variable and outliers and 40,384 samples are finally retained in the baseline regression. Characteristics of the interviewees included are shown in Table 2.
 |
Figure 2 Flowchart of population selection. |
The Impacts of HPAP on Poverty Vulnerability and Health Decline
The main estimation results about the impact of HPAP on rural poor residents’ poverty vulnerability and health decline are reported in Table 3, based on Equation (2). The estimated results indicate that the HPAP significantly reduces 3.3% (p < 0.01) the poverty vulnerability between treat group and control group in Table 3 column (1). In addition to family size, other individual, household, village, urban and provincial level characteristics can significantly reduce poverty vulnerability. Specifically, the HPAP alleviates 1.84% (p < 0.01) health decline for the rural poor population in Table 3 column (2).
 |
Table 3 The Impact of HPAP on Poverty Vulnerability and Health Decline |
The Impacts of HPAP on Healthcare Utilization and Healthcare Costs
The estimated results of the impact of HPAP on the healthcare utilization are presented in Table 4. The HPAP did not significantly increase the outpatient care utilization by poor rural residents. The estimation is not statistically significant and is not large in terms of economic implications (0.36%, p > 0.1) in Table 4 column (1). HPAP significantly promotes 9.34% (p < 0.01) inpatient care utilization and 4.1% (p < 0.01) self-treatment behavior among rural poor residents in Table 4 columns (2–3).
 |
Table 4 The Impact of HPAP on Healthcare Utilization |
We report that the estimated results of the impact of HPAP on the healthcare cost are presented in Table 5. The implementation of HPAP has significantly reduced 49.89% (p < 0.1) the total outpatient costs and 73.99% (p < 0.01) out-of-pocket payments for last month outpatient care in Table 5 columns (1–2). The implementation of HPAP reduced 58.93% (p < 0.05) the total outpatient costs and 72.8% (p < 0.05) out-of-pocket payments for last time outpatient care in Table 5 columns (3–4). The implementation of HPAP reduces 89.39% (p < 0.05) out-of-pocket payments for the last time inpatient care in Table 5 column (8) but has no significant effect on total costs for either the past year or the last time inpatient care and did not significantly reduce the total cost and out-of-pocket payments of self-treatment in the past month. We will explore the reasons in the discussion section as for the CHARLS data structure and the policy implementation characteristics. The implementation of HPAP increased 21.36% (p < 0.01) the household medical expenditure of rural poor households in Table 5 column (11), squeezing out 16.87% (p < 0.01) the household’s affordability in Table 5 column (12), and also raised the incidence of catastrophic health expenditure by 12.59% (p < 0.01) in Table 6 column (4). Physical examination increased by 6.45% (p < 0.01) after the implementation of HPAP, while HPAP did not significantly increase the unhealthy behavior of smoking (0.97%, p > 0.1); instead, there was a significant decrease in drinking by 2.76% (p < 0.1) in Table 6 columns (1–3).
 |
Table 5 The Impact of HPAP on Healthcare Costs |
 |
Table 6 The Impact of HPAP on Ex Ante Moral Hazard |
Mechanisms Analysis
We tested the mechanism of the impact of HPAP with physical examination and inpatient care as mediating effects. The mediation model is set according to Equation (2, 7, 8) for physical examination, and Equation (2, 9, 10) for inpatient care. The total effect (path c) of HPAP is significantly negative according to the estimation in Table 3 column (1) based on Equation (2). The main estimation results of mediation analyses are reported in Table 6. The coefficient of path a ( =6.45%, p < 0.01,
=6.45%, p < 0.01,  = 9.34%, p < 0.01) is significantly positive in Table 7 columns (1, 3) for physical examination and inpatient care, respectively. The coefficient of path b (
= 9.34%, p < 0.01) is significantly positive in Table 7 columns (1, 3) for physical examination and inpatient care, respectively. The coefficient of path b ( = 2.04%, p < 0.01,
= 2.04%, p < 0.01,  = 3.31%, p < 0.01) is significantly negative in Table 7 columns (2, 4). The indirect effect (path a*b) is between HPAP and poverty vulnerability through physical examination and inpatient care are −0.132%, −0.309% (
= 3.31%, p < 0.01) is significantly negative in Table 7 columns (2, 4). The indirect effect (path a*b) is between HPAP and poverty vulnerability through physical examination and inpatient care are −0.132%, −0.309% ( ,
, ). The proportion of indirect effect to total effect is 4.097%, 9.633% (
). The proportion of indirect effect to total effect is 4.097%, 9.633% ( ,
, ).
).
 |
Table 7 The Mediation Effect Test of Physical Examination and Inpatient Care |
The Parallel Trend Assumption Test and Robustness Check
We report the dynamic DID estimation results of poverty vulnerability and health decline in Table 8 columns (1–2). The  corresponding to t-1 period is used as the baseline control group in dynamic test to avoid the dummy variable trap. The coefficients on
corresponding to t-1 period is used as the baseline control group in dynamic test to avoid the dummy variable trap. The coefficients on  and
and  are not significant, and the estimated absolute values are not large. This result suggests that the parallel trend test is passed. Our study achieves the robustness test by transforming the measure of the poverty line, which is defined in terms of the World Bank’s poverty standard of $1.25 per person per day. The estimation result is still significant negative (3.79%, p < 0.01) reported in Table 8 column (3). We simulated a placebo test by shifting the occurrence of the policy forward by one year, and the estimation result indicates that the placebo test passes in Table 8 column (4).
are not significant, and the estimated absolute values are not large. This result suggests that the parallel trend test is passed. Our study achieves the robustness test by transforming the measure of the poverty line, which is defined in terms of the World Bank’s poverty standard of $1.25 per person per day. The estimation result is still significant negative (3.79%, p < 0.01) reported in Table 8 column (3). We simulated a placebo test by shifting the occurrence of the policy forward by one year, and the estimation result indicates that the placebo test passes in Table 8 column (4).
 |
Table 8 The Estimation of Dynamic DID and Robustness Check |
Discussion
The Policy Implications of HPAP on Poverty Population and Health Decline
From the perspective of cost–benefit analysis of poverty reduction policy, the implementation of HPAP reduces the poverty vulnerability of poor rural residents, and also alleviates the health decline of poor rural residents. The HPAP generates the policy benefits of anti-poverty goal. The important reasons for this may stem from the following three aspects: First, the implementation of HPAP adequately promotes the healthcare utilization for the rural poor, especially in physical examination and inpatient care. Although HPAP does not significantly promote the healthcare utilization of outpatient care in the policy evaluation of our study, HPAP can adequately reduce outpatient medical cost, whether total medical expenditures or out-of-pocket payments in the past month or the last time. The previous literature for evaluating NCMS has concluded that although NCMS has a significant effect on reducing the inpatient care cost for critical illnesses, rural residents who are impoverished by disease suffer from long-term chronic illnesses,39 and realizing that outpatient costs can be effectively reduced is the key to addressing poverty due to illness.15,40 Second, HPAP significantly promotes the inpatient care utilization and reduces out-of-pocket (OOP) payments for hospitalization, fully releasing the potential demand for healthcare services among the rural poor. The promotion of physical examination also shows that the HPAP raises the health expectations and awareness of the rural poor residents in terms of investment in their health and leads to an increase in the behavior of self-treatment. Third, rural residents often went to tertiary general hospitals in large cities for treatment of major diseases, with indirect costs in transportation, accommodation and loss of income from the labor of family members who cared for the sick, which resulted in more poor rural families being excluded from the medical service system. The important initiative of the HPAP is to allocate medical resource equity to impoverished areas in a policy-leaning manner, to improve the capacity of healthcare services in impoverished areas and the construction of medical infrastructures, and to establish a working mechanism for connecting tertiary-level hospitals in developed areas with county-level hospitals in impoverished areas for improving the quality of healthcare services in impoverished areas. All of these policy measures have greatly enhanced the accessibility of health care in impoverished areas of the countryside.
Reflections on Policy Impact of Mechanisms
Although our study of policy evaluation confirms that HPAP can significantly reduce the poverty vulnerability of the rural poor residents and mitigate health decline, and that poverty alleviation can also have indirect policy effects by promoting healthcare utilization (physical examination and inpatient care), we remain cautious about the policy evaluation’s conclusions.
The poverty reducing effects of HPAP exist (both direct and indirect policy effects), but the economic significance of the HPAP policy effects is to some extent limited. The government is investing large amounts of financial economic resources in upgrading the strength of health insurance protection for the rural resident and the ability of medical institutions to provide healthcare services in poor regions. The objective fact is that the rural poor residents in many cases do not have access to information on medical assistance policies (information bias), lack the knowledge to search for a diagnosis treatment plan that matches their medical needs (cognitive bias), and may be disabled or incapable of accessing medical care at home (disabled persons need assistance). Therefore, we should pay attention to the forces that link the rural poor residents to HPAP’s policy measures, such as the introduction of professional social work to provide social support, the working mechanism for matching informal charitable organizations to provide support with formal medical assistance, health education and policy advocacy within the community or village, these measures are likely to greatly enhance the effectiveness of HPAP.
The Policy Implications of HPAP on the Moral Hazard
There is uncertainty in the incidence of disease and in the efficacy of treatment.41 Significant information asymmetry between patients and doctors regarding treatment options for diseases will lead moral hazard. Moral hazard in health insurance has been proven to exist.42–45 Ex post moral hazard, from the demand-side perspective of healthcare services, is a situation in which patients face lower marginal prices for healthcare services when they have health insurance, and therefore financial incentives can lead to overconsumption of healthcare resources. Ex ante moral hazard refers to the fact that after enrollment in health insurance, a participant expects to pay lower marginal costs of health care after an accident, reducing the investment in health (physical examination, prevention, etc.), and elevating behaviors that potentially create health risks (smoking, drinking, etc.). Ex ante moral hazard leads the result of lowering health performance and overconsumption of healthcare resources.45–49
We evaluate the impact of HPAP on the healthcare utilization and healthcare cost of rural poor residents to analysis moral hazard. First, HPAP implements support policy of outpatient care co-payment reimbursement in poor region. The results indicated that HPAP did not significantly increase the outpatient care utilization, but HPAP did significantly reduce the total outpatient care and out-of-pocket (OOP) payments of poor rural residents. Second, the HPAP raises the protection level of basic medical insurance for rural residents by lowering the deductible and increasing the reimbursement rate for inpatient care expenses within the scope of the policy. The results of our study evaluation indicate that HPAP significantly promotes the inpatient care utilization while reducing the actual out-of-pocket expenditures for the last inpatient care, so we believe that HPAP actually promotes to reduce the cost of hospitalization for rural residents. Therefore, the HPAP has the potential possibility for raising ex post moral hazard. Third, we establish a simple analytical framework to identify that point. The first step is to confirm that whether the HPAP has increased the household medical expenditures to represent releasing demand for health care. The second step is to confirm that whether HPAP elicits medical expenditures that crowd out household affordability, and thus whether HPAP triggers households to incur catastrophic health expenditures (for the World Health Organization standards, household medical cost expenditures that represent more than 40% of the household’s affordability6,50). The empirical results indicate that the above two steps are confirmed. The HPAP has not triggered ex-post moral hazard, but rather the release of rural residents’ normal demand for medical services. The evaluation results of our study showed that the HPAP significantly facilitated physical examination and did not significantly increase smoking behavior but reduced drinking behavior to some extent, which may be due to the fact that the consultation process demanded a reduction in drinking behavior. Therefore, HPAP also did not raise ex ante moral hazard. If moral hazard is viewed as an implicit policy cost of HPAP, our analysis suggests that the implementation of HPAP does not incur serious potential policy costs. This has important policy implications for health transformation plan in developing countries aimed at reducing catastrophic health expenditures and reducing the incidence of poverty due to disease.51
Contributions and Limitations
Our study offers several key contributions to the existing literature: First, from the policy benefits perspective: our policy evaluation reveals that the implementation of HPAP effectively reduces poverty vulnerability and mitigates health deterioration. This emphasizes its role in not just short-term poverty alleviation but also its significance in providing long-term poverty relief. While the Chinese government departments have attempted to explore the possibility for a long-term mechanism of HPAP, our research underscores its sustained policy benefits. This offers a robust empirical basis, suggesting that HPAP could be adopted as a long-term strategy not only for China but also for other nations grappling with poverty. Second, for the implicit policy cost: prior research has not adequately addressed the potential implicit costs of HPAP, specifically its impact on moral hazard. By assessing the effect of HPAP on healthcare utilization and health cost, our findings suggest that HPAP does not introduce substantial hidden policy costs. Third, for the data and methodology: comparing to prior research which predominantly relied on localized city or provincial data,23–25 we utilize the nationally representative CHARLS data to evaluate the policy implications of HPAP. This strengthens the external validity of our empirical findings. Further, our dynamic policy effect estimation and placebo tests reinforce the internal validity of our study’s conclusions.
One limitation to note is the data availability. The most recent CHARLS data available extend only up to 2018. Although the four waves data allow us to test the parallel trend hypothesis pre-policy implementation, our evaluation of the dynamic policy effect of HPAP is confined to a single year. We recognize this constraint and anticipate that future releases with more extended tracking data will provide a more comprehensive evaluation of HPAP’s dynamic impacts.
Conclusion
The implementation of HPAP policy markedly diminishes poverty vulnerability and curtails health deterioration among rural inhabitants. Furthermore, HPAP augments the utilization of healthcare services, such as physical examinations and inpatient care, due to the demand release instead of the ex ante or ex post moral hazards.
Abbreviations
HPAP, Health Poverty Alleviation Project; NCMS, New Rural Cooperative Medical System; CII, Critical Illness Insurance; URBMI, Urban Resident Basic Medical Insurance; URRBMI, Urban-Rural Resident Basic Medical Insurance; Dibao, minimum subsistence allowance (Cash transfer programs for the poor in China); DID, difference-in-difference; FGLS, feasible generalized least squares; VEP, vulnerability as expected poverty; CHE, catastrophic health expenditure; OOP, out-of-pocket payments.
Data Sharing Statement
Publicly available datasets were analyzed in this study. These data can be found here: http://charls.pku.edu.cn/.
Ethics Approval and Informed Consent
We used CHARLS data for academic research, and the Ethical Approval reference citation is from 1.2 Ethical Approval in the 2018 User Guide of CHARLS with the following detail information. “Ethical approval for all the CHARLS waves was granted from the Institutional Review Board at Peking University. The IRB approval number for the main household survey, including anthropometrics, is IRB00001052-11015; the IRB approval number for biomarker collection, was IRB00001052-11014.”
Consent for Publication
All authors have agreed to the article’s content and that the manuscript conforms to the journal’s policies.
Acknowledgments
We are very grateful to Prof. Hua Li, from the School of Public Economics and Administration, Shanghai University of Finance and Economics, for insightful suggestions.
Funding
This study was supported by the grants of the National Social Science Fund of China, (Grant Number: 19CRK003), People’s Republic of China, Grant Recipient: Zhipeng Li.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wagstaff A, Flores G, Hsu J, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Health. 2018;6(2):e169–e179. doi:10.1016/S2214-109X(17)30429-1
2. van Doorslaer E, O’Donnell O, Rannan‐Eliya RP, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16(11):1159–1184. doi:10.1002/hec.1209
3. Wagstaff A. The economic consequences of health shocks: evidence from Vietnam. J Health Econ. 2007;26(1):82–100. doi:10.1016/j.jhealeco.2006.07.001
4. Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. 2003;12(11):921–934. doi:10.1002/hec.776
5. Wang H, Zhang L, Hsiao W. Ill health and its potential influence on household consumptions in rural China. Health Policy. 2006;78(2–3):167–177. doi:10.1016/j.healthpol.2005.09.008
6. Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362(9378):111–117. doi:10.1016/s0140-6736(03)13861-5
7. Xinhua News Agency. Nearly half of the poor people have been impoverished due to illness. China initiated relevant investigation work. The State Council The People’s Republic of China. Available from: https://www.gov.cn/xinwen/2016-04/28/content_5068915.htm.
8. Wang P Implementation of the Health Poverty Alleviation Project Preventing poverty caused by illness from returning to poverty. People’s Daily Online; August 09, 2023. Available from: http://health.people.com.cn/n1/2017/0321/c14739-29157995.html.
9. Zhou Y, Guo Y, Liu Y. Health, income and poverty: evidence from China’s rural household survey. Int J Equity Health. 2020;19(1):36. doi:10.1186/s12939-020-1121-0
10. Lei X, Lin W. The new cooperative medical scheme in rural China: does more coverage mean more service and better health? Health Econ. 2009;18(Suppl S2):S25–46. doi:10.1002/hec.1501
11. Wang N, Xu J, Ma M, et al. Targeting vulnerable groups of health poverty alleviation in rural China- what is the role of the New Rural Cooperative Medical Scheme for the middle age and elderly population? Int J Equity Health. 2020;19(1):161. doi:10.1186/s12939-020-01236-x
12. Babiarz KS, Miller G, Yi H, Zhang L, Rozelle S. China’s new cooperative medical scheme improved finances of township health centers but not the number of patients served. Health Aff (Millwood). 2012;31(5):1065–1074. doi:10.1377/hlthaff.2010.1311
13. Wagstaff A, Lindelow M, Jun G, Ling X, Juncheng Q. Extending health insurance to the rural population: an impact evaluation of China’s new cooperative medical scheme. J Health Econ. 2009;28(1):1–19. doi:10.1016/j.jhealeco.2008.10.007
14. Yi H, Zhang L, Singer K, Rozelle S, Atlas S. Health insurance and catastrophic illness: a report on the New Cooperative Medical System in rural China. Health Econ. 2009;18 Suppl 2:S119–27. doi:10.1002/hec.1510.
15. Yip W, Hsiao WC. Non-evidence-based policy: how effective is China’s new cooperative medical scheme in reducing medical impoverishment? Soc Sci Med. 2009;68(2):201–209. doi:10.1016/j.socscimed.2008.09.066
16. You X, Kobayashi Y. The new cooperative medical scheme in China. Health Policy. 2009;91(1):1–9. doi:10.1016/j.healthpol.2008.11.012
17. Meng Q, Fang H, Liu X, Yuan B, Xu J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. 2015;386(10002):1484–1492. doi:10.1016/S0140-6736(15)00342-6
18. Tang S, Yao L, Ye C, et al. Can health service equity alleviate the health expenditure poverty of Chinese patients? Evidence from the CFPS and China health statistics yearbook. BMC Health Serv Res. 2021;21(1):718. doi:10.1186/s12913-021-06675-y
19. Zou Q, He X, Li Z, Xu W, Zhang L. The effects of poverty reduction policy on health services utilization among the rural poor: a quasi-experimental study in central and western rural China. Int J Equity Health. 2019;18(1):186. doi:10.1186/s12939-019-1099-7
20. Zeng W, Zhao P, Zhao Y, Saddique R. The multidimensional relative poverty of rural older adults in China and the effect of the health poverty alleviation policy. Front Public Health. 2022;10:793673. doi:10.3389/fpubh.2022.793673
21. Chen C, Pan J. The effect of the health poverty alleviation project on financial risk protection for rural residents: evidence from Chishui City, China. Int J Equity Health. 2019;18(1):79. doi:10.1186/s12939-019-0982-6
22. Chen C, Chen T, Pan J. Effect of health poverty alleviation project on the economic burden of disease among poor households: empirical evidence from Sichuan Province. Sichuan Da Xue Xue Bao Yi Xue Ban. 2023;54(2):393–399. doi:10.12182/20230360105
23. Lu J, Zhang M, Zhang J, Xu C, Cheng B. Can health poverty alleviation project reduce the economic vulnerability of poor households? Evidence from Chifeng City, China. Comput Ind Eng. 2021;162:107762. doi:10.1016/j.cie.2021.107762
24. Xu L, Wei C, Wang J. Effects of and problems in health poverty alleviation program in Shandong province: 2015 – 2017. Chin J Public Health. 2019;35(9):1110–1113. doi:10.11847/zgggws1123579
25. Zhang X, Luo Y, Chen W, Huang J. Relative acquisition evaluation of health poverty alleviation project: a quantitative study of data from different regions of China. BMC Public Health. 2022;22(1):2204. doi:10.1186/s12889-022-14703-7
26. Chaudhuri S, Jalan J, Suryahadi A Assessing household vulnerability to poverty from cross-sectional data: a methodology and estimates from Indonesia*. Columbia University Discussion Paper; 2002:1–25.
27. Günther I, Harttgen K. Estimating households vulnerability to idiosyncratic and covariate shocks: a novel method applied in Madagascar. World Dev. 2009;37(7):1222–1234. doi:10.1016/j.worlddev.2008.11.006
28. Cunningham WV, Maloney WF. Measuring vulnerability: who su ered in the 1995 Mexican crisis; 2000.
29. Glewwe P, Hall G. Are some groups more vulnerable to macroeconomic shocks than others? Hypothesis tests based on panel data from Peru. J Dev Econ. 1998;56(1):181–206. doi:10.1016/S0304-3878(98)00058-3
30. Pritchett L, Suryahadi A, Sumarto S. Quantifying vulnerability to poverty: a proposed measure, applied to Indonesia; 2000.
31. Angelillo N. Vulnerability to poverty in China: a subjective poverty line approach. J Chin Econ Bus Stud. 2014;12(4):315–331. doi:10.1080/14765284.2014.952512
32. Amemiya T. The maximum likelihood and the nonlinear three-stage least squares estimator in the general nonlinear simultaneous equation model. Econometrica. 1977;45(4):955–968. doi:10.2307/1912684
33. Pan J, Lei X, Liu GG. Health insurance and health status: exploring the causal effect from a policy intervention. Health Econ. 2016;25(11):1389–1402. doi:10.1002/hec.3225
34. Zhou Q, He Q, Eggleston K, Liu GG. Urban-rural health insurance integration in China: impact on health care utilization, financial risk protection, and health status. Appl Econ. 2022;54(22):2491–2509. doi:10.1080/00036846.2021.1998323
35. Katz E. Bias in conditional and unconditional fixed effects logit estimation. Political Analysis. 2001;9(4):379–384. doi:10.1093/oxfordjournals.pan.a004876
36. von Hippel PT, Workman J. From Kindergarten through second grade, U.S. children’s obesity prevalence grows only during summer vacations. Obesity. 2016;24(11):2296–2300. doi:10.1002/oby.21613
37. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi:10.1037//0022-3514.51.6.1173
38. Judd CM, Kenny DA. Process analysis: estimating mediation in treatment evaluations. Evaluation Review. 1981;5(5):602–619. doi:10.1177/0193841x8100500502
39. Abegunde DO, Stanciole AE. The economic impact of chronic diseases: how do households respond to shocks? Evidence from Russia. Soc Sci Med. 2008;66(11):2296–2307. doi:10.1016/j.socscimed.2008.01.041
40. Miao Y, Gu J, Zhang L, He R, Sandeep S, Wu J. Improving the performance of social health insurance system through increasing outpatient expenditure reimbursement ratio: a quasi-experimental evaluation study from rural China. Int J Equity Health. 2018;17(1):89. doi:10.1186/s12939-018-0799-8
41. Arrow KJ. Uncertainty and the welfare economics of medical care: reply (the implications of transaction costs and adjustment lags). Am Econ Rev. 1965;55(1/2):154–158.
42. Einav L, Finkelstein A. Moral hazard in health insurance: what we know and how we know it. J Eur Econ Assoc. 2018;16(4):957–982. doi:10.1093/jeea/jvy017
43. Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS. Health insurance and the demand for medical care: evidence from a randomized experiment. Am Econ Rev. 1987;77(3):251–277.
44. Riphahn RT, Wambach A, Million A. Incentive effects in the demand for health care: a bivariate panel count data estimation. J Appl Econ. 2003;18(4):387–405.
45. Breyer F, Haufler A. Health care reform: separating insurance from income redistribution. Int Tax Public Finance. 2000;7(4):445–461. doi:10.1023/A:1008773103834
46. Dave D, Kaestner R. Health insurance and ex ante moral hazard: evidence from Medicare. Int J Health Care Finance Econ. 2009;9(4):367–390. doi:10.1007/s10754-009-9056-4
47. Ehrlich I, Becker GS. Market insurance, self-insurance, and self-protection. J Political Econ. 1972;80(4):623–648. doi:10.1086/259916
48. Pauly MV. The economics of Moral Hazard: comment. Parasitology. 1968;58(3):531–537. [The American Economic Review]. doi:10.1017/s0031182000028833
49. Zweifel P, Manning WG. Chapter 8 - Moral Hazard and consumer incentives in health care* *The authors wish to thank Andrew Jones, Joe Newhouse, Edward Norton, and Wynand van de Ven for excellent suggestions and criticisms. In: Culyer AJ, Newhouse JP, editors. Handbook of Health Economics. Elsevier. 2000:409–459.
50. Xu K, Evans DB, Kadama P, et al. Understanding the impact of eliminating user fees: utilization and catastrophic health expenditures in Uganda. Soc Sci Med. 2006;62(4):866–876. doi:10.1016/j.socscimed.2005.07.004
51. Nemati E, Khezri A, Nosratnejad S. The study of out-of-pocket payment and the exposure of households with catastrophic health expenditures following the health transformation plan in Iran. Risk Manag Healthc Policy. 2020;13:1677–1685. doi:10.2147/RMHP.S264943
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.