Back to Journals » International Journal of General Medicine » Volume 9
Health in a fragile state: a five-year review of mortality patterns and trends at Somalia’s Banadir Hospital
Authors Kulane A, Sematimba D, Mohamed L, H Ali A, Lu X
Received 23 March 2016
Accepted for publication 27 May 2016
Published 31 August 2016 Volume 2016:9 Pages 303—310
DOI https://doi.org/10.2147/IJGM.S109024
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Asli Kulane,1 Douglas Sematimba,1 Lul M Mohamed,2 Abdirashid H Ali,2 Xin Lu1,3,4
1Department of Public Health Sciences, Karolinska Institutet, Stockholm, Sweden; 2Women and Child Care Section, Banadir Maternity & Children Hospital, Mogadishu, Somalia; 3College of Information System and Management, National University of Defense Technology, Changsha, People’s Republic of China; 4Flowminder Foundation, Stockholm, Sweden
Background: The recurrent civil conflict in Somalia has impeded progress toward improving health and health care, with lack of data and poor performance of health indicators. This study aimed at making inference about Banadir region by exploring morbidity and mortality trends at Banadir Hospital. This is one of the few functional hospitals during war.
Methods: A retrospective analysis was conducted with data collected at Banadir Hospital for the period of January 2008–December 2012. The data were aggregated from patient records and summarized on a morbidity and mortality surveillance form with respect to age groups and stratified by sex. The main outcome was the number of patients that died in the hospital. Chi-square tests were used to evaluate the association between sex and hospital mortality.
Results: Conditions of infectious origin were the major presentations at the hospital. The year 2011 recorded the highest number of cases of diarrhea and mortality due to diarrhea. The stillbirth rate declined during the study period from 272 to 48 stillbirths per 1,000 live births by 2012. The sum of total cases that were attended to at the hospital by the end of 2012 was four times the number at the baseline year of the study in 2008; however, the overall mortality rate among those admitted declined between 2008 and 2012.
Conclusion: There was reduction in patient mortality at the hospital over the study period. Data from Banadir Hospital are consistent with findings from Banadir region and could give credible public health reflections for the region given the lack of data on a population level.
Keywords: Banadir Hospital, Somalia, hospital mortality, sex, health indicators
Background
Somalia, the easternmost nation in the Horn of Africa,1 is classified as a fragile state. The recurrent civil conflict for over 20 years has impeded progress toward improving health care in Somalia.2 Its capital Mogadishu has been a haven for armed gangs, Islamic militants, and pirates, and for more than two decades, the country has been characterized by insecurity and outbreaks of hunger and inadequate access to basic needs and services.3 According to a recent United Nations Population Fund report, Somalia’s population stands at 12.3 million people with 45.6% of its people <15 years of age.4 It is a youthful population, with a growth rate of 2.8%, which is among the highest in the world.5 On average, every woman bears 6.6 children6 and each household in Somalia has a mean of 5.9 persons.4
The current insecurity has undermined the impact of humanitarian assistance in Somalia, a country where half of the population is dependent on health relief and food aid. The government has been unable to implement the rule of law, and external aid including medical supplies constantly faces the threat of diversion.7 The increase and continuous influx of injured people has created conflict of interest for health care resources and prioritization of allocating funds. This precedent has created a gap in birth and death registration. Monitoring of progress in the public health arena has deteriorated, hence the need to provide progressive assessment of health outcomes. Since 2008, health reports and disease surveillance information have been scanty in Somalia. Demographic surveillance and birth and death registration systems have come to a standstill, and this limits tracking of progress of health indicators. Through the Multiple Indicator Cluster Survey, the United Nations International Children’s Fund established a platform to monitor child and maternal indicators; however, this was only possible until 2006.8 There has been a census recently; however, there is no Demographic and Health Surveillance data which are informative about the county’s health indicators.
Banadir region is the most populous among the 18 prewar regions of Somalia. It is mainly urban with a population of 1.6 million people, and it had the highest number of internally displaced persons in the country by 2014.4 Banadir Hospital,9 also known as the only national referral hospital in Somalia, has since its establishment been the center of health care delivery in Mogadishu. The hospital comprises both maternity and pediatric departments where mothers and children are treated, respectively; however its emergency department offers routine medical and surgical services.
In this article, our primary objective was to explore morbidity and mortality patterns of the presenting conditions in the different units at the hospital such that an overview of Somalia can be inferred. We also explore whether sex has an association with these outcomes. Sex is a multidimensional social construct10 and investigation of this precedent would provide an insight into health outcomes for males in a male-dominated community at war. The Gender Inequality Index11 for Somalia is 0.776 (with a maximum of 1, meaning complete inequality), which is the fourth highest position globally,12 and studies have shown that Gender Inequality Index is positively associated with under-5 mortality rates.13 We also highlight the hospital’s performance, gaps in management, and progress made during this study period.
Data and methods
Study design and setting
This study was done as a retrospective analysis of collected hospital data. Banadir Hospital is a teaching hospital located in the Wadajir district of Mogadishu in Somalia. It consists of four main sections: a pediatric section, a maternity section, a laboratory, and a section for general medicine with a bed capacity of 700. The hospital offers medical and surgical services and also voluntary counselling and testing (VCT) for human immunodeficiency virus (HIV), prevention of mother-to-child transmission (PMTCT),14 and the expanded program on immunization (EPI) services.15 Patients are usually admitted through the Out-Patient Department; however, emergencies are received at the Accident and Emergency unit. Surgical services are provided at the medical section. Admission and medicines are free, but laboratory tests and X-ray services are priced. The hospital is mainly funded by nongovernmental organizations, and they equally provide training to staff including doctors, nurses, and nurses’ assistants.
Data collection
Data were collected between January 2008 and December 2012. All patients that were diagnosed and attended to at the hospital were included in the study. Patient consent was not required as this was aggregated data that was anonymous and had no patient identifying information. For 5 years, aggregated data were obtained from patients’ records and it included age (dichotomized as <5 or >5 years), sex, their presenting diagnosis, and outcomes. Diagnoses were made by the doctors who attended to the patients in each unit in accordance with Somalia’s clinical guidelines and also laboratory confirmation. Data completeness were not ascertained; however, data of all patients treated at the hospital were recorded. Annual data were compiled into a report and recorded on a morbidity and surveillance form. This was recorded in Excel files for the 5-year period. Total number of admissions, discharges, and deaths were also compiled for every month.
Data obtained from the maternity ward included numbers of live births and stillbirths, deliveries, and cases of tetanus. Data from the pediatric section and the laboratory were also obtained. Data on mortality were also obtained from death certificates that are issued daily. Patients that died before diagnosis were diagnosed through post mortem done at the hospital by hospital staff, and those that lacked a diagnosis were included in a category of “others”. Information from patients’ files was summarized daily by persons in charge of the wards. This data were compiled weekly and monthly figures were compiled using the mortality and morbidity surveillance form by the data manager of the hospital. Proofreading to ascertain correct figures was done for the data collected from all the respective units for quality control.
Ethical clearance
Ethical clearance for the study was obtained from the staff in charge of hospital since the hospital has no ethics review board. Study protocol followed the principles outlined in the Declaration of Helsinki.
Data management and analysis
Data obtained during the 5 years were summarized according to the presented conditions with respect to age groups and stratified by sex. The main outcome indicator was the number of patients that died in the hospital. Univariate analyses were carried out to examine the association between sex and mortality. In these analyses, chi-square tests were used. A two-tailed P-value of 0.1 or less was considered to be significant. Crude odds ratios (CORs) were obtained for years in which outcomes were significantly associated with sex.
Results
Major diagnoses across all age groups included uncomplicated malaria, acute watery diarrhea, anemia, presence of intestinal parasites, and urinary tract infection (Table 1). The main diagnoses among children age <5 years were malaria, acute watery diarrhea, and respiratory tract infections. Meningitis, tetanus, whooping cough, and conjunctivitis presented the least cases during the study period. There was an exponential increase in measles cases every other year and a decrease in the year that followed, by 2012.The reported number of patients with sexually transmitted diseases (STDs) almost doubled each year making a sixfold increase by 2012. These cases were, however, reported only among girls >5 years of age. The percentage of complicated cases among the cases of malaria that presented reduced from 30% to 20% by 2012. Trauma cases reported increased across the study period with a higher number of males than females across the study period.
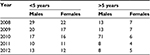
Between 2008 and 2010, the number of cases at the diarrhea treatment center declined (Figure 1). There was an exponential increase from September 2010 to November 2011 and cases there after reduced gradually toward the end of 2012. Maximum numbers (1,485) were reported in August 2011. Monthly reporting of cases throughout the study period indicated that cases were higher between April and August each study year. Mortality due to diarrhea followed a similar pattern in both age groups (Table 2). Between 2008 and 2009, mortality declined in both age groups and increased between 2009 and 2011. There was a decline in mortality in 2012.
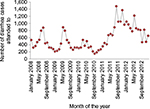  | Figure 1 Number of diarrhea cases by month attended to at the diarrhea treatment center from January 2008 to December 2012. |
  | Table 2 Diarrhea mortality rates per 1,000 among patients admitted to the pediatric unit, <5 and >5 years in males and females Note: Mortality = (Total deaths/Total cases) × 1,000. |
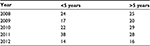
The number of live births at Banadir Hospital increased between 2008 and 2012; however, the number of stillbirths remained constant. The ratio of stillbirths to live births therefore declined over the study period (Figure 2). There was a consistent decline in the rate of stillbirths from 272 (per 1,000 live births) in 2008 to 102 in 2009. This reduced further to 71, 85, and 48 in 2010, 2011, and 2012, respectively. Death from neonatal tetanus stagnated at a mean rate of 27% for all the cases of neonatal tetanus presented.
  | Figure 2 Number and percentage of live births compared to stillbirths delivered at Banadir Hospital between 2008 and 2012. |
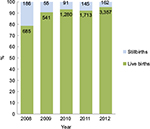
The sum of total cases that were attended to at the hospital by the end of 2012 was four times the number at the baseline year of the study in 2008 (Figure 3), an increase from 15,324 to 64,588. The overall mortality rate among those admitted declined between 2008 and 2012 (Table 3). At a significant level of 0.1, however, mortality in the age group >5 years was consistently associated with sex across the study period (Table 4). The odds of dying for males compared to females in the age group >5 years were as follows: COR =1.98 (95% confidence interval [CI]: 0.9–4.3, P<0.1) in 2008; COR =1.85 (95% CI: 0.9–3.7, P<0.1) in 2009; COR =1.80 (95% CI: 0.8–3.7, P<0.1) in 2010; COR =1.77 (95% CI: 1.0–3.1, P<0.1) in 2011; and COR =1.52 (95% CI: 1.1–2.1, P<0.1) in 2012. Under-5 mortality was not consistently associated with the sex.
  | Figure 3 Number of patient admissions by month at Banadir Hospital from January 2009 to December 2012. |
  | Table 3 Mortality rates per 1,000 among patients admitted to hospital, <5 and >5 years in males and females Note: Mortality = (Total deaths/Total cases) × 1,000. |
Discussion
Disease patterns
Given the lack of data on a population level, this analysis aimed at understanding the patterns of conditions presented at Banadir Hospital in order to make inference and conclusions about the general health status of Banadir region. It is evident from the results that malaria, acute watery diarrhea, and respiratory tract infections dominated the continuum of causes of admissions despite the integrated community case management, a result that is consistent with World Health Organization findings.16 Although measles cases were on the rise, current data indicates that Banadir region is a high endemic area and findings could not be generalized to the entire population.17 Measles is one of the leading killers of young children particularly in the malnourished, a situation that is consistent with findings in Somalia. Measles immunization coverage remains low with less than one-third of children under 1 year vaccinated against measles.17
According to the African Union Mission in Somalia,18 cases of HIV are on the rise with low case detection due to the absence of diagnostics and stigma from the community.18 This could explain the annual doubling of STD cases although the rate of STDs was normal. Absence of STD cases among boys age >5 years, however, shows a gap in case detection since females are usually investigated at the maternity section. The reduction in the proportion of complicated cases of malaria indicates that there is improvement in early case detection and diagnosis for malaria within the catchment area for Banadir Hospital; however, data on case fatality were not available.
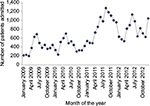
At the beginning of 2008, the gradual increase in the number of patients at Banadir Hospital was consistent with the country’s population increment.19 This trend; however, changed in mid-2010 (Figure 4) with an increase in the rate of hospitalization in relation to the population. This can be explained by the famine and hunger associated illnesses that the country faced during that time. Between 2010 and 2012, the United Nations reported the worst drought that ever hit Somalia in the last 60 years.20 The increased rate of hospitalization also implies that the hospital provides much more care now than before.
  | Figure 4 Comparison between changes in Somalia’s population in relation to the increase in the number of patients attended to in the hospital. Notes: (A) Somalia’s population;19 (B) admissions at Banadir Hospital. |
There was a clear relation between the annual rainfall pattern and that of diarrhea cases.21 In 2012, Médecins Sans Frontières documented the increased cases of acute watery diarrhea in southern Somalia,22 in line with findings of this study. The increase in cases observed between 2011 and 2012 could also be attributed to the cholera outbreak in the region. This was essentially due to poor sanitation, shortage of safe water, and overcrowding, which were exacerbated by the seasonal flooding of the Shebelle River.
A recent report by World Health Organization shows that trauma cases are on the rise,17 which has been highlighted in findings at the hospital. Violence and conflict continue to take a heavy toll on civilians in Somalia with escalating numbers of weapon-related injuries. Despite the conflict, the cause of trauma cases among children age <5 years needs to be investigated. The role of males in the civil strife has led to the increased numbers of trauma cases among males compared to the females.
There was no consistent association between sex and under-5 mortality in this study in contrast to previous studies.13,23 These studies found that male sex was not an independent predictor of mortality among hospitalized children <5 years of age in the presence of risk factors like age, associated comorbidities, and severity of respective illnesses.24 For the age group >5 years, sex was consistently associated with higher mortality among males. It was not possible to highlight possible risk factors because of the nature of the data. Although studies have shown that conflict overshadows the social and sex issues, rendering them “secondary” to the primary concern of safety and survival,25 further research in this area would yield better explanations. It is possible that males presented with more critical conditions than females; however, this could not be ascertained from the study data.
Health system implications
The overall reduction in hospital mortality despite the increased number of patients attended to over the years is indicative of the improvement in performance of the hospital. Although the World Bank reports an under-5 mortality rate of 146 in Somalia,26 this study was not able to highlight changes in mortality rate over time. It is important to reflect on the fact that the overall hospital under-5 mortality among admitted cases has reduced and to highlight the progress that has been made. The increase in the number of patients can also be attributed to the observed number of live births that was much higher than the death rate. The increase in live births at the hospital with no significant increase in stillbirths could explain the increase in the region’s population and also an increase in the number of patients attended to at the hospital during the study period. Somalia’s birth rate stands at 41 births per 1,000 population and the death rate reduced from 15.9 to 13.9 deaths per 1,000 population despite the fact that the country is at war.27 Owing to this, information from Banadir Hospital could be essential in evaluating health system performance and provide reliable facts on planning for this catchment area. According to the Performance Assessment Tool for Quality Improvement in Hospitals model, the increase in the number of patients attended to at the hospital with reduction in mortality is indicative of positive performance.28
Limitations
The study involved a large data set for making good comparisons and detecting trends over time, for the first time in 2 decades of war; however, the data were aggregated making it hard to perform detailed analyses and making more concrete conclusions. Categories had been prefixed before the data were collected, which could not allow flexibility in the data analysis. Analyzing trends in this context was not possible. Disease-specific mortality was not possible in the study, which would have provided a better analysis of conditions. There may have been a selection of more serious cases being admitted to the hospital, which may also distort the results; however, sufficient information on the primary health care system in this war setting was not readily available to back up some of our arguments.
Conclusion
Diseases of infectious origin dominated the continuum of cases attended to at the hospital, and hospital-based mortality reduced across the study period. Data from Banadir Hospital were consistent with findings from Banadir region although figures from hospital-based studies are higher than those in the general population. This data can be used to describe the health status of the community in the absence of credible demographic surveillance in Banadir region as earlier stated. Hospital-based studies would work as early surveillance tools in a sentinel site, since hospital cases may be observed to increase before the outbreak. Consistent use of hospital data could give credible public health reflections for Banadir region.
There was an association between mortality in the age group >5 years and sex with a protective advantage for females compared to males. Our results only reflect that there is a difference in outcome of patient admissions with respect to sex in the age group >5 years but do not show that the female sex is positioned better than the male. The situation of war and increased risk of injury for males should be put into context in this study. There are better outcomes at the hospital with progressive improvement during the study period; however, these outcomes are still low in comparison to global standards.
Acknowledgments
The authors acknowledge the tremendous contribution of the director of Banadir Hospital, who made it possible to carry out this survey despite the tedious process of compiling and obtaining the data. Special thanks to Professor Bo Burström for his wise counsel. Funding was obtained from the Public Health Sciences’ Department Research Grant of 2013 at Karolinska Institutet.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
WorldAtlas. Somalia: description [location and images of Somalia]; 2015 [cited September 5, 2015]. Available from: http://www.worldatlas.com/webimage/countrys/africa/so.htm. Accessed September 5, 2015. | ||
Guha-Sapir D, Ratnayake R. Consequences of ongoing civil conflict in Somalia: evidence for public health responses. PLoS One. 2009;6(8):e1000108. | ||
Maxwell D, Fitzpatrick M. The 2011 Somalia famine: context, causes, and complications. Glob Food Sec. 2012;1(1):5–12. | ||
United Nations Population Fund. Population Estimation Survey 2014. Nairobi: United Nations Population Fund; 2014. Available from: http://somalia.unfpa.org/sites/arabstates/files/pub-pdf/Population-Estimation-Survey-of-Somalia-PESS-2013-2014.pdf. Accessed September 5, 2015. | ||
World Health Organization. Somalia [map and statistics]; 2015 [cited September 4, 2015]. Available from: http://www.who.int/countries/som/en/. Accessed September 4, 2015. | ||
Gapminder. GapMinder World. Stockholm, Sweden: GapMinder; 2013 [cited September 15, 2015]. Available from: http://www.gapminder.org/world. Accessed September 15, 2015. | ||
Childress S. UN probes if Somalia’s contractors are diverting aid, funding rebels; 2009 [updated September 16, 2009]. The Wall Street Journal. Available from: http://www.wsj.com/articles/SB125305726840513913. Accessed September 15, 2015. | ||
United Nations International Children’s Fund. Somalia – Multiple Indicator Cluster Survey 2006. United Nations International Children’s Fund Somalia Support Center; 2006 [cited September 10, 2015]. Available from: http://www.childinfo.org/files/MICS3_Somalia_FinalReport_2006_eng.pdf. | ||
Banadir Hospital. About Banadir Hospital [services offered by the hospital]. Mogadishu, Somalia: Ministy of Health; 2015 [cited September 5, 2015]. Available from: http://banadirhospital.com/. Accessed September 5, 2015. | ||
World Health Organization. Health topics – gender. Available from: http://www.who.int/topics/gender/en/. Accessed September 20, 2015. | ||
UNDP. Human Developments Reports: Gender Inequality Index (GII). Available from: http://hdr.undp.org/en/content/gender-inequality-index-gii. Accessed September 5, 2015. | ||
UNDP-somalia. Gender in Somalia. 2015. Available from: http://www.undp.org/content/dam/rbas/doc/Women’s%20Empowerment/Gender_Somalia.pdf. Accessed September 10, 2015. | ||
Brinda EM, Rajkumar AP, Enemark U. Association between gender inequality index and child mortality rates: a cross-national study of 138 countries. BMC Public Health. 2015;15(1):1–6. | ||
Jennings L, Ong’ech J, Simiyu R, Sirengo M, Kassaye S. Exploring the use of mobile phone technology for the enhancement of the prevention of mother-to-child transmission of HIV program in Nyanza, Kenya: a qualitative study. BMC Public Health. 2013;13:1131. | ||
Fadnes LT, Nankabirwa V, Sommerfelt H, Tylleskar T, Tumwine JK, Engebretsen IM; PROMISE-EBF Study Group. Is vaccination coverage a good indicator of age-appropriate vaccination? A prospective study from Uganda. Vaccine. 2011;29(19):3564–3570. | ||
World Health Organization. Children: reducing mortality – children under the age of 5; 2014 [cited September 15, 2015]. Available from: http://www.who.int/mediacentre/factsheets/fs178/en/. Accessed September 15, 2015. | ||
Ngugi L. WHO Somalia health update. Warwick Centre; UN Avenue, Gigiri: May–June 2014. | ||
African Union Mission in Somalia. HIV infections on the rise in Somalia. AMISOM; 2013 [cited September 16, 2015]. Available from: http://amisom-au.org/so/2014/12/hiv-infections-on-the-rise-in-somalia/. Accessed September 15, 2015. | ||
United Nations. World Population Prospects; 2015 [cited October 7, 2015]. Available from: http://esa.un.org/unpd/wpp/DataQuery/. Accessed October 7, 2015. | ||
Maxwell D, Fitzpatrick M. The 2011 Somalia famine: Context, causes, and complications. Global Food Security. 2012;1(1):5–12. | ||
The World Bank. Somalia. The World Bank; 2015 [cited September 15, 2015]. Available from: http://data.worldbank.org/country/somalia. Accessed September 1, 2015. | ||
Médecins Sans Frontières. Somalia: Responding to Diarrhea in Kismayo [MSF is responding to increased cases of acute watery diarrhea among children and adults in the city of Kismayo in southern Somalia]; 2012 [cited September 16, 2015]. Available from: http://www.doctorswithoutborders.org/news-stories/field-news/somalia-responding-diarrhea-kismayo. Accessed September 10, 2015. | ||
Croce MA, Fabian TC, Malhotra AK, Bee TK, Miller PR. Does gender difference influence outcome? J Trauma. 2002;53(5):889–894. | ||
Crabtree TD, Pelletier SJ, Gleason TG, Pruett TL, Sawyer RG. Gender-dependent differences in outcome after the treatment of infection in hospitalized patients. JAMA. 1999;282(22):2143–2148. | ||
Halperin-Kaddari R, Yadgar Y. Between universal feminism and particular nationalism: politics, religion and gender (in)equality in Israel. Third World Q. 2010;31(6):905–920. | ||
The World Bank. Mortality rate, under-5 (per 1,000). The World Bank; 2015 [cited October 22, 2015]. Available from: http://data.worldbank.org/indicator/SH.DYN.MORT. Accessed October 20, 2015. | ||
CIA fact book-Historical data graphs per year. 2015 [cited September 16, 2015]. Available from: http://www.indexmundi.com/g/g.aspx?v=2224&c=so&l=en. Accessed September 16, 2015. | ||
Veillard J, Champagne F, Klazinga N, Kazandjian V, Arah OA, Guisset AL. A performance assessment framework for hospitals: the WHO regional office for Europe PATH project. Int J Qual Health Care. 2005;17(6):487–496. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


