Back to Journals » International Journal of Women's Health » Volume 15
Gonadotropin Levels and Underlying Diseases in Adolescent With Secondary Amenorrhea
Authors Novina N , Ritonga MA , Yusuf AS
Received 29 March 2023
Accepted for publication 30 August 2023
Published 6 September 2023 Volume 2023:15 Pages 1397—1404
DOI https://doi.org/10.2147/IJWH.S412482
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Elie Al-Chaer
Novina Novina,1 Mulyanusa Amarullah Ritonga,2 Aliyya Salsabila Yusuf3
1Department of Child Health, Faculty of Medicine, Universitas Padjadjaran / Hasan Sadikin General Hospital, Bandung, West Java, Indonesia; 2Department of Obstetrics and Gynecology, Faculty of Medicine, Universitas Padjadjaran / Hasan Sadikin General Hospital, Bandung, West Java, Indonesia; 3Faculty of Medicine, Universitas Padjadjaran, Bandung, West Java, Indonesia
Correspondence: Novina Novina, Department of Child Health, Faculty of Medicine, Universitas Padjadjaran / Hasan Sadikin General Hospital, Jl. Pasteur No. 38 Kel. Pasteur Kec. Sukajadi, Bandung, 40161, Indonesia, Tel/Fax +62 22 2035957, Email [email protected]
Purpose: To provide characteristics and hormonal profiles of secondary amenorrhea cases in adolescent patients treated at Hasan Sadikin General Hospital in Bandung.
Patients and Methods: The study was retrospective in nature and involved the analysis of medical records from 2017 to 2022 for 44 adolescent patients aged 10– 18 who had secondary amenorrhea.
Results: There were 44 adolescents included in this study after excluded 69 adults from 113 secondary amenorrhea cases. The majority of patients were 14– 17 years old (38.63%), in senior high school (45.45%), had started menarche at 11 years old (45.45%), had normal nutritional status (65.91%), and had normal stature (65.91%). The underlying diseases found in most patients were systemic lupus erythematosus (SLE) and tuberculosis. Among the patients, 29 had FSH, LH, and estradiol levels measured. The results of hormonal assays showed a wide range of abnormal serum levels, with normal to low concentrations of FSH and low levels of LH and estradiol. The median (interquartile range) results for FSH, LH, and estradiol were 4.57 (0.64, 90.65), 1.635 (0.06, 55.76), and 24.3 (0.2, 154.71), respectively. Positive significant correlation between FSH and LH (p < 0.01) was found in children with secondary amenorrhea.
Conclusion: Hormonal assay for FSH, LH, and Estradiol showed a wide range of abnormal serum level. Normal to low concentration levels of FSH and low LH and estradiol. The majority of secondary amenorrhea patients are associated with autoimmune disease and infection.
Keywords: adolescent, follicle-stimulating hormone, estradiol, luteinizing hormone, secondary amenorrhea, underlying disease
Introduction
Amenorrhea or loss of the menstrual cycle in adolescents can be divided into primary and secondary amenorrhea. If an adolescent patient does not menstruate until the age of 16 years with secondary sexual development or until the age of 14 years without secondary sexual development, the patient is considered to have primary amenorrhea, whereas secondary amenorrhea occurs in someone with normal menstrual periods but missing menstruation for 3 consecutive months or 6 months without regular menstruation.1 Secondary amenorrhea is a problem affecting 3% to 5% of the female population annually.2 The initial age for women to experience puberty is 8 years old with the secondary sexual development process started by thelarche (breast budding) followed by pubarche (pubic hair development), growth spurt and menstruation being the last developmental process.3
It is common for women within the first two years of menstruation and two years before menopause to experience anovulation and irregular cycle, especially for adolescents experiencing menstrual disorders or amenorrhea.1 Pregnancy, lactation, and menopause are considered psychological causes of amenorrhea. Apart from these three things, amenorrhea can be caused by pathological conditions.4 The most common risk factor and cause of amenorrhea is pregnancy; pregnancy tests are essential for diagnosing amenorrhea. Other factors are stress, weight loss, and excessive physical activity.5
Amenorrhea occurs due to disruptions in the Hypothalamus-Pituitary-Ovarian (HPO) axis. The hypothalamus secretes GnRH that will stimulate the production of Gonadotropins (LH and FSH), leading to the synthesis of follicles and steroids, which subsequently causes sloughing of the endometrium. Disruption of this axis can cause an imbalance in hormone secretion that will lead to amenorrhea. Both primary and secondary amenorrhea have risk factors and causes and can be distinguished from the presence or absence of a history of menstruation. Thus, the causes of amenorrhea can be classified based on the location of the disorder; disorders in the hypothalamus, pituitary, anatomical disorders of the uterus and anovulatory factors.6
Secondary amenorrhea is a concerning issue in some female populations, particularly among adolescents, and thus, requires further attention. However, the lack of understanding regarding the underlying diseases and gonadotropin levels in patients with secondary amenorrhea at Hasan Sadikin hospital has prompted the authors to conduct research on this topic.
Materials and Methods
This is a retrospective analytical study, in which data was collected from the medical records of Hasan Sadikin General Hospital in Bandung during the period of 2017 to 2022. Baseline characteristics including age, education level, age of menarche, nutritional status, underlying diseases, treatment, levels of serum FSH, LH, estradiol, TSH and free T4 were collected. The study design is illustrated in Figure 1. The total sampling method was employed to determine the sample size. Between 2017 and 2022, there were 113 secondary amenorrhea cases which consisted of 44 adolescents aged 10 to 18 years old included in this study after separated 69 adults. Exclusion criteria included incomplete or lost medical records. Subject flow chart is depicted in Figure 2. Hasan Sadikin General Hospital is a top referral hospital in West Java Province. West Java Province has 26 regencies/cities, comprising 17 regencies and 9 cities, with 625 districts and 5877 villages. Hasan Sadikin General Hospital is one of teaching hospitals of Universitas Padjadjaran. This study has been authorized by the Health Research Ethics Committee of Hasan Sadikin General Hospital Bandung under the reference number LB.02.01/X.2.2.1/26349/2021 and conformed to the ethical guidelines of the Declaration of Helsinki.
 |
Figure 1 Study Design. |
 |
Figure 2 Prevalence of secondary amenorrhea patients based on age group and its availability in Hasan Sadikin Hospital’s medical record period 2017–2022. |
The statistical analysis was facilitated using IBM® SPSS® version 26 software for the Windows 10 64-bit operating system and presented in the table. The subjects were anonymized and de-identified before analysis. Variables presented in frequency, percentage, mean, standard deviation and Pearson correlation test were used.
Results
Table 1 presents the most commonly observed age group was 14–16 years old (38.63%), followed by 17–18 years old (38.63%) and 10–13 years old (22.73%). Most of the patients were in Junior and Senior high school, had menarche at 11 years old, normal nutritional status and normal stature. The drug history of the patients was also recorded, with the majority of them having consumed antibiotics (52.27%), while half of the patients (50%) were treated with corticosteroids. Nine patients (20.45%) received chemotherapy agents.
 |
Table 1 Characteristics of Secondary Amenorrhea Patients |
Table 2 presents the most common underlying diseases observed in secondary amenorrhea patients, with Systemic Lupus Erythematosus (36.36%) and Tuberculosis (31.82%) being the two most prevalent conditions.
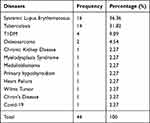 |
Table 2 Underlying Diseases of Secondary Amenorrhea Patients |
Out of 44 patients, only 29 had their hormone levels tested, with 15 individuals not being examined based on physician’s assessment. Table 3 and Table 4 present the gonadotropin and estradiol profiles of the patients. In Table 3, FSH, LH, and Estradiol levels were categorized into low, normal, or high levels based on follicular phase. Table 4 categorizes FSH based on follicular phase and underlying disease. Out of the 29 patients, the majority of FSH hormone levels were found to be normal (41.38%) and low (34.48%). On the other hand, the serum levels of LH and Estradiol were predominantly low, with 58.62% and 51.72% of patients displaying low levels, respectively. Patients with Systemic Lupus Erythematosus (SLE) are distributed across two categories of FSH levels: low and normal. Meanwhile, patients with Tuberculosis are found in all three categories: low, normal, and high FSH levels.
 |
Table 3 Hormonal Profiles of Secondary Amenorrhea Patients |
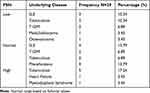 |
Table 4 Patient’s Underlying Disease Based On FSHLevel |
A total of 10 patients with secondary amenorrhea’s level of TSH and fT4 were collected, shown in Table 5. One patient was diagnosed previously with primary hypothyroidism (10%). Most of the patient’s level of TSH and fT4 (90%) were within the normal limit.
 |
Table 5 Thyroid Profiles of Secondary Amenorrhea Patients |
There was a positive significant correlation between FSH and LH (p < 0.01) in adolescent with secondary amenorrhea. However, there was no correlation between estradiol with FSH and LH (p > 0.05) (Table 6).
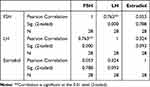 |
Table 6 Correlation Between FSH, LH, Estradiol in Children With Secondary Amenorrhea |
Discussion
It is common for half of the adolescent population to seek consultation within the first two years after menarche due to menstrual problems, which is often associated with the pubertal development process.7 This is attributed to the immaturity of the hypothalamic-pituitary-ovarian axis in adolescent females, leading to frequent menstrual issues.8 For a normal menstrual cycle, regular production of insulin, thyroid, ovarian, adrenal, and hypothalamus hormones is required. Any disruption in these circuits can interfere with the menstrual cycle’s natural rhythm. In addition, endocrine disturbances such as diabetes, thyroid disease, and PCOS can also lead to menstrual problems.9
The study found that the majority of menarche (45.45%) in the adolescent population occurred at the age of 11 years old. This is consistent with a study conducted in Semarang, where the highest age of menarche was also found in 11-year-old children (34%). Earlier age of menarche was 9 years old.10
The study found that the most common underlying disease in secondary amenorrhea patients was SLE (36.36%). It is important to note that out of all cases of SLE, 10–20% are diagnosed as childhood-onset systemic lupus erythematosus (cSLE), and a case series reported that 11% of female cSLE who receive cyclophosphamide (CYC) under 21 years old have a risk of premature ovarian failure. CYC is known to cause gonadal toxicity and premature ovarian failure in adult patients, and although it is considered less common in cSLE patients, it is still a significant risk. Prepubertal children may have less gonadal toxicity since their gonads are in a quiescent stage and less exposed to hazardous medicines.11,12 Additionally, SLE can affect reproductive health even without treatment by CYC.13 While CYC as a chemotherapy agent can cause significant damage in a patient with secondary amenorrhea, SLE patients also have a higher chance of experiencing secondary amenorrhea than a healthy girl. This study reported 16 (36.36%) SLE patients, and 9 (20.45%) underwent chemotherapy treatment due to causes other than SLE.
Tuberculosis (TB) is another common underlying disease observed in patients with secondary amenorrhea, accounting for 31.82% of cases. The incidence of TB among adolescents and young adults aged 10 to 24 was reported to be 1.78 million globally in 2012.14 Non-genital tuberculosis can affect menstrual function through a complex network of interconnected processes involving hypothalamic-pituitary-ovarian function, although the underlying pathophysiology is not yet fully understood. According to several studies, abnormality in menstrual function may occur due to hypo-estrogenic hormone levels.15 For instance, a case report of a girl with disseminated TB showed hypothalamic hypogonadotropic amenorrhea with decreased FSH and LH levels, leading to decreased estrogen production.16
Four patients (9.09%) in this study were diagnosed with type 1 diabetes mellitus, which has been associated with amenorrhea and oligomenorrhea, and further research is needed to confirm this association. Menstrual disorders in diabetic patients may be caused by reduced LH secretion, delay in the positive estrogen loop, and the development of hyperandrogenism.17 Amenorrhea has also been observed in patients with type 2 diabetes, which has been linked to insulin resistance in polycystic ovary syndrome (PCOS).18 In a study, PCOS was found to be associated with IR and other metabolic disorders, although no genetic link has been established.19 Another underlying disease observed in one patient (2.27%) was hypothyroidism, which can increase prolactin levels along with thyrotropin-releasing hormone (TRH). High levels of TRH and hyperprolactinemia in primary hypothyroidism patients can lead to amenorrhea.20 Besides the one individual who had already been diagnosed with hypothyroidism, the thyroid function of the other nine examined patients yielded results within normal limits.
Adolescents commonly experience menstrual irregularities such as hypo menstrual syndrome, dysmenorrhea, and amenorrhea, as found in a study conducted in Ukraine. This study also discovered a significant association between thyroid dysfunction and hypomenorrhea (shortened menstrual bleeding) as well as between thyroid function and amenorrhea.21 Therefore, endocrine problems such as thyroid dysfunction and hyperandrogenism should also be taken into account as potential causes of menstrual irregularities in adolescents.22 However, in this study, limited number of thyroid profile of subjects were checked revealed within normal limit (9 from 10 patients have normal thyroid function). Additionally, chronic kidney disease was identified in 1 (2.27%) patient in this study. While a study conducted in Aceh did not find a relationship between secondary amenorrhea and the duration of therapy for chronic kidney failure, it was found to be more related to disruption of reproductive hormones, uremia syndrome, and psychological factors.23
Although most of the patients in this study had normal nutritional status, a considerable number of patients (18.18%) were severely underweight, and 11.36% were moderately underweight. Children with chronic diseases are more susceptible to malnutrition due to increased caloric requirements, malabsorption, altered nutrient utilization, and limited nutrient availability due to fluid status and feeding tolerance.24 These chronic or diseases can also interfere with linear growth and, in severe cases, lead to growth failure and short stature.25 In fact, 34.09% of the patients in this study were found to have short stature. In addition to the underlying diseases discussed earlier, this study also identified other common chronic conditions in children, including cardiac diseases, malignancy, anemia, and renal disease, which were present in 2.27% of patients.
The hormonal profiles of the patients showed that a majority had abnormal hormone levels, with many showing low levels of LH and estradiol, and some showing low levels of FSH. LH and FSH work together in regulating reproductive function, and low levels of LH in both men and women can indicate various underlying issues such as anorexia, pituitary gland problems, stress, or hypothalamus injury. In cases where LH levels are lower than FSH, it is usually diagnosed as functional hypothalamic amenorrhea. Estradiol is an important hormone for bone health, and its levels are often monitored during therapy to prevent bone loss.26 Hypothalamic amenorrhea might be the underlying cause for most of the patients in this study with chronic diseases. Several theories have postulated chronic or systemic diseases cause nutritional deficiencies resulting in negative energy balance or chronic inflammatory states that lead to functional hypogonadotropic hypogonadism.27
This study was conducted in Central Referral Hospital in West Java Indonesia, which limits its generalizability to other populations and settings. The sample size was also relatively small, which may affect the accuracy and reliability of the results. This study requires a more extensive study, including larger and more diverse samples, to confirm the associations and findings presented in the current study. There may be potential biases or confounding factors in this retrospective study which could affect the study’s findings. The study did not include information on lifestyle factors, such as exercise and diet, which could also impact menstrual irregularities. Finally, the study did not investigate the long-term outcomes of patients, such as the development of osteoporosis or fertility issues.
Conclusion
In conclusion, this study found that the majority of patients with secondary amenorrhea at Hasan Sadikin General Hospital in Bandung had underlying autoimmune diseases or infections. The hormonal laboratory examination of FSH, LH, and estradiol revealed a wide range of abnormal serum levels, with normal to low levels of FSH and low levels of LH and estradiol. Most of the subjects have normal thyroid function. These findings suggest the need for further investigation into the potential causes of secondary amenorrhea in this patient population, as well as the development of appropriate treatment strategies.
Funding
The funding from Universitas Padjadjaran is to cover the article processing charges (APC) for this article which is gratefully acknowledged.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Klein DA, Paradise SL, Reeder RM. Amenorrhea: a systematic approach to diagnosis and management. Am Fam Physician. 2019;100(1):40–48.
2. Jameson JL. Harrison’s endocrinology. In: The Yale Journal of Biology and Medicine.
3. Lacroix AE, Gondal H, Shumway KR, et al. Physiology, menarche. In: StatPearls. StatPearls Publishing; 2022.
4. Rebar R. Evaluation of amenorrhea, anovulation, and abnormal bleeding. South Dartmouth MDText.com, Inc; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279144/.
5. Kafeel H, Rukh R, Zubair A, et al. Prevalence and factors associated with functional secondary amenorrhea. Int J Pharm. 2014;4(1):16–21.
6. Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Williams gynecology. In: Amenorrhea.
7. Montoya JS, Cabezza AH, Rojas OM, Navarrete RC, Keever MÁV. Menstrual disorders in adolescents. Bol Med Hosp Infant Mex. 2012;69(1):63–76.
8. Ali M, Yasmeen T, Naqvi Z, Farooqi R, Khan S. Evaluating underlying endocrine abnormalities in adolescents with menstrual disorders presenting at a tertiary care hospital. Pakistan J Med Heal Sci. 2022;16(4):1079–1082. doi:10.53350/pjmhs221641079
9. Naz MSG, Farahmand M, Dashti S, Tehrani FR. Factors affecting menstrual cycle developmental trajectory in adolescents: a narrative review. Int J Endocrinol Metab. 2022;20(1):e120438. doi:10.5812/ijem.120438
10. Puspitasari R, Udiyono A, Saraswati LD, Ginanjar P. Gambaran usia menarche dini di pada anak sekolah dasar di daerah urban. J Kesehat Masy. 2019;4:4.
11. Harry O, Yasin S, Brunner H. Childhood-onset systemic lupus erythematosus: a review and update. J Pediatr. 2018;196:22–30.e2. doi:10.1016/j.jpeds.2018.01.045
12. Aggarwal A, Srivastava P. Childhood onset systemic lupus erythematosus: how is it different from adult SLE? Int J Rheum Dis. 2014;18(2):182–191. doi:10.1111/1756-185X.12419
13. Knight JH, Howards PP, Pencer JBS, Tsagaris KC, Lim SS. Characteristics related to early secondary amenorrhoea and pregnancy among women diagnosed with systemic lupus erythematosus: an analysis using the GOAL study. Lupus Sci Med. 2016;3(1):1–10. doi:10.1136/lupus-2015-000139
14. Snow KJ, Sismanidis C, Denholm J, Sawyer SM, Graham SM. The incidence of tuberculosis among adolescents and young adults: a global estimate. Eur Respir J. 2018;51(2):1702352. doi:10.1183/13993003.02352-2017
15. Chen Y, Wang J. Amenorrhea in a patient with pulmonary tuberculosis. Thorac Med. 2015;30:321–325.
16. Rosenthal AH, Rothfield LD, Chamorro Dauer L. Disseminated tuberculosis in a healthy adolescent female. Cureus. 2019;11(6):10–14.
17. Rajan A. Type-1 diabetes mellitus and its relation with impairment of female fertility. Acta Sci Nutr Heal. 2019;3(5):210–214.
18. Panidis D, Tziomalos K, Chatzis P, et al. Association between menstrual cycle irregularities and endocrine and metabolic characteristics of the polycystic ovary syndrome. Eur J Endocrinol. 2013;168(2):145–152. doi:10.1530/EJE-12-0655
19. Bogari NM. Genetic construction between polycystic ovarian syndrome and type 2 diabetes. Saudi J Biol Sci. 2020;27(10):2539–2543. doi:10.1016/j.sjbs.2020.05.004
20. Fourman LT, Fazeli PK. Neuroendocrine causes of amenorrhea - an update. J Clin Endocrinol Metab. 2015;100(3):812–824. doi:10.1210/jc.2014-3344
21. Hafiichuk S. Characteristics of puberty period in adolescent girls and major risk factors of menstrual function disorders against the background of endemic goiter. Galician Med J. 2020;27(2):E202029. doi:10.21802/gmj.2020.2.9
22. Rajiwade SR, Sagili H, Soundravally R, Subitha L. Endocrine abnormalities in adolescents with menstrual disorders. J Obstet Gynecol India. 2018;68(1):58–64. doi:10.1007/s13224-017-1035-y
23. Prastiwi Yulianti D, Salwani D. Hubungan lama hemodialisis dengan kejadian amenore sekunder pada pasien gagal ginjal kronik di rsud dr. zainoel abidin Banda aceh dan rsud tgk.chik ditiro sigli. J Ilm Mhs Kedokt Medisia. 2017;2(1):5–11.
24. Larson-Nath C, Goday P. Malnutrition in children with chronic disease. Nutr Clin Pract. 2019;34(3):349–358. doi:10.1002/ncp.10274
25. Albalawi NAS, Alsabah BAB, Alrefaei AY. Short stature in children. Egypt J Hosp Med. 2018;70(2):228–233. doi:10.12816/0043081
26. Gardner DG, Shoback D. Greenspan’s basic & clinical endocrinology. In: Mcgraw-Hill Education.
27. Dwyer AA, Phan-Hug F, Hauschild M, Elowe-Gruau E, Pitteloud N. Hypogonadism in adolescence. Eur J Endocrinol. 2015;173(1):R15–24. doi:10.1530/EJE-14-0947
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
