Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Global Research Trends on the Link Between the Microbiome and COPD: A Bibliometric Analysis
Authors Chen D, Zeng Q, Liu L , Zhou Z, Qi W, Yu S, Zhao L
Received 3 February 2023
Accepted for publication 30 April 2023
Published 5 May 2023 Volume 2023:18 Pages 765—783
DOI https://doi.org/10.2147/COPD.S405310
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Daohong Chen, Qian Zeng, Lu Liu, Ziyang Zhou, Wenchuan Qi, Shuguang Yu, Ling Zhao
Acupuncture and Tuina School, Chengdu University of Traditional Chinese Medicine, Chengdu, People’s Republic of China
Correspondence: Ling Zhao; Shuguang Yu, Acupuncture and Tuina School, Chengdu University of Traditional Chinese Medicine, No. 37, Twelve Bridge Road, Chengdu, Sichuan Province, People’s Republic of China, Email [email protected]; [email protected]
Background: The pathogenesis of chronic obstructive pulmonary disease (COPD) has been studied in relation to the microbiome, providing space for more targeted interventions and new treatments. Numerous papers on the COPD microbiome have been reported in the last 10 years, yet few publications have used bibliometric methods to evaluate this area.
Methods: We searched the Web of Science Core Collection for all original research articles in the field of COPD microbiome from January 2011 to August 2022 and used CiteSpace for visual analysis.
Results: A total of 505 relevant publications were obtained, and the number of global publications in this field is steadily increasing every year, with China and the USA occupying the first two spots in international publications. Imperial College London and the University of Leicester produced the most publications. Brightling C from the UK was the most prolific writer, while Huang Y and Sze M from the USA were first and second among the authors cited. The American Journal of Respiratory and Critical Care Medicine had the highest frequency of citations. The top 10 institutions, cited authors and journals are mostly from the UK and the US. In the ranking of citations, the first article was a paper published by Sze M on changes in the lung tissue’s microbiota in COPD patients. The keywords “exacerbation”, “gut microbiota”, “lung microbiome”, “airway microbiome”, “bacterial colonization”, and “inflammation” were identified as cutting-edge research projects for 2011– 2022.
Conclusion: Based on the visualization results, in the future, we can use the gut–lung axis as the starting point to explore the immunoinflammatory mechanism of COPD, and study how to predict the effects of different treatments of COPD by identifying the microbiota, and how to achieve the optimal enrichment of beneficial bacteria and the optimal consumption of harmful bacteria to improve COPD.
Keywords: COPD, microbiome, bibliometric analysis, CiteSpace, gut microbiome, respiratory microbiome, bacterial colonization
Introduction
Chronic obstructive pulmonary disease (COPD), a respiratory condition marked by recurrent respiratory problems and air trapping brought on by abnormalities in the airways and/or alveoli, is frequently linked to prolonged exposure to harmful particles, with chronic cough, expectoration, shortness of breath, or dyspnea as the main symptoms, with high prevalence and case fatality.1–4 In 2020, it became the third-ranking cause of death globally.5–7 Especially in the world of novel coronavirus pneumonia, COPD sufferers are more prone to cause serious illness and death,8 so in the situation of the global spread of the epidemic, the diagnosis and treatment of COPD patients is particularly important.
A group of microbes that reside on and in the human body is known as the human microbiome9 and interact with the environment, enabling special metabolic processes for the human host as well as microbial environmental stimuli.10 Studies had shown that the microbiota was vital to the onset, development, and progression of lung illness.8,11,12 Lachnospiriaceae was favorably connected with COPD severity, while Parabolides goldsteinii and Escherichia coli were negatively correlated.13 Additionally, an imbalance in the lung microbiota can worsen COPD by downregulating miR-122 and miR-30a and enhancing the expression of interleukin-17a (IL-17a).14 An alternate method to treat COPD is to consume bad bacteria as much as possible or to enrich helpful bacteria as much as possible, for example, the isolated strains of Parabacteroides goldsteinii MTS01, Bifidobacterium brew and Lactobacillus rhamnosus can reduce inflammation of the airways and alveoli injury in COPD mice.13,15 A growing body of evidence13–17 also revealed that COPD patients had a different microbiome than healthy people and that the associated beneficial microorganisms, pathogenic organisms, and their induced immune flammatory responses were helpful to explore its pathogenesis, allowing space for more targeted interventions and new treatments. Numerous papers in the area of the microbiome in COPD had been published during the previous 10 or so years to characterize this dynamic interaction between microorganisms, therapeutics, and disease states. The massive literature growth necessitates new methods for reviewing and trend analysis. However, to date, no bibliometric research on microbiome in COPD have been reported.
The statistical evaluation and quantification of academic publications is known as bibliometrics18 and has been applied in many research areas to evaluate countries, organizations, authors, journals, cited references, and pertinent keywords.19 One of the most often used bibliometric analysis programs is CiteSpace, which was invented in early 2004 by Professor Chaomei Chen to explore the dynamic evolution of the development of the discipline.20–22 According to the bibliometric program CiteSpace, this study systematically analyzed the overall trend of the microbiota of COPD patients in the past decade through the time mapping from research frontiers to knowledge bases, using the most commonly used database in econometric research,23 namely Web of Science Core Collection (WoSCC), also foresaw potential new academic frontiers and spots in the future. This is wished here that work will offer some reference value for researchers in the field and encourage further development in this area.
Methods
Information Sources and Search Tactics
The WOSCC database was selected as the goal resource for the primary article search. WOSCC serves as the most popular and reliable web browser for academic literature, offering thorough coverage of important scientific outcomes across the globe.24 Numerous research have made extensive use of relevant research assessment and visualization of scientific literature.25–28 To guarantee the completeness of the bibliographic data, the search index utilized by WoSCC was standardized to cover all pertinent articles.
The following terms were included in the search method for both COPD and microbiota: TS= (microbiota OR microbial community OR microbial community composition OR microbial community structure OR human microbiome OR microbiome) AND TS= (chronic obstructive lung disease OR chronic obstructive pulmonary disease OR COAD OR COPD OR chronic obstructive airway disease OR chronic airflow obstruction) and the search dates are from 1 January 2011, to 31 August 2022. The extraction and output of documents should be completed within a day to eliminate bias brought on by continuing database updates (September 14, 2022). The National Library of Medicine (NLM)/PubMed provided a list of Medical Subject Headings (MeSHs), from which the aforementioned keywords were selected.
Inclusion and Exclusion Criteria
The following were the study’s inclusion and exclusion criteria: (1) The time period covered 13 years from 2010 to 2022; (2) only reviews and articles were included, and additional documentation categories (such as book chapters, proceedings papers, letters, publications that have been retracted, and editorial materials) were removed; (3) duplicate publications were excluded; (4) unpublished articles were excluded; and (5) irrelevant articles were excluded.
Data Analysis and Visualization
For visual analysis, the ultimate selected publications were loaded into CiteSpace (6.1.R3) and Microsoft Excel. The amount of papers produced each year was trended using Microsoft Office Excel. CiteSpace is a data analysis and document visualization application. Dr Chaomei Chen of Drexel University in Philadelphia, Pennsylvania, developed it. Co-occurring keyword, Co-authors and Co-citations analyses are just a few of CiteSpace’s outstanding features. It aids in offering clear instructions for moving on with analysis in a particular area of research.29 The following CiteSpace settings are in place: time slicing (from 2010 to 2022, years per slice = 1), node type (Select one option from keywords, countries, institutions, authors, references, cited authors and cited journals each time), links (scope: within slices, strength: cosine), selection criteria (g-index: k = 25). When the node is a keyword, the clipping method is selected Pruning the merged network, Pruning sliced networks, pathfinder.
Results
Article Distribution by Years of Publication
Considering the inclusion and exclusion criteria, a total of 505 articles were finally obtained after deleting 128 non-conforming records. The annual amount of papers pertaining to the COPD microbiome increased steadily, according to the worldwide trend in publication numbers shown in Figure 1. The quantity of books published in 2021 was the highest over the past decade,30 and since 2018, the number of publications has been greater than 50 each year. It is possible to estimate that the number of books published will keep growing gradually inside the years to come based on the expansion curve of articles over time.
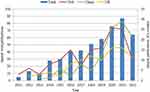 |
Figure 1 The quantity of yearly publications. |
In terms of the three highest prolific nations’ annual publications, the US consistently maintains high levels of output. China has seen the fastest growth, with annual production surging since 2018, surpassing the USA to peak in 2021. The UK’s trend in the volume of publications has also shown an overall growth trend in the last 10 years, reaching a peak in 2020. These findings suggest that study on the microbiota and COPD is expanding internationally.
Analysis of Countries or Regions
The papers on the study of the COPD microbiome included contributions from 49 nations or regions. Table 1 lists the best 10 nations or regions based on publications and centrality. The leading five countries in counts of papers were the USA, China, the UK, Australia, and Spain, whereas the top five nations in regards to centrality were the UK, the USA, Australia, Denmark, and Spain. China came in second with 111 papers, trailing the USA’s 144 papers as the more prolific nation. In Northern America and Europe, the USA, the UK, and Spain had the highest rates of productivity. In Oceania and Asia, China and Australia had the highest rates of productivity. The USA came in second with a centrality of 0.23, trailing only the UK with a 0.31 score, and Australia had the third centrality at 0.17. The UK, the USA, Australia, and Denmark all have a centrality of larger than 0.1, suggesting that those same four nations have some bearing on the research of the microbiome in COPD. High-productivity countries rank high level of publications and centrality, demonstrating that their influence on the world was inversely correlated with their output.
 |
Table 1 The Top 10 Countries or Regions in Aspects of Articles Published and Importance |
Figure 2 displays the cooperation network diagram between nations/regions. There are 49 nodes and 187 lines in this network, and its density is 0.159. Nodes in the map represent countries. The yearly circle width shows how many articles the nation publishes in a specific year. The annual ring gets broader the more publications that year are published. Cooperation relations are represented by lines connecting the nodes. The wider the line, the stronger the relationships. Overall, the top 10 countries or regions, as determined by publications and centrality, collaborate with one another, with the USA and the UK in particular having the largest number of national collaborators.
 |
Figure 2 Visualization map of countries or regions. |
Analysis of Institutions
From 2011 to 2022, 321 institutions in total listed inside this area. The 10 leading institutions, as determined by publications and centrality, are shown in Table 2. Imperial College London, University of Leicester, University of Manchester, University of Queensland, and Newcastle University were the list of top institutions. The five most important institutions in aspects of centrality were University of Michigan (0.19), Imperial College London (0.16), University of Dundee (0.13), University of Leicester (0.10) and University of Southampton (0.08). The centrality of University of Michigan, Imperial College London, University of Dundee and University of Leicester is greater than 0.1, showing that they have some impact inside the research on the microbiome and COPD. Institutions have mostly been centered at universities as well as a small number of hospitals, and were mainly located in the UK.
 |
Table 2 Top ten10 Institutions in Respect of Centrality and Amount of Publications |
Extensive cooperation between institutions were discovered as a result of the created institutional mesh node, which showed 321 nodes and 691 link lines representing the institutions with their collaborative links, accordingly (Figure 3A). Imperial College London, for example, which was symbolized by the greatest node, exhibited the most care coordination including several universities, such as University of Leicester, University of Queensland, Newcastle University, University of Manchester, Southern Medical University, University of Technology Sydney.
 |
Figure 3 (A) A visualization map of institutions. (B) A visualization map of authors. (C) A visualization map of cited authors. (D) A visualization map of cited journals. |
Examination of Authors and Those Cited
To find possible relationships, the co-authorship and writers who were mentioned were examined. With 378 nodes and 1008 links, the co-authorship network (Figure 3B) was constructed. As a result of his outstanding impact on the development of this subject, Brightling C from the UK held the top spot with all writers in the study of the microbiota in COPD. The two next-most prolific writers are Wang Z from the USA and Singh D from the UK, with 14 and 12 publications, respectively. We discovered that writers who produced a significant amount of publications typically had set partners and, as a result, formed their own research groups. In accordance with the findings of the 10 largest productive countries, the majority of the leading 10 authors originate from the UK, with a small number coming from the USA and Australia (Table 3).
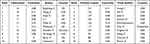 |
Table 3 Top 10 Authors, Include Highly Cited and Prolific Writers |
Figure 3C displays the network of cited authors, with 559 nodes and 3166 links. In total, 559 authors were cited, of which 7 were referenced at over 100 times. The American researcher Huang Y had the most citations (n = 151), following after Sze M (n = 130), and Sethi S (n = 176). Nine of the top 10 most mentioned writers are all Americans (Table 3).
Analysis of Cited Journals
To identify the interconnectedness and cross-relationship across journals in the study of the COPD microbiome, analysis of referenced journals was done. Table 4 contains information about the top 10 referenced journals in this field, and Figure 3D shows a map of the pertinent body of knowledge. The American Journal of Respiratory and Critical Care Medicine (341 citations), PLoS One (338 citations), European Respiratory Journal (291 citations), Thorax (273) and The New England Journal of Medicine were the top five cited journals (240). Among top 10 most referenced journals, Lancet had an IF of 202.73, which was followed by The New England Journal of Medicine, which had an IF of 176.079. The foundation of this discipline is shown in the published citations of such prestigious journals. The lion’s share of the top 10 journals are high-caliber American and British periodicals.
 |
Table 4 Top 10 Cited Journals |
Analysis of Cited Reference
The condition of cited literature in this area is shown in Figure 4A, which featured a network with 581 nodes and 2549 links. The 10 leading publications in terms of number of references are detailed in Table 5, with the most popular article, “The lung tissue microbiome in chronic obstructive pulmonary disease”, written by Sze et al and posted in the American Journal of Respiratory and Critical Care Medicine in 2012, receiving the highest number of citations.31 Among the 10 leading documents, 4 were published in the American Journal of Respiratory and Critical Care Medicine, two in the PLoS One, respectively, while the rest of the group were authored in different journals. These 10 references could be considered as the most popular articles and fundamental research inside this ground.
 |
Table 5 Top 10 Cited References |
 |
Figure 4 (A) Visualization map of cited references. (B) Co-occurring keywords map. (C) The cluster of keywords. (D) Timeline view for keywords. |
Analysis of Keywords and Research Hotspots
Hot subjects are represented by keywords with a high frequency, while terms with a significant centrality show the impact of relevant research in a particular area. The keyword co-occurrence knowledge map (Figure 4B) contained 381 nodes and 718 lines. Table 6 lists the most popular 10 high-frequency keywords here on subject, which were COPD, exacerbation, gut microbiota, microbiome, cystic fibrosis, lung microbiome, infection, bacterial, airway microbiome and inflammation. The most crucial 10 keywords were bacterial colonization, COPD, pseudomonas aeruginosa, diversity, 16s ribosomal rna, cystic fibrosis, association, inflammatory bowel disease, T cell and asthma. In addition, keyword clustering visualization was also constructed, as shown in Figure 4C. In the study of the microbiome in COPD, there have been 15 clustering patterns. The specifics are displayed in Table 7.
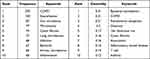 |
Table 6 The 10 Most Popular Keywords in Regards to Frequency and Centrality |
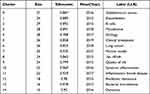 |
Table 7 Clustering of Keywords of COPD Microbiome-Related Research |
The microbiome research in the field of COPD mainly focused on gut microbiota and respiratory microbiome, and 16s RNA technology was often used for detection. Inflammation was important in the etiology of COPD, as well as the combination of inflammatory bowel illness could increase the mortality risk in COPD patients.40 The pathogenesis of the disease also included infection, bacteria, T cell immunity, B cell immunity, etc. Patients with COPD frequently have Staphylococcus aureus and Pseudomonas aeruginosa in their bodies. The top keyword in terms of centrality was bacterial colonization, and this was one of the primary factors in the severe COPD exacerbation.41
In addition, the emergence and progress of frontier research themes can be reflected in the timeline view of keywords (Figure 4D) and keyword burst term map (Figure 5). We found that “staphylococcus aureus” (Cluster 0), “exacerbation” (Cluster1), “B cells” (Cluster2), “etiology” (Cluster 4), “lung cancer” (Cluster 6), “16s rRNA” (Cluster 8), “quality of life” (Cluster 9), “antibiotic resistance” (Cluster 12) and “bacterial microbiome” (Cluster 13) were a relatively early hotspot, and “mycobiome” (Cluster 3), “clinical breakpoint” (Cluster 5), “murine model” (Cluster 7), “systemic inflammation” (Cluster 10), “inflammatory bowel disease” (Cluster 11) and “dynamics” (Cluster 14) were hot spots in the middle and late stages. Furthermore, Staphylococcus aureus, exacerbation, mycobiome, etiology, clinical breakpoint, quality of life, inflammatory bowel disease have continued on the timeline, which may be the focus of research in the next few years. The keyword “bacterial colonization” appeared in 2011 is the most explosive keyword, followed by “community” and “sputum”. In contrast, “community” and “non-typable haemophilus influenzae” were the terms that appeared more frequently in the last 5 years.
 |
Figure 5 Top eight keywords with the strongest citation bursts. |
Discussion
General Trends
In this work, CiteSpace was employed to conduct a thorough evaluation of ongoing research on the connection between COPD and the microbiota, identify hot themes in this field, and forecast prospective future directions for research. From 2011 to 2022, 505 papers about the microbiota and COPD were found by searching the WOSCC. In respect of yearly articles, we discovered that this field’s publications increased gradually annually, particularly after 2020, which demonstrates that scholars from all nations continued to pay attention to and show interest in this topic. This represented the recognition of the majority of scholars on the results of recent study in this area and the continuous research on the unknown and problems worth further exploration in this field. For example, more and more evidence showed that probiotics (Bifidobacterium,42 Lactobacillus plantarum,43 etc) can protect and treat lung diseases by optimizing the balance of gastrointestinal microorganisms (stimulating the balance of Th1/Th2,42 lowering the lung’s innate immune cell count,43 etc), but its therapeutic effect on COPD, exact mechanism, and many aspects of regulating immune response are still largely unknown.15 These unknowns can stimulate the motivation of researchers, and lay a good foundation for further exploring the internal relationship between COPD and microbiome, searching for its potential mechanisms, and developing potential beneficial bacteria strains and their functional components to treat COPD.
Analysis of Contributions from Nations/Regions, Organizations, and Journals
An assessment of annual papers related to the COPD microbiome found that the USA and the UK were the highest ranked nations in regards to central location, publishing more than 47% of the 505 publications, according to a visual analysis of the dispersion of countries, which showed that they were not only the most active countries that publish papers but also had great influence. In terms of research institutions, Imperial College London (UK) was the most productive research institution, and the research university with the greatest centrality was the University of Michigan (US), and the proportion of the USA and the UK in the 10 leading nations for productivity and centrality was more than half, which showed that the two countries’ prominence in this field of study. This may be related to the fact that both the University of Michigan and Imperial College London have top national lung research institutes, which have trained a large number of high-quality talents. For example, from Imperial College of Technology, Peter J Barnes, was one of the core expert group members of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines. He has written more than a thousand peer-reviewed articles in asthma, COPD, other relevant fields (h-index 186, cited more than 150,000 times), which has a huge impact. To sum up, the study of the link with COPD and microbiota is primarily conducted in the USA and the UK.
The number of papers published by China ranked second, demonstrating China’s substantial influence in this area. It was worth noting that in Table 2, except for China, other research institutions were located in industrialized nations, particularly the UK, the USA and Australia. This demonstrated that national impact on the world stage was inversely correlated with research institution production, and they showed great academic influence in this field. At the same time, Figures 2 and 3A show the tight collaboration between many nations and institutions, including close cooperation between China and European and American countries. In the context of global cooperation commons, researchers from many countries will cooperate to conduct more and more important research in the future, which will encourage the growth and consolidation of this field’s knowledge.
The 10 most popular journals, which were those that had produced high-quality studies and aroused the interest of researchers engaged in this area, are listed in Table 4. The findings of our study will aid researchers in this area in quickly locating pertinent publications, obtaining the most recent developments in COPD microbiology research, or submitting their works.
Influential Authors and Studies
Brightling C from the University of Leicester in the UK was the writer who had the most articles. His research has long focused on asthma, immunology, internal medicine, COPD and problems in sputum, and combined the topics of microbiome, lung disease, deterioration, lung and biomarkers with his research on COPD. In 2021, in a study his team conducted comparing the pulmonary microbiomes of healthy people and COPD patients, they found that as the disease got worse, the microbiomes of the lungs changed, the airway microbiome is connected to the decreased abundance of Prevotella and increased abundance of Moraxella.44 In another study, his team discovered that in some cases, eosinophilic and neutrophilic COPD are convertible, and that by tracking the respiratory microbiome’s temporal variability, one may follow the inflammation condition of patients across time.45 His and his team’s research has laid a good foundation for future scholars to explore the host microorganism interaction of COPD and the related immune response of lung microorganisms in COPD. Additionally, we discovered that University of Michigan student Yvonne J. Huang received the most citations. She is mainly engaged in the study of the microbiome–host interactions in COPD pathogenesis and phenotypes. For example, according to one of her studies, changes in the heterogeneity of the bronchial microbiome were associated with the progression of COPD, an upsurge in the species that are home to common COPD pathogens, and a decrease in the number of microbiota members that provide assistance to the structure and functionality of homeostasis.46 In terms of the quantity of published papers and publications referenced, Zhang Wang from the School of Life Sciences at South China Normal University ranked the highest 10. He is engaged in the research of respiratory system disease microbiology, and deeply revealed the characteristics of airway microecology in patients with COPD. His study, which was published in Nature Microbiology in 2022, showed that interleukin-22-mediated macrophage-epithelial cell cross-talk prevents lung function decrease, emphysema, apoptosis and neutrophilic inflammation in response to respiratory microbiome-derived IAA.47 These authors have had a significant academic impact on this field and have made remarkable contributions to its advancement.
The article by Sze31 that appeared in the American Journal of Respiratory and Critical Care Medicine in 2012 is the one that has received the most citations. This study found that the bacterial community in human lung tissue was both observable and dynamic. The follow-up research is mainly based on this to explore what this detectable and changeable bacterial community is, and what is the internal relationship with COPD disease.45,48,49 Zhang Wang was the author of the second-most-cited paper (European Respiratory Journal).32 This article showed that the change of pulmonary microbiota seemed to be related to the deterioration event, while Haemophilus might greatly affect the entire microbial community structure. The third most cited was written by John R Erb Downward (PLoS One).33 The pulmonary microbiome has been further demonstrated in this study, which also highlights macro- and micro-anatomical abnormalities in these microbial flora in individuals who have severe COPD. Based on the correlation between pulmonary microorganisms and COPD deterioration, the follow-up research deeply explored the specific flora and its mechanism leading to the deterioration, and looked for the optimal consumption of potentially harmful bacteria in order to determine potential therapeutic interventions.47,50,51 Analysis of the network of references reveals that the microbiome mainly studied in the top 10 cited references was from lung tissue and respiratory tract. The authors of these papers observed that the pulmonary microbiota would change when people with exacerbations of COPD,31,32 and the increased microbiota members were mainly Proteus.34 The most frequently cited articles have a good guiding role within the field, laying a foundation for upcoming studies on the influence and mechanism of the interaction between microorganisms and COPD, and providing a research basis for new prevention and treatment of COPD.
Hotspots and Frontiers
The paper’s study theme can be summed up using the keywords that reflect the main thesis and essential elements of the literature. We can therefore identify the current study centers in an area, anticipate future trends in research scientifically, and give researchers a place to start their research by looking at the frequency and centrality of keywords in that field. We analyzed the popular keywords involved in keyword co-occurrence, clustering, timeline and citation bursts, summarizing the following three major research directions: First, bacterial colonization, mainly involving Pseudomonas aeruginosa, Haemophilus influenzae and Staphylococcus aureus, is highly close to the deterioration of COPD; the second is respiratory microbiota; the third is gut microbiome: it mainly involves T cells and B cells, and the main representative product is short-chain fatty acid. COPD and inflammatory bowel illness are related. Because inflammation is the pathological basis and core mechanism of COPD, the above three points are mostly combined with inflammation analysis to explore the mechanism of interaction between COPD and microbiome. The following will be elaborated on the basis of these three points, with a view to finding a way forward for researchers.
Bacterial Colonization
The occurrence and development of COPD were related to inflammatory cells, which can produce inflammatory mediators after being activated by stimulators, and then damaged the airway wall and lung tissue.52,53 When referring to the presence of bacteria on or in the human body, the phrase “colonization” denotes that the host is unaffected by the germs. However, in all stages of COPD, bacterial colonization could enhance airway inflammation in stable COPD, reduce lung function54–56 and increase systemic inflammatory markers.57,58 With the decrease of immune capacity of COPD patients in the stable period,45 lower airway bacterial colonization (LABC) was most likely to occur,59,60 that is, the lower respiratory tract’s mucosal epithelium was covered in a lot of bacterial flora, which absorbed nutrients through the body and grew and reproduce in the lower respiratory tract’s mucous epithelium, thus causing host infection.61 It was proved that there was a clear correlation between bacterial pathogen isolation in peripheral bronchial tree and neutrophil airway inflammation in COPD, and the primary chemokine mediator throughout this mechanism appeared to be IL-8.62 According to Chung’s research,63 individuals with stable COPD who had bacterial colonization had higher levels of TNF- α, IL-6, and IL-8 in their sputum. Zhang64 clearly showed how LABC could impact inflammation of the airways and the occurrence of COPD acute exacerbations (AECOPD). If bacterial colonization increased the symptoms of stable COPD, it is expected that treatment (such as preventive antibiotics) can alleviate the COPD patients’ clinical signs and symptoms. At present, the species identified from COPD sufferers’ lower airways and showing signs of deterioration included65–67 Pseudomonas aeruginosa (PA), Streptococcus pneumoniae (SP), Moraxella catarrhalis (MC) and non-typeable Haemophilus influenzae (NTHI). Other potential pathogens that were not often isolated were Haemophilus parainfluenzae and Staphylococcus aureus.60
Non-Typeable Haemophilus Influenzae
Haemophilus influenzae may be a significant pathogen in both stable COPD and exacerbation of COPD.68 The bulk of Haemophilus influenzae analyzes the evidence in the airways,69 and the focus of much investigation are NTHI strains. In mice with a cellular and cytokine profile comparable to that of COPD,47 the retention of NTHI in the lower airway stimulated the respiratory epithelium to release proinflammatory cytokines, particularly those that enhance neutrophil chemokines.60 The development of small airway illness in COPD patients was aided by NTHI colonization, and the condition of COPD patients’ health deteriorated.70
Pseudomonas Aeruginosa
PA colonization was a recognized occurrence in COPD patients and hospitalized patients. It was usually seen in the late stage of COPD,54 which can lead to severe airway inflammation and secondary lung injury, leading to deterioration of clinical conditions.71 The colonization of PA in COPD was transient or persistent,72,73 which may be related to exoU and pKL-3 genes.74,75 PA colonization contributed to the production of autoantibodies against the bacterial/permeability invading protein (BPI), which maked BPI unable to clean pathogenic microorganisms, thus inducing inflammatory reaction.76 It had also been shown77 that the mechanism of COPD deterioration was related to the production of IL-6 and IL-8 in bronchial epithelial cells induced by PA-derived flagellin. The meta-analysis also revealed that individuals with COPD had an adjusted higher death risk when PA separated from sputum.78
Staphylococcus aureus
Toxins produced by Staphylococcus aureus induced necrosis and apoptosis,79 and triggered cell death via the RIPK1/RIPK3/MLKL cascade reaction, which resulted in the destruction of particular immune cell types, particularly macrophages, thus leading to inflammatory disorders and impairing bacterial clearance.80 Violent enterotoxins, such Staphylococcus aureus enterotoxin B (SEB), are released as a result of Staphylococcus aureus colonization, which has superantigen activity that causes T cells’ activation. The research of Wouter Huvenne’s team proved that combining SEB with cigarette smoke (CS) exposure led to the production of dense T and B cell aggregates in the lungs, and aggravated the inflammation of mice induced by CS.81 These results suggest that Staphylococcus aureus may have an impact on how COPD develops.
In summary, further elucidation of the pathogenesis of bacterial colonization affecting COPD will perhaps be the subject of current and upcoming studies in this area which could offer new treatment goals for Patients with COPD as well as diagnostic and prognostic indicators.
Respiratory Microbiome
The upper and lower airways (oropharynx, bronchial tree, and lungs) are covered by the respiratory microbiome, which has discrete populations and varying loads,82,83 which interact with the environment and are influenced by host inflammatory and immune responses, host genetics, and subject disease,84 presenting pathogenicity or beneficialness. There is mounting evidence that the clinical phenotype, long-term mortality and severity of COPD are all directly related to the respiratory microbiome.31,85 The diversity and composition of the respiratory microbiome of stable COPD patients varied with age, degree of airflow restriction, frequency of exacerbation, and peripheral blood eosinophils.86 Dysregulated airway microbiome ecology had been reported to lead to airway inflammation, immune dysregulation, infection susceptibility,32,87 and alterations in host epithelial repair mechanisms,44 and its metabolites were also somehow associated with inflammation.88,89 In slow-onset lung disease, Wang discovered that IAA produced by the respiratory microbiota reduced eosinophil inflammation and epithelial apoptosis.47 Based on this, a “vicious cycle” hypothesis of chronic inflammation had been proposed, whereby chronic inflammation resulting in the recurring onset of COPD, lowering the lung’s immune system’s defenses and leading to a dysregulated lung microbiome, which in turn amplified the COPD’s continuous inflammatory response and lead to disease progression.60
The two main airway inflammatory endotypes in COPD are neutrophilic or eosinophilic inflammation,49 both mediated through the interaction of microbial metabolism with host gene expression.47 Wang and his team emphasized the role of the respiratory microbiota in the management of patients based on inflammatory endotypes in COPD.45 Yadava90 used lipopolysaccharide and elastase in mice to induce chronic COPD-like lung inflammation, demonstrating that host microbial crosstalk promotes inflammation. The severity and course of COPD may be functionally influenced by lung microbial dysbiosis,32,87 and bacterial proteins or metabolites may be used to effectively promote host inflammatory signaling.30 Airway microbial communities shifted during episodes of healthy and COPD,36,91 disease exacerbation,34,92 such as bacteria from the phylum Mycobacterium, Thicket and Aspergillus.44 Whereas members of Aspergillus, Actinomyces and Thickobacter were major contributors to palmitate, homocysteine and urate biosynthesis;93 palmitate activated inflammation-associated enzymes94 to enhance inflammation;95 through the ERK1/2 pathway, homocysteine activated the pro-inflammatory substance MMP9;96 by triggering inflammatory vesicles with the CCL2 and NLRP3 genes, urate may potentially cause inflammation;77 these biosyntheses contributed to the development of COPD inflammation. Over time, the stability of the pulmonary microbiota may decrease in individuals who deteriorate, while recurrent deterioration within subjects was more likely to repeat bacterial and eosinophil deterioration.30
Additionally, it has been demonstrated that antibiotic therapy alters the COPD airway microbial population and that treatment with antibiotics alone reduces bacterial abundance, especially in the Proteobacteria members.9 After 8 weeks of daily azithromycin treatment for COPD patients, Segal et al discovered a decrease in respiratory microbial diversity while metabolites produced by the bacteria reduced lung inflammation, indicating that the effect of azithromycin on COPD patients may be partially mediated by interactions between the respiratory microbiome and the host immune system.89 Also several studies have shown that the airway microbiome abnormalities identified in patients with COPD exacerbations treated with antibiotics are still present 3 months after the exacerbation and may last longer.34
In conclusion, as described in the literature, COPD interacts with the pulmonary microbiota based on the idea that persistent inflammation causes disease progression in a “vicious circle”. In turn, the ongoing impact of antibiotic therapy on respiratory microbial changes in COPD helps to investigate the feasibility of resident bacteria as potential targets for immunomodulation to identify targets for treatment and intervention.
Gut Microbiome
The lungs and intestines are of the same histological origin, with the epithelial tissues of the lungs and large intestine originating from the proto-intestinal endoderm, and there is synchrony between the lungs and intestines in terms of mucosal immunity. Although COPD is a respiratory disease, it usually occurs in conjunction with chronic gastrointestinal disorders,97,98 such as inflammatory bowel disease.99,100 Recent research had connected pulmonary illness development to changes in the composition and function of the gut microbiome,101–103 discovering that COPD patients’ fecal microbiomes and metabolomes differed from those of healthy people.41 A new idea had been proposed that the “gut–lung” axis mediated the pathogenic link between the microbiota and respiratory diseases.104 It had been suggested that COPD pathogenesis was associated with imbalance in the gut microbiota,105 which adversely affected the gut mucosal barrier function and the body’s immune response, leading to elevated levels of local and systemic inflammatory mediators, a key mechanism of action in the development of COPD. The pyrin domain-containing protein 3 (NLRP3) has been shown to be a critical bidirectional regulator of the intestinal-pulmonary axis. This stimulated the recruitment of inflammatory cells and altered immunological reaction in the lungs and digestive system, which in turn affected the activity of NLRP3 inflammatory vesicles.104,106 Furthermore, experimental mice with gut bacteria dysregulation can cause a marked acceleration of neutrophil infiltration by stimulating the action of the organism’s TLR4, which in turn induced a large pulmonary response to bacterial attack and thus inflammation.107 Gut microbes can increase the quantity of extraintestinal T cells, and differentiated T cells with Th1 and/or Th17 pro-inflammatory cell characteristics activated anti-inflammatory or neutrophils cells as extra effector cells to regulate the immune reaction.108
In addition to the common mucosal immunity theory, another theory was that the gut flora produced metabolites that influence the immune response in the lungs.41,109 Li discovered that COPD patients had a different gut flora from healthy people, one that was dominated by Prevotella and had reduced amounts of short-chain fatty acids (SCFAs), such as butyrate, propionate and acetate.110,111 SCFAs played an significant role in vivo112–115 and were thought to be a group of metabolites that affected inflammation.116 By interacting with G protein-coupled receptors on cell membranes including HCA2, FFA2, and GRP43, SCFAs can activate downstream effector molecules like NLRP3, PI3K, and MAPK and change helper T cells and dendritic cells.117,118 SCFAs could also signaled through GPR43 and GPR109A on intestinal epithelial cells to activate NLRP3 inflammatory vesicles causing lung inflammation and immune cell activation.111 Additionally, the transporter proteins SLC5A8 or SLC16A1 can allow SCFAs to enter cells.119,120 SCFAs inhibit histone de acetylase (HDAC) activity to regulate the type of immune response.113 It had been shown that SCFAs played a role in COPD exacerbations, decreased lung function, COPD weight and physical frailty phenotypes, and emotional vulnerability phenotypes, and that it may play a role in controlling a variety of factors connected to the onset and advancement of COPD.121 Based on these mechanisms, Mao demonstrated that mucosal immunological response in rats with COPD was improved by administering drugs that remodeled the intestinal flora and inhibited the SCFAs/GPR43/NLRP3 pathway.122 We require a deeper comprehension of these systems in the future to facilitate the generation and development of more effective therapeutic intervention options.
To sum up, there is still a lot of work to be done in the study of COPD and gut microbiome. To define the mechanisms and clarify the link in greater detail, more study is required. How to explore its related mechanisms in depth from the viewpoint of the gastrointestinal-pulmonary axis and integrate the research results with clinical practice to generate more effective therapeutic interventions will be another hot spot for future research.
Strengths and Limitations
While CiteSpace-based analysis allows for more comprehensive and objective data analysis than traditional overviews, the study design has some constraints. First, if only the WoSCC database is searched, papers that are only available in other databases like Scopus and PubMed may not be found, which could lead to biased and incomplete studies that are included. Second, only articles and reviews are included, not book chapters, conference papers, letters, etc, which can lead to omissions. Finally, the publication deadline for our inclusion in our analysis is August 31, 2022, and although this already reflects the current situation and hotspots in the field, the data collected by the WOS core are constantly updated, but some newly published papers may have been overlooked; consequently, our articles do not accurately depict 2022. However, due to the credibility of the WoSCC database and the large number of publications analyzed, we believe that this study can still be utilized to illustrate current trends and research centers in the area. Future research with comparable objectives may take note of and overcome these constraints.
Conclusion
In summary, this analysis employed CiteSpace bibliometric analysis tools for the initial time to research the microbiome’s role in COPD and its hot topics from 2011 to 2022, and provided the latest analysis of relevant scientific outputs in this area. Every year, there are more publications in this field of study. The three countries that produce the most articles in this field of research are the USA, China, and the UK. Close international scientific cooperation, institutional cooperation and cooperation between researchers had been observed in this area, with institutional cooperation concentrated in universities. Due to the diversity of research directions, there was a variety of journals for researchers to choose from. Current research focused on inflammation, bacterial colonization, respiratory microbes, and gut microbes, which may be new research frontiers, and their outbreaks have been currently underway. The development and occurrence of COPD are tightly correlated with the gut–lung axis, and the microbiome in COPD has a strong anti-inflammatory ability. Studying the intestinal and pulmonary microbiome to explore the alleviation of airway inflammation in COPD could be a novel approach to researching COPD intervention and treatment strategies in the future. In addition, the microbiome and the host’s immunological health are tightly intertwined. Therefore, successful identification of microbiome populations may help predict the effectiveness of different treatments. Moreover, early intervention of related microorganisms can be carried out to delay the development of COPD by studying the potential mechanisms connected to the worsening of COPD. More work is needed on the internal relationship between COPD and microbiome to examine and confirm the involvement of advantageous bacterial strains in COPD, optimize the consumption of harmful bacteria, optimize the balance of microorganisms through diet, probiotics and flora transplantation, and find new strategies for prevention or treatment of COPD in the future. Our research revealed the basic scientific knowledge of the microbiome in COPD, timely sorting out and analyzing the current research trends and hot areas in the discipline. It may support the field’s ongoing development and assist scholars in better understanding the present general trends in the area.
Data Sharing Statement
The article contains the original findings discussed during the research. The research information used to support this study’s results shall be disclosed honestly and without undue reluctance.
Acknowledgments
Sincere appreciation goes out to reviewers for their insights and advice.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Innovation Team and Talents Cultivation Program of the National Administration of Traditional Chinese Medicine (Grant No. ZYYCXTD-D-202003), the Department of Science and Technology of Sichuan Province (2021ZYD0103 and 20ZDYF1199).
Disclosure
The study’s authors affirm that there were no financial or commercial ties that might be viewed as having a possible conflict of interest.
References
1. Raherison C, Girodet PO. Epidemiology of COPD. Eur Respir Rev. 2009;18(114):213–221. doi:10.1183/09059180.00003609
2. Agustí A, Vogelmeier C, Faner R. COPD 2020: changes and challenges. Am J Physiol Lung Cell Mol Physiol. 2020;319(5):L879–L883. doi:10.1152/ajplung.00429
3. Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet. 2017;389(10082):1931–1940. doi:10.1016/S0140-6736(17)31222-9
4. Polverino F, Sam A, Guerra S. COPD: to be or not to be, that is the question. Am J Med. 2019;132(11):1271–1278. doi:10.1016/j.amjmed.2019.04.047
5. Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi:10.1016/S0140-6736(12)61728-0
6. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;2017(9):691–706. doi:10.1016/S2213-2600(17)30293-X
7. Sin DD, Anthonisen NR, Soriano JB, et al. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245–1257. doi:10.1183/09031936.00133805
8. Hilty M, Burke C, Pedro H, et al. Disordered microbial communities in asthmatic airways. PLoS One. 2010;5(1):e8578. doi:10.1371/journal.pone.0008578
9. Mammen MJ, Sethi S. COPD and the microbiome. Respirology. 2016;21(4):590–599. doi:10.1111/resp.12732
10. Gill SR, Pop M, Deboy RT, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–1359. doi:10.1126/science.1124234
11. Chotirmall SH, Gellatly SL, Budden KF, et al. Microbiomes in respiratory health and disease: an Asia-Pacific perspective. Respirology. 2017;22(2):240–250. doi:10.1111/resp.12971
12. Tiew PY, Mac Aogain M, Ali NABM, et al. The mycobiome in health and disease: emerging concepts, methodologies and challenges. Mycopathologia. 2020;185(2):207–231. doi:10.1007/s11046-019-00413-z
13. Lai HC, Lin TL, Chen TW, et al. Gut microbiota modulates COPD pathogenesis: role of anti-inflammatory Parabacteroides goldsteinii lipopolysaccharide. Gut. 2022;71(2):309–321. doi:10.1136/gutjnl-2020-322599
14. Zhu K, Zhou S, Xu A, et al. Microbiota imbalance contributes to COPD deterioration by enhancing IL-17a production via miR-122 and miR-30a. Mol Ther Nucleic Acids. 2020;22:520–529. doi:10.1016/j.omtn.2020.09.017
15. Chunxi L, Haiyue L, Yanxia L, et al. The gut microbiota and respiratory diseases: new evidence. J Immunol Res. 2020;2020:2340670. doi:10.1155/2020/2340670
16. Russo C, Colaianni V, Ielo G, et al. Impact of lung microbiota on COPD. Biomedicines. 2022;10(6):1337. doi:10.3390/biomedicines10061337
17. Leiten EO, Nielsen R, Wiker HG, et al. The airway microbiota and exacerbations of COPD. ERJ Open Res. 2020;6(3):00168–2020. doi:10.1183/23120541.00168-2020
18. Moed HF. New developments in the use of citation analysis in research evaluation. Arch Immunol Ther Exp. 2009;57(1):13–18. doi:10.1007/s00005-009-0001-5
19. Wang C, Lv T, Deng X. Bibliometric and visualized analysis of China’s smart grid research 2008–2018. Front Res Metr Anal. 2020;5:551147. doi:10.3389/frma.2020.551147
20. Chen C, Hu Z, Liu S, et al. Emerging trends in regenerative medicine: a scientometric analysis in CiteSpace. Expert Opin Biol Ther. 2012;12(5):593–608. doi:10.1517/14712598.2012.674507
21. Synnestvedt MB, Chen C, Holmes JH. CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu Symp Proc. 2005;2005:724–728.
22. Gu D, Li T, Wang X, et al. Visualizing the intellectual structure and evolution of electronic health and telemedicine research. Int J Med Inform. 2019;130:103947. doi:10.1016/j.ijmedinf.2019.08.007
23. Leng Z, He X, Li H, et al. Olfactory ensheathing cell transplantation for spinal cord injury: an 18-year bibliometric analysis based on the Web of Science. Neural Regen Res. 2013;8(14):1286–1296. doi:10.3969/j.issn.1673-5374.2013.14.005
24. Shao H, Kim G, Li Q, Newman G. Web of science-based green infrastructure: a bibliometric analysis in CiteSpace. Land. 2021;10(7):711. doi:10.3390/land10070711
25. Wang N, Chen S, Zhang X, et al. Global research status and hot trends in stem cells therapy for Intervertebral disc degeneration: a bibliometric and clinical study analysis. Front Pharmacol. 2022;13:873177. doi:10.3389/fphar.2022.873177
26. Jiang B, Feng C, Li C, et al. A bibliometric and visualization analysis of glucocorticoid-induced osteoporosis research from 2012 to 2021. Front Endocrinol. 2022;13:961471. doi:10.3389/fendo.2022.961471
27. Wang S, Lin X, Guan Y, et al. Bibliometric and visual analysis of time-restricted eating. Front Nutr. 2022;9:979702. doi:10.3389/fnut.2022.979702
28. Ahmad T. Global research trends in MERS-CoV: a comprehensive bibliometric analysis from 2012 to 2021. Front Public Health. 2022;10:933333. doi:10.3389/fpubh.2022.933333
29. Chen C, Dubin R, Kim MC. Emerging trends and new developments in regenerative medicine: a scientometric update (2000–2014). Expert Opin Biol Ther. 2014;14(9):1295–1317. doi:10.1517/14712598.2014.920813
30. Mayhew D, Devos N, Lambert C, et al. Longitudinal profiling of the lung microbiome in the AERIS study demonstrates repeatability of bacterial and eosinophilic COPD exacerbations. Thorax. 2018;73(5):422–430. doi:10.1136/thoraxjnl-2017-210408
31. Sze MA, Dimitriu PA, Hayashi S, et al. The lung tissue microbiome in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1073–1080. doi:10.1164/rccm.201111-2075OC
32. Wang Z, Bafadhel M, Haldar K, et al. Lung microbiome dynamics in COPD exacerbations. Eur Respir J. 2016;47(4):1082–1092. doi:10.1183/13993003.01406-2015
33. Erb-Downward JR, Thompson DL, Han MK, et al. Analysis of the lung microbiome in the “healthy” smoker and in COPD. PLoS One. 2011;6(2):e16384. doi:10.1371/journal.pone.0016384
34. Huang YJ, Sethi S, Murphy T, et al. Airway microbiome dynamics in exacerbations of chronic obstructive pulmonary disease. J Clin Microbiol. 2014;52(8):2813–2823. doi:10.1128/JCM.00035-14
35. Morris A, Beck JM, Schloss PD, et al. Comparison of the respiratory microbiome in healthy nonsmokers and smokers. Am J Respir Crit Care Med. 2013;187(10):1067–1075. doi:10.1164/rccm.201210-1913OC
36. Pragman AA, Kim HB, Reilly CS, et al. The lung microbiome in moderate and severe chronic obstructive pulmonary disease. PLoS One. 2012;7(10):e47305. doi:10.1371/journal.pone.0047305
37. Molyneaux PL, Mallia P, Cox MJ, et al. Outgrowth of the bacterial airway microbiome after rhinovirus exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(10):1224–1231. doi:10.1164/rccm.201302-0341OC
38. Millares L, Ferrari R, Gallego M, et al. Bronchial microbiome of severe COPD patients colonised by Pseudomonas aeruginosa. Eur J Clin Microbiol Infect Dis. 2014;33(7):1101–1111. doi:10.1007/s10096-013-2044-0
39. Charlson ES, Bittinger K, Haas AR, et al. Topographical continuity of bacterial populations in the healthy human respiratory tract. Am J Respir Crit Care Med. 2011;184(8):957–963. doi:10.1164/rccm.201104-0655OC
40. Vutcovici M, Bitton A, Ernst P, et al. Inflammatory bowel disease and risk of mortality in COPD. Eur Respir J. 2016;47(5):1357–1364. doi:10.1183/13993003.01945-2015
41. Bowerman KL, Rehman SF, Vaughan A, et al. Disease-associated gut microbiome and metabolome changes in patients with chronic obstructive pulmonary disease. Nat Commun. 2020;11(1):5886. doi:10.1038/s41467-020-19701-0
42. Mahooti M, Abdolalipour E, Salehzadeh A, et al. Immunomodulatory and prophylactic effects of Bifidobacterium bifidum probiotic strain on influenza infection in mice. World J Microbiol Biotechnol. 2019;35(6):91. doi:10.1007/s11274-019-2667-0
43. Vareille-Delarbre M, Miquel S, Garcin S, et al. Immunomodulatory Effects of Lactobacillus plantarum on Inflammatory Response Induced by Klebsiella pneumoniae. Infect Immun. 2019;87(11):e00570–19. doi:10.1128/IAI.00570-19
44. Myr A, Kh A, Ec B, et al. Lung microbiome composition and bronchial epithelial gene expression in patients with COPD versus healthy individuals: a bacterial 16S rRNA gene sequencing and host transcriptomic analysis. Lancet Microbe. 2021;(7):e300–e310. doi:10.1016/S2666-5247(21)00035-5
45. Wang Z, Locantore N, Haldar K, et al. Inflammatory endotype-associated airway microbiome in chronic obstructive pulmonary disease clinical stability and exacerbations: a multicohort longitudinal analysis. Am J Respir Crit Care Med. 2021;203(12):1488–1502. doi:10.1164/rccm.202009-3448OC
46. Huang YJ, Boushey HA. The sputum microbiome in chronic obstructive pulmonary disease exacerbations. Ann Am Thorac Soc. 2015;12(Suppl 2):S176–80. doi:10.1513/AnnalsATS.201506-319AW
47. Yan Z, Chen B, Yang Y, et al. Multi-omics analyses of airway host-microbe interactions in chronic obstructive pulmonary disease identify potential therapeutic interventions. Nat Microbiol. 2022;7(9):1361–1375. doi:10.1038/s41564-022-01196-8
48. Tiew PY, Dicker AJ, Keir HR, et al. A high-risk airway mycobiome is associated with frequent exacerbation and mortality in COPD. Eur Respir J. 2021;57(3):2002050. doi:10.1183/13993003.02050-2020
49. Wang Z, Liu H, Wang F, et al. A refined view of airway microbiome in chronic obstructive pulmonary disease at species and strain-levels. Front Microbiol. 2020;11:1758. doi:10.3389/fmicb.2020.01758
50. Malvisi L, Yarraguntla A, Mortier MC, et al. Impact of bacterial strain acquisition in the lung of patients with COPD: the AERIS study. Infect Dis. 2022;54(11):784–793. doi:10.1080/23744235.2022.2092648
51. Qu L, Cheng Q, Wang Y, et al. COPD and gut-lung axis: how microbiota and host inflammasome influence COPD and related therapeutics. Front Microbiol. 2022;13:868086. doi:10.3389/fmicb.2022.868086
52. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
53. Di Stefano A, Caramori G, Ricciardolo FL, et al. Cellular and molecular mechanisms in chronic obstructive pulmonary disease: an overview. Clin Exp Allergy. 2004;34(8):1156–1167. doi:10.1111/j.1365-2222.2004.02030.x
54. Sethi S, Murphy TF. Infection in the pathogenesis and course of chronic obstructive pulmonary disease. N Engl J Med. 2008;359(22):2355–2365. doi:10.1056/NEJMra0800353
55. Soler N, Ewig S, Torres A, et al. Airway inflammation and bronchial microbial patterns in patients with stable chronic obstructive pulmonary disease. Eur Respir J. 1999;14(5):1015–1022. doi:10.1183/09031936.99.14510159
56. Bresser P, Out TA, van Alphen L, et al. Airway inflammation in nonobstructive and obstructive chronic bronchitis with chronic haemophilus influenzae airway infection. Comparison with noninfected patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162(3Pt1):947–952. doi:10.1164/ajrccm.162.3.9908103
57. Banerjee D, Khair OA, Honeybourne D. Impact of sputum bacteria on airway inflammation and health status in clinical stable COPD. Eur Respir J. 2004;23(5):685–691. doi:10.1183/09031936.04.00056804
58. Fuke S, Betsuyaku T, Nasuhara Y, et al. Chemokines in bronchiolar epithelium in the development of chronic obstructive pulmonary disease. Am J Respir Cell Mol Biol. 2004;31(4):405–412. doi:10.1165/rcmb.2004-0131OC
59. Aaron SD, Angel JB, Lunau M, et al. Granulocyte inflammatory markers and airway infection during acute exacerbation of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(2):349–355. doi:10.1164/ajrccm.163.2.2003122
60. Sethi S, Murphy TF. Bacterial infection in chronic obstructive pulmonary disease in 2000: a state-of-The-art review. Clin Microbiol Rev. 2001;14(2):336–363. doi:10.1128/CMR.14.2.336-363.2001
61. Jacobs DM, Ochs-Balcom HM, Zhao J, et al. Lower airway bacterial colonization patterns and species-specific interactions in chronic obstructive pulmonary disease. J Clin Microbiol. 2018;56(10):e00330–18. doi:10.1128/JCM.00330-18
62. Sethi S, Maloney J, Grove L, et al. Airway inflammation and bronchial bacterial colonization in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173(9):991–998. doi:10.1164/rccm.200509-1525OC
63. Chung KF. Inflammatory mediators in chronic obstructive pulmonary disease. Curr Drug Targets Inflamm Allergy. 2005;4(6):619–625. doi:10.2174/156801005774912806
64. Zhang M, Li Q, Zhang XY, et al. Relevance of lower airway bacterial colonization, airway inflammation, and pulmonary function in the stable stage of chronic obstructive pulmonary disease. Eur J Clin Microbiol Infect Dis. 2010;29(12):1487–1493. doi:10.1007/s10096-010-1027-7
65. Sethi S, Evans N, Grant BJ, et al. New strains of bacteria and exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 2002;347(7):465–471. doi:10.1056/NEJMoa012561
66. Miravitlles M, Espinosa C, Fernández-Laso E, et al. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Study Group of Bacterial Infection in COPD. Chest. 1999;116(1):40–46. doi:10.1378/chest.116.1.40
67. Garcha DS, Thurston SJ, Patel AR, et al. Changes in prevalence and load of airway bacteria using quantitative PCR in stable and exacerbated COPD. Thorax. 2012;67(12):1075–1080. doi:10.1136/thoraxjnl-2012-201924
68. Papi A, Bellettato CM, Braccioni F, et al. Infections and airway inflammation in chronic obstructive pulmonary disease severe exacerbations. Am J Respir Crit Care Med. 2006;173(10):1114–1121. doi:10.1164/rccm.200506-859OC
69. Finney LJ, Ritchie A, Pollard E, et al. Lower airway colonization and inflammatory response in COPD: a focus on Haemophilus influenzae. Int J Chron Obstruct Pulmon Dis. 2014;9:1119–1132. doi:10.2147/COPD.S54477
70. Marin A, Garcia-Aymerich J, Sauleda J, et al. Effect of bronchial colonisation on airway and systemic inflammation in stable COPD. COPD. 2012;9(2):121–130. doi:10.3109/15412555.2011.636407
71. King PT. Pseudomonas aeruginosa cross-infection: is this important in bronchiectasis and COPD? Respirology. 2019;24(10):926–927. doi:10.1111/resp.13578
72. Martínez-García MÁ, Faner R, Oscullo G, et al. Risk factors and relation with mortality of a new acquisition and persistence of Pseudomonas aeruginosa in COPD patients. COPD. 2021;18(3):333–340. doi:10.1080/15412555.2021.1884214
73. Gallego M, Pomares X, Espasa M, et al. Pseudomonas aeruginosa isolates in severe chronic obstructive pulmonary disease: characterization and risk factors. BMC Pulm Med. 2014;14:103. doi:10.1186/1471-2466-14-103
74. Martínez-Solano L, Macia MD, Fajardo A, et al. Chronic Pseudomonas aeruginosa infection in chronic obstructive pulmonary disease. Clin Infect Dis. 2008;47(12):1526–1533. doi:10.1086/593186
75. Rakhimova E, Wiehlmann L, Brauer AL, et al. Pseudomonas aeruginosa population biology in chronic obstructive pulmonary disease. J Infect Dis. 2009;200(12):1928–1935. doi:10.1086/648404
76. Schultz H, Weiss JP. The bactericidal/permeability-increasing protein (BPI) in infection and inflammatory disease. Clin Chim Acta. 2007;384(1–2):12–23. doi:10.1016/j.cca.2007.07.005
77. Nakamoto K, Watanabe M, Sada M, et al. Pseudomonas aeruginosa-derived flagellin stimulates IL-6 and IL-8 production in human bronchial epithelial cells: a potential mechanism for progression and exacerbation of COPD. Exp Lung Res. 2019;45(8):255–266. doi:10.1080/01902148.2019.1665147
78. Martinez-García MA, Rigau D, Barrecheguren M, et al. Long-term risk of mortality associated with isolation of Pseudomonas aeruginosa in COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2022;17:371–382. doi:10.2147/COPD.S346294
79. González-Juarbe N, Gilley RP, Hinojosa CA, et al. Pore-forming toxins induce macrophage necroptosis during acute bacterial pneumonia. PLoS Pathog. 2015;11(12):e1005337. doi:10.1371/journal.ppat.1005337
80. Ahn D, Prince A. Participation of necroptosis in the host response to acute bacterial pneumonia. J Innate Immun. 2017;9(3):262–270. doi:10.1159/000455100
81. Huvenne W, Lanckacker EA, Krysko O, et al. Exacerbation of cigarette smoke-induced pulmonary inflammation by Staphylococcus aureus enterotoxin B in mice. Respir Res. 2011;12(1):69. doi:10.1186/1465-9921-12-69
82. Budden KF, Shukla SD, Rehman SF, et al. Functional effects of the microbiota in chronic respiratory disease. Lancet Respir Med. 2019;7(10):907–920. doi:10.1016/S2213-2600(18)30510-1
83. Dickson RP, Erb-Downward JR, Freeman CM, et al. Spatial variation in the healthy human lung microbiome and the adapted island model of lung biogeography. Ann Am Thorac Soc. 2015;12(6):821–830. doi:10.1513/AnnalsATS.201501-029OC
84. Han MK, Agusti A, Calverley PM, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010;182(5):598–604. doi:10.1164/rccm.200912-1843CC
85. Dicker AJ, Huang JTJ, Lonergan M, et al. The sputum microbiome, airway inflammation, and mortality in chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2021;147(1):158–167. doi:10.1016/j.jaci.2020.02.040
86. Millares L, Pascual S, Montón C, et al. Relationship between the respiratory microbiome and the severity of airflow limitation, history of exacerbations and circulating eosinophils in COPD patients. BMC Pulm Med. 2019;19(1):112. doi:10.1186/s12890-019-0867-x
87. Dickson RP, Erb-Downward JR, Martinez FJ, et al. The microbiome and the respiratory tract. Annu Rev Physiol. 2016;78:481–504. doi:10.1146/annurev-physiol-021115-105238
88. Segal LN, Clemente JC, Tsay JC, et al. Enrichment of the lung microbiome with oral taxa is associated with lung inflammation of a Th17 phenotype. Nat Microbiol. 2016;1:16031. doi:10.1038/nmicrobiol.2016.31
89. Segal LN, Clemente JC, Wu BG, et al. Randomised, double-blind, placebo-controlled trial with azithromycin selects for anti-inflammatory microbial metabolites in the emphysematous lung. Thorax. 2017;72(1):13–22. doi:10.1136/thoraxjnl-2016-208599
90. Yadava K, Pattaroni C, Sichelstiel AK, et al. Microbiota promotes chronic pulmonary inflammation by enhancing IL-17A and autoantibodies. Am J Respir Crit Care Med. 2016;193(9):975–987. doi:10.1164/rccm.201504-0779OC
91. Einarsson GG, Comer DM, McIlreavey L, et al. Community dynamics and the lower airway microbiota in stable chronic obstructive pulmonary disease, smokers and healthy non-smokers. Thorax. 2016;71(9):795–803. doi:10.1136/thoraxjnl-2015-207235
92. Wang Z, Singh R, Miller BE, et al. Sputum microbiome temporal variability and dysbiosis in chronic obstructive pulmonary disease exacerbations: an analysis of the COPDMAP study. Thorax. 2018;73(4):331–338. doi:10.1136/thoraxjnl-2017-210741
93. Wang Z, Yang Y, Yan Z, et al. Multi-omic meta-analysis identifies functional signatures of airway microbiome in chronic obstructive pulmonary disease. ISME J. 2020;14(11):2748–2765. doi:10.1038/s41396-020-0727-y
94. Kanter JE, Kramer F, Barnhart S, et al. Diabetes promotes an inflammatory macrophage phenotype and atherosclerosis through acyl-CoA synthetase 1. Proc Natl Acad Sci U S A. 2012;109(12):E715–24. doi:10.1073/pnas.1111600109
95. Zhou BR, Zhang JA, Zhang Q, et al. Palmitic acid induces production of proinflammatory cytokines interleukin-6, interleukin-1β, and tumor necrosis factor-α via a NF-κB-dependent mechanism in HaCaT keratinocytes. Mediators Inflamm. 2013;2013:530429. doi:10.1155/2013/530429
96. Moshal KS, Sen U, Tyagi N, et al. Regulation of homocysteine-induced MMP-9 by ERK1/2 pathway. Am J Physiol Cell Physiol. 2006;290(3):C883–91. doi:10.1152/ajpcell.00359.2005
97. O’Hara AM, Shanahan F. The gut flora as a forgotten organ. EMBO Rep. 2006;7(7):688–693. doi:10.1038/sj.embor.7400731
98. Madan JC, Koestler DC, Stanton BA, et al. Serial analysis of the gut and respiratory microbiome in cystic fibrosis in infancy: interaction between intestinal and respiratory tracts and impact of nutritional exposures. mBio. 2012;3(4):e00251–12. doi:10.1128/mBio.00251-12
99. Rutten EPA, Lenaerts K, Buurman WA, et al. Disturbed intestinal integrity in patients with COPD: effects of activities of daily living. Chest. 2014;145(2):245–252. doi:10.1378/chest.13-0584
100. Keely S, Talley NJ, Hansbro PM. Pulmonary-intestinal cross-talk in mucosal inflammatory disease. Mucosal Immunol. 2012;5(1):7–18. doi:10.1038/mi.2011.55
101. Chakradhar S. A curious connection: teasing apart the link between gut microbes and lung disease. Nat Med. 2017;23(4):402–404. doi:10.1038/nm0417-402
102. Harris B, Morjaria SM, Littmann ER, et al. Gut microbiota predict pulmonary infiltrates after allogeneic hematopoietic cell transplantation. Am J Respir Crit Care Med. 2016;194(4):450–463. doi:10.1164/rccm.201507-1491OC
103. Schuijt TJ, Lankelma JM, Scicluna BP, et al. The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut. 2016;65(4):575–583. doi:10.1136/gutjnl-2015-309728
104. Budden KF, Gellatly SL, Wood DL, et al. Emerging pathogenic links between microbiota and the gut-lung axis. Nat Rev Microbiol. 2017;15(1):55–63. doi:10.1038/nrmicro.2016.142
105. Wang Y, Li N, Li Q, et al. Xuanbai Chengqi decoction ameliorates pulmonary inflammation via reshaping gut microbiota and rectifying Th17/Treg imbalance in a murine model of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2021;16:3317–3335. doi:10.2147/COPD.S337181
106. Donovan C, Liu G, Shen S, et al. The role of the microbiome and the NLRP3 inflammasome in the gut and lung. J Leukoc Biol. 2020;108(3):925–935. doi:10.1002/JLB.3MR0720-472RR
107. Pinkerton JW, Kim RY, Robertson AAB, et al. Inflammasomes in the lung. Mol Immunol. 2017;86:44–55. doi:10.1016/j.molimm.2017.01.014
108. Carbone C, Piro G, Di Noia V, et al. Lung and gut microbiota as potential hidden driver of immunotherapy efficacy in lung cancer. Mediators Inflamm. 2019;2019:7652014. doi:10.1155/2019/7652014
109. Wypych TP, Wickramasinghe LC, Marsland BJ. The influence of the microbiome on respiratory health. Nat Immunol. 2019;20(10):1279–1290. doi:10.1038/s41590-019-0451-9
110. Li N, Dai Z, Wang Z, et al. Gut microbiota dysbiosis contributes to the development of chronic obstructive pulmonary disease. Respir Res. 2021;22(1):274. doi:10.1186/s12931-021-01872-z
111. Raftery AL, Tsantikos E, Harris NL, et al. Links between inflammatory bowel disease and chronic obstructive pulmonary disease. Front Immunol. 2020;11:2144. doi:10.3389/fimmu.2020.02144
112. Trompette A, Gollwitzer ES, Yadava K, et al. Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nat Med. 2014;20(2):159–166. doi:10.1038/nm.3444
113. Thorburn AN, McKenzie CI, Shen S, et al. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nat Commun. 2015;6:7320. doi:10.1038/ncomms8320
114. Fagundes CT, Amaral FA, Vieira AT, et al. Transient TLR activation restores inflammatory response and ability to control pulmonary bacterial infection in germfree mice. J Immunol. 2012;188(3):1411–1420. doi:10.4049/jimmunol.1101682
115. Clarke TB. Early innate immunity to bacterial infection in the lung is regulated systemically by the commensal microbiota via nod-like receptor ligands. Infect Immun. 2014;82(11):4596–4606. doi:10.1128/IAI.02212-14
116. Vaughan A, Frazer ZA, Hansbro PM, et al. COPD and the gut-lung axis: the therapeutic potential of fibre. J Thorac Dis. 2019;11(Suppl 17):S2173–S2180. doi:10.21037/jtd.2019.10.40
117. Hussain K, Letley DP, Greenaway AB, et al. Helicobacter pylori-mediated protection from allergy is associated with IL-10-secreting peripheral blood regulatory T cells. Front Immunol. 2016;7:71. doi:10.3389/fimmu.2016.00071
118. Dang AT, Marsland BJ. Microbes, metabolites, and the gut-lung axis. Mucosal Immunol. 2019;12(4):843–850. doi:10.1038/s41385-019-0160-6
119. Felmlee MA, Morse BL, Morris ME. γ-hydroxybutyric acid: pharmacokinetics, pharmacodynamics, and toxicology. AAPS J. 2021;23(1):22. doi:10.1208/s12248-020-00543-z
120. Kent-Dennis C, Penner GB. Effects of a proinflammatory response on metabolic function of cultured, primary ruminal epithelial cells. J Dairy Sci. 2021;104(1):1002–1017. doi:10.3168/jds.2020-19092
121. Kotlyarov S. Role of short-chain fatty acids produced by gut microbiota in innate lung immunity and pathogenesis of the heterogeneous course of chronic obstructive pulmonary disease. Int J Mol Sci. 2022;23(9):4768. doi:10.3390/ijms23094768
122. Mao J, Li Y, Bian Q, et al. The Bufei Jianpi formula improves mucosal immune function by remodeling gut microbiota through the SCFAs/GPR43/NLRP3 pathway in chronic obstructive pulmonary disease rats. Int J Chron Obstruct Pulmon Dis. 2022;17:1285–1298. doi:10.2147/COPD.S359428
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
